Abstract
Background
The specific health benefits of meeting physical activity guidelines are unclear in older adults. We examined the association between meeting, not meeting, or change in status of meeting physical activity guidelines through walking and the 5-year incidence of metabolic syndrome in older adults.
Methods
A total of 1,863 Health, Aging, and Body Composition (Health ABC) Study participants aged 70–79 were followed for 5 years (1997–1998 to 2002–2003). Four walking groups were created based on self-report during years 1 and 6: Sustained low (Year 1, <150 min/week, and year 6, <150 min/week), decreased (year 1, >150 min/week, and year 6, <150 min/week), increased (year 1, <150 min/week, and year 6, >150 min/week), and sustained high (year 1, >150 min/week, and year 6, >150 min/week). Based on the Adult Treatment Panel III (ATP III) panel guidelines, the metabolic syndrome criterion was having three of five factors: Large waist circumference, elevated blood pressure, triglycerides, blood glucose, and low high-density lipoprotein (HDL) levels.
Results
Compared to the sustained low group, the sustained high group had a 39% reduction in odds of incident metabolic syndrome [adjusted odds ratio (OR) = 0.61; 95% confidence interval (CI), 0.40–0.93], and a significantly lower likelihood of developing the number of metabolic syndrome risk factors that the sustained low group developed over 5 years (β = −0.16, P = 0.04).
Conclusions
Meeting or exceeding the physical activity guidelines via walking significantly reduced the odds of incident metabolic syndrome and onset of new metabolic syndrome components in older adults. This protective association was found only in individuals who sustained high levels of walking for physical activity.
Introduction
Metabolic syndrome is a constellation of factors that, when present, substantially increases risk for diabetes mellitus, cardiovascular disease, coronary heart disease, and cardiovascular disease-related deaths.1 The prevalence of metabolic syndrome among adults in the United States is estimated to be 25%; however, prevalence increases with age such that an estimated 40% of adults aged 65 years and older have the condition.2,3 The third Adult Treatment Panel (ATP III) defines metabolic syndrome as having a combination of any three of the following conditions: Large waist circumference, elevated triglycerides, elevated blood pressure, elevated fasting blood glucose, and low high-density lipoprotein (HDL) levels.4
Public health guidelines for weekly physical activity recommend accumulating a minimum of 150 min/week of moderate intensity physical activity (such as brisk walking).5 Meeting these minimal physical activity guidelines is associated with risk reduction for multiple chronic diseases.6,7 Much of the public health information on risk reduction, however, is presented by combining adults and older adults5; literature on risk reduction specific to older adults is scarce, and no longitudinal studies have examined the relationship specifically between adherence to guidelines and incidence of metabolic syndrome. Because walking is the most popular form of physical activity,8 the objective of this study was to examine the association between meeting, not meeting, or change in status of meeting physical activity guidelines through walking and 5-year incidence of metabolic syndrome in older adults.
Methods
Health, Aging, and Body Composition Study
The Health Aging, and Body Composition (Health ABC) Study is a longitudinal, prospective study with the broad objectives of measuring higher functioning older adults to allow examination of health decline and improvement over several years. The study aims include investigation of interrelationships between health conditions, body composition, social and behavioral factors, and functional change.9 Data collection for the present study occurred during the periods 1997–1998 and 2002–2003.
Study population
The Health ABC study cohort consists of 3,075 well-functioning black and white men and women aged 70–79. Eligibility included reporting no difficulties performing activities of daily living (ADL), walking a quarter of a mile, or climbing 10 steps without resting. In addition, all participants were free of a terminal diagnosis and had no intention to move from the area for at least 3 years. White participants were recruited from a random sample of Medicare beneficiaries in the zip codes in and surrounding Pittsburgh, Pennsylvania, and Memphis, Tennessee. Black participants were recruited from all age-eligible residents of the areas in and surrounding Pittsburgh and Memphis. Exclusion criteria were: Self-reported difficulty walking a quarter of a mile, walking up ten steps, or performing ADL at enrollment; terminal illness; and plans to leave the area within 3 years. The University of Pittsburgh and University of Tennessee, Memphis, institutional review boards approved the study, and all participants provided written informed consent prior to participation.
For this analysis, 1,169 participants with metabolic syndrome at year 1, 43 participants with incomplete year 1 metabolic syndrome status data, and 367 participants with missing year 6 walking data were excluded, leaving 1,496 participants for this study.
Determination of metabolic syndrome
Metabolic syndrome was defined as having three or more factors identified by the ATP III.4 These criteria include: Waist circumference of greater than 102 cm for men and 88 cm for women; serum triglyceride level ≥150 mg/dL; serum HDL levels <40 mg/dL for men and 50 mg/dL for women; resting blood pressure ≥130/85; and fasting serum glucose ≥110 mg/dL. Individuals on blood pressure, lipid-lowering, or diabetes medications were considered positive for that particular factor. Waist circumference was measured by trained technicians using a tape measure at the level of the umbilicus directly on the skin. Resting blood pressure was recorded as the average of two measures after 5 min of seated rest. Blood assays for HDL, triglycerides, and serum glucose measures were obtained by venipuncture in the morning after an overnight fast, processed, frozen, and shipped to the Health ABC Core Laboratory for analysis.
Walking groups
Walking information was self-reported and consisted of total time spent walking for physical activity over the past 7 days. Four walking groups were constructed based on current physical activity guidelines. The sustained low group reported walking less than 150 min/week at year 1 and at year 6. The decreased group reported walking a minimum of 150 min/week at year 1 and less than 150 min/week at year 6. The increased group reported walking less than 150 min/week at year 1 and equal to or greater than 150 min/week at year 6. Finally, the sustained high group reported walking a minimum of 150 min/week at both year 1 and year 6.
Covariates
Covariates included year 1 age, sex, race, education, marital status, count of chronic diseases (cerebrovascular disease, lower limb osteoarthritis, pulmonary disease, circulation problems in extremities, and depression), smoking status, and alcohol consumption. Heart disease was considered a separate covariate due to its strong association with metabolic syndrome. Race was dichotomized into black and white. Chronic disease information was collected from self-report, clinic data, and current medication use. Smoking status, alcohol consumption, education, and marital status were self-reported.
Statistical analysis
Group characteristics were examined using univariate procedures. Unadjusted and adjusted stepwise logistic regression models were used to determine odds ratio (OR) and 95% confidence interval (CI), with the sustained low group as the referent group. Stepwise backward elimination was employed for covariates, with a significance level of P < 0.15 as a threshold for retention in adjusted models. Heart disease status was forced into the adjusted model. Linear regression models were used to determine associations between walking group and number of metabolic syndrome factors present at follow up. A P value of less than 0.05 indicated statistical significance. All analyses were conducted using SAS v8.2 software (SAS, Cary, NC) from 2006–2008.
Results
Year 1 characteristics
At year 1, all walking groups had a similar mean age of 74 years (Table 1).The sustained low group had a greater proportion of women (51%) compared to 45%, 38%, and 43% in the decreased, increased, and sustained high groups, respectively. Generally the sustained low and decreased groups had a greater proportion of participants with characteristics associated with poorer health outcomes, such as black race, currently smoking, low education, and more chronic diseases. Approximately 90% of the participants in every walking group had one or two metabolic syndrome conditions; however, more than half of the sustained low and decreased groups had two metabolic syndrome conditions.
Table 1.
Year 1 Characteristics of 1,496 Health ABC Participants, by Walking Group
| Characteristics | Sustained low (n = 933) | Decreased (n = 296) | Increased (n = 112) | Sustained high (n = 155) |
|---|---|---|---|---|
| Age [mean (SD)] | 73.6 (2.9) | 73.8 (3.0) | 73.7 (3.0) | 73.7 (2.6) |
| Female (%) | 51 | 45 | 38 | 43 |
| Demographics | ||||
| Race (%) | ||||
| White | 52 | 65 | 57 | 76 |
| Marital status (%) | ||||
| Married | 55 | 55 | 58 | 54 |
| Smoking status (%) | ||||
| Never | 44 | 41 | 39 | 49 |
| Former | 43 | 48 | 52 | 44 |
| Current | 13 | 11 | 9 | 7 |
| Education (%) | ||||
| Less than HS | 29 | 20 | 21 | 18 |
| HS graduate | 30 | 33 | 32 | 29 |
| Post-secondary | 41 | 47 | 47 | 53 |
| Number of diseases (%) | ||||
| 0 | 64 | 63 | 77 | 76 |
| 1 | 28 | 29 | 20 | 18 |
| 2+ | 8 | 8 | 4 | 6 |
| Number of metabolics syndrome factors (%) | ||||
| 0 | 8 | 10 | 15 | 13 |
| 1 | 36 | 38 | 49 | 46 |
| 2 | 56 | 52 | 36 | 41 |
Abbreviations: Health ABC Study, Health, Aging, and Body Composition Study; SD, standard deviation; HS, high school.
Year 1 and year 6 metabolic syndrome factors
The most prevalent individual metabolic syndrome factor at year 1 in all groups was elevated blood pressure affecting approximately 70% of participants (Table 2).Large abdominal circumference was present in approximately one-third of the decreased, increased, and sustained high groups, but was present in half of the sustained low group. At year 6, the individual factors generally showed a trend of increasing prevalence, particularly with the blood pressure and blood glucose factors. The sustained high had the most favorable panel of individual factors at year 6 compared to the other walking groups.
Table 2.
Metabolic Syndrome Factors Present at Year 1 and Year 6
| Metabolic syndrome factors | Sustained low (n = 933) | Decreased (n = 296) | Increased (n = 112) | Sustained high (n = 155) |
|---|---|---|---|---|
| Year 1 (%) | ||||
| Abd. circ. | 50 | 39 | 35 | 32 |
| HDL | 8 | 11 | 7 | 14 |
| Triglycerides | 9 | 12 | 8 | 9 |
| Blood pressure | 72 | 70 | 67 | 70 |
| Blood glucose | 9 | 10 | 4 | 4 |
| Year 6 (%) | ||||
| Abd. Circ. | 52 | 46 | 46 | 32 |
| HDL | 14 | 15 | 13 | 13 |
| Triglycerides | 14 | 15 | 15 | 13 |
| Blood pressure | 86 | 84 | 86 | 83 |
| Blood glucose | 19 | 14 | 12 | 12 |
Abbreviations: Abd. circ., abdominal circulation; HDL, high-density lipoprotein.
5-Year walking patterns
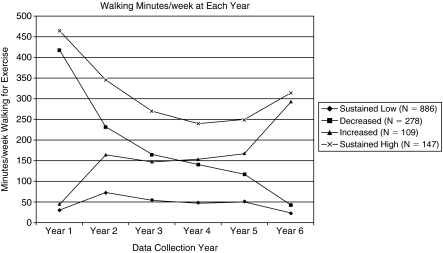
Figure 1 displays the 5-year walking patterns in the four walking groups. Notably, the sustained high group, on average, consistently maintained walking patterns that far exceeded minimal guidelines, with the lowest average of 240 min/week at year 4. The sustained low group was the least variable group from year to year, with minutes/week walked ranging from 23 (year 6) to 73 (year 2). The sustained low group was also the largest of the four walking groups, representing 64% of the cohort. By year 6, the decreased group reported walking, on average, 47 min/week, whereas by year 6 the increased group reported, on average, 293 min/ week of walking. This represents changes from year 1 of −375 and +248 min/week in the decreased and increased groups, respectively.
FIG. 1.
Mean weekly minutes spent walking for physical activity at each year, by walking group.
Walking groups and incident metabolic syndrome/ number of metabolic syndrome factors
Logistic regression models (Table 3)indicated that being in the sustained high group was protective against incident metabolic syndrome (adjusted OR = 0.61; 95% CI, 0.40–0.93), compared to being in the sustained low group. Neither the decreased nor the improved groups showed significant differences in odds of developing metabolic syndrome compared to the sustained low group.
Table 3.
Associations Between Walking Groups and Incident Metabolic Syndrome and Number of Metabolic Syndrome Risk Factors (N = 1,496)
| |
Metabolic syndromea |
Number of metabolic syndrome risk factorsb |
||||
|---|---|---|---|---|---|---|
| |
Model 1c |
Model 2d |
Model 1d |
Model 2e |
||
| Walking group | OR (95% CI) | OR (95% CI) | β | p | β | p |
| Sustained low | 1.00 | 1.00 | 0 | 0 | ||
| Decreased | 0.95 (0.71–1.26) | 0.97 (0.73–1.30) | −0.06 | 0.37 | −0.07 | 0.29 |
| Increased | 1.05 (0.69–1.61) | 1.04 (0.67–1.60) | −0.08 | 0.42 | 0.02 | 0.84 |
| Sustained high | 0.59 (0.38–0.89) | 0.61 (0.40–0.93) | −0.23 | 0.007 | −0.16 | 0.04 |
Estimates derived using logistic regression.
Estimates derived using linear regression.
Adjusted for race, education, number of diagnoses, and heart disease.
Adjusted for year 1 body weight, race, education, number of diagnoses, heart disease, and year 1 min/week in high-intensity exercise.
Adjusted for year 1 body weight, race, education, number of diagnoses, heart disease, baseline min/week in high-intensity exercise, and number of metabolic syndrome factors present at year 1.
Abbreviations: OR, odds ratio; CI, confidence interval.
The sustained high group also demonstrated a significantly lower likelihood of developing the number of metabolic syndrome risk factors that the sustained low group developed over 5 years (β= −0.23, P = 0.007). This significant difference, attenuated slightly, but persisted (β; = −0.16, P = 0.04) after adjustment for number of metabolic syndrome factors present at year 1.
Discussion
In this 5-year prospective study of well-functioning older adults, men and women who reported sustaining weekly walking patterns that met or exceeded current guidelines had a 39% reduced likelihood of incident metabolic syndrome (adjusted OR = 0.61; 95% CI, 0.40–0.93) compared to those who maintained walking patterns that did not meet guidelines. There was also a clear relationship between sustaining recommended weekly physical activity via walking and the number of metabolic syndrome conditions developed over time. This indicates that regular walking is associated with a reduced likelihood of developing additional metabolic syndrome risk factors over time, an important finding considering that approximately 90% of this cohort already had one or two metabolic syndrome risk conditions at year 1.
Our results also indicate that the benefit of meeting minimal physical activity recommendations may be negated if walking patterns are not maintained over time, because the decreased group showed no differences in odds of developing metabolic syndrome compared to the sustained low group (adjusted OR = 0.97; 95% CI, 0.73–1.30). The precipitating factors leading to the decreased group's substantial drop in weekly walking are not known. Previously, we reported that intercurrent illness or new-onset health conditions often precede noncompliance with activity recommendations,10,11 and it is plausible that these factors may have contributed to the decreased group's decline in minutes of walking per week. Future studies are warranted to better understand factors that predict changes in physical activity patterns in older adults.
These findings are consistent with previous studies that examined the association between physical activity and metabolic syndrome in older adults. Wannamethee and colleagues12 examined changes in physical activity patterns over a period of 3 years in 3,051 older men participating in the British Regional Heart Study and found a protective association, compared to habitually inactive men, between sustained physical activity patterns and development of metabolic syndrome (adjusted OR = 0.73; 95% CI, 0.57–0.94). Our findings provide additional support for the protective role of sustaining physical activity in old age, specifically when walking a minimum of 150 min/week for physical activity.
In contrast to our findings, Wannamethee and colleagues found that men who became active had lower odds of metabolic syndrome compared to men who remained inactive (adjusted OR = 0.76; 95% CI, 0.54–1.06). We did not observe similar protective associations with becoming active (adjusted OR = 1.04; 95% CI, 0.67–1.60). This is particularly interesting given that the increased group quickly reached minimal physical activity guidelines at year 2 and maintained minimal guideline walking patterns every subsequent year (Fig. 1). The fact that the Wanamethee study cohort was a younger (60 years and above) and considerably more active cohort (≈50% reported at least regular moderate physical activity) than the Health ABC study cohort is an important consideration. It is plausible that the cumulative burden of aging, disuse, and disease are not offset by initiation of a regular program of walking in the 70+ age group and that a higher volume of physical activity is required to impact metabolic syndrome.
Petrella and colleagues13 reported 10-year changes in individual metabolic syndrome risk factors between 161 regular exercisers and 136 sedentary persons aged 68 ± 6 years. The exercisers maintained 3 days per week of aerobic activities (walking, jogging) for 30–45 min at 75–85% of maximum aerobic capacity. These training zones are of moderate to vigorous intensity,14 and, compared to the sedentary comparison group, exercisers demonstrated improved profiles for all five metabolic syndrome factors. This suggests that in older adults, engaging in exercise activities of moderate to vigorous intensity for 90–135 min/week may be an alternative way for older adults to get an adequate exercise dose for preventing metabolic syndrome. Future studies are needed to confirm whether or not engaging in higher-intensity physical activities for less than 150 min/week produces health outcome benefits equivalent to those obtained by accumulating at least 150 min/week of moderate intensity physical activity.
Most recently, Park and colleagues15 used accelerometry to objectively examine year-long physical activity levels and prevalence of metabolic syndrome in 220 community-dwelling older Japanese men and women. They found the group that reached a minimum of 8,000 steps per day and engaged in activities that attained a level of intensity that was at least moderate for 20–30 min/day were the least likely to have metabolic syndrome. Although these findings were from a cross-sectional study, they add support to findings from our current study and those of Petrella and colleagues.13
The major limitation of this study was measurement of the full complement of metabolic syndrome components at years 1 and 6 only. Because we were not able to determine when incident metabolic syndrome occurred between these two time points, we cannot determine if amount of weekly walking may have been affected by the onset of metabolic syndrome, representing an order of occurrence opposite that assumed in this study. Nevertheless, given that around 75% of participants were in the sustained low or sustained high group, it is unlikely that new onset of a metabolic syndrome component resulted in marked changes in activity level. Use of a self-report measure of walking activity constitutes another possible limitation. Although direct activity measures, such as accelerometers, would provide more accurate data,16 the majority of participants were sedentary. The degree to which persons overreported their walking behavior would result in an underestimate of the true effect. Additionally, walking for physical activity was the only variable collected consistently over time in the Health ABC study. Ideally, we would have been able to measure participation in a number of other activities that may have contributed to meeting physical activity guidelines. We would have also preferred to control for dietary habits; however, these data were not completely available. We did have a year 2 dietary summary score available on about 90% of the cohort,17 and, when this variable was included in the models (not reported), there was no statistical impact on the estimates reported above.
It has been over a decade since the Surgeon General's guidelines for physical activity were published, and these guidelines remain near the forefront of public health efforts with newly published guidelines maintaining a minimum of 150 min/week in physical activity.5,18 We are just now starting to see research on the impact of meeting guidelines on health outcomes.19 Our findings add support to the guidelines, in that maintaining or exceeding the minimal physical activity guidelines of 150 min/week via walking is effective in significantly reducing the likelihood of developing metabolic syndrome in older adults. We also found some evidence that the protective role of meeting physical activity guidelines is only sustained with long-term maintenance of these healthy lifestyle habits. To our knowledge, this is the first study to establish an association between meeting current public health physical activity recommendations and decreased likelihood of metabolic syndrome in older adults.
Acknowledgements
This research was supported in part by the Intramural Research program of the National Institutes of Health (NIH), National Institute of Aging, contracts N01-AG-6-2101, N01-AG-6-2103, N01-AG-6-2106, and AG-028716.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ford E. Giles W. Dietz W. Prevalence of the metabolic syndrome among U.S. adults: Findings from the third national health and nutrition examination survey. JAMA. 2002;287:356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 2.Park Y. Zhu S. Palaniappan L. Heshka S. Carnethon M. Heymsfield S. The metabolic syndrome: Prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2003;63:427–436. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scuteri A. Morrell C. Najjar S. Lakatta E. The metabolic syndrome in older individuals: Prevalence and prediction of cardiovascular events. Diabetes Care. 2005;28:882–887. doi: 10.2337/diacare.28.4.882. [DOI] [PubMed] [Google Scholar]
- 4.The Expert Panel on Detection Evaluation, Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. Washington (DC): U.S. Department of Health and Human Services; 2008. 2008. [Google Scholar]
- 6.Blair S. Lamonte M. Nichaman M. The evolution of physical activity recommendations: how much is enough? Am J Clin Nutr. 2004;79:913S–920S. doi: 10.1093/ajcn/79.5.913S. [DOI] [PubMed] [Google Scholar]
- 7.Pate R. Pratt M. Blair S. Haskell WL. Macera CA. Bouchard C. Buchner D. Ettinger W. Heath GW. King AC, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 8.Eyler A. Brownson R. Bacak S. Housemann R. The epidemiology of walking for physical activity in the United States. Med Sci Sports Exerc. 2003;35:1529–1536. doi: 10.1249/01.MSS.0000084622.39122.0C. [DOI] [PubMed] [Google Scholar]
- 9.Simonsick E. Newman A. Nevitt M. Kritchevsky SB. Ferrucci L. Guralnik JM. Harris T. Health ABC Study Group. Measuring higher level physical function in well-functioning older adults: Expanding familiar approaches in the health ABC study. J Gerontol A Biol Sci Med Sci. 2001;56A:M644–M649. doi: 10.1093/gerona/56.10.m644. [DOI] [PubMed] [Google Scholar]
- 10.Cowper P. Morey M. Bearon L. Sullivan R. DiPasquale R. Crowley G. Feussner J. The impact of supervised exercise on psychological well-being and health status in older veterans. J Appl Gerontol. 1991;10:469–485. doi: 10.1177/073346489101000408. [DOI] [PubMed] [Google Scholar]
- 11.Morey M. Sloane R. Ekelund C, et al. Impact of intercurrent illness on functional outcomes in a clinical trial to improve elder fitness. Med Sci Sports Exerc. 2005;37(5 Suppl):S338. [Google Scholar]
- 12.Wannamethee S. Shaper A. Whincup P. Modifiable lifestyle factors and the metabolic syndrome in older men: Effects of lifestyle changes. JAm Geriatr Soc. 2006;54:1909–1914. doi: 10.1111/j.1532-5415.2006.00974.x. [DOI] [PubMed] [Google Scholar]
- 13.Petrella R. Varallo V. Lattanzio C. Blore R. Demeray A. Can adoption of regular exercise later in life prevent metabolic risk for cardiovascular disease? Diabetes Care. 2005;28:694–701. doi: 10.2337/diacare.28.3.694. [DOI] [PubMed] [Google Scholar]
- 14.American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. 6th. Baltimore (Maryland): Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 15.Park S. Park H. Togo F. Watanabe E. Yasunaga A. Yoshiuchi K. Shephard RJ. Aoyagi Y. Year-long physical activity and metabolic syndrome in older Japanese adults: Cross-sectional data from the Nakanojo Study. J Gerontol A Biol Sci Med Sci. 2008;63A:1119–1123. doi: 10.1093/gerona/63.10.1119. [DOI] [PubMed] [Google Scholar]
- 16.Bassett D. Validity and reliability issues in objective monitoring of physical activity. Res Q Exerc Sport. 2000;71:S30–S36. [PubMed] [Google Scholar]
- 17.Koster A. Penninx B. Newman A. Visser M. van Gool CH. Harris TB. van Eijk JT. Kempen GI. Brach JS. Simonsick EM. Houston DK. Tylavsky FA. Rubin SM. Kritchevsky SB. Lifestyle factors and incident mobility limitation in obese and non-obese older adults. Obesity. 2007;15:3122–3132. doi: 10.1038/oby.2007.372. [DOI] [PubMed] [Google Scholar]
- 18.Nelson M. Rejeski W. Blair S. Duncan PW. Judge JO. King AC. Macera CA. Casteneda-Sceppa C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 19.Church T. Earnest C. Skinner J. Blair S. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: A randomized controlled trial. JAMA. 2007;297:2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]