Abstract
Sarcoidosis is a multisystem disease that most commonly involves the lungs and the lymph nodes, but with genitourinary tract involvement, can easily mimic testicular cancer with metastasis to the lungs. We describe the case of a 30-year-old African-American male who presented with complaints of a headache, skin lesions, and a scrotal mass. A computed tomography scan of the head showed lesions in the frontotemporal and pons region, causing obstructive hydrocephalus. An ultrasound of the scrotum showed an enlarged epididymis bilaterally as well as a solid hypoechoic ill-defined mass on the right side, separate from the intact testis. Given the high suspicion for testicular malignancy with brain metastasis, a right orchiectomy was completed. The pathology revealed non-caseating necrotizing granulomas that stained negative for tubercular and fungal organisms, which was consistent with sarcoidosis. Additionally, the patient's skin and central nervous system (CNS) lesions improved on steroids that had been started for cerebral edema. Given the predilection of testicular cancer for CNS metastasis, neurosarcoidosis can also be mistaken for testicular cancer metastasis to the CNS, as seen in our case. Differentiating testicular cancer from genitourinary sarcoidosis is difficult but can be clarified using a combination of clinical presentation, epidemiology, serum markers (ACE, AFP, B-HCG), biopsies from skin/lymph nodes, and sometimes imaging. It is critical to differentiate genitourinary sarcoidosis from malignancy, as a misdiagnosis can lead to unnecessary surgical interventions, which have important implications for future fertility. There can also be a coexistence of as well as an association between testicular cancer and sarcoidosis, which should be recognized by health care providers.
Key Words: Genitourinary sarcoidosis, Systemic sarcoidosis, Testicular cancer, Differentiation, Serum prognostic markers, Ultrasound, Biopsy
Case Presentation
A 30-year-old African-American male presented with a 3-week history of a gradually progressive frontal headache, with enlarging skin nodules and a progressively enlarging painless right hemiscrotal mass during the past year. The patient's mother and several first-degree relatives had a history of sarcoidosis. The patient denied any history of contact with tuberculosis, fever, anorexia, weight loss, hematuria, testicular pain, cough or visual disturbances. A PPD test (tuberculin skin test) taken 2 months before admission was negative. Vitals on presentation were unremarkable, and pertinent positive physical examination findings included an indurated, nodular lesion on the upper lip, with a lesion on the left nasolabial fold. There was no palpable lymphadenopathy. Laboratory studies such as complete metabolic panel, complete blood count, and urinalysis were within normal limits. A computed tomography (CT) scan of the head showed lesions in the frontotemporal and pons region, causing obstructive hydrocephalus. A CT of the chest did not reveal any hilar/mediastinal lymphadenopathy or evidence of sarcoidosis, and a CT of the abdomen/pelvis demonstrated a hydrocele with a right hemiscrotal mass without any lymphadenopathy. An ultrasound of the scrotum showed an enlarged epididymis bilaterally as well as a solid hypoechoic ill-defined mass on the right side (fig. 1), separate from the intact testis. Laboratory work-up for testicular malignancy revealed normal human chorionic gonadotropin (HCG), LDH and alpha fetoprotein (AFP) levels. A HIV antibody and a repeat PPD test were nonreactive. Given the high suspicion for testicular malignancy with brain metastasis, a right orchiectomy was completed, with the subsequent pathology days later displaying a normal testis with a distorted architecture of the epididymis. Pathology also identified granulomas (fig. 2, fig. 3, fig. 4) that stained negative for fungal organisms as well as for Mycobacterium tuberculosis. Aspirated hydrocele fluid did not reveal any bacterial, fungal or mycobacterial growth. At the time of presentation, the patient was initiated on steroids, given the concern for cerebral edema from a central nervous system (CNS) malignancy. The patient's headache improved and his skin lesions started to resolve within a few days. Based on the clinical presentation, his family history, response to steroids and the testicular pathology report, a diagnosis of sarcoidosis was made. The patient was discharged on prednisone for a 3-month time period. A follow-up head CT showed a decrease in the patient's obstructive hydrocephalus as well as a decrease in size of the CNS lesions.
Fig. 1.

Scrotal ultrasound showing a solid hypoechoic ill-defined mass.
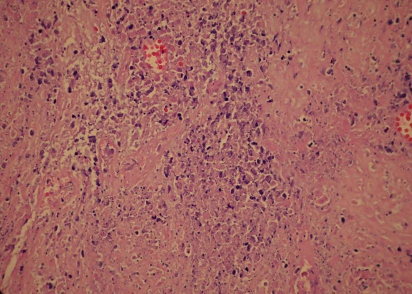
Fig. 2.
Photomicrograph showing a granulomatous inflammation next to the testes.
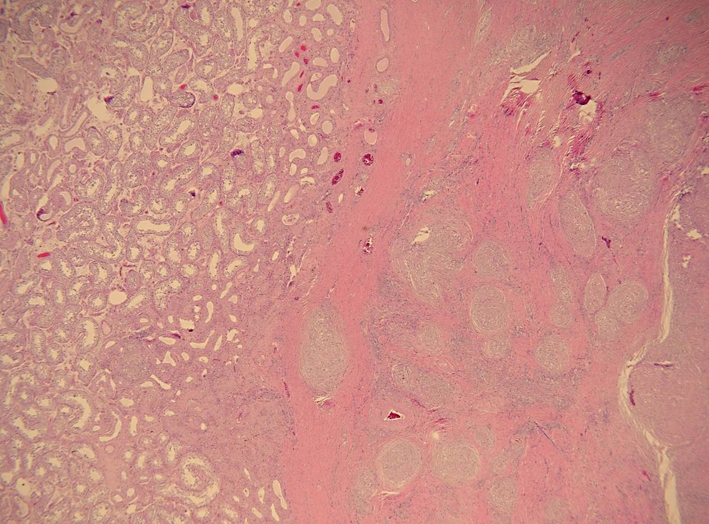
Fig. 3.
Photomicrograph showing noncaseating sarcoid-like granulomas.
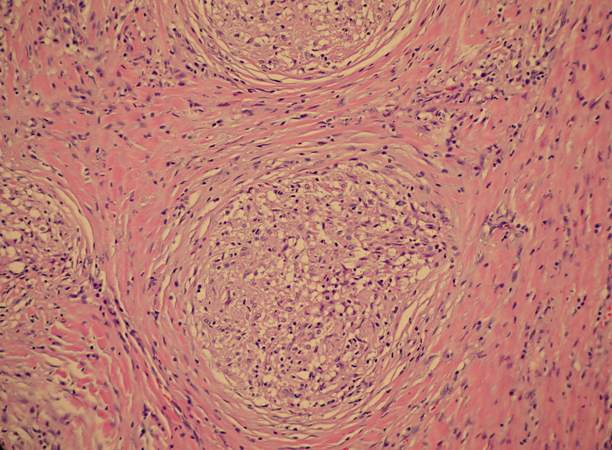
Fig. 4.
Photomicrograph showing necrosis within noncaseating granulomas.
Discussion
Testicular malignancy, which is the most common tumor in young males, is the leading differential that must be ruled out in males younger than 35 years old who experience scrotal swelling or a scrotal mass, especially given the fact that genitourinary sarcoidosis is also likely to present in this same population. In fact, testicular cancer and sarcoidosis can be very difficult to distinguish. For example, there are reported cases where systemic sarcoidosis has been interpreted as metastatic testicular cancer, leading to inadvertent chemotherapy [1] as well as orchiectomy (as in our case). It is also critical to distinguish sarcoidosis from testicular cancer early on, as testicular cancer requires aggressive surgery and systemic chemotherapy, especially given the favorable response to chemotherapy in testicular cancer.
Thus, how can testicular cancer be differentiated from sarcoidosis? There are subtleties that help distinguish the two from each other epidemiologically, serologically, and pathologically. Generally, testicular cancer affects Caucasian males while sarcoidosis is more common among African-American males [2]. However, the rates of testicular cancers are rising in African-American males [2]. The imaging modalities in evaluating testicular masses (ultrasound) can be helpful in differentiating sarcoidosis from testicular cancer, but often times it is unrevealing (as seen in our patient). Serum markers can also be extremely helpful in the differentiation between these two conditions, as serum angiotensin-converting enzyme (ACE) is elevated in 75% of untreated active sarcoidosis patients, but not in patients with testicular cancer [2]. Additionally, in non-seminoma testicular cancers, serum AFP and beta-HCG (B-HCG) levels are elevated in approximately 50% of patients [2]. Lastly, pathology of an extratesticular lesion may be very useful in differentiation. Biopsy of skin lesions in sarcoidosis or endoscopic ultrasound biopsy of mediastinal lymph nodes can reveal a more definitive diagnosis. In our patient, corticosteroids, originally started to decrease cerebral edema due to supposed testicular cancer metastasis, subsequently shrunk the CNS lesions. However, this was unfortunately after the orchiectomy.
There is also an association between testicular cancer and sarcoidosis, which seems to be not well known to most health care providers. A review of the literature performed by Paparel, a urologist at the Memorial Sloan-Kettering Cancer Center, and his colleagues [3] noted that there was a coexistence of sarcoidosis or a sarcoid-like reaction in patients with testicular cancer. In half of the cases where testicular cancer and sarcoidosis coexisted, testicular cancer was diagnosed prior to sarcoidosis. Thirty-one percent of cases of testicular cancer that coexisted with sarcoidosis were diagnosed simultaneously. Sarcoidosis was associated with different types of testicular cancer, with seminoma being the most common. In 80% of these cases with concomitant sarcoidosis, the sarcoidosis regressed simultaneously. The coexistence of sarcoidosis and testicular cancer did not change the management of testicular cancer or the overall prognosis [3]. With reference to the aforementioned, the dilemma arises in cases where a false diagnosis of testicular cancer is made, when, in fact, sarcoidosis is the correct diagnosis, as seen in our patient. However, given this strong association between sarcoidosis and testicular cancer, it is noted that long-term monitoring and follow-up of our patient may be necessary.
Genitourinary sarcoidosis, although rare, should also be considered in differentials of urologic conditions. Pulmonary hilar lymphadenopathy is present in 90% of patients with genitourinary sarcoidosis, which makes distinguishing it from malignancy even more difficult [4]. Over 80% of patients with genitourinary sarcoidosis present with intrathoracic manifestations [5], but approximately 30% present with extrapulmonary involvement of the skin, liver, spleen, eyes, CNS, salivary glands, mucosa, joints, heart, bone marrow, muscle and kidneys [6]. The frequent involvement of pulmonary sarcoidosis can be mistaken for pulmonary metastasis in the setting of genitourinary sarcoidosis or a testicular mass [6]. Additionally, there have been case reports of bilateral epididymal sarcoidosis presenting without radiological evidence of intrathoracic lesions [7]. Similarly, CNS sarcoidosis can be mistaken as CNS metastasis from testicular cancer in the setting of a testicular mass [7], which was seen in our patient. Testicular cancer does have a predilection for CNS metastasis and is among the 5 most common cancers to metastasize to the brain. Furthermore, cases of caseating granulomas have also been reported in genitourinary sarcoidosis, which requires sarcoidosis to also be differentiated from fungus or tuberculosis [8], which was performed in our case. The differential for genitourinary sarcoidosis is broad: tuberculosis, syphilis, sperm granuloma, filarial granuloma, lymphogranuloma venereum, granuloma inguinale, blastomycosis, coccidiomycosis, actinomycosis, schistosomiasis, and Wegener's granulomatosis [7] need to be ruled out in the evaluation of genitourinary sarcoidosis. Lastly, other malignancies such as lymphoma or other genitourinary malignancies besides testicular cancer must be considered in the appropriate clinical context.
The last consideration that clinicians must recognize is that testicular cancer may also have a primary extragonadal presentation, which involves an initial presentation without testicular involvement. The aforementioned least commonly involves seminomas [9]. Lastly, there is an entity called the ‘burned out phenomenon’, in which there is extragonadal involvement without any histologic involvement of the testes, which may occur in advanced seminoma. In the rare case of the ‘burned out phenomenon’, the area of the primary testicular tumor may be replaced by scar tissue. Often, the diagnosis may only be made by histologic examination after removal of the testicle. Adjuvant radiotherapy or chemotherapy along with testicular removal will be based on the histologic diagnosis of the extranodal presentation [9].
Thus, management of testicular cancer and genitourinary sarcoidosis should have an emphasis on differentiation based on risk factors, serum prognostic markers, skin/lymph node biopsies, response to medical treatment, tolerance for surgery, and fertility status. Some experts in the field of genitourinary sarcoidosis advocate reserving orchiectomy and steroid therapy for severe refractory or disseminated cases, while other experts prefer an exploration with intra-operative ultrasound/biopsies/frozen section analysis to rule out malignancy [4].
Conclusion
Sarcoidosis is a multisystem disease that most commonly involves the lungs and the lymph nodes but, with genitourinary tract involvement, can easily mimic testicular cancer with metastasis to the lungs. Given the predilection of testicular cancer for CNS metastasis, neurosarcoidosis can also be mistaken for CNS testicular cancer metastasis, as seen in our case. Differentiating testicular cancer from genitourinary sarcoidosis is difficult but can be clarified using a combination of clinical presentation, epidemiology, serum markers (ACE, AFP, B-HCG), biopsies from skin/lymph nodes, and sometimes imaging. It is critical to differentiate genitourinary sarcoidosis from malignancy, as a misdiagnosis can lead to unnecessary surgical interventions, which have important implications for future fertility. There can also be a coexistence of testicular cancer and sarcoidosis, which should be recognized by health care providers.
Acknowledgements
We would like to thank Dr. Ian Hoffman in the Department of Pulmonary/Critical Care for his support and encouragement. We appreciate his dedication to ensuring the highest standard of care. We would also like to thank Dr. Stanley Redwood in the Department of Urology for his guidance, support, and input. We especially appreciate Dr. Redwood's input into the extragonadal presentation of testicular cancer as well as the burned out phenomenon.
Footnotes
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
Both authors contributed equally to the manuscript.
References
- 1.Kok TC, Haasjes JG, Spinter TA, ten Kate FJ. Sarcoid-like lymphadenopathy mimicking metastatic testicular cancer. Cancer. 1991;68:1845–1847. doi: 10.1002/1097-0142(19911015)68:8<1845::aid-cncr2820680835>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 2.Baughman RP: Sarcoidosis: Lung Biology in Health and Disease, vol 210. Taylor & Francis Group, 2006, pp 656-657.
- 3.Paparel P, Devonec M, Perrin P, Ruffion A, Decaussin-Petrucci M, Akin O, Sheinfeld J, Guillonneau B. Association between sarcoidosis and testicular carcinoma: a diagnostic pitfall. Sarcoidosis Vasc Diffuse Lung Dis. 2007;24:95–101. [PubMed] [Google Scholar]
- 4.Massarweh NN, Bhalani VK, Shaw KK, Crawford B, Lang E, Davis R. Testicular presentation of sarcoidosis and organ preservation: case report and review of management strategies. Urology. 2006;67:200. doi: 10.1016/j.urology.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 5.Kodama K, Hasegawa T, Egawa M, Tomosugi N, Mukai A, Namiki M. Bilateral epididymal sarcoidosis presenting without radiographic evidence of intrathoracic lesion: review of sarcoidosis involving the male reproductive tract. Int J Uro. 2004;11:345–348. doi: 10.1111/j.1442-2042.2004.00783.x. [DOI] [PubMed] [Google Scholar]
- 6.Rizzato G. Extrapulmonary presentation of sarcoidosis. Curr Opin Pulm Med. 2001;7:295–297. doi: 10.1097/00063198-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Ryan DM, Lesser BA, Crumley LA, Cartwright HA, Peron S, Haas GP, Bower G. Epididymal sarcoidosis. J Urol. 1993;149:134–136. doi: 10.1016/s0022-5347(17)36023-8. [DOI] [PubMed] [Google Scholar]
- 8.Kuramoto Y, Shindo Y, Tagami H. Subcutaneous sarcoidosis with extensive caseation necrosis. J Cutan Pathol. 1988;15:188–190. doi: 10.1111/j.1600-0560.1988.tb00541.x. [DOI] [PubMed] [Google Scholar]
- 9.Perimenis P, Athanasopoulos A, Geraghty J, Macdonagh R. Retroperitoneal seminoma with 'burned out' phenomenon in the testis. Int J Urol. 2005;12:115–116. doi: 10.1111/j.1442-2042.2004.00987.x. [DOI] [PubMed] [Google Scholar]