Abstract
Purpose
Dense breasts have been suggested as a risk factor for breast cancer, but controversy still remains. This study evaluates the association of reproductive and hormonal factors with dense breasts among Korean women.
Materials and Methods
Using a cross-sectional design, 516 women were recruited and classified for breast density patterns as being either fatty or dense, using the Breast Imaging Reporting and Data System (BI-RADS) of the American College of Radiology. Univariate and multivariate logistic regression models were used for statistical analysis.
Results
In univariate logistic regression, older age, higher body mass index, older age at menarche, and oral contraceptive use were associated with more fatty breasts. On the contrary, longer duration of education, alcohol consumption, lower parity, menopause and use of hormone replacement therapy were associated with dense breasts. After adjustment, age and body mass index were inversely associated with breast density (p-value for trend <0.01, respectively), whereas nulliparous and premenopausal status were positively associated. Compared to women who had ≥2 children, nulliparous women had an 11.8-fold increase of dense breasts (p-value for trend <0.01). Compared to postmenopausal women, premenopausal women had 2.4-fold increase of dense breasts (odds ratio, 2.42; 95% confidence interval, 1.36 to 4.32).
Conclusion
Young age, lower body mass index, lower parity, and premenopausal status were significantly associated with dense breasts in Korea.
Keywords: Breast, Mammography, Risk factors, Cross-sectional study, Korea
Introduction
Mammographic density is suggested as a strong predictor for breast cancer [1]. Women in the highest breast density category are thought to have a 4 to 6-fold increased risk of breast cancer [1,2]. For Asians, breast cancer risk is thought to be increased by 2 to 5-fold in women with dense breasts [3,4]. Although controversies remain in choosing the precise method of measuring breast density in comparisons between ethnic groups, mammographic density positively correlates with breast cancer [5].
Previous studies have evaluated the relationships between reproductive factors and mammographic density. Having a full-term birth is consistently suggested to have an inverse association with breast density [6,7]. However, the evidence relating menarche, menopausal duration, oral contraceptive use and hormone replacement therapy to breast density is inconsistent [8]. Additionally, only a few studies have examined menstrual and reproductive risk factors for correlation with dense breasts in an Asian population [3,6].
Asian countries show a rapidly increasing rate of breast cancer mortality, and Korea has the highest rate of increase [9,10]. Rapid change to a Westernized lifestyle is suggested to be a crucial factor in the increased breast cancer incidence and mortality rate in Asian countries [11]. Breast density is related to lifestyle factors, and identifying factors that influence breast density may reveal associations that need to be taken into account when using breast density as a marker for breast cancer risk.
In this study, we examined associations among dense breast patterns, body mass index, reproductive and menstrual hormone-related factors in Korean women and we stratified our analysis by menopausal status.
Materials and Methods
Women 40 to 80 years of age, with no history of breast cancer, were included in this cross-sectional study conducted in three cities of Gyeonggi-do, in Korea, during two months in 2008. Study subjects were volunteers who visited mobile vans to receive digital mammography and had offered informed consent before enrollment. Using a computerised system, one radiologist classified breast density patterns on the basis of the Breast Imaging Reporting and Data System (BI-RADS, American College of Radiology, Reston, VA) of the American College of Radiology, and another radiologist, who was a specialist in radiologic testing of breasts, supervised the interpretation. Four density patterns were classified using the mediolateral oblique and caudocranial views; (I) almost entirely fat, (II) scattered fibroglandular densities, (III) heterogeneously dense, and (IV) extremely dense. To compare fatty breasts and dense breasts, we categorized "almost entirely fat" and "scattered fibroglandular densities" as fatty breasts, and "heterogeneously dense" and "extremely dense" as dense breasts.
A self-administered questionnaire was used to gather information on demographics (age and education), height, weight, history of breast diseases, family history of breast cancers, alcohol consumption, cigarette smoking, age at menarche, menopausal status, age at menopause, number of children, oral contraceptive use, and hormone therapy use. In total, 521 women underwent the screening test. After five women who did not answer the questionnaire were excluded; 516 women were included in the analysis. Among those, one was suspected of having cancer and five were diagnosed with benign breast diseases.
Family histories of breast cancer were limited to relatives of the first and second degree. Body mass index (BMI) were calculated as weight/height2 (kg/m2) and subdivided into three categories based on the Asian classification as follows: lower than 23.0 as normal or underweight, 23.0-24.9 as overweight, and 25.0 or more as obese. Menopausal duration was calculated by subtracting age at menopause from current age and was classified into three groups: ≤4, 5-14, and ≥15 years. Variables including menopausal duration and hormone replacement therapy were considered among postmenopausal women.
The logistic regression model was applied to estimate odds ratios (ORs) and 95% confidence intervals (CIs). To evaluate the independent effects of each factor, we used multivariate logistic regression analysis which included age, family history of breast cancer, years of education, BMI, alcohol consumption, age at menarche, menopausal status, parity, and oral contraceptive use. All statistical analyses were conducted using SPSS ver. 12.0 (SPSS Inc., Chicago, IL).
Results
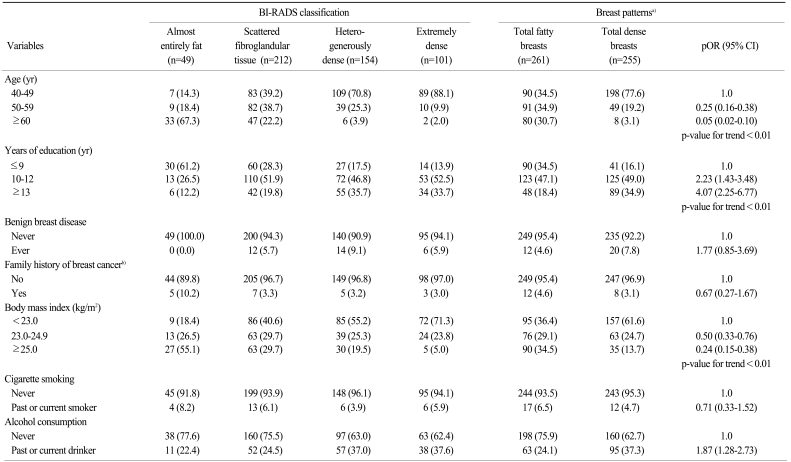
The distribution of the study population into BI-RADS classes and breast patterns is presented using basic characteristics including: BMI, smoking and alcohol consumption (Table 1). Of 516 women, 49 (9.5%) had almost entirely fatty breasts and 212 (41.1%) had breasts with scattered fibroglandular tissue, resulting in a total of 261 (50.6%) classified as fatty breasts. There were 255 (49.4%) subjects with dense breasts. Among dense breasts, 154 (29.8%) were heterogeneously dense and 101 (19.6%) were extremely dense. The mean age of the participants was 50.6 years (SD, 8.8 years). Compared to women in their 40s, women in their 50s or older than 60 tended to have lesser dense breasts. Women who were highly educated and consumed alcohol had a greater incidence of dense breasts. As BMI increased, fewer women had dense breasts (p-value for trend<0.01).
Table 1.
Distribution of BI-RADS classification and breast patterns by basic characteristics and life style factors among Korean women, 2008
BI-RADS, Breast Imaging Reporting and Data System from the American College of Radiology; pOR, prevalent odds ratio; CI, confidence interval. a)'Total fatty breasts' includes 'almost entirely fat' and 'scattered fibroglandular tissue', and 'total dense breasts' includes 'hetero-generously dense' and 'extremely dense', b)Limited in 1st and 2nd degree.
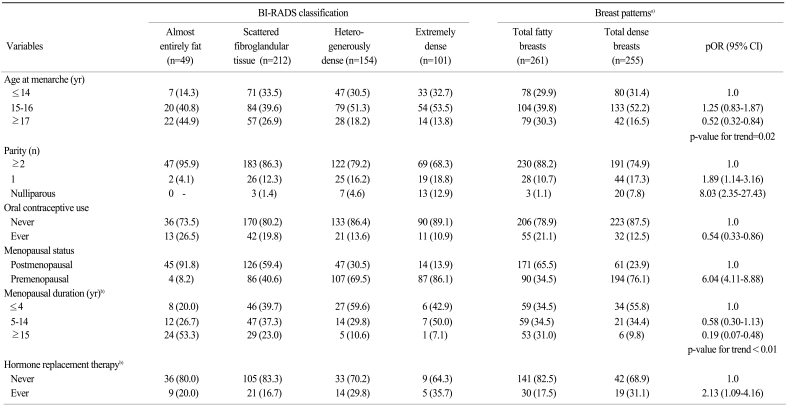
Table 2 presents the distribution of the study population into BI-RADS classes and breast patterns by hormonal and reproductive factors. Late menarche (p-value for trend=0.02) and oral contraceptive use were associated with fatty breasts. Compared to women who had given birth to two or more children, nulliparous women had an 8-fold higher incidence of dense breasts (p-value for trend<0.01). Premenopausal status was significantly related to dense breasts (prevalent OR, 6.14; 95% CI, 4.11 to 8.88). Among postmenopausal women, longer menopausal years were inversely associated with dense breasts (p-value for trend<0.01), whereas hormone replacement therapy was positively related to dense breasts.
Table 2.
Distribution of BI-RADS classification and breast patterns by reproductive and hormonal factors among Korean women, 2008
BI-RADS, Breast Imaging Reporting and Data System from the American College of Radiology; pOR, prevalent odds ratio; CI, confidence interval. a)'Total fatty breasts' includes 'almost entirely fat' and 'scattered fibroglandular tissue', and 'total dense breasts' includes 'hetero-generously dense' and 'extremely dense', b)Postmenopausal women without missing (total=226).
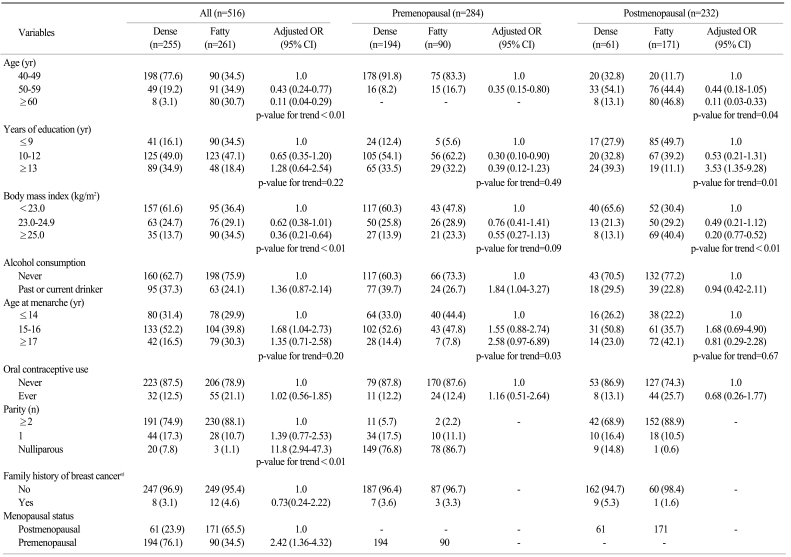
In the multivariate regression model, age and BMI were inversely associated with dense breasts (p-value for trend<0.01, both) (Table 3). Compared to women who had delivered two or more children, women with one child had a 1.4-fold, and nulliparous women had eleven-fold incidence of more dense breasts (p-value for trend<0.01). Premenopausal women had 2.4-fold higher incidence of dense breasts than postmenopausal women (OR, 2.42; 95% CI, 1.36 to 4.32). Younger age, alcohol drinking and older menarche were related to dense breasts among premenopausal women, whereas lesser age, lesser education years and lesser body mass index were related to dense breasts among postmenopausal women.
Table 3.
Adjusted odds ratios of selected variables on breast patterns among Korean women stratified by menopausal status, 2008
OR, odds ratio; CI, confidence interval. a)Limited in 1st and 2nd degree.
Discussion
In this cross-sectional study, we found that age, BMI, age at menarche and oral contraceptive use are inversely associated with dense breasts. On the other hand, years of education, alcohol consumption, nulliparity, premenopausal status and hormone replacement therapy are positively associated with dense breasts. After adjustment, age and BMI remained to be associated with fatty breasts, whereas nulliparity and premenopausal status were related to dense breasts.
It has been suggested that more than 40% of breast density could be explained by demographic, anthropometric, reproductive and lifestyle factors [5]. It is consistently reported that dense breasts are less widespread among older women [12]. Parity and a greater number of live births also correlate with lower levels of dense breasts [12-14]. Menopause has been well established to be associated with lesser dense breasts [6,13].
Age at menarche is a proxy to exposure of ovarian hormones as well as to adolescent nutrition, and it is hypothesized that older menarche is related to lower breast density. Most of the previous studies reported a slight inverse association between breast density and older age at menarche, but the relationship was statistically insignificant [6,13]. A few studies have found relationships between older age at menarche and increased breast density, which were remarkable among women younger than 60 years old [8,15]. In our study, age at menarche was not associated with dense breast patterns for the entire population, whereas older menarche was significantly correlated with dense breasts among premenopausal women; these results were opposite from what we expected. After stratifying our study population by menopausal status, however, we could not exclude any possibility of "chance effect," due to the small size of our study population. In our study, longer duration of menopause was associated with lower numbers of dense breasts. Studies examining the relationship between menopausal years and breast density are few, and the results are inconsistent [6]. One study reported that women older than 51 years had 1.5 times the incidence of dense breasts vs. women younger than 48 years, which is consistent with our study [16].
Most previous studies, but not all, found positive relationships between hormonal replacement therapy and breast density [7,15]. Some, but not all, studies have shown negative relationships between oral contraceptive use and dense breasts [6,8,17].
Previous studies have consistently shown strong positive correlations between obesity and breast density [7,12], and it has been suggested that anthropometric factors present at a young age act throughout life [18].
It is well known that reproductive or hormonal factors have an effect on breast cancer development and it has been hypothesized that they similarily effect risks associated with dense breasts, but studies focusing on biologic mechanisms are limited [19]. One possible mechanism is that breast glandular tissue is overwhelmingly concentrated in the dense areas [19,20], which is correlated to the "estrogen augmentation by progesterone" hypothesis of breast cancer, which states that longer exposure to estrogen and progesterone may induce breast epithelial cell proliferation [21]. Ethnicity also has been suggested as a factor associated with breast density [22]. It has been proposed that cumulative exposure to inherited and environmental factors affect breast density and breast cancer risk throughout life [5,12].
The proportion of dense breasts found in 40-49 year old women in New Hampshire, USA was 48% [15], whereas it was 68.8% in our study. Although a "chance effect" is not totally excluded, a high proportion (60-70%) of dense breasts has been consistently reported among Korean women of young age [23,24]. Acculturation, including a higher level of education, lower age at menarche, strong family history of breast cancer, less parity and late child bearing may have increased breast density in young ages in Koreans [25]. More studies are warranted to reveal the role of ethnicity in relation to breast density and cancer, including studies on the effects of breast size and genetic interaction [20,22].
One limitation of our study is the relatively small number of subjects, which may have reduced study power, especially after stratifying our analysis by menopausal status. However, the reason why we have produced an adjusted odds ratio, by menopausal status, was to check for any possible relationship in each strata. A second limitation is that we dichotomised breast density into two groups using the BI-RADS system, resulting in detailed information being omitted. Also, BI-RADS scores are a qualitative measurement of breast density, so a precise, quantitative estimation was impossible.
The strength of our study is that it included various variables, including age at menarche, hormone replacement therapy and oral contraceptive use, which may contribute to the current knowledge regarding the association between hormonal factors and breast density.
In summary, as in previous studies conducted in Western countries, younger age, lower BMI, lower parity, and premenopausal status were significantly associated with dense breasts in Korea. Further studies on the effects of age at menarche, hormone replacement therapy, oral contraceptive use, on breast density, using a larger Asian population are needed.
Conclusion
It has been suggested that dense breasts, as categorized by mammography, are related to other risk factors for breast cancer, but controversy still remains. In our study, compared to fatty breasts, dense breast women were younger, premenopausal, nulliparous and had a lower body mass index. Factors associated with dense breasts in our study are indicators of higher exposure to estrogen and progesterone, which are also risk factors for breast cancer. Our findings may significantly add to the present knowledge on the association between hormonal factors and breast density, especially for the Asians who have highly westernized lifestyles which may result in increased incidence of and mortality from breast cancer.
Acknowledgments
This study was supported by a grant from the National Cancer Center Korea (Grant No. 1010200).
Footnotes
Conflict of interest relevant to this article was not reported.
References
- 1.Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356:227–236. doi: 10.1056/NEJMoa062790. [DOI] [PubMed] [Google Scholar]
- 2.McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15:1159–1169. doi: 10.1158/1055-9965.EPI-06-0034. [DOI] [PubMed] [Google Scholar]
- 3.Nagata C, Matsubara T, Fujita H, Nagao Y, Shibuya C, Kashiki Y, et al. Mammographic density and the risk of breast cancer in Japanese women. Br J Cancer. 2005;92:2102–2106. doi: 10.1038/sj.bjc.6602643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ursin G, Ma H, Wu AH, Bernstein L, Salane M, Parisky YR, et al. Mammographic density and breast cancer in three ethnic groups. Cancer Epidemiol Biomarkers Prev. 2003;12:332–338. [PubMed] [Google Scholar]
- 5.Maskarinec G, Pagano I, Chen Z, Nagata C, Gram IT. Ethnic and geographic differences in mammographic density and their association with breast cancer incidence. Breast Cancer Res Treat. 2007;104:47–56. doi: 10.1007/s10549-006-9387-5. [DOI] [PubMed] [Google Scholar]
- 6.Heng D, Gao F, Jong R, Fishell E, Yaffe M, Martin L, et al. Risk factors for breast cancer associated with mammographic features in Singaporean chinese women. Cancer Epidemiol Biomarkers Prev. 2004;13:1751–1758. [PubMed] [Google Scholar]
- 7.El-Bastawissi AY, White E, Mandelson MT, Taplin SH. Reproductive and hormonal factors associated with mammographic breast density by age (United States) Cancer Causes Control. 2000;11:955–963. doi: 10.1023/a:1026514032085. [DOI] [PubMed] [Google Scholar]
- 8.Butler LM, Gold EB, Greendale GA, Crandall CJ, Modugno F, Oestreicher N, et al. Menstrual and reproductive factors in relation to mammographic density: the Study of Women's Health Across the Nation (SWAN) Breast Cancer Res Treat. 2008;112:165–174. doi: 10.1007/s10549-007-9840-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bray F, McCarron P, Parkin DM. The changing global patterns of female breast cancer incidence and mortality. Breast Cancer Res. 2004;6:229–239. doi: 10.1186/bcr932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Won YJ, Sung J, Jung KW, Kong HJ, Park S, Shin HR, et al. Nationwide cancer incidence in Korea, 2003-2005. Cancer Res Treat. 2009;41:122–131. doi: 10.4143/crt.2009.41.3.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chia KS, Reilly M, Tan CS, Lee J, Pawitan Y, Adami HO, et al. Profound changes in breast cancer incidence may reflect changes into a Westernized lifestyle: a comparative population-based study in Singapore and Sweden. Int J Cancer. 2005;113:302–306. doi: 10.1002/ijc.20561. [DOI] [PubMed] [Google Scholar]
- 12.Boyd NF, Rommens JM, Vogt K, Lee V, Hopper JL, Yaffe MJ, et al. Mammographic breast density as an intermediate phenotype for breast cancer. Lancet Oncol. 2005;6:798–808. doi: 10.1016/S1470-2045(05)70390-9. [DOI] [PubMed] [Google Scholar]
- 13.Maskarinec G, Meng L, Ursin G. Ethnic differences in mammographic densities. Int J Epidemiol. 2001;30:959–965. doi: 10.1093/ije/30.5.959. [DOI] [PubMed] [Google Scholar]
- 14.Kang EY, Shin JH, Kang SG, Hwang YN, Cha ES, Song SW. Relationship between mammographic dense breast and other risk factors of breast cancer in Korean women. J Korean Acad Fam Med. 2007;28:937–942. [Google Scholar]
- 15.Titus-Ernstoff L, Tosteson AN, Kasales C, Weiss J, Goodrich M, Hatch EE, et al. Breast cancer risk factors in relation to breast density (United States) Cancer Causes Control. 2006;17:1281–1290. doi: 10.1007/s10552-006-0071-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gram IT, Bremnes Y, Ursin G, Maskarinec G, Bjurstam N, Lund E. Percentage density, Wolfe's and Tabár's mammographic patterns: agreement and association with risk factors for breast cancer. Breast Cancer Res. 2005;7:R854–R861. doi: 10.1186/bcr1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCormack VA, Perry N, Vinnicombe SJ, Silva Idos., S Ethnic variations in mammographic density: a British multiethnic longitudinal study. Am J Epidemiol. 2008;168:412–421. doi: 10.1093/aje/kwn169. [DOI] [PubMed] [Google Scholar]
- 18.Jeffreys M, Warren R, Gunnell D, McCarron P, Smith GD. Life course breast cancer risk factors and adult breast density (United Kingdom) Cancer Causes Control. 2004;15:947–955. doi: 10.1007/s10522-004-2473-3. [DOI] [PubMed] [Google Scholar]
- 19.Ursin G, Hovanessian-Larsen L, Parisky YR, Pike MC, Wu AH. Greatly increased occurrence of breast cancers in areas of mammographically dense tissue. Breast Cancer Res. 2005;7:R605–R608. doi: 10.1186/bcr1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stuedal A, Ma H, Bernstein L, Pike MC, Ursin G. Does breast size modify the association between mammographic density and breast cancer risk? Cancer Epidemiol Biomarkers Prev. 2008;17:621–627. doi: 10.1158/1055-9965.EPI-07-2554. [DOI] [PubMed] [Google Scholar]
- 21.Pike MC, Spicer DV, Dahmoush L, Press MF. Estrogens, progestogens, normal breast cell proliferation, and breast cancer risk. Epidemiol Rev. 1993;15:17–35. doi: 10.1093/oxfordjournals.epirev.a036102. [DOI] [PubMed] [Google Scholar]
- 22.Boyd NF, Dite GS, Stone J, Gunasekara A, English DR, McCredie MR, et al. Heritability of mammographic density, a risk factor for breast cancer. N Engl J Med. 2002;347:886–894. doi: 10.1056/NEJMoa013390. [DOI] [PubMed] [Google Scholar]
- 23.Kim SH, Kim MH, Oh KK. Analysis and comparison of breast density according to age on mammogram between Korean and Western women. J Korean Radiol Soc. 2000;42:1009–1014. [Google Scholar]
- 24.Cho JJ, Song HJ, Koh EY, Song YM, Han BK, Yun YS, et al. Mammographic breast density and risk factors of breast cancer in Korean women using multicenter study. J Korean Acad Fam Med. 2006;27:33–41. [Google Scholar]
- 25.Tseng M, Byrne C, Evers KA, London WT, Daly MB. Acculturation and breast density in foreign-born, U.S. Chinese women. Cancer Epidemiol Biomarkers Prev. 2006;15:1301–1305. doi: 10.1158/1055-9965.EPI-06-0159. [DOI] [PubMed] [Google Scholar]