Abstract
Posterior reversible encephalopathy syndrome is a clinicoradiologic entity that may present with headaches, altered mental status, seizures and visual loss as well as specific neuroimaging findings. We report a case of a 74-year-old woman receiving adjuvant gemcitabine chemotherapy as monotherapy for a stage IIa pancreatic adenocarcinoma, who developed posterior reversible encephalopathy syndrome.
Key Words: Posterior reversible encephalopathy syndrome, Gemcitabine, Chemotherapy
Introduction
Posterior reversible encephalopathy syndrome (PRES) is a clinicoradiologic entity characterized by headaches, altered mental status, seizures, and visual loss and is associated with white matter vasogenic edema predominantly affecting the posterior occipital and parietal lobes of the brain [1, 2, 3, 4, 5, 6].
The pathophysiology of PRES remains unclear. Two pathophysiologic mechanisms have been proposed regarding cerebral autoregulation: cerebral vasospasm, which results in cytotoxic edema [7, 8], and vasodilatation, which results in vasogenic edema [3, 9, 10]. The latter is more favored by most experimental and clinical data [11, 12, 13, 14, 15]. The pathophysiology of PRES also implicates endothelial dysfunctions, such as preeclampsia or cytotoxic therapies, especially in cases without severe hypertension [1, 16, 17].
Numerous factors can trigger this syndrome, the most common being acute elevation of blood pressure, abnormal renal function and immunosuppressive therapy [1]. Other possible etiologies are eclampsia [7, 18, 19, 20, 21], lupus [22, 23], transplantation [24], neoplasia and chemotherapy treatment [25], systemic infections [26], and acute or chronic renal disease [27, 28].
Gemcitabine has been associated with PRES; nevertheless, the contributory effects of other drugs administered simultaneously with or previously to gemcitabine are not well clarified [29]. The purpose of this report is to present a case treated with gemcitabine as monotherapy.
Case Report
A 74-year-old woman was diagnosed with pancreatic cancer without evidence of metastasis. She underwent pancreaticoduodenectomy, which revealed no regional lymph node metastases or microscopic residual disease (T3 N0 M0). After 4 weeks, the patient was started on her first course of adjuvant treatment with gemcitabine (1,000 mg/m2 on days 1, 8 and 15 of each 28-day cycle). Her ECOG performance status was 1.
One day after the beginning of the third chemotherapy cycle, the patient developed severe headache. After a few hours, she experienced a tonic-clonic seizure and visual blurring. At that time, her blood pressure was 170/90 mm Hg and her creatinine level was 1.4 mg/dl (2 months before, it was 1.0 mg/dl). A head computed tomography was obtained, which showed mild focal hypodensity in both occipital lobes without any evidence of brain metastasis. In addition, a brain magnetic resonance imaging (MRI; T2 and fluid-attenuated inversion recovery image sequences) was performed, which revealed a subcortical T2 hyperintensity without enhancement, apparent on both the occipital and temporal lobes (fig. 1).
Fig. 1.
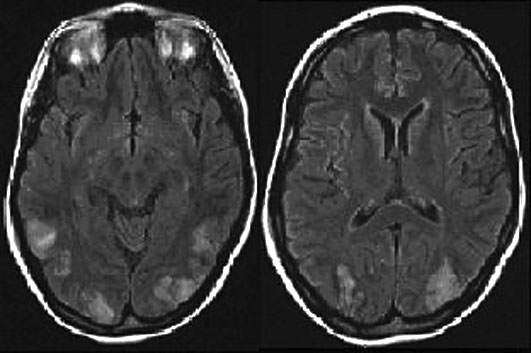
Brain MRI showing the subcortical edema in the occipital and temporal lobes.
The patient was treated with phenytoin and had no further seizures. After 10 days, the patient was asymptomatic and after 2 weeks, she underwent a follow-up brain MRI, which showed no cortical or subcortical T2 hyperintensity (fig. 2).
Fig. 2.
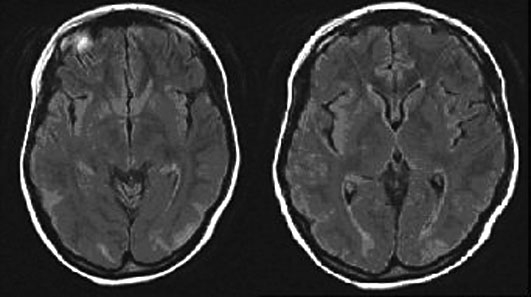
Brain MRI showing a reduction of the subcortical edema.
Discussion
The cause of PRES is not yet understood. Hypertension with failed autoregulation and hyperperfusion remains a popular consideration for developing brain edema [1]. The suggested pathophysiologic mechanisms are cerebral vasospasm with resulting ischemia within the involved territories and a breakdown in cerebrovascular autoregulation with ensuing interstitial extravasation of fluid [8].
The most characteristic imaging pattern in PRES is the presence of an edema involving the white matter of the posterior portions of both cerebral hemispheres, especially the parieto-occipital regions, in a relatively symmetric pattern that spares the calcarine and paramedian parts of the occipital lobes [1, 3, 30, 31]. However, other structures such as the brain stem, cerebellum, and frontal and temporal lobes may also be involved, and although the abnormality primarily affects the subcortical white matter, the cortex and the basal ganglia may also be affected [5, 32, 33, 34].
No single antineoplastic class or agent has been consistently associated with PRES, although some chemotherapeutic agents may cause direct CNS microvascular injury [35]. PRES is more likely to be encountered after high-dose multidrug cancer therapy, typically in hematopoietic malignancies [36, 37, 38, 39].
Gemcitabine is a nucleoside analogue antineoplastic agent structurally similar to cytarabine that is approved by the US Food and Drug Administration for the use in non-small cell lung, breast, ovarian, and pancreatic cancers [40]. It is unclear if gemcitabine can cross the blood-brain barrier [41]. Neurologic toxicities with gemcitabine are uncommon and include peripheral neuropathy and somnolence in 3 and 9% of patients, respectively [42]. Few data are available showing the association of PRES and gemcitabine. Gemcitabine-associated PRES was first identified in 2001 in the treatment of non-small cell carcinoma of the lung [29]. Two studies demonstrated the association of PRES and gemcitabine in gallbladder and pancreatic cancer treatment [35, 43]. This case is the first report of PRES associated with gemcitabine monotherapy in a treatment with adjuvant intent.
Conclusion
PRES is an entity not well known by neurologists and radiologists. Due to the poor knowledge of this syndrome, i.e. its cause and pathophysiology are not yet fully defined, it is sometimes not recognized. However, because of the increasing number of neuroimaging studies that have been conducted as well as of therapies that can induce PRES (which increases the number of patients treated with chemotherapy or immunosuppression), this phenomenon is becoming increasingly common.
Our report demonstrates that gemcitabine per se is associated with PRES, independent of other drugs.
Footnotes
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
References
- 1.Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, Pessin MS, Lamy C, Mas JL, Caplan LR. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494–500. doi: 10.1056/NEJM199602223340803. [DOI] [PubMed] [Google Scholar]
- 2.Sheth RD, Riggs JE, Bodenstenier JB, Gutierrez AR, Ketonen LM, Ortiz OA. Parietal occipital edema in hypertensive encephalopathy: a pathogenic mechanism. Eur Neurol. 1996;36:25–28. doi: 10.1159/000117195. [DOI] [PubMed] [Google Scholar]
- 3.Hauser RA, Lacey DM, Knight MR. Hypertensive encephalopathy: magnetic resonance imaging demonstration of reversible cortical and white matter lesions. Arch Neurol. 1988;45:1078–1083. doi: 10.1001/archneur.1988.00520340032007. [DOI] [PubMed] [Google Scholar]
- 4.Weingarten K, Barbut D, Filippi C, Zimmerman RD. Acute hypertensive encephalopathy: findings on spin-echo and gradient-echo MR imaging. AJR Am J Roentgenol. 1994;162:665–670. doi: 10.2214/ajr.162.3.8109519. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz RB, Jones KM, Kalina P, Bajakian RL, Mantello MT, Garada B, Holman BL. Hypertensive encephalopathy: findings on CT, MR imaging, and SPECT imaging in 14 cases. AJR Am J Roentgenol. 1992;159:379–383. doi: 10.2214/ajr.159.2.1632361. [DOI] [PubMed] [Google Scholar]
- 6.Fisher M, Maister B, Jacobs R. Hypertensive encephalopathy: diffuse reversible white matter CT abnormalities. Ann Neurol. 1985;18:268–270. doi: 10.1002/ana.410180219. [DOI] [PubMed] [Google Scholar]
- 7.Lewis LK, Hinshaw DB, Jr, Will AD, Hasso AN, Thompson JR. CT and angiographic correlation of severe neurological disease in toxemia of pregnancy. Neuroradiology. 1988;30:59–64. doi: 10.1007/BF00341945. [DOI] [PubMed] [Google Scholar]
- 8.Port JD, Beauchamp NJ., Jr Reversible intracerebral pathologic entities mediated by vascular autoregulatory dysfunction. Radiographics. 1998;18:253–267. doi: 10.1148/radiographics.18.2.9536483. [DOI] [PubMed] [Google Scholar]
- 9.Strandgaard S, Paulson OB. Cerebral autoregulation. Stroke. 1984;15:413–416. doi: 10.1161/01.str.15.3.413. [DOI] [PubMed] [Google Scholar]
- 10.Nag S, Robertson DM, Dinsdale HB. Cerebral cortical changes in acute experimental hypertension: an ultrastructural study. Lab Invest. 1977;36:150–161. [PubMed] [Google Scholar]
- 11.Schwartz RB, Mulkern RV, Gudbjartsson H, Jolesz F. Diffusion-weighted MR imaging in hypertensive encephalopathy: clues to pathogenesis. Am J Neuroradiol. 1998;19:859–862. [PMC free article] [PubMed] [Google Scholar]
- 12.Mukherjee P, McKinstry RC. Reversible posterior leukoencephalopathy syndrome: evaluation with diffusion-tensor MR imaging. Radiology. 2001;219:756–765. doi: 10.1148/radiology.219.3.r01jn48756. [DOI] [PubMed] [Google Scholar]
- 13.Schaefer PW, Buonanno FS, Gonzalez RG, Schwamm LH. Diffusion-weighted imaging discriminates between cytotoxic and vasogenic edema in a patient with eclampsia. Stroke. 1997;28:1082–1085. doi: 10.1161/01.str.28.5.1082. [DOI] [PubMed] [Google Scholar]
- 14.Coley SC, Porter DA, Calamante F, Chong WK, Connelly A. Quantitative MR diffusion mapping and cyclosporine-induced neurotoxicity. AJNR Am J Neuroradiol. 1999;20:1507–1510. [PMC free article] [PubMed] [Google Scholar]
- 15.Ay H, Buonanno FS, Schaefer PW, Le DA, Wang B, Gonzalez RG, Koroshetz WJ. Posterior leukoencephalopathy without severe hypertension: utility of diffusion-weighted MRI. Neurology. 1998;51:1369–1376. doi: 10.1212/wnl.51.5.1369. [DOI] [PubMed] [Google Scholar]
- 16.Donaldson JO. The brain in eclampsia. Hypertens Pregnancy. 1994;13:115. [Google Scholar]
- 17.Roberts JM, Redman CWG. Pre-eclampsia: more than pregnancy-induced hypertension. Lancet 1993;341:1447-1451; erratum. 1993;342:504. doi: 10.1016/0140-6736(93)90889-o. [DOI] [PubMed] [Google Scholar]
- 18.Schwartz RB, Feske SK, Polak JF, DeGirolami U, Iaia A, Beckner KM, Bravo SM, Klufas RA, Chai RY, Repke JT. Preeclampsia-eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology. 2000;217:371–376. doi: 10.1148/radiology.217.2.r00nv44371. [DOI] [PubMed] [Google Scholar]
- 19.Colosimo C, Jr, Fileni A, Moschini M, Guerrini P. CT findings in eclampsia. Neuroradiology. 1985;27:313–317. doi: 10.1007/BF00339563. [DOI] [PubMed] [Google Scholar]
- 20.Naheedy MH, Biller J, Schiffer M, Azar-Kia B, Gaianopoulous J, Zarandy S. Toxemia of pregnancy: cerebral CT findings. J Comput Assist Tomogr. 1985;9:497–501. doi: 10.1097/00004728-198505000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Ishimori ML, Pressman BD, Wallace DJ, Weisman MH. Posterior reversible encephalopathy syndrome: another manifestation of CNS SLE? Lupus. 2007;16:436–443. doi: 10.1177/0961203307078682. [DOI] [PubMed] [Google Scholar]
- 22.Punaro M, Abou-Jaoude P, Cimaz R, Ranchin B. Unusual neurologic manifestations (II): posterior reversible encephalopathy syndrome (PRES) in the context of juvenile systemic lupus erythematosus. Lupus. 2007;16:576–579. doi: 10.1177/0961203307079811. [DOI] [PubMed] [Google Scholar]
- 23.Baizabal-Carvallo JF, Barragán-Campos HM, Padilla-Aranda HJ, Alonso-Juarez M, Estañol B, Cantú-Brito C, García-Ramos G. Posterior reversible encephalopathy syndrome as a complication of acute lupus activity. Clin Neurol Neurosurg. 2009;111:359–363. doi: 10.1016/j.clineuro.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 24.Bartynski WS, Tan HP, Boardman JF, Shapiro R, Marsh JW. Posterior reversible encephalopathy syndrome after solid organ transplantation. AJNR Am J Neuroradiol. 2008;29:924–930. doi: 10.3174/ajnr.A0960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hourani R, Abboud M, Hourani M, Khalifeh H, Muwakkit S. L-asparaginase-induced posterior reversible encephalopathy syndrome during acute lymphoblastic leukemia treatment in children. Neuropediatrics. 2008;39:46–50. doi: 10.1055/s-2008-1076740. [DOI] [PubMed] [Google Scholar]
- 26.Bartynski WS, Boardman JF, Zeigler ZR, Shadduck RK, Lister J. Posterior reversible encephalopathy syndrome in infection, sepsis, and shock. AJNR Am J Neuroradiol. 2006;27:2179–2190. [PMC free article] [PubMed] [Google Scholar]
- 27.Onder AM, Lopez R, Teomete U, Francoeur D, Bhatia R, Knowbi O, Hizaji R, Chandar J, Abitbol C, Zilleruelo G. Posterior reversible encephalopathy syndrome in the pediatric renal population. Pediatr Nephrol. 2007;22:1921–1929. doi: 10.1007/s00467-007-0578-z. [DOI] [PubMed] [Google Scholar]
- 28.Gokce M, Dogan E, Nacitarhan S, Demirpolat G. Posterior reversible encephalopathy syndrome caused by hypertensive encephalopathy and acute uremia. Neurocrit Care. 2006;4:133–136. doi: 10.1385/NCC:4:2:133. [DOI] [PubMed] [Google Scholar]
- 29.Russell MT, Nassif AS, Cacayorin ED, Awwad E, Perman W, Dunphy F. Gemcitabine-associated posterior reversible encephalopathy syndrome: MR imaging and MR spectroscopy findings. Magn Reson Imaging. 2001;19:129–132. doi: 10.1016/s0730-725x(01)00217-x. [DOI] [PubMed] [Google Scholar]
- 30.Duncan R, Hadley D, Bone I, Symonds EM, Worthington BS, Rubin PC. Blindness in eclampsia: CT and MR imaging. J Neurol Neurosurg Psychiatry. 1989;52:899–902. doi: 10.1136/jnnp.52.7.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Truwit CL, Denaro CP, Lake JR, DeMarco T. MR imaging of reversible cyclosporin A-induced neurotoxicity. AJNR Am J Neuroradiol. 1991;12:651–659. [PMC free article] [PubMed] [Google Scholar]
- 32.Lamy C, Oppenheim C, Méder JF, Mas JL. Neuroimaging in posterior reversible encephalopathy syndrome. J Neuroimaging. 2004;14:89–96. [PubMed] [Google Scholar]
- 33.Sanders TG, Clayman DA, Sanchez-Ramos L, Vines FS, Russo L. Brain in eclampsia: MR imaging with clinical correlation. Radiology. 1991;180:475–478. doi: 10.1148/radiology.180.2.2068315. [DOI] [PubMed] [Google Scholar]
- 34.De Klippel N, Sennesael J, Lamote J, Ebinger G, de Keyser J. Cyclosporin leukoencephalopathy induced by intravenous lipid solution. Lancet. 1992;339:1114. doi: 10.1016/0140-6736(92)90707-a. [DOI] [PubMed] [Google Scholar]
- 35.Rajasekhar A, George TJ., Jr Gemcitabine-induced reversible posterior leukoencephalopathy syndrome: a case report and review of literature. Oncologist. 2007;12:1332–1335. doi: 10.1634/theoncologist.12-11-1332. [DOI] [PubMed] [Google Scholar]
- 36.Cooney MJ, Bradley WG, Symko SC, Patel ST, Groncy PK. Hypertensive encephalopathy: complication in children treated for myeloproliferative disorders – report of three cases. Radiology. 2000;214:711–716. doi: 10.1148/radiology.214.3.r00mr19711. [DOI] [PubMed] [Google Scholar]
- 37.Morris EB, Laningham FH, Sandlund JT, Khan RB. Posterior reversible encephalopathy syndrome in children with cancer. Pediatr Blood Cancer. 2007;48:152–159. doi: 10.1002/pbc.20703. [DOI] [PubMed] [Google Scholar]
- 38.Sánchez-Carpintero R, Narbona J, López de Mesa R, Arbizu J, Sierrasesúmaga L. Transient posterior encephalopathy induced by chemotherapy in children. Pediatr Neurol. 2001;24:145–148. doi: 10.1016/s0887-8994(00)00242-3. [DOI] [PubMed] [Google Scholar]
- 39.Pihko H, Tyni T, Virkola K, Valanne L, Sainio K, Hovi L, Saarinen UM. Transient ischemic cerebral lesions during induction chemotherapy for acute lymphoblastic leukemia. J Pediatr. 1993;123:718–724. doi: 10.1016/s0022-3476(05)80845-5. [DOI] [PubMed] [Google Scholar]
- 40.Burris HA, 3rd, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo AM, Tarassoff P, Nelson R, Dorr FA, Stephens CD, Von Hoff DD. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol. 1997;15:2403–2413. doi: 10.1200/JCO.1997.15.6.2403. [DOI] [PubMed] [Google Scholar]
- 41.Plunkett W, Huang P, Xu YZ, Heinemann V, Grundewald R, Gandhi V. Gemcitabine: metabolism, mechanisms of action, and self-potentiation. Semin Oncol. 1995;22(suppl 11):3–10. [PubMed] [Google Scholar]
- 42.Gemzar_ (gemcitabine HCl for injection) [package insert] Indianapolis: Eli Lilly and Company; 2006. [Google Scholar]
- 43.Kwon EJ, Kim SW, Kim KK, Seo HS, Kim do Y. A case of gemcitabine and cisplatin associated posterior reversible encephalopathy syndrome. Cancer Res Treat. 2009;41:53–55. doi: 10.4143/crt.2009.41.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]


