Abstract
Background
The prompt administration of coronary reperfusion therapy for patients with an evolving acute myocardial infarction (AMI) is crucial in reducing mortality and the risk of serious clinical complications in these patients. However, long-term trends in extent of pre-hospital delay, and factors affecting patient’s care seeking behavior, remain relatively unexplored, especially in men and women of different ages. The objectives of this study were to examine the overall magnitude, and 20 year trends (1986–2005), in duration of pre-hospital delay in middle-aged and elderly men and women hospitalized with AMI.
Methods and Results
The study sample consisted of 5, 967 residents of the Worcester, MA, metropolitan area hospitalized at all greater Worcester medical centers for AMI between 1986 and 2005 who had information available about duration of pre-hospital delay.
Compared with men <65 years, patients in other age-sex strata exhibited longer pre-hospital delays over the 20-year period under study. The multivariable adjusted medians of pre-hospital delay were 1.96, 2.07, and 2.57 hours for men <65 years, men 65 –74 years, and men ≥75 years, and 2.08, 2.33, and 2.27 hours for women <65 years, women 65–74 years, and women ≥75 years, respectively. These age and sex differences have narrowed over time which has been largely explained by changes in patient’s comorbidity profile and AMI associated characteristics.
Conclusions
Our results suggest that duration of pre-hospital delay in persons with symptoms of AMI has remained essentially unchanged during the 20 year period under study and elderly individuals are more likely to delay seeking timely medical care than younger persons.
Keywords: Pre-hospital Delay, Acute Myocardial Infarction, Age and Sex differences
Introduction
The prompt administration of reperfusion therapy to patients with an evolving acute myocardial infarction (AMI) can be crucial to reducing mortality and serious complications in these patients. Results from prior studies have shown that reperfusion treatment is most effective if patients with ST-segment elevation myocardial infarction are treated promptly, particularly within one hour of acute symptom onset.1,2 Although an association between extent of pre-hospital delay and outcomes after non-ST-segment elevation myocardial infarction has not been firmly established, it is assumed that earlier evaluation and management of these patients would be preferable.
Despite the importance of seeking medical care as soon as possible after the onset of acute coronary symptoms, upwards of one half of patients with AMI delay seeking medical care by more than 2 hours,3,4 and upwards of one quarter of patients with AMI delay seeking care by more than 6 hours.3–5 Several previous studies have also suggested that extent of pre-hospital delay is associated with delays in the receipt of effective hospital therapies,4,6 primarily coronary reperfusion therapy.
Although considerable efforts have been expended to educate patients about the symptoms of AMI, and the importance of seeking medical care promptly, the care seeking behavior of patients hospitalized with AMI has not changed appreciably.7–9 The Rapid Early Action for Coronary Treatment (REACT) trial, a randomized, controlled trial of 20 pair-matched U.S. communities, was designed to examine the effects of a community-wide intervention on patient delay and emergency medical service use in patients with acute coronary disease.10,11 The intervention targeted the mass media, community organizations, and professional, public, and patient education. Despite the intensive 18-month long intervention, time from symptom onset to hospital arrival for patients with acute chest pain did not change significantly between intervention and control communities over the course of this trial. A recent trial (2000–2006) using a nurse-counseling intervention for patients with documented coronary heart disease (CHD) that focused on information, emotional issues, and social factors also failed to reduce extent of pre-hospital delay in approximately 3,500 patients with documented CHD.12
A limited number of previous studies have examined age and sex differences in duration of pre-hospital delay in patients hospitalized with AMI. Several studies have found that women are more likely to delay seeking timely medical care compared with men8,9,13–15 whereas other studies have suggested that there are no sex differences in patterns of delay.3,7 The majority of prior studies have demonstrated that older individuals are more likely to delay seeking medical care after developing symptoms of AMI,7–9 though several studies have failed to find differences in medical care seeking behavior according to age.13,15,16 More importantly, few studies have examined whether age and sex differences in extent of delay in patients hospitalized with AMI have changed over time, particularly from the more generalizable perspective of a population-based investigation.7–9
Due to national interest in age and sex differences in disease outcomes, the increasing number of women and older individuals hospitalized with acute coronary disease, and because a number of prior studies have not controlled for the effects of various potentially confounding variables in examining age and sex differences in extent of pre-hospital delay, it is important to assess long-term trends in delay patterns among different age-sex groups to see if improvement, or lack thereof, is occurring in some groups but not others. Targeting of educational efforts to high-risk groups to decrease extent of pre-hospital delay may also have an important impact on patient related outcomes. Therefore, we examined age and sex differences, as well as 20 year trends (1986–2005), in duration of pre-hospital delay in residents of a large central New England metropolitan area hospitalized with validated AMI at all central Massachusetts medical centers.17,18
Methods
The Worcester Heart Attack Study is an ongoing population-based investigation that is examining long-term trends in the incidence and case-fatality rates of AMI among residents of the Worcester metropolitan area hospitalized at all 16 greater Worcester medical centers in 15 biennial periods between 1975 and 2005.17,18 Fewer hospitals (n=11) have been included during recent study years due to hospital closures, mergers, and conversion to chronic care facilities.
The details of this study have been described previously.17,18 In brief, computerized printouts of patients discharged from all greater Worcester hospitals with possible AMI were obtained, and International Classification of Disease (ICD) codes for possible AMI (ICD-9 codes 410–414, 786.5) were reviewed for purposes of sample selection. The vast majority of validated cases of AMI came from ICD-9 diagnostic rubric 410 (AMI), followed by a small number of cases from ICD rubric 411 (other acute and subacute forms of CHD). Cases of possible AMI treated at all greater Worcester medical centers were independently validated according to predefined criteria for AMI. The diagnosis of AMI was made on the basis of the well accepted criteria developed by the World Health Organization which includes a suggestive clinical history, serum enzyme elevations, and serial electrocardiographic findings during hospitalization; these criteria have been previously utilized in other population-based investigations of AMI including the MONICA study.19
Patients who satisfied at least 2 of these 3 criteria, and were residents of the Worcester metropolitan area, were included in this population-based investigation. Patients who developed symptoms of AMI after hospital admission, or after an interventional procedure or surgery, were excluded as were patients with an unknown time of acute symptom onset.
Data Collection
Information about patient’s demographic characteristics, medical history, clinical presentation, hospital treatment approaches, and hospital discharge status was abstracted from the hospital medical records of patients with confirmed AMI. Pre-hospital delay was defined as the time interval between the onset of symptoms suggestive of AMI and arrival time in the emergency department.6,7 This information was collected by our trained nurse and physician reviewers who reviewed any information they could find in hospital medical records which described extent of pre-hospital delay from emergency personnel, nurses, and physicians notes. Information on pre-hospital delay was collected in minutes (as a continuous variable). This variable was further categorized according to cut-points that had been commonly utilized in the published literature, based on the distribution of our data, and according to what we considered to be clinically meaningful cut-points of pre-hospital delay.
While information about age was collected from hospital medical records as a continuous variable, we described age- specific differences in extent of pre-hospital delay using categories (<65 years, 65–74 years, and ≥75 years) that have been previously used in this and in other investigations for ease of reporting and for consistency with the literature. Candidate variables considered as potential confounders of the association between age/sex and pre-hospital delay were chosen based on findings from prior studies including study year, race (white vs non-white), marital status (single, married, divorced, widowed), comorbidities (e.g., heart failure, diabetes), time of hospital admission (weekday vs. weekend), time of day (12 am-5:59 am; 6 am-11:59 am; 12 pm-5:59 pm and 6 pm-11:59 pm), and AMI order (initial vs. prior), type (Q wave vs. non–Q wave) and location (anterior vs. other). Information about whether the AMI was a non–ST-segment elevation myocardial infarction (NSTEMI) or an ST-segment elevation myocardial infarction (STEMI) was recorded beginning in 1997.
Data Analysis
Categorical data were compared between patients who delayed ≥2 hours or ≥6 hours, and those who delayed for shorter intervals, using the chi-square test. Distributions of continuous variables were checked and some variables were not normally distributed (e.g., serum triglycerides); therefore, Wilcoxon sum rank tests were used to compare the values of all variables between various patient groups according to extent of delay (e.g., <2 hours vs. ≥2 hours) for consistency. Patient characteristics were also analyzed according to age and sex (data not shown).
We examined the possible association between age/sex and extent of pre-hospital delay using two approaches. In the first approach, we used a median regression model to examine the association between age/sex with duration of pre-hospital delay (hours), taking into account the skewed distribution of pre-hospital delay. In addition, we created both multinomial logistic and ordered logistic regression models to determine the association of age/sex with our principal study outcome expressed as an ordinal variable (e.g., pre-hospital delay 0–1.9, 2–5.9, and ≥ 6 hours). Results were similar, and the assumptions of ordered logit were met, so we reported the results from our ordered logistic regression model.
In each analysis, a series of regression models were used to examine the impact of demographic characteristics, comorbidities, and clinical presentation on the association between age/sex and pre-hospital delay. The first model included only age, sex, and study year. Model 2 further adjusted for other demographic factors and medical history of various cardiovascular diseases and comorbidities. Model 3 was further adjusted for AMI associated characteristics and acute presenting symptoms (see footnotes to each table for the list of controlling variables). To assess whether any age or sex differences in extent of pre-hospital delay have changed over time, 2-way and 3-way interaction terms between age, sex, and study year were created and included in each regression model. Since the evidence supporting an association between decreased pre-hospital delay and improved short-term outcomes is strongest in patients with STEMI, we repeated all analyses in this patient subgroup.
Since 42% of the study sample had information missing from hospital records on extent of pre-hospital delay, we conducted a sensitivity analysis using a propensity-weighted method to assess whether the missing data influenced our primary study results. We constructed logistic regression models predicting missing vs. non-missing data on extent of pre-hospital delay using baseline characteristics which yielded a c statistic of 0.70. Propensity scores for non-missing data were calculated for each patient. We estimated the median regression models weighted for 1/propensity score for missing data and compared the results with analyses among patients with information available on pre-hospital delay. All covariates included in our analyses had missing information in less than 5% of cases; inasmuch, missing data were not imputed.
We also used random effect models (random intercept) to assess whether the different patient clusters within participating hospitals might have affected our observed results. To examine the impact of hospital level effects, we estimated linear random effect models with log of pre-hospital delay as the outcome. This study was approved by the Institutional Review Board at the University of Massachusetts Medical School.
Results
A total of 10,310 patients were hospitalized with a validated AMI at all greater Worcester medical centers during the 11 study years between 1986 and 2005. Patients who had information missing on pre-hospital delay (42%; n=4,334) were more likely to be older and women, to have a history of diabetes, hypertension or heart failure, to have developed important clinical complications or to have died during hospitalization, and were less likely to have reported chest pain, and to have an initial, Q-wave, or anterior MI compared with patients who had information available on delay time (Appendix 1).
The final study sample consisted of 5,976 patients in whom information on duration of pre-hospital delay was available. The average age of this sample, which was comprised of approximately three-fifths men, was 67.5 years; of these, 40% were <65 years, 26% were between the ages of 65–74 years, and 34% were ≥75 years. Women were considerably older than men at the time of hospital admission (means: 73 years vs. 64 years, p<0.001). Among 2,771 patients who were hospitalized for AMI between 1997 and 2005, approximately 47% were diagnosed as having STEMI at the time of hospital admission.
Patient Characteristics According to Duration of Pre-Hospital Delay
Patients who delayed ≥2 hours in seeking medical care after the onset of symptoms suggestive of AMI were more likely to be older (≥65 years), female, and widowed compared to those who delayed <2 hours (Table 1). Patients who delayed seeking medical care were more likely to have a history of diabetes, hypertension and heart failure, and present at greater Worcester hospitals from 6 am to 6 pm; on the other hand, these patients were less likely to have developed a Q-wave and STEMI and to report chest pain, shortness of breath, or diaphoresis than patients who sought medical care at an earlier time. Patients who delayed seeking medical care were more likely to present with higher heart rates and systolic blood pressure on admission compared to patients who exhibited shorter delay (Table 1). Demographic and clinical differences between patients who delayed ≥6 hours in seeking medical care and those who delayed < 6 hours are also displayed in Table 1.
Table 1.
Characteristics of Patients with Acute Myocardial Infarction (AMI) according to Extent of Delay in Seeking Medical Care
| Characteristic | < 2 hours (n=2,762) | ≥ 2 hours (n=3,267) | P-value | < 6 hours (n=4791) | ≥ 6 hours (n=1,238) | P-value |
|---|---|---|---|---|---|---|
| Age (years, mean) | 66.2 | 68.7 | 0.004 | 67.4 | 68.2 | 0.15 |
| Age (years, %) | ||||||
| <65 | 43.5 | 36.2 | <0.001 | 40.3 | 36.4 | 0.002 |
| 65–74 | 25.7 | 26.2 | 25.7 | 26.9 | ||
| ≥75 | 30.8 | 37.6 | 23.0 | 36.6 | ||
| Female (%) | 36.2 | 40.8 | <0.001 | 38.4 | 39.7 | 0.43 |
| White (%) | 94.6 | 94.8 | 0.82 | 94.5 | 95.4 | 0.26 |
| Marital Status (%) | ||||||
| Single | 10.9 | 9.7 | 0.001 | 10.1 | 10.7 | 0.71 |
| Married | 63.3 | 61.1 | 62.5 | 60.3 | ||
| Divorced | 7.1 | 6.4 | 6.6 | 6.9 | ||
| Widowed | 18.7 | 22.7 | 20.6 | 21.9 | ||
| Medical history (%) | ||||||
| Atrial fibrillation | 9.4 | 9.3 | 0.85 | 9.3 | 9.6 | 0.76 |
| Diabetes mellitus | 24.9 | 30.1 | <0.001 | 27.2 | 29.8 | 0.07 |
| Hypertension | 58.4 | 61.6 | 0.012 | 60.6 | 58.4 | 0.17 |
| Heart failure | 15.0 | 16.9 | 0.047 | 16.0 | 16.2 | 0.90 |
| Stroke | 8.7 | 9.2 | 0.55 | 8.9 | 9.1 | 0.84 |
| PCI* | 34.9 | 34.7 | 0.94 | 36.6 | 25.5 | 0.06 |
| CABG | 6.4 | 5.4 | 0.12 | 6.0 | 5.2 | 0.25 |
| AMI characteristics (%) | ||||||
| Initial | 66.4 | 67.1 | 0.52 | 65.9 | 70.1 | 0.005 |
| Q-wave | 42.8 | 39.2 | 0.006 | 40.3 | 42.8 | 0.13 |
| Anterior | 30.3 | 31.8 | 0.23 | 30.7 | 32.9 | 0.15 |
| STEMI† | 52.6 | 41.7 | <0.001 | 48.4 | 40.5 | 0.001 |
| Acute symptoms (%) | ||||||
| Chest pain | 39.5 | 35.0 | <0.001 | 38.1 | 33.2 | 0.002 |
| Shortness of breath | 28.5 | 24.6 | 0.001 | 27.3 | 22.9 | 0.002 |
| Nausea | 18.4 | 16.9 | 0.13 | 17.9 | 16.6 | 0.27 |
| Diaphoresis | 25.5 | 19.3 | <0.001 | 23.6 | 15.9 | <0.001 |
| Fatigue | 5.3 | 5.5 | 0.80 | 5.2 | 6.1 | 0.21 |
| Weekday hospitalization (%) | 70.6 | 71.5 | 0.19 | 71.2 | 72.4 | 0.40 |
| Time of day hospitalization (%) | ||||||
| 12am-5:59 am | 21.6 | 18.6 | <0.001 | 22.1 | 12.0 | <0.001 |
| 6-11:59 am | 30.6 | 32.2 | 29.8 | 37.9 | ||
| 12 pm-5:59 pm | 25.2 | 28.7 | 25.8 | 31.9 | ||
| 6 pm-11:59 pm | 22.7 | 20.4 | 22.3 | 18.2 | ||
| DNR order‡ (%) | 14.4 | 15.8 | 0.20 | 15.1 | 15.1 | 0.97 |
| Clinical presentations, median | ||||||
| Heart rate, beats/min | 80 | 82 | <0.001 | 80 | 83 | 0.001 |
| Systolic BP, mmHg | 142 | 145 | 0.018 | 144 | 145 | 0.36 |
| Diastolic BP, mmHg | 80 | 80 | 0.89 | 80 | 80 | 0.55 |
| BMI (kg/m2)¶ | 27.1 | 27.0 | 0.31 | 27.1 | 26.8 | 0.59 |
| Laboratory findings, median | ||||||
| Cholesterol (mg/dl) | 198 | 201 | 0.14 | 199 | 203 | 0.08 |
| LDL (mg/dl) | 109 | 112 | 0.18 | 109 | 116 | 0.034 |
| Triglyceride (mg/dl) | 121 | 123 | 0.97 | 120 | 130 | 0.34 |
| Glucose (mg/dl) | 145 | 147 | 0.27 | 147 | 142 | 0.019 |
| Creatinine (mg/dl) | 1.1 | 1.1 | 0.56 | 1.1 | 1.1 | 0.99 |
Data on history of PCI were recorded beginning in 2003 and available for 546 patients.
Data were recorded beginning in 1997 and available for 2,771 patients.
Data were recorded beginning in 1991 and available for 4,384 patients.
Data were recorded beginning in 1995 and available for 2,931 patients.
Pre-hospital Delay in Patients Hospitalized with AMI and Trends over Time
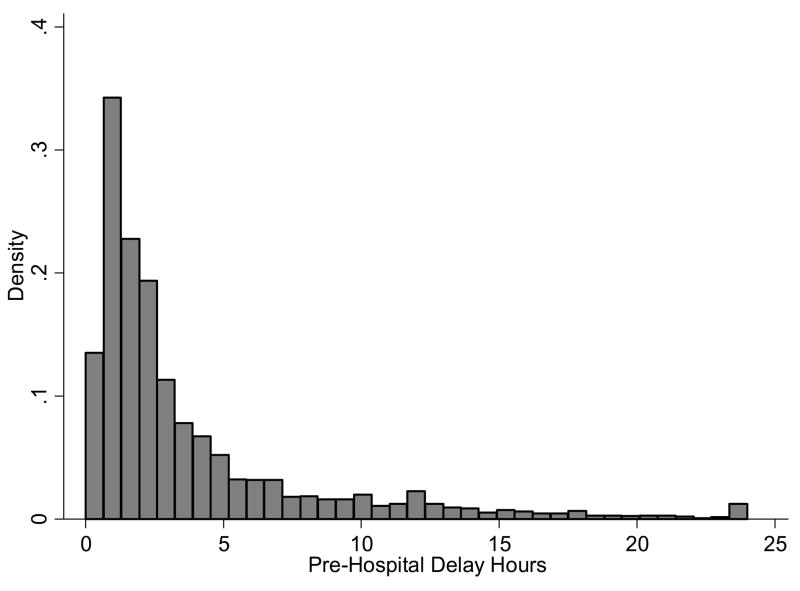
The overall median duration of pre-hospital delay in our total study population was 2 hours (mean: 3.6 hours). The proportions of patients who delayed <1 hour, 1–1.9 hours, 2–3.9 hours, 4–5.9 hours, 6–11.9 hours, and ≥12 hours were 18%, 28%, 25%, 9%, 11%, and 9%, respectively (Figure 1). Women delayed seeking medical care significantly longer than men (Medians: 2.2 hours vs. 2.0 hours, p<0.001). The median durations of pre-hospital delay were 2.0, 2.1, and 2.4 hours in patients <65 years, 65 –74 years, and in those ≥75 years, respectively (p<0.001).
Figure 1.
Distribution of Pre-Hospital Delay in Patients Hospitalized With Acute Myocardial Infarction
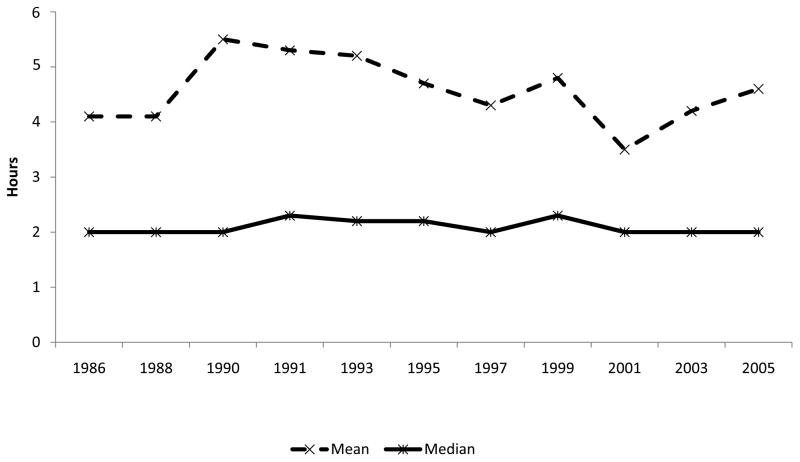
Duration and distribution of pre-hospital delay for patients further stratified according to age and sex are presented in Table 2. Over the 2 decade long period under study, duration of pre-hospital delay in patients hospitalized with AMI was relatively unchanged (Figure 2). Similar patterns in the delay time distributions were observed between 1986 and 2005. For example, the proportion of patients who delayed ≥2 hours and ≥6 hours were 53.6% and 18.4%, respectively, in 1986/1988 (initial 2 study years), and were 52.2% and 17.4%, respectively, in 2003/2005 (2 most recent study years).
Table 2.
Unadjusted Pre-hospital Delay Duration and Distribution according to Age and Sex
| Men | Women | |||||
|---|---|---|---|---|---|---|
| <65y | 65–74y | ≥75y | <65y | 65–74y | ≥75y | |
| Mean (SD), hour | 4.00 (5.8) | 4.65 (8.0) | 5.21 (9.3) | 4.50 (7.6) | 5.00 (7.0) | 4.63(6.4) |
| Median (IQR), hour | 1.92 (1.00–4.17) | 2.00 (1.00–4.65) | 2.25 (1.25–5.18) | 2.00 (1.03–4.67) | 2.43 (1.30–5.50) | 2.28 (1.22–5.10) |
| Distribution (%) | ||||||
| <2 h | 51 | 47 | 39 | 47 | 41 | 41 |
| 2–<6 h | 30 | 32 | 38 | 34 | 36 | 38 |
| ≥6 h | 19 | 21 | 23 | 19 | 23 | 21 |
SD: Standard deviation; IQR: inter quartile range.
Figure 2.
Duration of Pre-Hospital Delay According to Study Year
Pre-hospital Delay in Patients Hospitalized with AMI According to Age and Sex
Delay Time Modeled as a Continuous Outcome
A significant interaction between age and sex in relation to duration of pre-hospital delay was found when pre-hospital delay was examined as a continuous outcome (Table 3). Among patients <65 years, there were no differences in pre-hospital delay between men and women. Among patients 65–74 years, women were more likely to delay seeking medical care compared with men; however, among patients ≥75 years, men were more likely to have delayed seeking medical care compared with women.
Table 3.
Overall Association between Age/Sex and Duration of Pre-hospital delay
| Men | Women | P value† | P value‡ | |||||
|---|---|---|---|---|---|---|---|---|
| < 65 y | 65–75 y | ≥75 y | < 65 y | 65–75 y | ≥75 y | |||
| Difference in Median of Pre-hospital Delay (95% CIs), hours | ||||||||
| Model 1 | 0 (reference) | 0.12 (−0.07; 0.30) | 0.62 (0.43; 0.81) | 0.13 (−0.09; 0.36) | 0.48 (0.27; 0.70) | 0.4 (0.23;0.57) | 0.001 | 0.004 |
| Model 2 | 0 (reference) | 0.12 (−0.13; 0.36) | 0.55 (0.29; 0.82) | 0.14 (−0.16; 0.44) | 0.37 (0.07; 0.66) | 0.37 (0.10;0.65) | 0.10 | 0.18 |
| Model 3 | 0 (reference) | 0.11 (−0.10; 0.32) | 0.61 (0.39; 0.84) | 0.12 (−0.14; 0.37) | 0.37 (0.21; 0.72) | 0.31 (0.08;0.55) | 0.001 | 0.69 |
| Absolute Medians of Pre-hospital Delay (95% CIs), hours | ||||||||
| Model 1 | 1.89 (1.78–1.99) | 2.01 (1.85–2.15) | 2.51 (2.35–2.66) | 2.02 (1.82–2.22) | 2.37 (2.18–2.56) | 2.29 (2.15–2.42) | 0.001 | 0.004 |
| Model 2 | 1.94 (1.79–2.09) | 2.06 (1.86–2.26) | 2.49 (2.29–2.70) | 2.08 (1.82–2.34) | 2.31 (2.06–2.56) | 2.31 (2.11–2.52) | 0.10 | 0.18 |
| Model 3 | 1.96 (1.83–2.09) | 2.07 (1.90–2.24) | 2.57 (2.40–2.75) | 2.08 (1.85–2.30) | 2.33 (2.22–2.63) | 2.27 (2.10–2.45) | 0.001 | 0.69 |
Model 1: Included age, sex, and study year.
Model 2: Further adjusted for race, marital status, and history of angina, diabetes, heart failure, hypertension, stroke, and CABG.
Model 3: Further adjusted for clinical presentation including day of week admission, time of day, chest pain, AMI order (intial vs. prior), AMI type (Q wave vs. non-Q wave), and AMI location (anterior vs. inferior/posterior).
Notes: Information on DNR and STEMI was recorded beginning in 1991 and 1997, respectively; therefore, they were not included as controlling variables in regression model #3.
p values for interaction between age and sex
p values for interaction among age, sex, and study year
Overall, compared with men <65 years, other groups, with the exception of women <65 years, delayed seeking medical care significantly longer in all 3 regression models (Table 2, model 3). Compared with men <65 years, duration of pre-hospital delay increased by 0.11 and by 0.61 hours for men 65 –74 years and men ≥75 years, and by 0.12, 0.37, and 0.31 hours for women <65 years, women 65–74 years, and women ≥75 years, respectively (Table 3 model 3). In absolute terms, the adjusted medians of pre-hospital delay were 1.96, 2.07, and 2.57 hours for men <65 years, men 65 –74 years, and men ≥75 years, and 2.08, 2.33, and 2.27 hours for women <65 years, women 65–74 years, and women ≥75 years, respectively (Table 3, model 3).
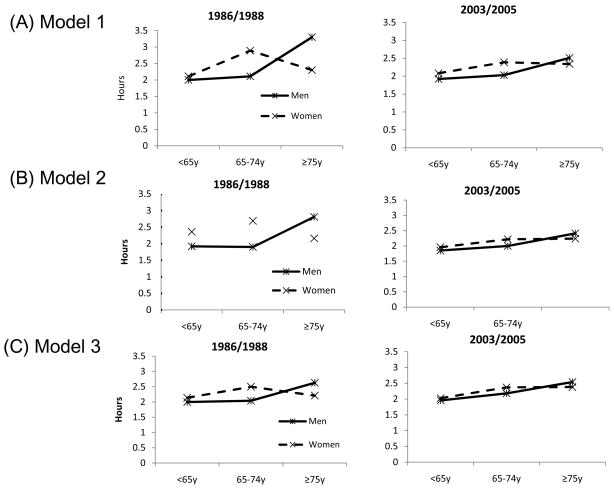
The significant 3- way interactions among age, sex, and study period in model 1 (p=0.004) indicated that the overall age and sex differences in extent of pre-hospital delay have changed over time (Table 3, figure 3A). Adjustment for other variables and comorbidities (particularly a history of diabetes) made the interaction between age, sex, and study period no longer statistically significant (p=0.18), suggesting that more recent trends in the increasing frequency of important comorbidities partially explained the narrowing in age and sex differences over time in extent of pre-hospital delay (Table 3, Figure 3B). Additional adjustment for clinical presentation and AMI associated characteristics further contributed to these narrowing trends (Table 3, Figure 3C).
Figure 3.
Age and Sex Differences in Duration of Pre-Hospital Delay According to Study Year
Alternative median estimates of pre-hospital delay obtained from a propensity-weighted adjustment, which took into account missing data on delay times, are presented in appendix 2 (supplemental document). These estimates were essentially similar to the estimates previously obtained (Table 3). In random intercept models (outcome was log of pre-hospital delay) assessing the effect of different patient clusters within hospitals, we obtained a within hospital correlation of 0.04; the estimated coefficients and standard errors were similar to models without the random effect, suggesting that the effects of cluster data by hospitals were small.
Delay Time Modeled as an Ordinal Outcome
Overall odd ratios for delaying seeking medical care after the onset of symptoms suggestive of AMI, stratified according to age and sex, showed that, compared with men <65 years, men ≥75 years and women ≥65 years were significantly more likely to delay seeking medical care in all 3 regression models (Table 4). The interaction between age and sex was significant in models further adjusted for clinical presentation only (Table 4, model 3); among patients <65 years, there were no differences in pre-hospital delay between men and women. Among patients 65–74 years, women were more likely to delay seeking medical care compared with men; however, among patients ≥75 years, men were more likely to delay seeking acute medical care compared with women.
Table 4.
Overall Odds Ratios (95% CIs) From Ordered Logistic Model for Extent of Delay in Seeking Medical Care According to Age and Sex
| Men | Women | P value† | P value‡ | |||||
|---|---|---|---|---|---|---|---|---|
| < 65 y | 65–75 y | ≥75 y | < 65 y | 65–75 y | ≥75 y | |||
| Model 1 | 1.00 | 1.14 (0.98–1.32) | 1.51 (1.31–1.75) | 1.15 (0.96–1.37) | 1.43 (1.21–1.70) | 1.43 (1.25–1.64) | 0.06 | 0.12 |
| Model 2 | 1.00 | 1.13 (0.97–1.31) | 1.50 (1.28–1.75) | 1.12 (0.93–1.34) | 1.34 (1.11–1.61) | 1.34 (1.14–1.58) | 0.10 | 0.19 |
| Model 3 | 1.00 | 1.12 (0.96–1.32) | 1.55 (1.31–1.84) | 1.11 (0.91–1.35) | 1.34 (1.11–1.62) | 1.28 (1.07–1.53) | 0.013 | 0.56 |
Model 1: Included age, sex, and study year.
Model 2: Further adjusted for race, marital status, and history of angina, diabetes, heart failure, hypertension, stroke, and CABG.
Model 3: Further adjusted for clinical presentation including day of week admission, time of day, chest pain, AMI order (intial vs. prior), AMI type (Q wave vs. non-Q wave), and AMI location (anterior vs. inferior/posterior).
Notes: Information on DNR and STEMI was recorded beginning in 1991 and 1997, respectively; therefore, these variables were not included in regression model #3
p values for interaction between age and sex
p values for interaction among age, sex, and study year
Subgroup analyses in patients with STEMI (n=1,299)
In the subgroup of patients with STEMI (n=1,299), there was a non- significant 3 way interaction among age, sex, study year, and extent of pre-hospital delay (p=0.88). Furthermore, there was no evidence of any interaction between age and sex in relation to extent of pre-hospital delay (p=0.24)
In absolute terms, the adjusted medians of pre-hospital delay were 1.73, 1.76, and 1.89 hours for men <65 years, 65–74 years, and ≥75 years, and 1.66, 2.20, and 2.07 hours for women <65 years, 65–74 years, and for those ≥ 75 years, respectively.
Discussion
The results of this study in nearly 6,000 residents of a large central New England metropolitan area hospitalized with AMI found that patient’s care seeking behavior after the onset of acute coronary symptoms has been relatively unchanged between 1986 and 2005. In addition, and compared with younger men, other age/sex groups were significantly more likely to have delayed seeking medical care after the onset of symptoms suggestive of AMI, with the exception of women <65 years. Differences in duration of pre-hospital delay (continuous outcome) according to age and sex have narrowed over time and were largely explained by changes in patient’s comorbidities and AMI associated characteristics during the years under study.
Our results are consistent with the findings from previous studies7–9 which have shown that older persons were significantly more likely to delay seeking medical care than younger individuals. Older patients are more likely to have atypical symptoms of AMI compared with younger patients.20–22 Older patients are also more likely to have additional comorbidities present, including diabetes, hypertension, and heart failure,5,23,24 which may make patients misinterpret the symptoms of AMI and delay seeking medical care. Other factors such as limited health care access, denial and embarrassment, and living alone may also have contributed to the longer delays noted in older persons.
Sex differences in extent of delay were found in patients ≥65 years, but not in patients <65 years, which is consistent with the findings from previous studies.15,22 For example, findings from the Northern Sweden MONICA myocardial infarction registry, which included approximately 6,500 patients with a confirmed AMI over the period 1989–2003, demonstrated that among patients <65 years there were no sex differences in duration of pre-hospital delay; on the other hand, among patients 65–74 years, women were more likely to delay seeking medical care than men.22 Since there was no upper age cap in our study, we were able to further stratify older patients into two subgroups, finding that women were more likely to delay seeking medical attention than men among patients 65–74 years old, whereas men 75 years and older were more likely to delay seeking hospital care compared with older women. This may be partially explained by the fact that women <75 years old in the present study had more comorbidities present, and were less likely to have developed a Q wave and/or STEMI, compared with men; on the other hand, in patients 75 years and older this sex profile was reversed. Previous studies have shown that these comorbidities are associated with patient’s care seeking behavior.5,24,25
We also found that age and sex differences in duration of pre-hospital delay have narrowed over time, and were largely explained by changes in patient’s comorbidity profile and AMI associated characteristics. These findings are consistent with the results from a limited number of other studies.9,24 Data from the National Registry of Myocardial Infarction, which included nearly 480,000 patients hospitalized with STEMI, suggested that age and sex differences in pre-hospital delay slightly narrowed between 1995 and 2004.24
Although we found that age and sex differences in pre-hospital delay have narrowed over time, our findings suggest that overall duration of pre-hospital delay has remained relatively constant over time and that approximately one half of patients who presented with AMI to metropolitan Worcester hospitals did so after delaying for at least 2 hours following the onset of symptoms suggestive of AMI; these results are consistent with the findings from prior studies.3–5 In the present study, all age-sex subgroups experienced a relatively long duration of pre-hospital delay (medians >1.9 hours). These results reinforce the need for the development of intervention programs to educate patients about the importance of seeking medical care promptly after the onset of symptoms suggestive of AMI. This is because excessive delay may increase an individual’s risk of sudden cardiac death and may also be associated with delays in the receipt of effective hospital therapies, primarily coronary reperfusion therapy.
Several community intervention trials have been undertaken with the expressed purpose of reducing extent of pre-hospital delay in patients with signs and symptoms of AMI; however, 2 recent trials which employed both broad population approaches and more personalized interventions12,26 failed to reduce extent of pre-hospital delay. These and earlier findings suggest that our understanding of the reasons for care seeking behavior in patients with symptoms suggestive of AMI is inadequate as may be our educational approaches and intervention efforts. The findings from the present study demonstrated that both older men and women were at greatest risk for prolonged delay. Inasmuch, interventions designed to reduce pre-hospital delay might be primarily focused on these high risk groups and address specific issues that may contribute to delay in these individuals.
Further in depth qualitative studies should be carried out in older men and women to identify the reasons why these high risk groups fail to react promptly to their symptoms of acute coronary disease focusing on their levels of cognition, knowledge, and attitudes toward health care. Further studies remain needed to explore the effects of educational attainment, extent of insurance coverage, neighborhood level characteristics, psychosocial variables, and other factors that may serve as either facilitators or obstacles by patients to the more timely seeking of medical care, particularly of those factors that may be amenable to change. Indeed, two recent investigations provide insights into how the lack of health insurance and financial concerns about utilizing health care services may lead to delays in seeking medical care in patients with AMI27 and how patient’s perspectives about the trustworthiness of others to provide care, and functional limitations due to angina, could contribute to longer delay times.28 While unknown, the distribution and/or impact of these factors may differ according to a person’s age and sex and may differentially impact younger versus older individuals as well as men in comparison with women. Knowledge of these factors should assist in the design of future interventions to reduce extent of pre-hospital delay in persons with signs and symptoms suggestive of AMI.
Study Strengths and Limitations
This study has several strengths including its population-based design that captured all validated cases of AMI occurring among residents of the Central Massachusetts area hospitalized at all greater Worcester medical centers over a 20 year period. However, several limitations need to be kept in mind in interpreting the present findings. First, a considerable proportion of patients had data missing on pre-hospital delay and missing data differed by age and sex; therefore, our findings should be interpreted with appropriate caution. However, we used propensity-weight adjusted analysis to take into account missing data and we also examined some simple estimates of median delay times assuming missing patients had 50% higher or lower delay times. The combined estimated delay time (actual + imputed missing) resulted in similar patterns of differences by age and sex. Second, information about pre-hospital delay was abstracted from hospital medical records whose documentation may have varied over time and according to patient’s demographic and/or clinical characteristics. In addition, the majority of the study population was White; therefore, the generalizability of our findings may be limited. We did not have information available on several patient associated characteristics (e.g., socioeconomic status) which may have confounded some of the observed associations, nor did we have information on the reasons why patients delayed seeking medical care and how these contributory factors may have differed according to age and sex. Since patients who died out of the hospital from AMI were not included, our findings may only apply to patients hospitalized with AMI; the direction and magnitude of the associations between age/sex and pre-hospital delay in patients who died before reaching the hospital may be different from those who are hospitalized. Lastly, we did not examine the relation between delay times and various clinical outcomes since it was beyond the scope of the present investigation.
Conclusions and implications
The results of our study suggest that duration of pre-hospital delay has remained relatively unchanged over time, and the elderly are more likely to delay seeking medical attention after the development of symptoms suggestive of AMI compared to younger persons. While public educational campaigns and interventions targeted at older individuals are needed to encourage patients to seek medical care promptly to maximize the benefits of currently available therapies, further research remains needed to identify why all patients, including men and women of different ages, delay seeking medical care in the setting of AMI and the best means to encourage patients to seek medical care in a timely fashion.
Supplementary Material
Acknowledgments
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area.
Funding sources: Provided by the National Institutes of Health (RO1 HL35434).
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. The GUSTO investigators. N Engl J Med. 1993;329:673–682. doi: 10.1056/NEJM199309023291001. [DOI] [PubMed] [Google Scholar]
- 2.Newby LK, Rutsch WR, Califf RM, Simoons ML, Aylward PE, Armstrong PW, Woodlief LH, Lee KL, Topol EJ, Van de Werf F. Time from symptom onset to treatment and outcomes after thrombolytic therapy. GUSTO-1 Investigators. J Am Coll Cardiol. 1996;27:1646–1655. doi: 10.1016/0735-1097(96)00053-8. [DOI] [PubMed] [Google Scholar]
- 3.Bertoni AG, Bonds DE, Lovato J, Goff DC, Brancati FL. Sex disparities in procedure use for acute myocardial infarction in the United States, 1995 to 2001. Am Heart J. 2004;147:1054–1060. doi: 10.1016/j.ahj.2003.11.019. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg RJ, Steg PG, Sadiq I, Granger CB, Jackson EA, Budaj A, Brieger D, Avezum A, Goodman S. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry) Am J Cardiol. 2002;89:791–796. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 5.Sheifer SE, Rathore SS, Gersh BJ, Weinfurt KP, Oetgen WJ, Breall JA, Schulman KA. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation. 2000;102:1651–1656. doi: 10.1161/01.cir.102.14.1651. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg RJ, Gurwitz J, Yarzebski J, Landon J, Gore JM, Alpert JS, Dalen PM, Dalen JE. Patient delay and receipt of thrombolytic therapy among patients with acute myocardial infarction from a community-wide perspective. Am J Cardiol. 1992;70:421–425. doi: 10.1016/0002-9149(92)91183-5. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: the Worcester Heart Attack study. Arch Intern Med. 2000;160:3217–3223. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg RJ, Gurwitz JH, Gore JM. Duration of, and temporal trends (1994–1997) in, prehospital delay in patients with acute myocardial infarction: the second National Registry of Myocardial Infarction. Arch Intern Med. 1999;159:2141–2147. doi: 10.1001/archinte.159.18.2141. [DOI] [PubMed] [Google Scholar]
- 9.McGinn AP, Rosamond WD, Goff DC, Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987–2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 10.Hedges JR, Feldman HA, Bittner V, Goldberg RJ, Zapka J, Osganian SK, Murray DM, Simons-Morton DG, Linares A, Williams J, Luepker RV, Eisenberg MS. Impact of community intervention to reduce patient delay time on use of reperfusion therapy for acute myocardial infarction: rapid early action for coronary treatment (REACT) trial. REACT Study Group. Acad Emerg Med. 2000;7:862–872. doi: 10.1111/j.1553-2712.2000.tb02063.x. [DOI] [PubMed] [Google Scholar]
- 11.Nguyen JT, Berger AK, Duval S, Luepker RV. Gender disparity in cardiac procedures and medication use for acute myocardial infarction. Am Heart J. 2008;155:862–868. doi: 10.1016/j.ahj.2007.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dracup K, McKinley S, Riegel B, Moser DK, Meischke H, Doering LV, Davidson P, Paul SM, Baker H, Pelter M. A randomized clinical trial to reduce patient prehospital delay to treatment in acute coronary syndrome. Circ Cardiovasc Qual Outcomes. 2009;2:524–532. doi: 10.1161/CIRCOUTCOMES.109.852608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Banks AD, Dracup K. Are there gender differences in the reasons why African Americans delay in seeking medical help for symptoms of an acute myocardial infarction? Ethn Dis. 2007;17:221–227. [PubMed] [Google Scholar]
- 14.Meischke H, Larsen MP, Eisenberg MS. Gender differences in reported symptoms for acute myocardial infarction: impact on prehospital delay time interval. Am J Emerg Med. 1998;16:363–366. doi: 10.1016/s0735-6757(98)90128-0. [DOI] [PubMed] [Google Scholar]
- 15.Moser DK, McKinley S, Dracup K, Chung ML. Gender differences in reasons patients delay in seeking treatment for acute myocardial infarction symptoms. Patient Educ Couns. 2005;56:45–54. doi: 10.1016/j.pec.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 16.Banks AD, Dracup K. Factors associated with prolonged prehospital delay of African Americans with acute myocardial infarction. Am J Crit Care. 2006;15:149–157. [PubMed] [Google Scholar]
- 17.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Incidence and case fatality rates of acute myocardial infarction (1975–1984): The Worcester Heart Attack Study. American Heart Journal. 1988;115:761–767. doi: 10.1016/0002-8703(88)90876-9. [DOI] [PubMed] [Google Scholar]
- 18.Goldberg RJ, Gorak EJ, Yarzebski J, Hosmer DW, Jr, Dalen P, Gore JM, Alpert JS, Dalen JE. A communitywide perspective of sex differences and temporal trends in the incidence and survival rates after acute myocardial infarction and out-of-hospital deaths caused by coronary heart disease. Circulation. 1993;87:1947–1953. doi: 10.1161/01.cir.87.6.1947. [DOI] [PubMed] [Google Scholar]
- 19.Tunstall-Pedoe H, Kuulasmaa K, Mahonen M, Tolonen H, Ruokokoski E, Amouyel P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet. 1999;353:1547–1557. doi: 10.1016/s0140-6736(99)04021-0. [DOI] [PubMed] [Google Scholar]
- 20.Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid B, Shoultz DA, Frederick PD, Every N. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;36:2056–2063. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 21.Barakat K, Wilkinson P, Deaner A, Fluck D, Ranjadayalan K, Timmis A. How should age affect management of acute myocardial infarction? A prospective cohort study. Lancet. 1999;353:955–959. doi: 10.1016/S0140-6736(98)07114-1. [DOI] [PubMed] [Google Scholar]
- 22.Isaksson RM, Holmgren L, Lundblad D, Brulin C, Eliasson M. Time trends in symptoms and prehospital delay time in women vs. men with myocardial infarction over a 15-year period. The Northern Sweden MONICA Study. Eur J Cardiovasc Nurs. 2008;7:152–158. doi: 10.1016/j.ejcnurse.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Lovlien M, Schei B, Hole T. Prehospital delay, contributing aspects and responses to symptoms among Norwegian women and men with first time acute myocardial infarction. Eur J Cardiovasc Nurs. 2007;6:308–313. doi: 10.1016/j.ejcnurse.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 24.Ting HH, Bradley EH, Wang Y, Lichtman JH, Nallamothu BK, Sullivan MD, Gersh BJ, Roger VL, Curtis JP, Krumholz HM. Factors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarction. Arch Intern Med. 2008;168:959–968. doi: 10.1001/archinte.168.9.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saczynski JS, Yarzebski J, Lessard D, Spencer FA, Gurwitz JH, Gore JM, Goldberg RJ. Trends in Prehospital Delay in Patients With Acute Myocardial Infarction (from the Worcester Heart Attack Study) Am J Cardiol. 2008;102:1589–1594. doi: 10.1016/j.amjcard.2008.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luepker RV, Raczynski JM, Osganian S, Goldberg RJ, Finnegan JR, Jr, Hedges JR, Goff DC, Jr, Eisenberg MS, Zapka JG, Feldman HA, Labarthe DR, McGovern PG, Cornell CE, Proschan MA, Simons-Morton DG. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: The Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA. 2000;284:60–67. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- 27.Smolderen KG, Spertus JA, Nallamothu BK, Krumholz HM, Tang F, Ross JS, Ting HH, Alexander KP, Rathore SS, Chan PS. Health care insurance, financial concerns in accessing care, and delays to hospital presentation in acute myocardial infarction. JAMA. 2010;303:1392–1400. doi: 10.1001/jama.2010.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sullivan MD, Ciechanowski PS, Russo JE, Soine LA, Jordan-Keith K, Ting HH, Caldwell JH. Understanding why patients delay seeking care for acute coronary syndromes. Circ Cardiovasc Qual Outcomes. 2009;2:148–154. doi: 10.1161/CIRCOUTCOMES.108.825471. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.