Abstract
Background
Coronary heart disease is the leading cause of morbidity and mortality in American men and women. While there have been dramatic changes in the management of patients hospitalized with acute myocardial infarction (AMI) over the past several decades, a considerable proportion of patients with AMI continue to delay seeking medical care in a timely manner. This review provides an overview of the published literature that has examined age and sex differences in extent of pre-hospital delay in patients hospitalized with AMI.
Methods and Results
A systematic review of the literature from 1960 to 2008, including publications that provided data on duration of pre-hospital delay in patients hospitalized with AMI, was conducted. A total of 44 articles (42 studies) were included in the present analysis. The majority of studies showed that, in patients hospitalized with AMI, women and older persons were more likely to arrive at the hospital later than men and younger persons. Several factors associated with duration of pre-hospital delay, including sociodemographic, medical history, clinical, and contextual characteristics differed according to sex.
Conclusions
The elderly and women were more likely to exhibit longer delays in seeking medical care after the development of symptoms suggestive of acute coronary disease compared to other groups. Further research remains needed to more fully understand the reasons for delay in these vulnerable groups.
Keywords: Acute myocardial infarction, pre-hospital delay, age and sex differences, systematic review
Background
Coronary heart disease (CHD) is the leading cause of mortality in American men and women; in 2009, it is estimated that more than one million Americans will experience an acute myocardial infarction (AMI).1 Older individuals and women have been shown to be at greater risk for dying after AMI than respective comparison groups. Persons with an AMI have a sudden death rate four to six times that of the general population and upwards of one half of patients with AMI will die before reaching the hospital with men more likely to die out-of-hospital than women. 1
Coronary reperfusion therapies and thrombolytic medications have been consistently shown to be more effective at reducing mortality and the development of important clinical complications if patients are treated with these interventions as promptly as possible.2–4 However, more than one-half of patients with AMI delay seeking medical care by more than 2 hours, and more than one-quarter of patients with AMI delay seeking care by more than 6 hours.5–8 Although considerable efforts have been made to educate the general public about the symptoms of AMI, and the importance of seeking medical care immediately in the setting of possible acute coronary disease, little change in medical care seeking behavior has occurred over the past several decades.8–10
A number of studies have examined possible age and sex differences in the extent of pre-hospital delay in patients with AMI.7–9,11–22 Several studies have found that women are more likely to experience longer delays compared with men,9,10,12,23–25 while other studies have suggested that there are no sex differences in duration of pre-hospital delay.6,8 In terms of age, most prior studies have found that older individuals are more likely to experience prolonged delay in seeking medical care in the setting of AMI than younger persons.8–10,24 However, several studies have found that there were no age differences in medical care seeking behavior in patients hospitalized with AMI.11,12,25,26
Some studies have suggested that socio-demographic factors, acute symptom profile, associated co-morbidities, psychological, and acute contextual factors are associated with patient’s care seeking behavior;7,8,22 little is known, however, about whether these associations differ according to age or according to sex.
The primary objectives of this review are to summarize the published literature that has examined age and sex differences in duration of pre-hospital delay in patients hospitalized with AMI. This review will also examine whether factors associated with pre-hospital delay differ according to patient’s age and sex and provide recommendations for future research in this important area.
Methods
Data sources
A formal search of the electronic literature through Ovid including Medline, PsycINFO, the CINAHL database, as well as a manual search of relevant journals from 1960 to September, 2008, was performed using the following search terms as key words (chest pain OR myocardial infarction OR heart attack OR unstable angina OR angina pectoris OR acute coronary syndromes OR heart disease) AND (delay OR pre-hospital delay OR treatment seeking OR care seeking OR help seeking OR timely treatment OR treatment delay OR hospital arrival OR emergency medical care OR decisions OR decision making) AND (age differences OR sex differences OR women).
Review papers, expert opinions or discussions, case reports, studies that did not clearly define pre-hospital delay, had sample sizes less than 50 subjects, and those that did not report delay times according to sex or age were excluded. In addition, since we were unable to review non-English publications, they were excluded from the present review.
Definition of pre-hospital delay
Duration of pre-hospital delay was defined as the time interval between the onset of signs and symptoms suggestive of AMI and arrival in the hospital emergency department. Pre-hospital delay was normally reported in minutes, hours, or days.
Data extraction
A data abstraction form was used to extract the following information from published studies: (1) study description: author, study year, study design, study population, study setting/location, definition of AMI, inclusion/exclusion criteria, sample size (by age and sex if available), mean age, sex distribution, and definition of pre-hospital delay, (2) information on distribution of pre-hospital delay by age and/or by sex, (3) possible factors associated with pre-hospital delay including socio-demographic (e.g., race, education, insurance), clinical (e.g., medical history, clinical presentation), and psychosocial (e.g., knowledge, anxiety, coping mechanisms) factors by age and/or by sex and (4) information on whether the study findings were adjusted for possible confounding factors.
Quality assessment and grading
The quality of each study reviewed was assessed using Downs and Black criteria.27 The checklist includes 27 items in 5 categories (reporting, external validity, internal validity-bias, internal validity-confounding, and power). The quality score was the number of items from the checklist addressed in the article under review as a percentage of the total number of items applicable (minimum of 23 and maximum of 27). Studies with a quality score of <50% were excluded from further consideration.
Data analysis
We characterized duration of pre-hospital delay by mean, median, and distribution, with further stratification according to patient’s age and sex. Given the heterogeneity of studies included, no formal meta-analytic techniques were performed.
The authors had full access to the data and take responsibility for its integrity. All authors have read and agreed to the manuscript as written.
Results
Search
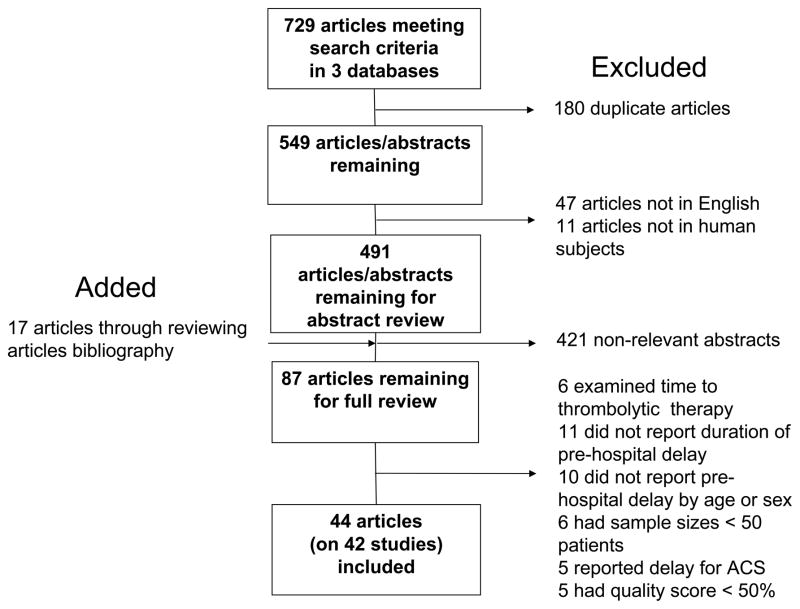
The initial search identified 729 articles/abstracts from Medline, PsyINFO, and the CINHL databases (Figure 1). We initially excluded 180 duplicate articles, 47 non-English studies, and 11 non-human subject studies. Abstracts from 491 studies were reviewed; 421 abstracts determined not to be relevant were excluded. An additional 17 potential studies were identified from the review of bibliographies of published studies. A total of 87 full articles were reviewed and 43 of these were excluded based on previously described criteria, resulting in full abstraction of 44 articles representing 42 independent studies (Figure 1).
Figure 1.
Flow Chart of Review Process
Characteristics of Included Studies
The characteristics of studies included5,7–26,28–50 in this review are shown in Table 1. All studies were conducted after 1985. There was significant heterogeneity between these investigations in terms of study design, population demographic and clinical characteristics, inclusion criteria, and sample sizes. A majority of the studies (54%) were prospective cohort investigations, 29% were cross-sectional in nature, 12% were retrospective cohort studies, and a limited number (5%) were randomized clinical trials.
Table 1.
Characteristics of Included Studies
| First Author | Study period | Study Design | Study location/Setting | Sample Size | Male (%) | Age (mean, yrs) | Sources of pre- hospital delay |
|---|---|---|---|---|---|---|---|
| Karlson et al28 | 1986–1987 | Prospective | Goteborg, Sweden, 1 local hospital | 912 | 76 | NA | Medical record |
| Meischke et al29 | 1988–1991 | Prospective | Washington State, 19 hospitals | 2,947 | 66 | 66 | Medical record |
| Goldberg et al8 | 1986–1997 | Prospective | Worcester, MA, 16 area hospitals | 3,837 | 61 | NA | Medical record |
| Leizorovicz et al30 | 1988–1992 | RCT | 15 European countries and Canada | 5,469 | 77 | 61 | Medical record |
| McGinn et al10 | 1987–2000 | Retrospective | ARIC, U.S., 31 hospitals | 18,928 | 67 | NA | Medical record |
| Barakat et al31 | 1988–1994 | Prospective | England, 1 district hospital | 1,225 | 76 | NA | Medical record |
| Magid et al32 | 1989–1994 | Retrospective | MITI, Washington, 19 hospitals, | 1,331 | 66 | NA | Medical record |
| Isaksson et al19 | 1989–2003 | Prospective | MONICA, Sweden, 2 counties | 6,542 | 78 | NA | Medical record |
| Ottesen et al33 | 1990–1992 | Prospective | TRACE, Denmark, 27 hospitals | 5978 | 68 | NA | Medical record |
| Gibler et al*16 | 1990–1993 | RCT | GUSTO I - U.S., Multiple sites | 23,105 | 73 | 61 | Medical record |
| Maynard et al34 | 1990–1994 | Prospective | NRMI- U.S., 904 hospitals | 212,990 | 65 | 65 | Medical record |
| Meischke et al23 | 1991–1993 | Prospective | Washington State, 19 hospitals | 4,497 | 66 | 67 | Medical record |
| Behar et al13 | 1992 | Cross sectional | Israel, 25 CCUs | 1,014 | 76 | NA | Medical record |
| Gurwitz et al18 | 1992–1993 | Retrospective | Minnesota, 37 hospitals | 2,409 | 62 | NA | Medical record |
| Kaplan et al35 | 1993–1994 | Retrospective | Rochester, NY, 4 hospitals | 573 | 67 | NA | Medical record |
| Lambrew et al36 | 1993–1994 | Prospective | NRMI-1- San Francisco, CA, 42 hospitals | 1,755 | 72 | NA | Medical record |
| Bouma et al14 | 1993–1995 | Prospective | Netherlands, 3 hospitals | 400 | 78 | NA | Interview |
| Sheifer et al5 | 1994–1996 | Prospective | U.S. Medicare | 102,339 | 54 | 76 | Medical record |
| Goldberg et al9 | 1994–1997 | Prospective | NRMI 2-1624 hospitals | 364,131 | 67 | 66 | Medical record |
| Heer et al37 | 1994–1997 | Prospective | Southwest Germany, 54 hospitals | 6,066 | 66 | NA | Medical record |
| Brophy et al38 | 1995–1996 | Prospective | Quebec, Canada, 40 hospitals | 1,357 | 74 | 60 | Questionnaire |
| Gibler et al*16 | 1995–1997 | RCT | GUSTO III U.S., Multiples sites | 4,744 | 70 | 62 | Medical record |
| Ting et al39 | 1995–2004 | Prospective | NRMI 2 U.S. | 482,327 | 67 | NA | Medical record |
| Sawaya et al24 | 1996 | Prospective | Lebanon,18 medical centers | 432 | 77 | NA | Medical record |
| Lovlien et al20 | 1999 | Cross sectional | Norway,13 hospitals | 82 | 54 | NA | Questionnaire |
| Goldberg et al ||7 | 1999–2001 | Prospective | GRACE,14 countries, 94 hospitals | 3,693 | 72 | NA | Medical record |
| Walsh et al40 | 2000 | Cross sectional | Galway, Ireland, 1 university hospital | 61 | 72 | 62 | Interview |
| Carrabba et al41 | 2000–2001 | Prospective | Florence, Italy, 6 hospitals | 920 | 68 | NA | Medical record |
| Morgan et al42 | 2001–2002 | Cross sectional | Northeast U.S., 2 rural hospitals | 98 | 63 | NA | Interview |
| O’Donnell et al43 | 2001–2002 | Prospective | Dublin, Ireland, 6 hospitals | 890 | 69 | NA | Medical record |
| Al-Hassan et al44 | 2002 | Cross sectional | Northern Jordan, 3 district hospitals | 83 | 69 | 52 | Interview |
| Pitsovos et al †45 | 2003–2004 | Prospective | Athens, Lamia, Kardista, Halkida, Kalamata, Zakynthos, Greece, 6 hospitals | 2,172 | 76 | NA | Medical record |
| Lovlien et al21,22 | 2003–2004 | Prospective | Norway, 5 hospitals | 533 | 72 | NA | Questionnaire |
| Bleeker et al46 | NA | Retrospective | Rotterdam, Netherlands, 3 hospitals | 300 | 79 | NA | Interview |
| Dracup et al15 | NA | Cross sectional | North America, 43 hospitals | 277 | 72 | 58 | Questionnaire |
| McKinley et al*26 | NA | Prospective | GUSTO, Australia, 2 hospitals | 145 | 66 | 62 | Interview |
| McKinley et al*26 | NA | Prospective | GUSTO, U.S., Canada, 41 hospitals | 277 | 71 | 58 | Interview |
| Grace et al17 | NA | Cross sectional | Ontario, Canada, 12 CCUs | 482 | 72 | 62 | Questionnaire, Medical record |
| Rosenfeld et al47 | NA | Cross sectional | Pacific Northwest, 3 tertiary hospitals | 52 | 0 | NA | Interview |
| Moser et al25 | NA | Cross sectional | Midwest, 2 hospitals/medical centers | 194 | 51 | NA | Interview |
| Quinn et al48 | NA | Cross sectional | Rochester, NY, 1 hospital | 100 | 59 | 63 | Medical record |
| King et al49 | NA | Cross sectional | Rochester, NY, 1 medical center | 60 | 50 | NA | Interview |
| Zerwic et al50 | NA | Cross sectional | Midwestern state, 3 hospitals | 212 | 53 | NA | Interview |
RCT: Randomized Clinical Trial; NA: Not available
GRACE study included AMI and Unstable Angina (UA). Data presented in Table 1 were for ST-segment elevation myocardial infarction only, data for ST-segment elevation myocardial infarction were not presented since they could not be separated from unstable angina
The GREESC study included AMI and UA. Data presented in Table 1 were for all patients since no information about sample size, sex distribution, and mean age specific for AMI and UA was available. However, information about pre-hospital delay was available for each group presented in Table 2.
These studies included two populations, data were extracted separately.
In terms of the patient populations, most of the studies (90%) included all cases of AMI, regardless of a history of MI (the prevalence of prior MI ranged from 7% to 33%), whereas the remaining investigations focused on patients with a first AMI only. A majority (88%) of the studies were conducted in the U.S., Canada or Europe, with one multi-national registry of patients with acute coronary syndromes. The sample sizes of the published studies ranged widely from 51 to upwards of 480,000 participants. The average age of the patient populations ranged from 52 to 76 years and women accounted for between 20% and 50% of study participants. Women were considerably older than men in the majority of the studies reviewed.
In terms of the measurement of pre-hospital delay, the majority of investigations defined pre-hospital delay as the time interval from the onset of symptoms suggestive of AMI to arrival at the hospital or emergency department (ED). While some studies specifically examined patient associated delay (time from onset of acute symptoms to seeking medical help, such as calling 911), some also included physician related delay (time between the call for assistance and call for an ambulance by the doctor) or transportation delay (period between initiation of travel to the emergency room and ED arrival). Information about duration of pre-hospital delay was abstracted from hospital medical records in 27 studies and was obtained from in-person interviews or self reported questionnaires in 15 studies. Most interviews were conducted between 3–5 days after hospitalization for AMI. Duration of pre-hospital delay was slightly longer in studies in which patients were interviewed11,12,40 than in studies using data from hospital medical records.36,38
Sex Differences in Pre-hospital Delay
In general, the median duration of pre-hospital delay in women ranged from 1.8 hours to 7.2 hours while the range in men was from 1.4 to 3.5 hours (Table 2). A total of 24 studies (median sample size=3,700 patients) found that women were more likely to experience longer delays than men (Tables 2, 3 and 4).9,14,23,28–30,32,33,36–41,43 In these studies, the median differences in duration of pre-hospital delay between women and men ranged from 0.3 to 3.7 hours. Fourteen studies, with a median sample size of 280 patients, found no differences between men and women in terms of pre-hospital delay (Tables 2, 3 and 4).11,17,20–22,35,49 In these studies, the median differences between women and men ranged from 0.02 to 0.9 hours.
Table 2.
Summary of Selected Studies Reporting Duration of Pre-hospital Delay According to Age and Sex
| First Author | Mean Delay (hours) | Median Delay (hours) | Adjusted confounders | Conclusions | ||||
|---|---|---|---|---|---|---|---|---|
| Men (M) | Women (W) | Age groups | Men (M) | Women (W) | Age groups | |||
| Ting et al39 | 1.9 | 2.4 | <60y: 1.8 60–69y: 2.0 70–79y: 2.3 ≥80y: 2.6 |
NA | NA | NA | Yes | Women increased delay (↑) Older patients >60 y ↑ Age and sex differences slightly narrowed over time |
| Maynard et al34 | NA | NA | NA | NA | NA | <60y: 1.8 >75y: 2.5 |
No | Women ↑ least apparent in patients <60y Older patients >75y↑ |
| Heer et al37 | NA | NA | NA | 2.5 | 3.3 | NA | Yes | Women↑ |
| Ottesen et al33 | NA | NA | NA | 3 | 3.8 | NA | No | Women↑ |
| Leizorovicz et al30 | NA | NA | NA | 1.2* | 1.5* | <65y: 1.1 >65y: 1.4 |
Yes | Women↑ Older patients >65y↑ |
| Lambrew et al36 | 2.5±0.1 | 3.1±0.2 | NA | 1.4 | 1.9 | NA | No | Women ↑ |
| Brophy et al38 | NA | NA | NA | 1.5 | 2.0 | ≤65y: 1.4 <65y: 2.0 |
No | Women↑ |
| Magid et al32 | NA | NA | NA | 2.2 | 2.5 | <65y: 2.0 ≥65y: 2.5 |
Age only | Women ↑ Older patients >65y↑ |
| Carrabba et al41 | NA | NA | NA | 2.2 | 2.8 | NA | No | Women ↑ |
| Karlson et al28 | NA | NA | NA | 2.8 | 3.8 | NA | No | Women ↑ |
| O’Donnell et al43 | NA | NA | NA | 1.8 | 3.1 | <65: 1.7 ≥65: 2.5 |
Yes | Women ↑ Older patients ↑ |
| Bouma et al14 | NA | NA | NA | 1.92 | 2.3 | 35–44y: 2.0 45–54y: 1.9 55–64y: 1.8 65–74y: 2.1 |
Age & sex | Women ↑ |
| Walsh et al40 | NA | NA | NA | 3.4 | 7.2 | NA | Yes | Women ↑ |
| Grace et al17 | NA | NA | NA | 1.5 | 1.8 | NA | No | No age and sex differences |
| Dracup et al15 | 1.9±1.4 | 1.0±1.2 | 29–40y: 1.1 41–60y: 1.8 61–86y: 2.0 |
NA | NA | NA | No | No sex differences Older patients↑ |
| Mckinkey et al26 | 1.9±1.3 | 1.8±1.2 | 29–60y: 1.1 41–60y:1.8 61–86y:2.0 |
NA | NA | NA | No | No sex differences Older patients |
| Mckinkey et al26 | 1.9±1.3 | 2.3±1.5 | 29–60y: 1.7 41–60y: 2.0 61–86y: 2.1 |
NA | NA | NA | No | No age and sex differences |
| Zerwic JJ et al50 | NA | NA | NA | 2 | 2.5 | NA | No | No age and sex differences |
| Moser et al25 | NA | NA | NA | 3.1 | 3.1 | ≤55y: M:2.1; W:1.4 >56y: M:2.8; W:3.7 |
Yes | No age and sex differences Age and sex interaction |
| Bank et al11,12 | NA | NA | <55y: 13.9 >55y: 13.3 |
3.5 | 4.4 | <55y: 4.1 >55y: 4.1 |
No | No age and sex differences |
| Morgan et al42 | NA | NA | NA | 1.6 | 1.8 | NA | No | NA |
| Rosenfeld et al47 | NA | NA | NA | NA | 4.3 | NA | No | NA |
NA: Not available;
duration of patient delay
Table 3.
Summary Of Selected Studies Reporting Distributions of Pre-hospital Delay According to Age and Sex
| First Author | Men vs Women | Age Groups (%) | Adjusted confounders | Conclusions | |
|---|---|---|---|---|---|
| Behar et al13 | <6 hours (h): 62% vs 47% | NA | No | Women had increased delay (↑) | |
| Sawaya et al24 | ≤3 h: 41.4% vs 27.3 % 3–6h: 9.6% vs 11.1% 6–12h: 8.1% vs 8.1 % >12h: 34.5% vs 48.5% |
NA | No | Women ↑ | |
| Isaksson et al19 | Age< 65 years (y) <2h: 41.2% vs 41.1% <4h: 20.2% vs 19.8% 4–24h: 27.7% vs 29.2% >24h: 10.9% vs 9.8% |
Age≥65years 41.1% vs 40.2% 21.2% vs 20.2% 25.4% vs 27.1% 12.3% vs 12.5% |
NA | No | Age<65y: no sex differences Age ≥ 65y: women ↑; Sex differences did not narrow over time |
| Kaplan et al35 | <6h: 82% vs 80% | <6h: <65y: 81% >65y: 59% |
No | No sex differences Age differences: marginally significant |
|
| Lovlien et al21,22 | ≤1h: 23% vs 20% 1–2h: 26% vs 27% 2–6h: 25% vs 30% >6h: 26% vs 22% |
NA | No | No sex differences | |
| Grace et al17 | Delayed*: 84.4% vs 77.8% | NA | No | No sex differences | |
| Lovlien et al20 | Patient delay ≥2h: 36% vs 34% Health care delay:≥1h: 50% vs 50% |
Health care delay: patients≤50 y <1h: 62%; >1h:37% |
No | No sex differences | |
| Bank et al11 | Delayed*: 46% vs 54% | NA | No | No sex differences | |
| King et al49 | <1h: 26.7% vs 26.7% | <1h: mean age: 66.1y >1h: mean age: 61.2y |
No | No age or sex differences | |
| Ting et al39 | ≥12 h: 7.8% vs 10.5% | ≥12 h: <60y: 71% 60–69y: 8.3% 70–79y: 10.1% >79y: 12.0% |
NA | NA | |
NA: Not available;
no definition of being delayed was reported
Table 4.
Summary of Studies Reporting Distribution of Age and Sex According to Different Pre-hospital Delay Cutoffs
| First Author | <2 h | ≥2h | 2–4 h | <4h | >4h | 2–6 h | <6h | ≥6h | ORs (95%CI) | Adjusted confounders | Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gibler et al16 | Yes | Older patients | |||||||||
| Age, means, y | 60 | 63 | 63 | ≤40 y: 0.82(0.73–0.93) >40 y: 0.92(0.81–1.04) For 10 year ↑ of age |
increased delay (↑) Women↑ |
||||||
| Men (%) | 75 | 69 | 68 | W vs M: 1.08(1.05–1.11) | |||||||
| Goldberg et al7|| | Yes | Older patients ≥65↑ | |||||||||
| Age group(%) | Women↑ | ||||||||||
| <55y | 33 | 26 | 25 | 1.00 | |||||||
| 55–64y | 24 | 21 | 20 | NA | |||||||
| 65–74y | 26 | 26 | 30 | 1.35(1.09–1.66) | |||||||
| ≥75y | 17 | 27 | 25 | 2.16(1.69–2.77) | |||||||
| Men (%) | 6 | 71 | 67 | M vs W: 0.79 (0.65–0.98) | |||||||
| McGinn et al10 | Yes | Older patients ≥65↑ | |||||||||
| Age group (%) | Women↑ | ||||||||||
| ≤65y | 48 | 52 | 1.00 | Sex differences | |||||||
| >65y | 52 | 48 | 1.22(1.11–1.33) | narrowed over time | |||||||
| Men (%) | 53 | 47 | W vs M: 1.23(1.12–1.36) | ||||||||
| Ottensen et al33 | >2h: 1.02(1.01–1.58) | Yes | Older patients ↑ | ||||||||
| Age group (%) | >6h: 1.01(1.00–1.02) | Women↑ | |||||||||
| <45y | 5 | 4 | 3 | For 1 year ↑ of age | |||||||
| 45–55y | 15 | 11 | 11 | ||||||||
| 55–65y | 26 | 22 | 22 | ||||||||
| 65–75y | 31 | 34 | 33 | ||||||||
| >75y | 23 | 29 | 31 | ||||||||
| Male (%) | 73 | 67 | 64 | M vs W >2h: 0.81 (0.70–0.93) M vs W >6h:0.85 (0.74–0.98) |
|||||||
| Maynard et al34* | Arrival 1h Women↑ Older age†: 0.86(0.83–0.88) M vs W: 1.26 (1.21–1.31) |
Yes | Older patients↑ Women↑ |
||||||||
| Dracup et al15* | Arrival ≤ 1h: ≥60y: 1.00 <60y: 2.87 |
Yes | Older patients ↑ | ||||||||
| Sheifer et al5 | Yes | Older patients↑ | |||||||||
| Age, means, y | 75.4 | 76.0 | 1.01(1.00–1.01) For 5 year ↑ of age |
Female, Blacks, diabetes interacted | |||||||
| Male (%) | 55 | 51 | NA | ||||||||
| Goldberg et al8 | Yes | Older patients↑ | |||||||||
| Age group (%) | no sex differences | ||||||||||
| <55y | 22 | 16 | 19 | 17 | 1.00 | ||||||
| 55–64y | 22 | 21 | 22 | 20 | ≥h: 1.39(1.11–1.74) ≥6h: 1.08(0.80–1.41) |
||||||
| 65–74y | 29 | 29 | 29 | 30 | ≥2h: 1.49(1.19–1.85) ≥6h: 1.29(0.99–1.69) |
||||||
| ≤75y | 27 | 34 | 30 | 33 | ≥2h: 2.07(1.64–2.61) ≥6h:1.55(1.17–2.05) |
||||||
| Men (%) | 64 | 59 | 67 | 61 | W vs M: >2h: 1.05(0.91–1.21) W vs M: >6h: 0.90(0.76–1.07) |
||||||
| Gurwitz et al18 | Yes | No age differences | |||||||||
| Age group (%) | Women↑ | ||||||||||
| <55y | 21 | 20 | 1.00 | ||||||||
| 55–64y | 21 | 17 | 0.83(0.64–1.09) | ||||||||
| 65–74y | 28 | 26 | 0.95(0.74–1.22) | ||||||||
| 75–84y | 22 | 25 | 1.07(0.83–1.39) | ||||||||
| 85y | 8 | 12 | 1.40(1.00–1.95) | ||||||||
| Men (%) | 65 | 57 | W vs M: 1.24(1.04–1.48) |
GRACE study included AMI and Unstable Angina (UA). Data presented in table 1 were for STEMI only, data for NSTEMI was not presented since they could not be separated from UA
Age code: (1) ≤60y, (2)61–74; (3)≥75;
no distribution of age and sex according to pre-hospital delay 1h was available
In summarizing differences in the distributions of men and women according to cutoffs at 2 hours and 6 hours after the onset of AMI5,7,8,16,18,33, patients arriving at the hospital within 2 hours of symptom onset were more likely to be male (range: 64%–76%) compared to those arriving after 2 hours (range: 59%–69%); similar findings were observed when we used a cutpoint at 6 hours to separate early from late care seekers (range: 55%–73% vs. range 51%–67%).
A limited number of studies have examined changes over time in duration of pre-hospital delay in patients hospitalized with AMI according to sex8–10,19,39. The majority of these studies8,9,19 reported that there were either inconsistent or no changes in delay patterns in general, as well as between women and men. On the other hand, the multi-site ARIC study of nearly 19,000 patients hospitalized with AMI over a 14 year period (1987–2000) reported that, although there were no significant changes in the proportion of patients delaying 4 or more hours after acute symptom onset, there was a narrowing of differences between men and women in duration of pre-hospital delay during the period under study.10 Similar findings of narrowing gaps between men and women were observed in NRMI 2.39
Age Specific Differences in Pre-hospital Delay
In general, the median duration of pre-hospital delay in older patients hospitalized with AMI (≥ 65 years) ranged from 1.4 hours to 2.5 hours while the range in younger patients was between 1.1 hours to 2.0 hours (Table 2). In examining the relation between age and duration of pre-hospital delay, the findings from 24 studies (median sample size: 3,700 patients) suggested that older individuals were more likely to exhibit prolonged delay than younger patients (Tables 2, 3, and 4).5,7–10,15,16,18,26,30–33,38,39,43 On the other hand, nine studies with a median sample size of approximately 280 patients found no age-related differences in extent of pre-hospital delay (Tables 2, 3 and 4).11,12,14,20,26,49 Only one small study (n=79) in Jordan found younger age to be associated with prolonged delay in seeking acute medical care.44
In summarizing differences in the distribution of age according to care seeking cutpoints at 2 hours and 6 hours after the onset of AMI7,8,18,33, patients arriving at the hospital within 2 hours of symptom onset were more likely to be younger than 65 years of age (range: 44%–57%) compared to those arriving after 2 hours (range: 36%–46%); similar findings were observed when we used a cutpoint at 6 hours to separate early from late care seekers (range: 41%–52% vs. range 35%–45%).
Studies examining potentially changing trends in pre-hospital delay in patients with AMI according to age have shown that the previously observed gaps between patients of different age groups have not narrowed over time.8,9,39 Two publications from the Worcester Heart Attack Study, which included nearly 4,000 patients hospitalized with AMI in central New England medical centers between 1986 and 2005, found that patients ≥75 years were more likely to delay seeking medical care than patients <55 years and these differences were relatively unchanged over the 20 year period under study.8,51 On the other hand, data from the NRMI 2 suggest that these gaps have slightly narrowed over time (patients 70 years and older delayed longer than younger patients by an average of 39 minutes in 1995 and by 25 minutes in 2004).39
Interaction Between Age and Sex and Extent of Pre-hospital Delay
The interaction between age and sex is important when examining the impact of these demographic characteristics on patient’s care seeking behavior since sex differences in pre-hospital delay may be modified by age and vice versa. A limited number of studies have suggested that differences in duration of pre-hospital delay were greater between older men and women compared to those who were younger.19,25,34
Factors associated with pre-hospital delay according to sex and age
A variety of socio-demographic (in addition to age and sex), clinical, situational, and psychological factors have been associated with prolonged care seeking behavior. These factors included non-White race,5,9,10,21,22,39 low socioeconomic status,15,26 history of angina,5,8,29,33,39 diabetes,5,8,9,11,12,15,16,23,26,29,33,38,39 and hypertension,8,10,18,26,45 consulting a spouse or other relative,20 consulting a physician,21,22,43,50 self treatment,21,22,50 waiting for symptoms to go away, stuttering symptom pattern,12,25 not viewing symptoms as serious or experiencing anxiety about them,25,40 and lack of knowledge about the symptoms of AMI.12,25 On the other hand, having Medicare or private health insurance,16,23,43 history of MI,5,7,9,23,29,33,39 sudden onset of severe chest pain,10,18,23,26,39 onset of symptoms in the evening,39 calling EMS,10,21,22 presenting with shock,30,39 sweating,23 recognition by patient that symptoms were heart related26,46, and concordance between expected and experienced symptoms21,22,49,50 were associated with shortened delay times. Socio-demographic and clinical factors were typically investigated in large cohort studies in which data were collected through the review of hospital medical records, whereas psychological factors were primarily examined in small studies, where data were gathered through self-reported questionnaires or direct patient interviews.
Among men, low education,22 having a partner with low education,22 having symptom onset at home,12 not asking for help or calling 911,12 not taking the ambulance,12 experiencing early musculoskeletal pain,21 developing a non-Q wave AMI,25 lack of consistency between expected and experienced symptoms50, and not knowing about thrombolytic therapy when having symptoms of AMI25 placed men at greater risk for prolonged pre-hospital delay; a history of a previous MI25 and symptom appraisal21 were associated with reduced pre-hospital delay in men.
Factors associated with delays in seeking medical care in women slightly differed from those noted in men. Women who were older,25 single,12 had a history of a previous MI,25 were alone during symptom onset,12 and did not want to trouble anyone12,25 were more likely to seek medical care at a later time than women who did not have these characteristics; women who were transported to the hospital by ambulance were more likely to arrive at the hospital earlier than those who were transported by other methods.36
Among studies included in the present review, we could not identify any study that examined whether factors associated with pre-hospital delay differed in persons of different age groups.
Discussion
Overall, the findings of the studies reviewed were somewhat mixed with regards to possible age and sex differences in duration of pre-hospital delay in patients hospitalized with AMI. A significant number of studies found that women were more likely to present at the hospital later than men, and older persons were more likely to experience longer delays than younger persons; these associations were particularly noted in studies that were broader in scale and that adjusted for the role of other potentially confounding variables. There were some suggestions for an interaction between age and sex with regards to extent of pre-hospital delay, in which differences in pre-hospital delay between men and women were less pronounced in younger as compared to older individuals. Several factors were differentially associated with care seeking behavior between men and women.
Sex Differences in Duration of Pre-hospital Delay
The majority of studies reviewed found that women were more likely to delay seeking medical care than men, even after adjustment for the important potentially confounding influence of age and other comorbidities. There are several possible explanations for this finding. First, women were considerably older than men when experiencing their first AMI12,13,17,21,25,35,36,41,43,49,50 and many studies have found that advancing age is associated with prolonged delay in seeking medical care in patients hospitalized with AMI.8,9,15,30,38,39,43 Second, women were more likely to report atypical symptoms of AMI than men.52 Women may lack knowledge about the symptoms of AMI or consider heart attack as a “male disease”; therefore, they may not recognize the importance of their symptoms in seeking medical care in a timely fashion. Women were more likely to contact their physician initially than men which likely contributed to the more prolonged delay patterns observed.50 Women were also more likely to be widowed and living alone at the time of symptom onset21 and living alone has been previously shown to be an independent predictor of prolonged delay.12,18 Women were more likely to have additional comorbidities present than men, including diabetes, hypertension, and heart failure,21,35 and these conditions have been associated with prolonged delay times.5,7,8,18,39 Women also tended to cope with their illness by themselves and these coping mechanisms have been previously associated with longer delay times.12,25 Interventional strategies specifically targeting women may be needed to improve their understanding about the nature of this disease, differences in symptom patterns between women and men, and the need for seeking medical care promptly after developing symptoms suggestive of AMI.
Age Differences in Duration of Pre-hospital Delay
Older individuals were more likely to experience greater delays in seeking acute medical care than younger individuals in the setting of AMI. Several factors may have contributed to this observation. Older patients are more likely to have atypical symptoms of AMI,31,53 and have additional comorbidities present compared to younger patients,6–8,19,43,31 that may lead to delays in seeking medical care in a timely manner. Other factors such as limited health care access, denial and embarrassment, living alone, or failure to recognize the symptoms associated with AMI in older patients may also have contributed to the longer delays noted in older persons.
Given the markedly increased risk for initial coronary events in older as compared to younger individuals, as well as in the risk of recurrent coronary events in patients with an initial AMI, older persons need to be educated about the symptoms of AMI they may experience and appropriate care seeking steps they should take when experiencing these symptoms. Family members as well as care providers should be encouraged to become involved in these educational programs since they play important roles in the decision making process of older persons.
Interaction between Age and Sex and Duration of Pre-hospital Delay
A limited number of studies have examined the interaction between age and sex with regards to extent of pre-hospital delay showing that sex differences in pre-hospital delay were greater in older compared to younger persons with older women more likely to exhibit greater delay, highlighting the need for targeted interventions in older women.19,25,34
Limitations of Published Studies
The studies we included in this summary overview have several limitations. First, some studies used either convenience11,12,20,40,44,47,49 or restricted patient samples16,20–22,32,39,47 that may have resulted in selection biases or findings with limited generalizability. Several studies had small sample sizes,11,12,20,40,44,47,49 with a consequent lack of statistical power. Many studies relied primarily on information from medical records which may be associated with information bias5,7–9,16–18,30,37,39 and may not have precisely characterized extent of delay in comparison to data collected through in person interviews. Indeed, differences were noted in average delay times based on information collected from medical records as compared to data collected by direct standardized patient interviews. Similarly, studies that relied exclusively on patient interviews15,44,46,49 may have been subject to recall bias, depending on the patient’s cognitive status and time when the interviews were performed. None of the studies reviewed adjusted for cognitive impairment status. Lastly, a number of studies did not report on, or perform, multivariate analyses which may have led to concerns in the interpretation of the study findings.11,12,15,17,28,34,36,38,41
Future Research
Women and older persons, particularly older women, have been shown to delay seeking medical care for AMI to a greater extent compared to respective comparison groups. In addition, factors associated with delay are likely to differ by age and according to sex which needs to be confirmed in well designed future studies. Further qualitative studies (e.g., in-depth interviews or focus groups) are needed to better understand the relation between age and sex with care seeking behavior in patients developing an AMI. Greater understanding of differences in, and reactions to, premonitory, as well as acute, symptoms of coronary disease is needed and of the steps that individuals take in seeking acute medical care. Future studies should report means, medians, and distributions of pre-hospital delay by age and by sex for more meaningful comparisons. Multivariate as well as stratified analyses should also be performed to minimize the effects of other potentially confounding variables.
Interventions to Reduce Extent of Pre-hospital Delay
Several community intervention trials have been undertaken with the goal of reducing extent of pre-hospital delay in patients with signs and symptoms of AMI, with inconsistent results. Some trials, using interventions ranging from mass to specialized media campaigns, have shown significant reductions in either median delay times or increases in the proportion of patients presenting for medical care relatively soon after the onset of acute coronary symptoms.54–57 On the other hand, several studies have failed to observe reductions in delay times in patients experiencing symptoms of AMI.58–65 The results of these trials, especially 2 recent trials which employed both broad population approaches and more personalized interventions,64,65 suggest that our understanding of the reasons for delay in seeking care in patients with symptoms suggestive of AMI may be inadequate as may be our educational approaches and intervention efforts.
Conclusions and Implications for Clinical Practice
Women and older individuals are more likely to delay seeking medical care after the onset of AMI. Factors associated with duration of pre-hospital delay including socio-demographic, medical history, clinical presentation, and psychological variables have been shown to affect medical care seeking behavior; the role of these and additional factors that may affect acute care seeking behavior need to be more systematically examined in future studies. Research remains needed to particularly address delays in seeking medical care after the onset of acute coronary symptoms in vulnerable groups.
Acknowledgments
Funding Sources: Grant support for this project was provided by the National Heart, Lung, and Blood Institute (RO1 HL35434).
Footnotes
Disclosures: There are no conflicts of interest with any of the authors.
References
- 1.Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, Hailpern SM, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O’Donnell C, Roger V, Sorlie P, Steinberger J, Thom T, Wilson M, Hong Y. Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 2.Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Gruppo Italiano per lo Studio della Streptochinasi nell’Infarto Miocardico (GISSI) Lancet. 1986;1:397–402. [PubMed] [Google Scholar]
- 3.An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. The GUSTO investigators. N Engl J Med. 1993;329:673–682. doi: 10.1056/NEJM199309023291001. [DOI] [PubMed] [Google Scholar]
- 4.Newby LK, Rutsch WR, Califf RM, Simoons ML, Aylward PE, Armstrong PW, Woodlief LH, Lee KL, Topol EJ, Van de Werf F. Time from symptom onset to treatment and outcomes after thrombolytic therapy. GUSTO-1 Investigators. J Am Coll Cardiol. 1996;27:1646–1655. doi: 10.1016/0735-1097(96)00053-8. [DOI] [PubMed] [Google Scholar]
- 5.Sheifer SE, Rathore SS, Gersh BJ, Weinfurt KP, Oetgen WJ, Breall JA, Schulman KA. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation. 2000;102:1651–1656. doi: 10.1161/01.cir.102.14.1651. [DOI] [PubMed] [Google Scholar]
- 6.Goff DC, Jr, Feldman HA, McGovern PG, Goldberg RJ, Simons-Morton DG, Cornell CE, Osganian SK, Cooper LS, Hedges JR. Prehospital delay in patients hospitalized with heart attack symptoms in the United States: the REACT trial. Rapid Early Action for Coronary Treatment (REACT) Study Group. Am Heart J. 1999;138:1046–1057. doi: 10.1016/s0002-8703(99)70069-4. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg RJ, Steg PG, Sadiq I, Granger CB, Jackson EA, Budaj A, Brieger D, Avezum A, Goodman S. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry) Am J Cardiol. 2002;89:791–796. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: the Worcester Heart Attack study. Arch Intern Med. 2000;160:3217–3223. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 9.Goldberg RJ, Gurwitz JH, Gore JM. Duration of, and temporal trends (1994–1997) in, prehospital delay in patients with acute myocardial infarction: the second National Registry of Myocardial Infarction. Arch Intern Med. 1999;159:2141–2147. doi: 10.1001/archinte.159.18.2141. [DOI] [PubMed] [Google Scholar]
- 10.McGinn AP, Rosamond WD, Goff DC, Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987–2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 11.Banks AD, Dracup K. Factors associated with prolonged prehospital delay of African Americans with acute myocardial infarction. Am J Crit Care. 2006;15:149–157. [PubMed] [Google Scholar]
- 12.Banks AD, Dracup K. Are there gender differences in the reasons why African Americans delay in seeking medical help for symptoms of an acute myocardial infarction? Ethn Dis. 2007;17:221–227. [PubMed] [Google Scholar]
- 13.Behar S, Gottlieb S, Hod H, Narinsky R, Benari B, Rechavia E, Pauzner H, Rougin N, Kracoff OH, Katz A. Influence of gender in the therapeutic management of patients with acute myocardial infarction in Israel. The Israeli Thrombolytic Survey Group. Am J Cardiol. 1994;73:438–443. doi: 10.1016/0002-9149(94)90672-6. [DOI] [PubMed] [Google Scholar]
- 14.Bouma J, Broer J, Bleeker J, van Sonderen E, Meyboom-de Jong B, DeJongste MJ. Longer pre-hospital delay in acute myocardial infarction in women because of longer doctor decision time. J Epidemiol Community Health. 1999;53:459–464. doi: 10.1136/jech.53.8.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dracup K, Moser DK. Beyond sociodemographics: factors influencing the decision to seek treatment for symptoms of acute myocardial infarction. Heart Lung. 1997;26:253–262. doi: 10.1016/s0147-9563(97)90082-0. [DOI] [PubMed] [Google Scholar]
- 16.Gibler WB, Armstrong PW, Ohman EM, Weaver WD, Stebbins AL, Gore JM, Newby LK, Califf RM, Topol EJ. Persistence of delays in presentation and treatment for patients with acute myocardial infarction: The GUSTO-I and GUSTO-III experience. Ann Emerg Med. 2002;39:123–130. doi: 10.1067/mem.2002.121402. [DOI] [PubMed] [Google Scholar]
- 17.Grace SL, Abbey SE, Bisaillon S, Shnek ZM, Irvine J, Stewart DE. Presentation, delay, and contraindication to thrombolytic treatment in females and males with myocardial infarction. Womens Health Issues. 2003;13:214–221. doi: 10.1016/j.whi.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 18.Gurwitz JH, McLaughlin TJ, Willison DJ, Guadagnoli E, Hauptman PJ, Gao X, Soumerai SB. Delayed hospital presentation in patients who have had acute myocardial infarction. Ann Intern Med. 1997;126:593–599. doi: 10.7326/0003-4819-126-8-199704150-00001. [DOI] [PubMed] [Google Scholar]
- 19.Isaksson RM, Holmgren L, Lundblad D, Brulin C, Eliasson M. Time trends in symptoms and prehospital delay time in women vs. men with myocardial infarction over a 15-year period. The Northern Sweden MONICA Study. Eur J Cardiovasc Nurs. 2008;7:152–158. doi: 10.1016/j.ejcnurse.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 20.Lovlien M, Schei B, Gjengedal E. Are there gender differences related to symptoms of acute myocardial infarction? A Norwegian perspective. Prog Cardiovasc Nurs. 2006;21:14–19. doi: 10.1111/j.0197-3118.2006.04656.x. [DOI] [PubMed] [Google Scholar]
- 21.Lovlien M, Schei B, Hole T. Prehospital delay, contributing aspects and responses to symptoms among Norwegian women and men with first time acute myocardial infarction. Eur J Cardiovasc Nurs. 2007;6:308–313. doi: 10.1016/j.ejcnurse.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 22.Lovlien M, Schei B, Hole T. Myocardial infarction: psychosocial aspects, gender differences and impact on pre-hospital delay. J Adv Nurs. 2008;63:148–154. doi: 10.1111/j.1365-2648.2008.04654.x. [DOI] [PubMed] [Google Scholar]
- 23.Meischke H, Larsen MP, Eisenberg MS. Gender differences in reported symptoms for acute myocardial infarction: impact on prehospital delay time interval. Am J Emerg Med. 1998;16:363–366. doi: 10.1016/s0735-6757(98)90128-0. [DOI] [PubMed] [Google Scholar]
- 24.Sawaya JI, Jazra C, Eid EV, Sabra RF. Gender differences in the diagnosis and treatment of acute myocardial infarction in Lebanon. J Med Liban. 1999;47:2–6. [PubMed] [Google Scholar]
- 25.Moser DK, McKinley S, Dracup K, Chung ML. Gender differences in reasons patients delay in seeking treatment for acute myocardial infarction symptoms. Patient Educ Couns. 2005;56:45–54. doi: 10.1016/j.pec.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 26.McKinley S, Moser DK, Dracup K. Treatment-seeking behavior for acute myocardial infarction symptoms in North America and Australia. Heart Lung. 2000;29:237–247. doi: 10.1067/mhl.2000.106940. [DOI] [PubMed] [Google Scholar]
- 27.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karlson BW, Herlitz J, Hartford M. Prognosis in myocardial infarction in relation to gender. Am Heart J. 1994;128:477–483. doi: 10.1016/0002-8703(94)90620-3. [DOI] [PubMed] [Google Scholar]
- 29.Meischke H, Eisenberg MS, Larsen MP. Prehospital delay interval for patients who use emergency medical services: the effect of heart-related medical conditions and demographic variables. Ann Emerg Med. 1993;22:1597–1601. doi: 10.1016/s0196-0644(05)81267-3. [DOI] [PubMed] [Google Scholar]
- 30.Leizorovicz A, Haugh MC, Mercier C, Boissel JP. Pre-hospital and hospital time delays in thrombolytic treatment in patients with suspected acute myocardial infarction. Analysis of data from the EMIP study. European Myocardial Infarction Project. Eur Heart J. 1997;18:248–253. doi: 10.1093/oxfordjournals.eurheartj.a015227. [DOI] [PubMed] [Google Scholar]
- 31.Barakat K, Wilkinson P, Deaner A, Fluck D, Ranjadayalan K, Timmis A. How should age affect management of acute myocardial infarction? A prospective cohort study. Lancet. 1999;353:955–959. doi: 10.1016/S0140-6736(98)07114-1. [DOI] [PubMed] [Google Scholar]
- 32.Magid DJ, Koepsell TD, Every NR, Martin JS, Siscovick DS, Wagner EH, Weaver WD. Absence of association between insurance copayments and delays in seeking emergency care among patients with myocardial infarction. N Engl J Med. 1997;336:1722–1729. doi: 10.1056/NEJM199706123362406. [DOI] [PubMed] [Google Scholar]
- 33.Ottesen MM, Kober L, Jorgensen S, Torp-Pedersen C. Determinants of delay between symptoms and hospital admission in 5978 patients with acute myocardial infarction. The TRACE Study Group. Trandolapril Cardiac Evaluation. Eur Heart J. 1996;17:429–437. doi: 10.1093/oxfordjournals.eurheartj.a014876. [DOI] [PubMed] [Google Scholar]
- 34.Maynard C, Weaver WD, Lambrew C, Bowlby LJ, Rogers WJ, Rubison RM. Factors influencing the time to administration of thrombolytic therapy with recombinant tissue plasminogen activator (data from the National Registry of Myocardial Infarction). Participants in the National Registry of Myocardial Infarction. Am J Cardiol. 1995;76:548–552. doi: 10.1016/s0002-9149(99)80152-0. [DOI] [PubMed] [Google Scholar]
- 35.Kaplan KL, Fitzpatrick P, Cox C, Shammas NW, Marder VJ. Use of thrombolytic therapy for acute myocardial infarction: effects of gender and age on treatment rates. J Thromb Thrombolysis. 2002;13:21–26. doi: 10.1023/a:1015312007648. [DOI] [PubMed] [Google Scholar]
- 36.Lambrew CT, Bowlby LJ, Rogers WJ, Chandra NC, Weaver WD. Factors influencing the time to thrombolysis in acute myocardial infarction. Time to Thrombolysis Substudy of the National Registry of Myocardial Infarction-1. Arch Intern Med. 1997;157:2577–2582. [PubMed] [Google Scholar]
- 37.Heer T, Schiele R, Schneider S, Gitt AK, Wienbergen H, Gottwik M, Gieseler U, Voigtlander T, Hauptmann KE, Wagner S, Senges J. Gender differences in acute myocardial infarction in the era of reperfusion (the MITRA registry) Am J Cardiol. 2002;89:511–517. doi: 10.1016/s0002-9149(01)02289-5. [DOI] [PubMed] [Google Scholar]
- 38.Brophy JM, Diodati JG, Bogaty P, Theroux P. The delay to thrombolysis: an analysis of hospital and patient characteristics. Quebec Acute Coronary Care Working Group. Cmaj. 1998;158:475–480. [PMC free article] [PubMed] [Google Scholar]
- 39.Ting HH, Bradley EH, Wang Y, Lichtman JH, Nallamothu BK, Sullivan MD, Gersh BJ, Roger VL, Curtis JP, Krumholz HM. Factors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarction. Arch Intern Med. 2008;168:959–968. doi: 10.1001/archinte.168.9.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Walsh JC, Lynch M, Murphy AW, Daly K. Factors influencing the decision to seek treatment for symptoms of acute myocardial infarction: an evaluation of the Self-Regulatory Model of illness behaviour. J Psychosom Res. 2004;56:67–73. doi: 10.1016/S0022-3999(03)00082-5. [DOI] [PubMed] [Google Scholar]
- 41.Carrabba N, Santoro GM, Balzi D, Barchielli A, Marchionni N, Fabiani P, Landini C, Scarti L, Santoro G, Valente S, Verdiani V, Buiatti E. In-hospital management and outcome in women with acute myocardial infarction (data from the AMI-Florence Registry) Am J Cardiol. 2004;94:1118–1123. doi: 10.1016/j.amjcard.2004.07.076. [DOI] [PubMed] [Google Scholar]
- 42.Morgan DM. Effect of incongruence of acute myocardial infarction symptoms on the decision to seek treatment in a rural population. J Cardiovasc Nurs. 2005;20:365–371. doi: 10.1097/00005082-200509000-00011. [DOI] [PubMed] [Google Scholar]
- 43.O’Donnell S, Condell S, Begley C, Fitzgerald T. Prehospital care pathway delays: gender and myocardial infarction. J Adv Nurs. 2006;53:268–276. doi: 10.1111/j.1365-2648.2006.03722.x. [DOI] [PubMed] [Google Scholar]
- 44.Al-Hassan MA, Omran SM. The effects of health beliefs on health care-seeking decisions of Jordanian patients with myocardial infarction symptoms. Int J Nurs Pract. 2005;11:13–20. doi: 10.1111/j.1440-172X.2005.00497.x. [DOI] [PubMed] [Google Scholar]
- 45.Pitsavos C, Kourlaba G, Panagiotakos DB, Stefanadis C. Factors associated with delay in seeking health care for hospitalized patients with acute coronary syndromes: the GREECS study. Hellenic J Cardiol. 2006;47:329–336. [PubMed] [Google Scholar]
- 46.Bleeker JK, Lamers LM, Leenders IM, Kruyssen DC, Simoons ML, Trijsburg RW, Erdman RA. Psychological and knowledge factors related to delay of help-seeking by patients with acute myocardial infarction. Psychother Psychosom. 1995;63:151–158. doi: 10.1159/000288952. [DOI] [PubMed] [Google Scholar]
- 47.Rosenfeld AG. Treatment-seeking delay among women with acute myocardial infarction: decision trajectories and their predictors. Nurs Res. 2004;53:225–236. doi: 10.1097/00006199-200407000-00005. [DOI] [PubMed] [Google Scholar]
- 48.Quinn JR. Delay in seeking care for symptoms of acute myocardial infarction: applying a theoretical model. Res Nurs Health. 2005;28:283–294. doi: 10.1002/nur.20086. [DOI] [PubMed] [Google Scholar]
- 49.King KB, McGuire MA. Symptom presentation and time to seek care in women and men with acute myocardial infarction. Heart Lung. 2007;36:235–243. doi: 10.1016/j.hrtlng.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 50.Zerwic JJ, Ryan CJ, DeVon HA, Drell MJ. Treatment seeking for acute myocardial infarction symptoms: differences in delay across sex and race. Nurs Res. 2003;52:159–167. doi: 10.1097/00006199-200305000-00005. [DOI] [PubMed] [Google Scholar]
- 51.Saczynski JS, Yarzebski J, Lessard D, Spencer FA, Gurwitz JH, Gore JM, Goldberg RJ. Trends in Prehospital Delay in Patients With Acute Myocardial Infarction (from the Worcester Heart Attack Study) The American Journal of Cardiology. 2008;102:1589–1594. doi: 10.1016/j.amjcard.2008.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen W, Woods SL, Puntillo KA. Gender differences in symptoms associated with acute myocardial infarction: a review of the research. Heart Lung. 2005;34:240–247. doi: 10.1016/j.hrtlng.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 53.Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, Ornato JP, Barron HV, Kiefe CI. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. Jama. 2000;283:3223–3229. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 54.Herlitz J, Hartford M, Blohm M, Karlson BW, Ekstrom L, Risenfors M, Wennerblom B, Luepker RV, Holmberg S. Effect of a media campaign on delay times and ambulance use in suspected acute myocardial infarction. Am J Cardiol. 1989;64:90–93. doi: 10.1016/0002-9149(89)90659-0. [DOI] [PubMed] [Google Scholar]
- 55.Rowley JM, Hill JD, Hampton JR, Mitchell JR. Early reporting of myocardial infarction: impact of an experiment in patient education. Br Med J (Clin Res Ed) 1982;284:1741–1746. doi: 10.1136/bmj.284.6331.1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mitic WR, Perkins J. The effect of a media campaign on heart attack delay and decision times. Can J Public Health. 1984;75:414–418. [PubMed] [Google Scholar]
- 57.Gaspoz JM, Unger PF, Urban P, Chevrolet JC, Rutishauser W, Lovis C, Goldman L, Heliot C, Sechaud L, Mischler S, Waldvogel FA. Impact of a public campaign on pre-hospital delay in patients reporting chest pain. Heart. 1996;76:150–155. doi: 10.1136/hrt.76.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ho MT, Eisenberg MS, Litwin PE, Schaeffer SM, Damon SK. Delay between onset of chest pain and seeking medical care: the effect of public education. Ann Emerg Med. 1989;18:727–731. doi: 10.1016/s0196-0644(89)80004-6. [DOI] [PubMed] [Google Scholar]
- 59.Meischke H, Eisenberg MS, Schaeffer SM, Larsen MP, Henwood DK. Impact of direct mail intervention on knowledge, attitudes, and behavioral intentions regarding use of emergency medical services for symptoms of acute myocardial infarction. Eval Health Prof. 1994;17:402–417. doi: 10.1177/016327879401700403. [DOI] [PubMed] [Google Scholar]
- 60.Meischke H, Dulberg EM, Schaeffer SS, Henwood DK, Larsen MP, Eisenberg MS. ‘Call fast, Call 911’: a direct mail campaign to reduce patient delay in acute myocardial infarction. Am J Public Health. 1997;87:1705–1709. doi: 10.2105/ajph.87.10.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moses HW, Engelking N, Taylor GJ, Prabhakar C, Vallala M, Colliver JA, Silberman H, Schneider JA. Effect of a two-year public education campaign on reducing response time of patients with symptoms of acute myocardial infarction. Am J Cardiol. 1991;68:249–251. doi: 10.1016/0002-9149(91)90753-8. [DOI] [PubMed] [Google Scholar]
- 62.Bett JH, Tonkin AM, Thompson PL, Aroney CN. Failure of current public educational campaigns to impact on the initial response of patients with possible heart attack. Intern Med J. 2005;35:279–282. doi: 10.1111/j.1445-5994.2004.00798.x. [DOI] [PubMed] [Google Scholar]
- 63.Bett N, Aroney G, Thompson P. Impact of a national educational campaign to reduce patient delay in possible heart attack. Aust N Z J Med. 1993;23:157–161. doi: 10.1111/j.1445-5994.1993.tb01810.x. [DOI] [PubMed] [Google Scholar]
- 64.Luepker RV, Raczynski JM, Osganian S, Goldberg RJ, Finnegan JR, Jr, Hedges JR, Goff DC, Jr, Eisenberg MS, Zapka JG, Feldman HA, Labarthe DR, McGovern PG, Cornell CE, Proschan MA, Simons-Morton DG. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: The Rapid Early Action for Coronary Treatment (REACT) Trial. Jama. 2000;284:60–67. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- 65.Dracup K, McKinley S, Riegel B, Meischke H, Doering LV, Moser DK, Pelter M. A randomized cotrolled trial to reduce prehospital delay to treatment in acute coronary syndrome. Abstract. Circulation. 2007:388. doi: 10.1161/CIRCOUTCOMES.109.852608. [DOI] [PMC free article] [PubMed] [Google Scholar]