Abstract
An appendicolith is composed of firm feces and some mineral deposits. After increased use of abdominal computed tomography, appendicoliths are more frequently detected. Most of the patients with appendicolith are asymptomatic. However, an appendicolith may be associated with complicated appendicitis with serious outcomes. We reported three patients who exhibited different clinical symptoms due to appendicolithiasis. While one of the patients was confused with urolithiasis, the other two patients presented with phlegmenous and perforated appendicitis. We submit that appendicoliths may present different clinical findings and can mimic several pathologies including urinary disorders.
Keywords: Abdominal pain, appendicitis, appendicolith
Background
Appendicolith is a conglomeration of firm feces with some mineral deposits. It is usually found accidentally in abdominal computed tomography (CT) without any signs of appendicitis. Appendicolith may obstruct the appendix lumen, causing appendicitis and is found in approximately 10% of patients with appendix inflammation.1 Appendicitis which is caused by appendicolith is more commonly associated with perforation and abscess formation.
Appendicoliths are more commonly encountered after the development of imaging techniques in recent decades. They can present with different clinical symptoms. Most of the patients with appendicoliths are asymptomatic. However, appendicoliths may also cause serious appendicular inflammation and peritonitis. In this study, we reported three patients who had been operated on for appendicitis, caused by appendicolithiasis.
Case 1
A twenty-seven year old male patient was admitted to the emergency department, three days ago with abdominal pain, nausea and vomiting. There was minimal tenderness in the right lower quadrant on physical examination. Labaratory tests including leukocyte count, urine analysis, hepatic and renal function tests were normal. A stone, approximately 1 cm in diameter inside the right kidney was detected in abdominal ultrasonography. The diagnosis of renal colic had been established and the patient was treated with analgesics. He was re-admitted to the emergency room after three days with continous abdominal pain, nausea and vomiting. His vital signs were normal. On physical examination, there was rebound tenderness and defence in the right lower quadrant. White blood cell count was 13.400 cell/mm3 (Normal: 4.800–10.800 cell/mm3) and CRP was 12.5 mg/dL (Normal: 0.0–1.0 mg/dL). Abdominal computed tomography revealed an opacity, 1.5 cm in diameter, inside the appendix. Laparotomy was performed. Upon examination a phlegmenous appendicitis was found. An appendicolith was detected inside the appendix lumen. An appendectomy was performed. The postoperative period was uneventful. He was discharged without complication.
Case 2
A twenty year old male patient presented with a two day history of abdominal pain, nausea and vomiting. On physical examination, there was muscular defence and rebound tenderness in the right lower quadrant. A white blood cell count of 15.800 cell/mm3 (Normal: 4.800–10.800 cell/mm3) was detected. Other labarotory tests were within normal limits. Abdominal x-ray examination revealed a radio-opacity in the right lower quadrant (Fig. 1). Abdominal ultrasonography showed a tubular lesion, confirming the diagnosis of acute appendicitis. The patient underwent laparotomy and phlegmenous appendicitis was identified (Fig. 2). Appendectomy was performed successfully. An appendicolith was extracted (Fig. 3). The postoperative course was uneventful. Histopathological examination revealed a phlegmenous appendicitis (Fig. 4). The patient was discharged home on the first postoperative day.
Figure 1.
An opacity (appendicolith) in abdominal x-ray.
Figure 2.
A huge appendicolith, located in the base of the appendix causing appendicitis.
Figure 3.
Extracted appendicolith.
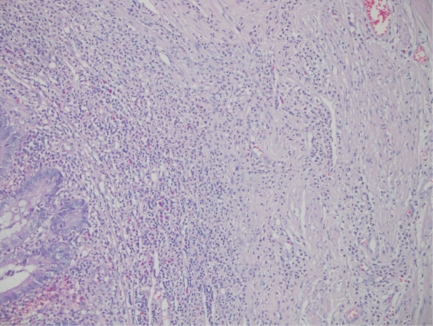
Figure 4.
Phlegmenous appendicitis. Neutrophils are infiltrating mucosa, submucosa and lamina propria (H&E × 200).
Case 3
An eighteen year old male patient presented with one day of abdominal pain, nausea and vomiting. On physical examination, rebound tenderness and defence in right lower quadrant were detected. The leukocyte count was 15.400 cell/mm3 (Normal: 4.800–10.800 cell/mm3) and CRP was 17.5 mg/dL (Normal: 0.0–1.0 mg/dL). The appendix was 9.8 mm in diameter in abdominal USG and there was an appendicolith within the appendix lumen. A gangrenous and perforated appendix was found in surgical exploration. There was purulent fluid in the right paracolic region. The appendectomy was performed. A drain was placed into the douglas pouch. The abdominal layers were closed. The patient was treated postoperatively with intravenous Ceftriaxone 2 gr/day and Metronidazole 1 gr/day. Histopathological examination of the appendix revealed a gangrenous appendicitis (Fig. 5). There was no problem in the postoperative period. The patient was discharged on the 3rd postoperative day.
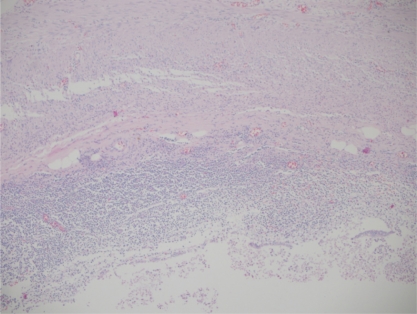
Figure 5.
Gangrenous appendicitis. Ulceration in appendix mucosa and neutrophil infiltration in submucosa and lamina propria (H&E ×100).
Discussion
Acute appendicitis is one of the most common surgical emergencies worldwide affecting approximately 7% of the general population in a lifetime.2 The obstruction of the lumen triggers the inflammation process in the appendix. The most common pathologies associated with lumen obstruction are lymphoid hyperplasia, fecalith, stricture and appendicolith. Stasis and bacterial colonization in the appendix lumen result in appendicitis.
The appendicolith is formed by firm, dense stool and mineral deposits. It is also known as appendiceal calculi, appendiceal enterolith or appendicular lithiasis. Appendicoliths are usually seen in pediatric populations and young adults. They are detected more frequently in men.3 As a nidus for appendicolith, the prevelance of fecalith has been reported as 3% in the population by Jones et al. They also stated that the low-fiber diet has been associated with increased risk of fecalith formation.4
Most appendicoliths are asymptomatic. They are usually detected incidentally with CT in an otherwise normal appendix. Robinowitz et al5 conducted a study on 74 patients with appendicolithiasis. They followed-up patients without surgery, in their first presentation. Fifty-two of these patients (70%) did not return with any complaint. Twenty-two patients were re-admitted with abdominal pain and appendectomy was performed. There were only five patients with inflammed appendix at operation. They concluded that an appendicolith may be associated with increased risk of appendicitis but was not a pure indication for appendectomy. One of our patients presented with classical signs of acute appendicitis. He was diagnosed as acute appendicitis with giant appendicolith in exploration. The appendicolith was found in the base of the appendix. Although it was a very huge stone, there was no signs of gangrene or perforation. We found only two cases of giant appendicolithiasis reported in the literature.6,7
Appendicoliths are seen in about 10% of patients with acute appendicitis.1 They are more frequently associated with appendix perforation and abscess formation.8,9 The appendicolith obstructs the appendix lumen. It also destroys the mucosa with it’s local mass effect. Gangrene in the appendix is inevitable. The patient, in case 2 was operated on due to perforated, gangrenous appendicitis within 24 hours after the beginning of his symptoms. It is important to point out that patients with appendicolithiasis are at increased risk of appendix perforation and abscess formation.
Appendicolith may cause intermittent abdominal pain. It may mimic stone disease of the genitourinary tract. Sometimes it can be difficult to differentiate acute appendicitis from urolithiasis. Both of these pathologies may cause leukocytosis and hematuria. Abdominal findings such as right lower quadrant pain and rebound tenderness can be detected in appendicitis and urolithiasis. Appendicoliths can be detected in abdominal x-ray when they are sufficiently calcified. USG and CT may also help in the diagnosis of an appendicolith. The patient, in case 3 was misdiagnosed as urolithiasis with USG in his first admittance. The definitive diagnosis of appendicitis and appendicolithiasis could be done with abdominal CT.
In conclusion, after widespread use of CT, appendicoliths were encountered more commonly. They have different clinical presentation. While most of the cases are asymptomatic, appendicoliths may also cause appendicitis with serious complications including perforation and intra-abdominal abscess formation.
Footnotes
Authors Contributions
BK and CE treated and followed-up the patients. BK conducted the literature search and wrote the manuscript. Both authors have read and approved the final manuscript.
Disclosures
This manuscript has been read and approved by all authors. This paper is unique and is not under consideration by any other publication and has not been published elsewhere. The authors and peer reviewers of this paper report no conflicts of interest. The authors confirm that they have permission to reproduce any copyrighted material. Written consent was obtained from the patient or relative for publication of this study.
References
- 1.Teke Z, Kabay B, Erbiş H, Tuncay OL. Appendicolithiasis causing diagnostic dilemma: a rare cause of acute appendicitis (report of a case) Ulus Travma Acil Cerrahi Derg. 2008;14:323–5. [PubMed] [Google Scholar]
- 2.Singh AK, Hahn PF, Gervais D, Vijayraghavan G, Mueller PR. Dropped appendicolith: CT findings and implications for management. AJR Am J Roentgenol. 2008;190:707–11. doi: 10.2214/AJR.07.2917. [DOI] [PubMed] [Google Scholar]
- 3.Nitecki S, Karmeli R, Sarr MG. Appendiceal calculi and fecaliths as indications for appendectomy. Surg Gynecol Obstet. 1990;171:185–8. [PubMed] [Google Scholar]
- 4.Jones BA, Demetriades D, Segal I, Burkitt DP. The prevalance of appendiceal fecaliths in patients with and without appendicitis. A comparative study from Canada and South Africa. Ann Surg. 1985;202:80–2. doi: 10.1097/00000658-198507000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rabinowitz CB, Egglin TK, Beland MD, Mayo-Smith WW. Outcomes in 74 patients with an appendicolith who did not undergo surgery: is follow-up imaging necessary? Emerg Radiol. 2007;14:161–5. doi: 10.1007/s10140-007-0613-1. [DOI] [PubMed] [Google Scholar]
- 6.Keating JP, Memon S. Giant appendicolith. Gastrointest Endosc. 2005;61:292–3. doi: 10.1016/s0016-5107(04)02547-7. [DOI] [PubMed] [Google Scholar]
- 7.Seshanarayana KN, Keats TE. Giant appendicolith. Va Med Mon. 1970;97:544–5. [PubMed] [Google Scholar]
- 8.Lin BH, Stull MA, Grant T. Extraluminal appendicolith in perforating appendicitis. AJR Am J Roentgenol. 1996;166:1499. doi: 10.2214/ajr.166.6.8633481. [DOI] [PubMed] [Google Scholar]
- 9.Vyas RC, Sides C, Klein DJ, Reddy SY, Santos MC. The ectopic appendicolith from perforated appendicitis as a cause of tubo-ovarian abscess. Pediatr Radiol. 2008;38:1006. doi: 10.1007/s00247-008-0889-7. [DOI] [PubMed] [Google Scholar]