Abstract
This study evaluated a five-item screening measure of Callous Unemotional (CU) traits using items drawn from the Preschool Form of the Achenbach System of Empirically Based Assessment (ASEBA). Using data from the Durham Child Health and Development study (N=178), confirmatory factor analyses demonstrated that CU items could be distinguished from Attention Deficit/Hyperactivity Disorder (ADHD) and Oppositional Defiant (ODD) items. The two-year stability (N=137) of CU (ϕ=.84) was comparable to that of ADHD (ϕ=.79) and ODD (ϕ=.69). Three groups of children were selected based on parent-rated ODD and CU behaviors at the 36-month assessment (N=37; ODD+CU, N=7; ODD-only, N=12; non-ODD, N=18). Multiple measures of infant temperament predicted group membership with 84% accuracy. Consistent with Frick and Morris’ (Journal of Clinical Child and Adolescent Psychology 33(1):54–68, 2004) hypotheses, ODD+CU and ODD-only children exhibited temperamental profiles in infancy that were consistent with low fear and emotionally dysregulated pathways into conduct problems, respectively.
Keywords: Callous Unemotional, Screening measure, Early childhood
The construct of Callous Unemotional (CU) traits refer to a set of behaviors that include diminished guilt following negative actions, low empathy and fear, poor recognition of fear or distress in others, reduced reactivity to challenging events, and an over-focus on reward and insensitivity to punishment (Frick and White 2008). There is a growing recognition that CU traits provide unique information relative to more well established conceptualizations of disruptive behavior in childhood, including oppositional defiant disorder, conduct disorder, and attention-deficit/hyperactivity disorder (APA 2000). For example, factor analytic studies show that CU traits emerge as a distinct factor even when measures of ADHD, ODD and CD are also included in the analysis (Dadds et al. 2005; Frick et al. 2000; Pardini et al. 2006). Moreover, approximately one-third of all youth who exhibit elevated levels of conduct problems (CP) also exhibit elevated levels of CU traits (e.g., Christian et al. 1997; Frick et al. 2000; Murrie and Cornell 2002; Woodworth and Waschbusch 2008).
Compared to children with elevated conduct problems (CP) but low on CU (CP-CU), children who are high on both CP and CU (CP+CU): (a) exhibit a higher frequency, severity, and greater persistence of antisocial behavior; (b) are less likely to exhibit a hostile attribution bias but more likely to have positive evaluations of aggression; (c) have higher rates of antisocial behavior in their families and higher heritability estimates of their antisocial behavior; (d) are more likely to exhibit fearless (low fear) temperamental styles; (e) show lower physiological responses to negative emotions; (f) are less likely to show empathy toward victims; and (g) are less accurate in identifying emotions in others (see Blair et al. 2006; Frick and White 2008; Kotler and McMahon 2005 for reviews). The consistent pattern of group differences observed between CP+CU and CP-CU youth in middle childhood and adolescence provides a strong rationale for incorporating measures of CU into studies of disruptive behavior. Doing so holds the promise of providing new insights into the causes and course of disruptive behavior, as well as for generating novel approaches for treatment (Dadds and Salmon 2003; Hawes and Dadds 2005; Salekin 2010; Salekin et al. 2010; Viding et al. 2005; Waschbusch et al. 2007). This potential promise is a major reason why CU is being considered as a modifier to Conduct Disorder diagnoses in DSM-V (Frick and Moffitt 2010).
Although the validity and utility of extending the measurement of CU into middle childhood is well established (Frick 2009), there is a paucity of research on CU in early childhood. In fact, we are only aware of one study that explicitly examined CU in a preschool age sample (Kimonis et al. 2006). However, Dadds and colleagues have included children as young as 3 years old in studies investigating the measurement of CU, as well as the association between empathy and psychopathy (Dadds et al. 2005, 2009). Moreover, Raine and colleagues established that poor fear conditioning, fearlessness, and stimulation seeking—temperamental characteristics related to CU—measured at age 3 years were predictive of childhood aggression, adult criminality, and adult psychopathy (Gao et al. 2010a, 2010b; Glenn et al. 2007; Raine et al. 1998). Others have also established the validity of measuring guilt and empathy in children as young as 3 years old (Cornell and Frick 2007; Kochanska et al. 2009; Luby et al. 2009). Hence, although few studies have explicitly focused on CU in early childhood, individual differences in fearlessness, guilt, and empathy are evident as young as age three, which implies that the measurement of CU may be useful. Moreover, given that the measurement of CP in early childhood is well accepted, it may be particularly useful to measure CU at the same time (Alink et al. 2006; Tremblay et al. 2004).
Measuring CU in conjunction with other disruptive behaviors in early childhood would facilitate efforts to reduce heterogeneity within the group of children with early onset conduct problems. Frick and Morris (2004) proposed that among children with early onset conduct problems, those with low and high CU followed emotional dysregulation and low fear pathways into conduct problems, respectively. The emotional dysregulation pathway was characterized by high negative reactivity, especially to challenge, as well as poor regulation of negative affect which includes low effortful control. The low fear pathway was characterized by low fear and physiological under-arousal, including potential insensitivity to parental socialization efforts. Although provocative, we are unaware of any study that has directly tested Frick and Morris’ (2004) hypotheses using data that were collected prospectively from infancy into early childhood. Although there is at least some evidence to suggest that childhood antisocial behavior is associated with reduced autonomic nervous system activity (ANS) both at rest and in reactivity to stress (consistent with a low fear pathway), extant studies are limited by (1) a failure to distinguish antisocial behavior as a function of CU and (2) typically are based on child and adolescent samples with little consideration of potential developmental variations in ANS activity (van Goozen et al. 2007). Similarly, although numerous studies have considered temperamental precursors to subsequent externalizing or antisocial behavior, virtually none has distinguished antisocial behavior as a function of CU (e.g., Bates et al. 1998; Gilliom and Shaw 2004; Hirshfeld-Becker et al. 2002).
The primary goal of the current study was to investigate whether a screening measure of CU could be developed from the preschool version of the Achenbach System of Empirically Based Assessment (ASEBA). Given its wide use, the availability of a CU screener from items on the ASEBA would stimulate secondary analyses of extant and ongoing studies that use this instrument. Doing so would represent a financially and time efficient method for more fully testing whether CU helps reduce heterogeneity within the group of children with early onset conduct problems (Frick and Viding 2009). There is a well established precedent for utilizing short, screening measures of children’s behavior. For example, the Strengths and Difficulty (SDQ) questionnaire, which consists of five, 5-item scales including hyperactivity, conduct problems, emotional problems, peer problems, and prosocial behavior, is widely used dimensional measure of psychopathology in large scale studies and does a reasonably good job of screening for psychiatric diagnosis (Goodman and Goodman 2009; Goodman et al. 2000, 2004; Goodman and Scott 1999). Similarly, the IOWA Conners rating scale, which consists of two, 5-items scales including inattention/overactivity and oppositional/defiance, is widely used as a measure of treatment response (e.g., Kolko et al. 2009; Pelham et al. 2002; Remschmidt et al. 2005; Wilens et al. 2003).
In sum, the proposed study investigated the factor structure, stability, and utility of a 5-item screening measure of CU behaviors derived from the preschool form of the ASEBA. Specifically, confirmatory factor analyses were used to test whether parents of young children could differentiate CU from ADHD and ODD behaviors. It was hypothesized that CU would factor separately from both ADHD and ODD. Confirmatory factor analyses were also used to evaluate the stability of CU. Early childhood is a developmental period characterized by reductions in disruptive behaviors (Cote et al. 2006; Shaw et al. 2005). This raises questions about whether individual differences in CU are stable across time. It was hypothesized that individual differences in CU would be as stable as those for the more commonly assessed dimensions of ADHD and ODD. Finally, in order to evaluate the utility of measuring CU, children with elevated oppositional defiant behaviors were distinguished on the basis of their CU (i.e., ODD+CU and ODD-only groups). Prospective measures of infant temperament were used to predict group membership at age 36-months. It was hypothesized that children in the ODD+CU group would be characterized by low fear and low reactivity to challenge in infancy, whereas children in the ODD-only group would be characterized by emotional dysregulation in infancy.
Methods
Participants
Participants were drawn from the Durham Child Health and Development Study, a prospective longitudinal study consisting of 206 healthy, full-term infants who were recruited at 3 months of age. The sampling design of the DCHD study involved recruiting approximately equal numbers of African and European American families from lower- and higher-income groups. Families who were expecting a new child were targeted for inclusion in the DCHD study. Families were recruited from a largely urban community via fliers and postings at birth and parenting classes, as well as through telephone contact information from birth records. Infants included in the study were healthy, full-term, and born without significant birth complications. Family’s race was determined from mother self-report; income status was determined by whether the family was above or below 200% of the federally established poverty threshold.
Questions about the factor structure and stability of CU items were addressed by using data from the N=178 and N=137 children who participated in the 36 and 36+60 month assessments, respectively. The question about the utility of CU was addressed using a sub-sample of youth (N=37) with elevated ODD behaviors at the 36-month assessment. Specially, we identified N=19 children with T scores on the parent-rated ASEBA ODD scale that were greater than or equal to 63. Although not in the clinical range, T scores of 63 denote developmentally inappropriate levels of behavior (90th percentile by norms). This group was subdivided as a function of their CU factor scores. CU factors scores of >=2 represented developmentally inappropriate behavior (96th percentile in the total sample) and identified the approximately one-third of children with elevated ODD that were also rated as high on CU—a proportion that has been observed in numerous previous studies (Frick and White 2008). A third group of N=18 children were randomly drawn from the remaining sample. Children in the third group did not exhibit elevated ODD or CU behaviors but were similar to children with elevated ODD with respect to gender (71%, 50%, and 67% male for ODD+CU, ODD-only, and non-ODD groups, respectively; p=.56), poverty level at the time of recruitment (86%, 50%, 61% poor for ODD+CU, ODD-only, and non-ODD groups, respectively; p=.30), and race (57%, 67%, and 44% African American for ODD+CU, ODD-only, and non-ODD groups, respectively; p=.48). Demographic characteristics of the full and partial samples are summarized in Table 1.
Table 1.
Sample description (36 month assessment)
| Total N=178 M (SD) | Subsample N=37 M (SD) | ODD+CU N=7 M (SD) | ODD-only N=12 M (SD) | Non-ODD N=18 M (SD) | |
|---|---|---|---|---|---|
| ODD | 0.5 (0.4) | 0.9 (0.6) | 1.5 (0.2) | 1.3 (0.2) | 0.4 (0.3) |
| CU | 0.2 (0.3) | 0.4 (0.5) | 1.2 (0.3) | 0.4 (0.2) | 0.1 (0.2) |
| ADHD | 0.7 (0.5) | 0.9 (0.6) | 1.8 (0.4) | 1.0 (0.5) | 0.6 (0.5) |
| % | % | % | % | % | |
| Poverty | 49 | 62 | 86 | 50 | 61 |
| African American | 56 | 54 | 57 | 67 | 44 |
| Male | 51 | 62 | 71 | 50 | 67 |
ODD = mean score for 6 Oppositional defiant items; CU = mean score for 5 callous unemotional trait items; ADHD = mean score for 6 attention deficit/hyperactivity disorder items; Below Poverty = family income <=200% poverty threshold for given household size at study entry
Procedure
Families were part of an ongoing prospective longitudinal study that began when children were 3 months old. The current analyses examine physiologic, observational, and questionnaire data from laboratory visits that occurred when the infants were 3, 6, 36, and 60 months of age. At each of these visits, infants and their mothers participated in several joint and individual tasks followed by a standardized interview and completion of demographic questionnaires by the mother. Child affect and physiology were later coded by trained and reliable coders (see below).
Measures
Infant Behavior Questionnaire-Revised (IBQ-R; Gartstein and Rothbart 2003)
Primary caregivers completed the IBQ-R at the 3- and 6-month visits. The items on the IBQ-R ask caregivers to rate the frequency of specific temperament-related behaviors that may have occurred in a variety of everyday situations and that were observed over the past 1–2 weeks. Items were rated on a 7-point Likert scale (1 = never, 4 = half of the time, 7 = always). Three infant temperament scales were used in the current study including Fear (16 items; e.g., startles to a sudden or loud noise; never warms up to unfamiliar adults), Soothability (18 items; e.g., soothes immediately after rocking, after singing), and Falling Reactivity /Rate of Recovery (13 items; e.g., hard time settling down to sleep; stays upset for 20 min or longer), each of which had good internal consistency in the total sample (Fear α=.90 and .93; Soothability α=.75 and .84; Falling Reactivity/Rate of Recovery α=.83 and .83, at 3- and 6-month visits respectively).
Achenbach System of Empirically Based Assessment, Preschool Forms (ASEBA; Achenbach and Rescorla 2000)
Primary caregivers completed the ASEBA at the 36 and 60 month visits. The ASEBA is a standardized assessment that indexes children’s behavioral/emotional problems by having caregivers rate their children on items describing the children currently or within the last 2 months. This version of the ASEBA consists of 99 items describing behavioral/emotional problems, plus an open-ended item for additional problems. In addition to traditional composites of internalizing and externalizing behaviors, a new feature in the ASEBA scoring is a profile of DSM-referenced scales, which comprise items that experienced psychiatrists and psychologists from ten cultures rated as being very consistent with DSM diagnostic categories. The current study used 17 items in order to evaluate the dimensionality of disruptive behavior at age 3. Specifically, 6 items each were drawn from the DSM-IV referenced ADHD (e.g., can’t concentrate; can’t sit still; gets into everything) and ODD (e.g., defiant; uncooperative) scales. Five items representing callous unemotional traits were also included (i.e., item 27—doesn’t seem to feel guilty after misbehaving; item 58—punishment doesn’t change behavior; item 67—seems unresponsive to affection; item 70—shows little affection toward people; item 72—shows too little fear of getting hurt).
Face-to-Face Still-Face Paradigm (FFSFP; Adamson and Frick 2003; Tronick et al. 1978)
To assess infants’ behavioral and physiological reactivity, they were observed in the FFSFP during laboratory visits at 3- and 6-months of age. Mothers placed infants in an infant seat and sat in a chair directly in front of the infants. Mothers were given specific, standard instructions for each episode of the FFSFP (normal play, still-face, reunion). For the normal play episode mothers were instructed to play with their babies as they normally would. Immediately after the 2-min normal play episode, mothers were told to turn away from their infants for 15 s, then to turn back toward their infants for the still-face episode. Mothers were instructed to look at their infants for 2 min without responding in any way with facial or vocal expressions and were assured that the examiner would stop the still-face episode if the infant became too distressed. A 2-min reunion episode followed the still-face in which mothers were instructed to respond to their babies in any way they felt was appropriate. If an infant was unable to be soothed at any point in the procedure, the FFSFP was stopped. The episodes of the FFSFP were video recorded using a split-screen procedure so that the behaviors of both mothers and infants could be observed.
Infant Observed Affect During the FFSFP
As described previously (Moore et al. 2009), infants’ affect during the FFSFP was coded by trained coders, naïve to hypotheses of the current study, in 1-s intervals as positive, neutral, negative, or missing if coders were unable to see infants’ faces. Coders were initially trained to reliability using a large pool of recorded FFSFP interactions. In the current study, interobserver agreement for infant affect codes (K=.89) was calculated on 15% of the interactions (selected randomly). Agreement was calculated as both coders observing the same behavior within 1 s of each other and quantified using kappa to correct for chance agreement. The total number of seconds in which each affective state code occurred was calculated for each infant during each episode of the FFSFP and was expressed as a percentage of valid (not missing) time.
Cardiac Monitoring During the FFSFP
As described previously (Moore et al. 2009), the researcher placed two disposable pediatric electrodes on the child’s chest. Electrodes were connected to a preamplifier, the output of each was transmitted to a monitor configured to collect heart interbeat intervals (IBIs; Mini Logger 2000; Mini-Mitter Corp., Bend, OR). Data files containing the IBIs for the entire period of collection for infants were transferred to a computer for later artifact editing and analysis using MXEdit software (Delta Biometrics, Bethesda, MD). Two researchers trained to reliability in MXEdit, with Porges’s Lab at the University of Maryland, edited the files by scanning the data for outlier points relative to adjacent data and replacing those points by dividing them or summing them so that they would be consistent with the surrounding data. Due to difficulties in collecting cardiac data from infants of this age (i.e., pulling on electrodes, equipment failure), only participants who had full and sufficient data with less than 10% editing were used in the current analyses. Heart Period (HP) was calculated in 15-s epochs during each episode of the FFSFP using Porges’s (1985) method. These epoch durations are typical and valid for studies of short duration tasks with infants (Bar-Haim et al. 2000).
Mean values of HP during each episode of the FFSFP were computed. Larger values of HP indicated longer mean HP (or lower heart rate). Analyses involved three HP variables: (1) mean HP during the normal talk period, (2) HP reactivity, computed as the simple difference in mean HP between the normal talk and still face periods (i.e., still face—normal talk), and (3) HP recovery, computed as the simple difference in mean HP the still face and reunion periods (i.e., reunion—still face). Negative values for HP reactivity and recovery indicated decreases in heart period (hence, increases in heart rate), while positive values for HP reactivity and recovery indicated increases in heart period (hence decreases in heart rate).
Analytic Strategy
The first research question tested the dimensionality of ADHD, ODD, and CU items. Five Confirmatory Factor Analyses (CFAs) were estimated using parent rated data on ASEBA items at the 36-month assessment. A one-factor model implied that ADHD, CP, and CU behaviors were indistinguishable to parents and were best represented as unidimensional. Three, two-factor models (i.e., CU vs. other; CP vs. other; ADHD vs. other) implied that parents could individually differentiate ADHD, CP, or CU as a distinct factor but could not differentiate the remaining items. The final, three-factor model implied that parents could reliably differentiate ADHD, CP, and CU from each other. Chi square differences tests, were used to test the hypothesis that the three-factor model would provide the best fit to the data. The second research question evaluated the stability of CU behaviors. A longitudinal CFA was estimated involving items assessed at 36 and 60 month assessments. The latent correlation between CU factors at two times provided a stability estimate that was free of measurement error. The third research question tested whether children who exhibited elevated ODD and CU exhibited a different profile of infant temperament than did those who exhibited elevated ODD but not CU at 36 months. CFAs used a weighted least squares estimator with mean and variance adjustments, as implemented in Mplus version 5 (Muthén and Muthén 1998–2008) in order to accommodate the ordinal nature of items. Discriminant function analysis and all descriptive statistics were estimated using of SAS© version 9.2.
Results
Question 1—Dimensionality of CU, ODD, and ADHD Behaviors at 36-months of Age
Item frequencies and polychorric correlations for the 17 items selected to measure ADHD, ODD, and CU at the 36-month assessment are summarized in Table 2. Item frequencies indicate that most children were perceived as having low levels of any behavior problems, though 5–10% of the sample was rated highly for each item. Items were moderately to strongly correlated with most bivariate correlations ranging from .4 to .7.
Table 2.
Item frequencies and polychoric correlations for ADHD, ODD, and CU items at 36-months
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Can’t concentrate | – | ||||||||||||||||
| 2. Can’t sit still | .82 | – | |||||||||||||||
| 3. Can’t stand wait | .55 | .59 | – | ||||||||||||||
| 4. Demands met | .58 | .53 | .69 | – | |||||||||||||
| 5. Into everything | .62 | .59 | .40 | .45 | – | ||||||||||||
| 6. Quickly shifts | .64 | .58 | .58 | .54 | .45 | – | |||||||||||
| 7. Defiant | .46 | .34 | .33 | .59 | .49 | .39 | – | ||||||||||
| 8. Disobedient | .30 | .40 | .39 | .46 | .56 | .34 | .69 | – | |||||||||
| 9. Angry moods | .48 | .55 | .54 | .48 | .57 | .56 | .55 | .50 | – | ||||||||
| 10. Stubborn | .39 | .41 | .46 | .52 | .49 | .33 | .43 | .56 | .61 | – | |||||||
| 11. Temper tantrum | .49 | .53 | .55 | .58 | .52 | .52 | .52 | .58 | .63 | .60 | – | ||||||
| 12. Uncooperative | .55 | .48 | .44 | .45 | .57 | .50 | .67 | .69 | .65 | .66 | .63 | – | |||||
| 13. No guilt after misbehave | .64 | .69 | .57 | .54 | .57 | .67 | .55 | .64 | .67 | .56 | .56 | .64 | – | ||||
| 14. Punish doesn’t change | .56 | .50 | .41 | .54 | .60 | .52 | .57 | .66 | .49 | .49 | .60 | .71 | .66 | – | |||
| 15. Unresponsive affection | .58 | .24 | .58 | .58 | .52 | .43 | .64 | .28 | .51 | .20 | .55 | .61 | .52 | .37 | – | ||
| 16. Shows little affection | .27 | .28 | .24 | .16 | .27 | .36 | .02 | .02 | .55 | .27 | .08 | .16 | .56 | .31 | .58 | – | |
| 17. Too little fear get hurt | .46 | .37 | .32 | .48 | .43 | .60 | .49 | .42 | .47 | .44 | .51 | .36 | .62 | .56 | .35 | .33 | – |
| % Not true | 62 | 49 | 28 | 43 | 38 | 44 | 51 | 41 | 73 | 58 | 49 | 57 | 74 | 61 | 96 | 93 | 76 |
| % Sometimes true | 33 | 43 | 56 | 49 | 48 | 45 | 42 | 53 | 24 | 37 | 44 | 38 | 21 | 36 | 3 | 7 | 16 |
| % Often true | 6 | 8 | 17 | 8 | 14 | 11 | 7 | 6 | 3 | 5 | 7 | 6 | 6 | 4 | 1 | 0 | 8 |
N=178; items were rated on a 3-point ordinal scales (0 = not true, 1 = sometimes true, 2 = often true)
All five CFAs provided a relatively good fit to the observed data; however, consistent with our hypothesis, the three-factor model provided a statistically superior fit to the observed data than did the competing one- and two-factor CFAs. Information regarding model fit and model comparisons is summarized in Table 3. Inspection of results from the 3-factor CFA indicated that all of the latent factors had significant variances (ps<.0001) and that all of the factor loadings were statistically significant. With the exception of a single indicator for CU (“shows little affection”), the three latent variables explained 43–76% of the observed variation in items (the CU latent variable only explained 16% of the observed variation in the “shows little affection” item). Moreover, the average item-level R2 was very similar across constructs (mean R2 for ADHD, CP, and CU items=.61, .61, and .49; CU improved to .57 after the omission of the “shows little affection” item). For purposes of comparison, the corresponding coefficient alphas for the ADHD, CP, and CU items were .83, .83, and .65, respectively; however, given a violation of tau equivalence in these data (i.e., differential strength of association between individual items and the underlying construct), the average item-level R2 values are a better indicator of item reliability than are coefficient alphas (Graham 2006; Raykov 1997). Collectively, these results suggested that the measurement properties of the CU items were very similar to those of the more commonly rated ADHD and CP items. Despite the fact that the three-factor model provided the best fit to the observed data and that item-level characteristics for all three constructs were comparable, the correlations between latent variables were large (ϕADHD/CP=.78; ϕADHD/CU=.88; ϕCP/CU=.91, all ps<.0001). Children who were rated highly on any given measure of CU, ODD, or ADHD, tended to be rated as scoring highly on the other two dimensions as well.
Table 3.
CFA model fit at 36-month assessment
| Model | Description | χ2 (df) | prob | CFI | TLI | RMSEA |
|---|---|---|---|---|---|---|
| 1 | 1 factor | 102.7 (35) | <.0001 | .92 | .96 | .10 |
| 2 | 2 factor (CU vs. other) | 102.5 (35) | <.0001 | .92 | .96 | .10 |
| 3 | 2 factor (ODD vs. other) | 88.0 (36) | <.0001 | .94 | .97 | .09 |
| 4 | 2 factor (ADHD vs. other) | 87.4 (37) | <.0001 | .94 | .97 | .09 |
| 5 | 3 factor (CU, ODD, ADHD) | 80.4 (36) | <.0001 | .95 | .97 | .08 |
| 1 vs. 5 | 22.4 (2) | <.0001 | – | – | – | |
| 2 vs. 5 | 25.2 (2) | <.0001 | – | – | – | |
| 3 vs. 5 | 13.3 (2) | <.0001 | – | – | – | |
| 4 vs. 5 | 11.7 (2) | .003 | – | – | – |
N=178; WLSMV estimator for ordinal items
Question 2—Stability of ADHD, CP, and CU Behaviors from 36- to 60-months of Age
One-hundred thirty seven families were successfully located and agreed to participate in a 60-month assessment.1 A longitudinal three-factor CFA model was fit to item level data from 36- and 60-month assessments. One CU item (“unresponsive to affection”) was omitted from CU factor at 60-months due to a lack of variation, which complicated the estimation of polychorric correlations. The longitudinal CFA model, which included data from a total of N=182 children, fit the data well, χ2 (55)=99.6, p=.0002, CFI=.95, TLI=.97, RMSEA=.07. As is summarized in Table 4, the latent correlations between ADHD, CP, and CU factors at the 60-month assessment were nearly as large as those observed at the 36-month assessment (60-month: ϕADHD/CP=.81; ϕADHD/CU=.82; ϕCP/CU=.79, all ps<.0001). The latent correlations representing the across time stability of ADHD, ODD, and CU factors were also large and statistically significant (across time ADHD, CP, and CU ϕs=.79, .69, and .84, respectively, all ps<.0001). This result confirms that individual differences in CU are as stable as those for ODD and ADHD across the preschool period.
Table 4.
Stability of ADHD, ODD, and CU from 36- to 60-months
| 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|
| 1. ADHD (36 months) | – | |||||
| 2. ODD (36 months) | .78 | – | ||||
| 3. CU (36 months) | .88 | .90 | – | |||
| 4. ADHD (60 months) | .79 | .49 | .75 | – | ||
| 5. ODD (60 months) | .52 | .69 | .72 | .81 | – | |
| 6. CU (60 months) | .54 | .55 | .84 | .82 | .79 | – |
N=182; Stability estimates (in bold) are latent correlations between ADHD, ODD, and CU factors across 36- and 60-month assessments; the WLSMV estimator was used due to ordinal items
Question 3—Utility of Measuring CU in Early Childhood
In order to evaluate the utility of measuring CU behaviors in early childhood, multiple indices of infant temperament were evaluated as potential predictors of group membership (ODD+CU, N=7; ODD-only , N=12; non-ODD, N=18) at 36-months of age. Descriptive statistics and effect sizes for pairwise comparisons are summarized in Table 5. Three results are noteworthy. First, as infants, children in the ODD-only group were rated by their parents as having lower scores on the IBQ falling reactivity scale, indicating that they had a more difficult time recovering after becoming upset relative to either the ODD+CU or non-ODD groups (Cohen ds=|.42 and .54|). Similarly, parents described ODD-only youth as more fearful than other groups (Cohen ds=|.44 and .62|). Given that the fear system is relatively undeveloped in the first 6-months of life, this rating likely reflects greater negative affect for infants who were ODD-only at 36 months. Finally, parents perceived both ODD-only and ODD+CU groups to be less soothable as infants than non-ODD youth (Cohen ds=−.74 and −1.00).
Table 5.
Group differences at 36-months on multiple indices of temperament at 3- and 6-months
| Instrument/Task | Scale/Epoch | Groups |
Pairwise comparisons |
|||||
|---|---|---|---|---|---|---|---|---|
| All M (SD) | ODD+CU (N=7) M | ODD-only (N=12) M | Non-ODD (N=18) M | ODD+CU/ODD-only Cohen d | ODD+CU/Non-ODD Cohen d | ODD-only/Non-ODD Cohen d | ||
| IBQ | Falling react | 5.0 (0.9) | 5.1 | 4.7 | 5.2 | 0.42 | −0.12 | −0.54 |
| Fear | 2.3 (1.0) | 2.2 | 2.7 | 2.0 | −0.44 | 0.16 | 0.62 | |
| Soothability | 5.0 (0.5) | 4.8 | 4.9 | 5.3 | −0.26 | −1.00 | −0.74 | |
| FFSFP positive affect1 | Normal play | 0.19 (0.15) | 0.26 | 0.17 | 0.17 | 0.54 | 0.54 | 0.00 |
| Still face | 0.05 (0.05) | 0.06 | 0.04 | 0.05 | 0.40 | 0.14 | −0.26 | |
| Reunion | 0.17 (0.17) | 0.28 | 0.10 | 0.18 | 1.08 | 0.58 | −0.48 | |
| Reactivity | −0.14 (0.14) | −0.19 | −0.13 | −0.12 | −0.42 | −0.52 | −0.10 | |
| Recovery | 0.12 (0.16) | 0.22 | 0.06 | 0.13 | 1.04 | 0.58 | −0.46 | |
| FFSFP negative affect1 | Normal play | 0.03 (0.04) | 0.03 | 0.04 | 0.02 | −0.32 | 0.10 | 0.42 |
| Still face | 0.18 (0.24) | 0.09 | 0.18 | 0.22 | −0.38 | −0.52 | −0.16 | |
| Reunion | 0.24 (0.29) | 0.13 | 0.31 | 0.22 | −0.62 | −0.30 | 0.32 | |
| Reactivity | 0.15 (0.24) | 0.07 | 0.14 | 0.20 | −0.32 | −0.56 | −0.24 | |
| Recovery | 0.06 (0.23) | 0.04 | 0.13 | 0.01 | −0.38 | 0.12 | 0.50 | |
| FFSFP HP | Normal play | 422.6 (42) | 412.0 | 429.2 | 423.6 | −0.42 | −0.28 | 0.14 |
| Still face | 413.7 (55) | 404.5 | 409.2 | 420.7 | −0.08 | −0.30 | −0.20 | |
| Reunion | 414.8 (40) | 402.7 | 425.9 | 413.7 | −0.58 | −0.28 | 0.30 | |
| Reactivity | −8.9 (24) | −7.6 | −19.9 | −2.9 | 0.52 | −0.20 | −0.72 | |
| Recovery | −1.0 (25) | −1.8 | 8.8 | −6.5 | −0.42 | 0.18 | 0.62 | |
p<.10,
p<.05,
p<.01,
p<.001;
IBQ = Infant Behavior Questionnaire; FFSFP = Face-to-Face Still Face Procedure; Reactivity = Difference from normal talk to still face period (still face—talk); Regulation = Difference fromstill face to reunion period (reunion—still face).
Affect coding from FFSFP was only available at the 6-month visit (non-ODD N=12; ODD-only N=12; ODD+CU N=6)
Second, groups differed in their behavioral response to FFSFP procedure at 6-months of age (see Fig. 1). Specifically, as infants, children in the ODD+CU group showed less negative reactivity (i.e., exhibited smaller increases in negative affect) to the still face than either non-ODD or ODD-only groups (Cohen ds=−.56 and −.32, respectively). Moreover, as infants, children in the ODD-only group exhibited poorer recovery (i.e., exhibited continued increasing negative affect) during the reunion period than children in either the non-ODD or ODD+CU groups (Cohen ds=|.50 and .38|, respectively). Although not expected, as infants, the ODD+CU group was also unique in showing greater recovery (i.e., exhibited greater increases) in positive affect during the reunion period than either non-ODD or ODD-only groups (Cohen ds=.58 and 1.04, respectively).
Fig. 1.
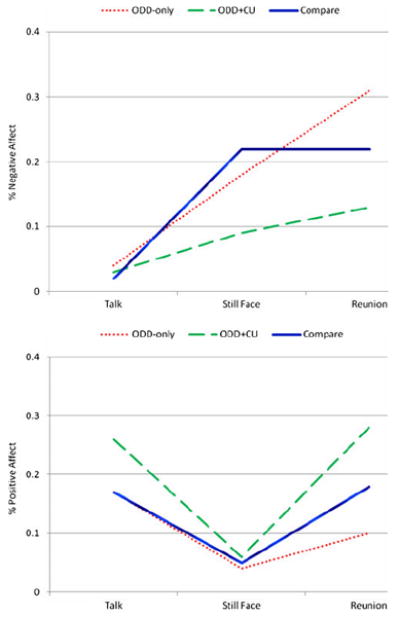
Observed affect during the face to face still face procedure at the 6-month visit
Third, as infants, the ODD-only group exhibited greater heart period reactivity (Cohen d=|.72 and .52|, respectively) and recovery (Cohen d=|.62 and .42|, respectively) during the still face procedure relative to both non-ODD and ODD+CU youth. As depicted in Fig. 2, children in the ODD+CU group exhibited the lowest levels heart period across all three phases of the FFSFP, which was indicative of a higher level of general arousal. Because heart period data were aggregated across 3- and 6-month visits, this information is not directly comparable to the affect data that was described above, which was only coded at the 6-month visit.
Fig. 2.
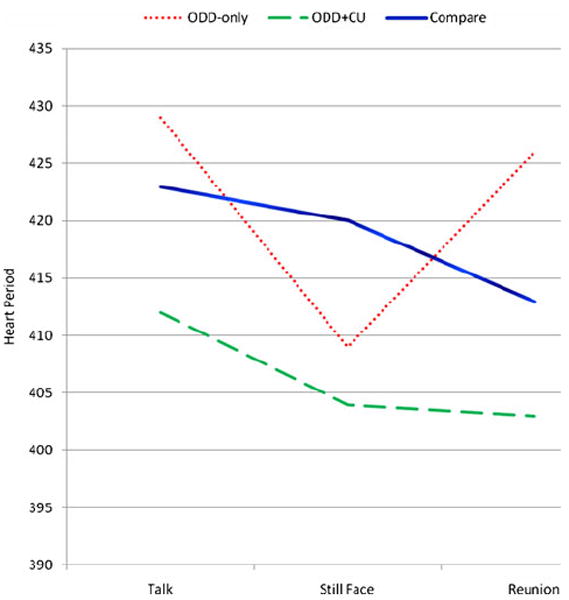
Observed heart period during the face to face still face procedure aggregated across 3- and 6-month visits
Discriminant Function Analysis (DFA) was used to test whether infant temperament measures could reliably predict membership in ODD+CU, ODD-only, and non-ODD groups at 36-months. Because DFA required that the number of predictors be less than the number of observations in the smallest sized group, only six of the variables in Table 3 were included.2 We included one parent report (IBQ soothability), three measures of observed affect during the FFSFP (negative reactivity and recovery; positive recovery), and two heart rate measures (normal talk, reactivity). Measures were selected based on the magnitude of group differences (per Table 3), as well as to reflect multiple dimensions of functioning (behavior, physiology) and informants (parent, observers).
Taken together, there was a significant overall multivariate effect for these variables in the prediction of group status, Wilks’ λ=0.46, F (12, 58)=2.29, p=.02. The canonical correlations between the first and second discriminant functions with group membership were .60 and .53, respectively, indicating that the first and second functions explained 36% and 28% of the relationship between infancy predictors and group membership. The first discriminant function (p=.02), which was defined primarily by the two heart period measures (normal talk, reactivity) and positive affect recovery, primarily differentiated the ODD-only from ODD+CU and non-ODD groups. The second discriminant function (p=.07), which was defined primarily by IBQ soothability, baseline heart period, and positive affect recovery, differentiated the ODD+CU group from the ODD-only and especially the non-ODD groups. The set of six infancy variables correctly classified 84% of children into ODD+CU (7/7; 100% accuracy), ODD-only (10/12; 83% accuracy), and non-ODD (14/18; 78% accuracy) groups at age 36 months.
Discussion
It has long been known that children with elevated conduct problems are heterogeneous with respect to their etiologies, risk factors, developmental outcomes, and possibly treatment response. There is growing interest in using callous unemotional traits to reduce this heterogeneity. It is for this reason that CU is being considered as a modifier for diagnoses of conduct disorder in DSM-V (Frick and Moffitt 2010). Despite a burgeoning research literature on CU in middle childhood and adolescent samples, relatively little is known about CU traits in early childhood, despite the fact that this is the developmental period in which individual differences in empathy and guilt are first evident. The primary goal of this study was to introduce a five-item screening measure of CU for use in early childhood that is drawn directly from the preschool version of the ASEBA. The availability of a CU screener, especially one derived from an instrument that is widely used, has the potential to stimulate new and secondary data analyses involving CU in early childhood, thereby attending to an important gap in the research literature.
Consistent with results involving older children, parents were able to differentiate CU from two commonly measured dimensions of disruptive behavior in early childhood, ODD and ADHD. Moreover, the measurement properties of CU items were very similar to those of ODD and ADHD items. That is, the factor loadings and item level R2 values of CU items were comparable to that of ODD and ADHD items. Given the widespread use of 5-item screening measures for disruptive behaviors (e.g., SDQ; IOWA Conners), our results suggest that expanding screens to include CU behaviors may be useful. Moreover, it is noteworthy that one of the most widely used measures of psychopathy in older children and adolescents (i.e., the Antisocial Process Screening Device) is limited to a seven item scale for CU (Frick and Hare 2002).
Due to rapidly increasing self regulatory abilities, early childhood is a developmental period characterized by marked improvement in disruptive behaviors. This may lead to questions about whether individual differences in CU behaviors assessed at a single point in time are sufficiently stable for study. Longitudinal analyses demonstrated that CU behaviors were at least as stable as ODD and ADHD behaviors measured using a similar format across the same time span. Although high levels of stability do not undermine the possibility of substantial mean level change, high stability estimates indicate that the rank ordering of individual differences is preserved over time. To the extent that researchers routinely measure ODD and ADHD during early childhood, there is no reason to believe that, on the basis of the stability of individual differences, that they cannot do so for CU too.
Despite the fact that CU behaviors were differentiated from ODD and ADHD behaviors and were stable over time, the latent correlations between factors were large. Large correlations between CU, ODD, and ADHD raise questions about the utility of measuring CU in early childhood. To address this concern, we tested whether children who had elevated ODD at 36 months but who differed with respect to their CU exhibited unique temperamental profiles. Children in the ODD-only group were characterized by both parents and observers as having difficulty regulating negative affect after becoming upset during infancy. By contrast, children in the ODD+CU group were observed to become less upset (both behaviorally and in terms of cardiac response) to the FFSFP and were reported to be the least responsive to parent efforts to sooth them when upset. These results are consistent with Frick and Morris’ (2004) hypotheses regarding low fear and emotionally dysregulated pathways into conduct problems.
The primary motivation for this work is to encourage more widespread study of CU in early childhood. Because CU is a relatively new construct, most existing data sets have not routinely included a CU-specific measure, raising a barrier to research in this area. The availability of a screening measure of CU, particularly one that is available in many extant datasets that utilize the ASEBA, may overcome this barrier and facilitate this work. Nonetheless, we do not intend to suggest that screening measures of CU are sufficient for developing a robust body of research on CU in early childhood. Clearly, more detailed measures of CU are necessary and appropriate. For example, Frick and colleagues recently developed the Inventory of Callous Unemotional traits, which is a 24-item rating scale, in order to overcome concerns about the low reliability of the 7-item CU scale on the Antisocial Process Screening Device (Kimonis et al. 2008). Moreover, as evidence continues to emerge regarding the central role of the amygdala as a neural substrate that underlies CU (Blair 2007), it will be equally important for studies to incorporate lab based tasks that are sensitive to amygdala functions (e.g., emotion processing tasks) into their assessments. Additionally, studies that begin in infancy and toddlerhood will also benefit from direct assessments of early temperament, including tasks that pull for individual differences in fearlessness (Kagan 2010; Rothbart 2004). Nonetheless, given the paucity of information about CU in early childhood, all efforts directed toward this goal will be informative. Given the early stage of research in this area, secondary analyses of collected data may be especially helpful in that they hold the potential to increase knowledge quickly and efficiently.
This study is characterized by three limitations. First, some of the items in the CU screener are not specific to CU and, when considered alone, may be equally indicative of other disorders (e.g., shows little affection may be characteristic of the autism spectrum of behaviors). Second, this study is based on a small and normative sample of participants. For purposes of grouping, it was not possible to locate any children who had elevated CU with low ODD (i.e., a CU-only group). The small number of children who were characterized by both elevated ODD and CU also constrained the number of variables that could be used infancy for purposes of prediction. These issues can be addressed by future studies that seek to replicate this work using larger samples of young children. Third, substantively, we would be remiss in not pointing out that although ODD+ CU, ODD-only, and non-ODD children exhibited temperamental profiles that were consistent with Frick and Morris’ (2004) hypotheses, as infants, children in the ODD+CU group were observed to be more highly physiologically aroused during all phases of the FFSFP than were children in the ODD-only or non-ODD groups. This is inconsistent with the low fear pathway, which would predict hypo- not hyper-arousal. Given that no previous study has reported differences in cardiac functioning in infancy among children subsequently characterized by both elevated ODD and CU, the interpretation of this result is ambiguous. It may undermine the low fear pathway hypothesis. Alternatively, it may point to a developmental hypothesis regarding the role of arousal in children following the low fear pathway (e.g., these children may start life being hyper-aroused but may down regulate this arousal, towards an eventual hypoaroused state, in order to deal with early harsh and/or non-contingent experiences).
This study provided initial evidence for the factor structure, stability, and utility of measuring CU traits using a 5-item screening measure that was derived from the preschool ASEBA. There is a long precedent in behavioral research for using screening measures of multiple dimensions of disruptive behaviors disorders, including with young children. The results of this study suggest that researchers may benefit from the similar utilization of screening measures for CU. This has the potential to facilitate much needed work involving CU in early childhood. Attending to heterogeneity within groups of children with early onset conduct problems has the potential to greatly improve causal models of disruptive behavior disorders, as well as to facilitate the routine implementation of treatments that are tailored to the behavioral, cognitive and/or physiological profiles of individual children.
Acknowledgments
This study was supported by The North Carolina Child Development Research Collaborative, which is funded by the National Science Foundation through a Children’s Research Initiative grant #BCS-0126475. The authors would like to thank all of the parents who participated in the Durham Child Health and Development Study and the research assistants for their valuable help in collecting these data.
Footnotes
The reduction in participants reflected a ‘gap’ period in funding for the study.
In order to ensure that all cases were included for prediction, group mean substitution was used to address the very low rates of missing data (i.e., one child in the ODD+CU group had missing values on FFSFP affect; three children in the ODD-only had missing cardiac data; three children in the non-ODD group had missing cardiac data and five had missing FFSFP affect).
Contributor Information
Michael T. Willoughby, FPG Child Development Institute, University of North Carolina at Chapel Hill, Campus Box 8185, 521 South Greensboro Street, Carrboro, NC 27510, USA, willoughby@unc.edu
Daniel A. Waschbusch, Department of Psychology, Florida International University, Miami, FL, USA
Ginger A. Moore, Department of Psychology, Pennsylvania State University, University Park, PA, USA
Cathi B. Propper, Center for Developmental Science, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
References
- Achenbach TM, Rescorla LA. Manual for the aseba preschool forms and profiles: An integrated system of multi-informant assessment. Burlington: University of Vermont Department of Psychiatry; 2000. [Google Scholar]
- Adamson LB, Frick JE. The still face: a history of a shared experimental paradigm. Infancy. 2003;4(4):451–473. [Google Scholar]
- Alink LRA, Mesman J, van Zeijl J, Stolk MN, Juffer F, Koot HM, et al. The early childhood aggression curve: development of physical aggression in 10-to 50-month-old children. Child Development. 2006;77(4):954–966. doi: 10.1111/j.1467-8624.2006.00912.x. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and statistical manual of mental disorders fourth edition-text revision (DSM-IV-TR) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Bar-Haim Y, Marshall PJ, Fox NA. Developmental changes in heart period and high-frequency heart period variability from 4 months to 4 years of age. Developmental Psychobiology. 2000;37(1):44–56. doi: 10.1002/1098-2302(200007)37:1<44::aid-dev6>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Bates JE, Pettit GS, Dodge KA, Ridge B. Interaction of temperamental resistance to control and restrictive parenting in the development of externalizing behavior. Developmental Psychology. 1998;34(5):982–995. doi: 10.1037//0012-1649.34.5.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair RJR. The amygdala and ventromedial prefrontal cortex in morality and psychopathy. Trends in Cognitive Sciences. 2007;11(9):387–392. doi: 10.1016/j.tics.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Blair RJR, Peschardt KS, Budhani S, Mitchell DGV, Pine DS. The development of psychopathy. Journal of Child Psychology and Psychiatry. 2006;47(3-4):262–276. doi: 10.1111/j.1469-7610.2006.01596.x. [DOI] [PubMed] [Google Scholar]
- Christian RE, Frick PJ, Hill NL, Tyler L, Frazer DR. Psychopathy and conduct problems in children.2. Implications for subtyping children with conduct problems. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(2):233–241. doi: 10.1097/00004583-199702000-00014. [DOI] [PubMed] [Google Scholar]
- Cornell AH, Frick PJ. The moderating effects of parenting styles in the association between behavioral inhibition and parent-reported guilt and empathy in preschool children. Journal of Clinical Child and Adolescent Psychology. 2007;36(3):305–318. doi: 10.1080/15374410701444181. [DOI] [PubMed] [Google Scholar]
- Cote SM, Vaillancourt T, LeBlanc JC, Nagin DS, Tremblay RE. The development of physical aggression from toddlerhood to pre-adolescence: a nation wide longitudinal study of canadian children. Journal of Abnormal Child Psychology. 2006;34(1):71–85. doi: 10.1007/s10802-005-9001-z. [DOI] [PubMed] [Google Scholar]
- Dadds M, Salmon K. Punishment insensitivity and parenting: temperament and learning as interacting risks for antisocial behavior. Clinical Child and Family Psychology Review. 2003;6:69–86. doi: 10.1023/a:1023762009877. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Fraser J, Frost A, Hawes DJ. Disentangling the underlying dimensions of psychopathy and conduct problems in childhood: a community study. Journal of Consulting and Clinical Psychology. 2005;73(3):400–410. doi: 10.1037/0022-006X.73.3.400. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Hawes DJ, Frost AD, Vassallo S, Bunn P, Hunter K, et al. Learning to ‘talk the talk’: the relationship of psychopathic traits to deficits in empathy across childhood. Journal of Child Psychology and Psychiatry. 2009;50(5):599–606. doi: 10.1111/j.1469-7610.2008.02058.x. [DOI] [PubMed] [Google Scholar]
- Frick PJ. Extending the construct of psychopathy to youth: implications for understanding, diagnosing, and treating antisocial children and adolescents. Canadian Journal of Psychiatry-Revue Canadienne De Psychiatrie. 2009;54(12):803–812. doi: 10.1177/070674370905401203. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Hare RD. Antisocial process screening device. Toronto: Multi-Health Systems; 2002. [Google Scholar]
- Frick PJ, Moffitt TE. A proposal to the DSM-V childhood disorders and the ADHD and disruptive behavior disorders work groups to include a specifier to the diagnosis of conduct disorder based on the presence of callous-unemotional traits. Washington, DC: American Psychiatric Association; 2010. [Google Scholar]
- Frick PJ, Morris AS. Temperament and developmental pathways to conduct problems. Journal of Clinical Child and Adolescent Psychology. 2004;33(1):54–68. doi: 10.1207/S15374424JCCP3301_6. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Viding E. Antisocial behavior from a developmental psychopathology perspective. Development and Psychopathology. 2009;21(4):1111–1131. doi: 10.1017/S0954579409990071. [DOI] [PubMed] [Google Scholar]
- Frick PJ, White SF. Research review: the importance of callous-unemotional traits for developmental models of aggressive and antisocial behavior. Journal of Child Psychology and Psychiatry. 2008;49(4):359–375. doi: 10.1111/j.1469-7610.2007.01862.x. [DOI] [PubMed] [Google Scholar]
- Frick P, Bodin S, Barry C. Psychopathic traits and conduct problems in communicty and clinic-referred samples of children: further development of the psychopathy screening device. Psychological Assessment. 2000;12:382–393. [PubMed] [Google Scholar]
- Gao Y, Raine A, Venables PH, Dawson ME, Mednick SA. Reduced electrodermal fear conditioning from ages 3 to 8 years is associated with aggressive behavior at age 8 years. Journal of Child Psychology and Psychiatry. 2010a;51(5):550–558. doi: 10.1111/j.1469-7610.2009.02176.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Y, Raine A, Venables PH, Dawson ME, Mednick SA. Association of poor childhood fear conditioning and adult crime. The American Journal of Psychiatry. 2010b;167(1):56–60. doi: 10.1176/appi.ajp.2009.09040499. [DOI] [PubMed] [Google Scholar]
- Gartstein M, Rothbart MK. Studying infant temperament via the revised infant behavior questionnaire. Infant Behavior & Development. 2003;26:64–86. [Google Scholar]
- Gilliom M, Shaw D. Codevelopment of externalizing and internalizing problems in early childhood. Development and Psychopathology. 2004;16:313–333. doi: 10.1017/s0954579404044530. [DOI] [PubMed] [Google Scholar]
- Glenn AL, Raine A, Venables PH, Mednick SA. Early temperamental and psychophysiological precursors of adult psychopathic personality. Journal of Abnormal Psychology. 2007;116(3):508–518. doi: 10.1037/0021-843X.116.3.508. [DOI] [PubMed] [Google Scholar]
- Goodman A, Goodman R. Strengths and difficulties questionnaire as a dimensional measure of child mental health. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(4):400–403. doi: 10.1097/CHI.0b013e3181985068. [DOI] [PubMed] [Google Scholar]
- Goodman R, Scott S. Comparing the strengths and difficulties questionnaire and the child behavior checklist: is small beautiful? Journal of Abnormal Child Psychology. 1999;27(1):17–24. doi: 10.1023/a:1022658222914. [DOI] [PubMed] [Google Scholar]
- Goodman R, Ford R, Simmons H, Gatward R, Meltzer H. Using the strength and difficulties questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. The British Journal of Psychiatry. 2000;177:534–539. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- Goodman R, Ford T, Corbin T, Meltzer H. Using the strengths and difficulties questionnaire (SDQ) multi-informant algorithm to screen looked-after children for psychiatric disorders. European Child & Adolescent Psychiatry. 2004;13:25–31. doi: 10.1007/s00787-004-2005-3. [DOI] [PubMed] [Google Scholar]
- Graham JM. Congeneric and (essentially) tau-equivalent estimates of score reliability—what they are and how to use them. Educational and Psychological Measurement. 2006;66(6):930–944. [Google Scholar]
- Hawes DJ, Dadds MR. The treatment of conduct problems in children with callous-unemotional traits. Journal of Consulting and Clinical Psychology. 2005;73(4):737–741. doi: 10.1037/0022-006X.73.4.737. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker D, Biederman J, Faraone S, Violette H, Wrightsman J, Rosenbaum J. Temperamental correlates of disruptive behavior disorders in young children: preliminary finding. Biological Psychiatry. 2002;50:563–574. doi: 10.1016/s0006-3223(01)01299-9. [DOI] [PubMed] [Google Scholar]
- Kagan J. The temperamental thread: How genes, culture, time, and luck make us who we are. Dana Foundation; 2010. [Google Scholar]
- Kimonis ER, Frick PJ, Boris NW, Smyke AT, Cornell AH, Farrell JM, et al. Callous-unemotional features, behavioral inhibition, and parenting: independent predictors of aggression in a high-risk preschool sample. Journal of Child and Family Studies. 2006;15:745–756. [Google Scholar]
- Kimonis ER, Frick PJ, Skeem JL, Marsee MA, Cruise K, Munoz LC, et al. Assessing callous-unemotional traits in adolescent offenders: validation of the inventory of callousunemotional traits. International Journal of Law and Psychiatry. 2008;31(3):241–252. doi: 10.1016/j.ijlp.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Kochanska G, Barry RA, Jimenez NB, Hollatz AL, Woodard J. Guilt and effortful control: two mechanisms that prevent disruptive developmental trajectories. Journal of Personality and Social Psychology. 2009;97(2):322–333. doi: 10.1037/a0015471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolko DJ, Dorn LD, Bukstein OG, Pardini D, Holden EA, Hart J. Community vs. clinic-based modular treatment of children with early-onset ODD or CD: a clinical trial with 3-year follow-up. Journal of Abnormal Child Psychology. 2009;37(5):591–609. doi: 10.1007/s10802-009-9303-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotler JS, McMahon RJ. Child psychopathy: theories, measurement, and relations with the development and persistence of conduct problems. Clinical Child and Family Psychology Review. 2005;8(4):291–325. doi: 10.1007/s10567-005-8810-5. [DOI] [PubMed] [Google Scholar]
- Luby J, Belden A, Sullivan J, Hayen R, McCadney A, Spitznagel E. Shame and guilt in preschool depression: evidence for elevations in self-conscious emotions in depression as early as age 3. Journal of Child Psychology and Psychiatry. 2009;50(9):1156–1166. doi: 10.1111/j.1469-7610.2009.02077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore GA, Hill-Soderlund AL, Propper CB, Calkins SD, Mills-Koonce WR, Cox MJ. Mother-infant vagal regulation in the face-to-face still-face paradigm is moderated by maternal sensitivity. Child Development. 2009;80(1):209–223. doi: 10.1111/j.1467-8624.2008.01255.x. [DOI] [PubMed] [Google Scholar]
- Murrie DC, Cornell DG. Psychopathy screening of incarcerated juveniles: a comparison of measures. Psychological Assessment. 2002;14(4):390–396. [PubMed] [Google Scholar]
- Muthén B, Muthén L. Mplus user’s guide. 5. Los Angeles: Muthén and Muthén; 1998–2008. [Google Scholar]
- Pardini D, Obradovic J, Loeber R. Interpersonal callousness, hyperactivity/impulsivity, inattention, and conduct problems as precursors to delinquency persistence in boys: a comparison of three grade-based cohorts. Journal of Clinical Child and Adolescent Psychology. 2006;35(1):46–59. doi: 10.1207/s15374424jccp3501_5. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Hoza B, Pillow DR, Gnagy EM, Kipp HL, Greiner AR, et al. Effects of methylphenidate and expectancy on children with ADHD: behavior, academic performance, and attributions in a summer treatment program and regular classroom settings. Journal of Consulting and Clinical Psychology. 2002;70(2):320–335. [PubMed] [Google Scholar]
- Porges SW. Method and apparatus for evaluating rhythmic oscillations in a periodic physiological response system. 4,510,944. Washington, DC: U.S. Patent and Trademark Office; U.S. Patent. 1985
- Raine A, Reynolds C, Venables PH, Mednick SA, Farrington DP. Fearlessness, stimulation-seeking, and large body size at age 3 years as early predispositions to childhood aggression at age 11 years. Archives of General Psychiatry. 1998;55(8):745–751. doi: 10.1001/archpsyc.55.8.745. [DOI] [PubMed] [Google Scholar]
- Raykov T. Scale reliability, Cronbach’s coefficient alpha, and violations of essential tau-equivalence with fixed congeneric components. Multivariate Behavioral Research. 1997;32(4):329–353. doi: 10.1207/s15327906mbr3204_2. [DOI] [PubMed] [Google Scholar]
- Remschmidt H, Hoare P, Ettrich C, Rothenberger A, Santosh P, Schmidt M, et al. Symptom control in children and adolescents with attention-deficit/hyperactivity disorder on switching from immediate-release mph to oros (r) mph—results of a 3-week open-label study. European Child & Adolescent Psychiatry. 2005;14(6):297–304. doi: 10.1007/s00787-005-0467-6. [DOI] [PubMed] [Google Scholar]
- Rothbart MK. Commentary: differentiated measures of temperament and multiple pathways to childhood disorders. Journal of Clinical Child and Adolescent Psychology. 2004;33(1):82–87. doi: 10.1207/S15374424JCCP3301_8. [DOI] [PubMed] [Google Scholar]
- Salekin RT. Treatment of child and adolescent psychopathy: Focusing on change. In: Salekin RT, Lynam D, editors. Handbook of child and adolescent psychopathy. New York: Guilford Press; 2010. pp. 343–372. [Google Scholar]
- Salekin RT, Worley C, Grimes RD. Treatment of psychopathy: a review and brief introduction to the mental model approach for psychopathy. Behavioral Sciences & the Law. 2010;28(2):235–266. doi: 10.1002/bsl.928. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Lacourse E, Nagin DS. Developmental trajectories of conduct problems and hyperactivity from ages 2 to 10. Journal of Child Psychology and Psychiatry. 2005;46(9):931–942. doi: 10.1111/j.1469-7610.2004.00390.x. [DOI] [PubMed] [Google Scholar]
- Tremblay RE, Nagin DS, Seguin JR, Zoccolillo M, Zelazo PD, Boivin M, et al. Physical aggression during early childhood: trajectories and predictors. Pediatrics. 2004;114(1):E43–E50. doi: 10.1542/peds.114.1.e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tronick E, Als H, Adamson L, Wise S, Brazelton TB. Infants response to entrapment between contradictory messages in face-to-face interaction. Journal of the American Academy of Child and Adolescent Psychiatry. 1978;17(1):1–13. doi: 10.1016/s0002-7138(09)62273-1. [DOI] [PubMed] [Google Scholar]
- van Goozen SHM, Fairchild G, Snoek H, Harold GT. The evidence for a neurobiological model of childhood antisocial behavior. Psychological Bulletin. 2007;133(1):149–182. doi: 10.1037/0033-2909.133.1.149. [DOI] [PubMed] [Google Scholar]
- Viding E, Blair RJR, Moffitt TE, Plomin R. Evidence for substantial genetic risk for psychopathy in 7-yearolds. Journal of Child Psychology and Psychiatry. 2005;46(6):592–597. doi: 10.1111/j.1469-7610.2004.00393.x. [DOI] [PubMed] [Google Scholar]
- Waschbusch DA, Carrey NJ, Willoughby MT, King S, Andrade BF. Effects of methylphenidate and behavior modification on the social and academic behavior of children with disruptive behavior disorders: the moderating role of callous/ unemotional traits. Journal of Clinical Child and Adolescent Psychology. 2007;36(4):629–644. doi: 10.1080/15374410701662766. [DOI] [PubMed] [Google Scholar]
- Wilens T, Pelham W, Stein M, Conners CK, Abikoff H, Atkins M, et al. Adhd treatment with once-daily oros methylphenidate: interim 12-month results from a long-term open-label study. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(4):424–433. doi: 10.1097/01.CHI.0000046814.95464.7D. [DOI] [PubMed] [Google Scholar]
- Woodworth M, Waschbusch D. Emotional processing in children with conduct problems and callous/unemotional traits. Child: Care, Health and Development. 2008;34(2):234–244. doi: 10.1111/j.1365-2214.2007.00792.x. [DOI] [PubMed] [Google Scholar]


