Abstract
Objectives
We undertook a meta-analysis to assess outcomes for drug-eluting (DES) and bare metal stents (BMS) in percutaneous coronary intervention (PCI) for unprotected left main coronary stenosis (LMCA).
Background
Uncertainty exits regarding the relative performance of DES versus BMS in unprotected LMCA PCI.
Methods
Of a total of 838 studies, 44 met inclusion criteria (N=10,342). The co-primary endpoints were mortality, myocardial infarction (MI), target vessel/target lesion revascularization (TVR/TLR), and major adverse cardiac events (MACE: mortality, MI, TVR/TLR).
Results
Event rates for DES and BMS were calculated at 6–12 months, at 2 years and at 3 years. Crude event rates at 3 years were: mortality (8.8% and 12.7%), MI (4.0% and 3.4%), TVR/TLR (8.0% and 16.4%), and MACE (21.4% and 31.6%). Nine studies were included in a comparative analysis (N=5,081). At 6–12 months the adjusted odds ratio (OR) for DES vs. BMS were: mortality 0.94 (95% confidence interval [CI] 0.06–15.48; p=0.97), MI 0.64 (95% CI 0.19–2.17; p=0.47), TVR/TLR 0.10 (95% CI 0.01–0.84; p=0.01) and MACE 0.34 (95% CI 0.15–0.78; p=0.01). At 2 years the OR were: mortality 0.42 (95% CI 0.28–0.62; p<0.01), MI 0.16 (95% CI 0.01–3.53; p=0.13), and MACE 0.31 (95% CI 0.15–0.66; p<0.01). At 3 years the OR were: mortality 0.70 (95% CI 0.53–0.92; p=0.01), MI 0.49 (95% CI 0.26–0.92; p=0.03), TVR/TLR 0.46 (95% CI 0.30–0.69; p<0.01), and MACE 0.78 (95% CI 0.57–1.07; p=0.12).
Conclusion
Our meta-analysis suggests that DES is associated with favorable outcomes for mortality, MI, TVR/TLR, and MACE as compared to BMS in unprotected LMCA PCI.
Introduction
Unprotected left main coronary artery stenosis (LMCA) is associated with poor clinical outcomes. Studies have shown improved long-term outcomes in those who undergo surgical revascularization as compared to optimal medical therapy alone (1,2). This is the basis for the ACC/AHA class I recommendation for coronary artery bypass surgery (CABG) in patients with ≥ 50% left main stenosis (3).
Early percutaneous attempts at revascularization with balloon-only angioplasty were associated with suboptimal clinical outcomes (4). This led to an ACC/AHA class III (contraindicated) guidelines recommendation for percutaneous coronary intervention (PCI) in CABG-eligible patients (5). The subsequent advent of coronary stents, which reduced peri-procedural risks and improved clinical outcomes, renewed interest in unprotected LMCA PCI. This interest was further fueled by the subsequent introduction of drug-eluting stents (DES), which led to substantially lower rates of restenosis in coronary lesions (6,7). On the basis of improved clinical outcomes, the most recent ACC/AHA guidelines have given unprotected LMCA PCI a class IIb recommendation (8).
However, there remains some clinical uncertainty over the ideal stent type for unprotected LMCA PCI. The use of DES in the left main position is considered an off-label application; prior studies have identified increased adverse events for such off-label applications (9). Additionally, although the reduction in restenosis seen with DES use is particularly attractive for unprotected LMCA PCI, the large caliber of most left main arteries could attenuate this benefit. Finally, concern exists over potentially increased rates of late stent thrombosis with DES, which has serious implications in unprotected LMCA PCI (10).
We performed a meta-analysis of the current literature to assess outcomes of PCI in unprotected LMCA and to compare the relative performance of DES and BMS in this application.
Methods
Search strategy
Pubmed, clinicaltrials.gov, and BioMedCentral databases were searched from January 2000 to September 2009; there were no language restrictions. Search terms included “left main”, “coronary”, “intervention”, and “stenting”. Citations were screened and evaluated using the established inclusion/exclusion criteria at the abstract level by two operators (SP and NB), and relevant studies were retrieved as full manuscripts. Inclusion criteria were: a) involving unprotected left main disease, b) involving bare metal or drug eluting stents, and c) involving at least 20 patients in the overall study cohort. Exclusion criteria were defined as: a) unpublished studies, b) abstract only, c) angioplasty without stenting d) ST elevation myocardial infarction, e) cardiogenic shock, f) experimental devices, g) non-English studies, h) studies not reporting relevant clinical outcomes. Data regarding patient demographics and clinical outcomes were then entered into a database.
Endpoints
The co-primary endpoints were mortality, myocardial infarction (MI), target vessel/target lesion revascularization (TVR/TLR), and major adverse cardiovascular events (MACE, defined as mortality, MI, and TVR/TLR). These endpoints were reported for the following time periods post-PCI: 6–12 months, 2 years, and 3 years. Data for all endpoints at each time period were not available for every study.
Statistical analysis
Crude event rates were reported for mortality, MI, and TVR/TLR for both DES and BMS. Since these estimates were based, in part, on studies for which a causal link between stent type and outcome was not established, direct comparison of rates is not appropriate, and rates can only be seen as descriptive in nature. Subsequent comparative analysis was performed evaluating studies that provided adjusted outcomes on relevant endpoints or were randomized according to stent types; odds ratios (OR) were reported for this analysis. When both hazard ratios (HR) and OR were reported as endpoints across trials they were combined, assuming that the follow-up was fairly complete (and thus the HR would be similar to the expected OR). Similarly, Kaplan-Meier rates and percentages were combined when one of the two was not available for an endpoint. Several endpoints did not meet the assumption of homogeneity of rates across studies, and thus random effects modeling techniques were used to combine rates and calculate confidence intervals. Comprehensive Meta Analysis software version 2.2.048 was used for all analyses (Comprehensive Meta Analysis, www.Meta-Analysis.com)(11).
Results
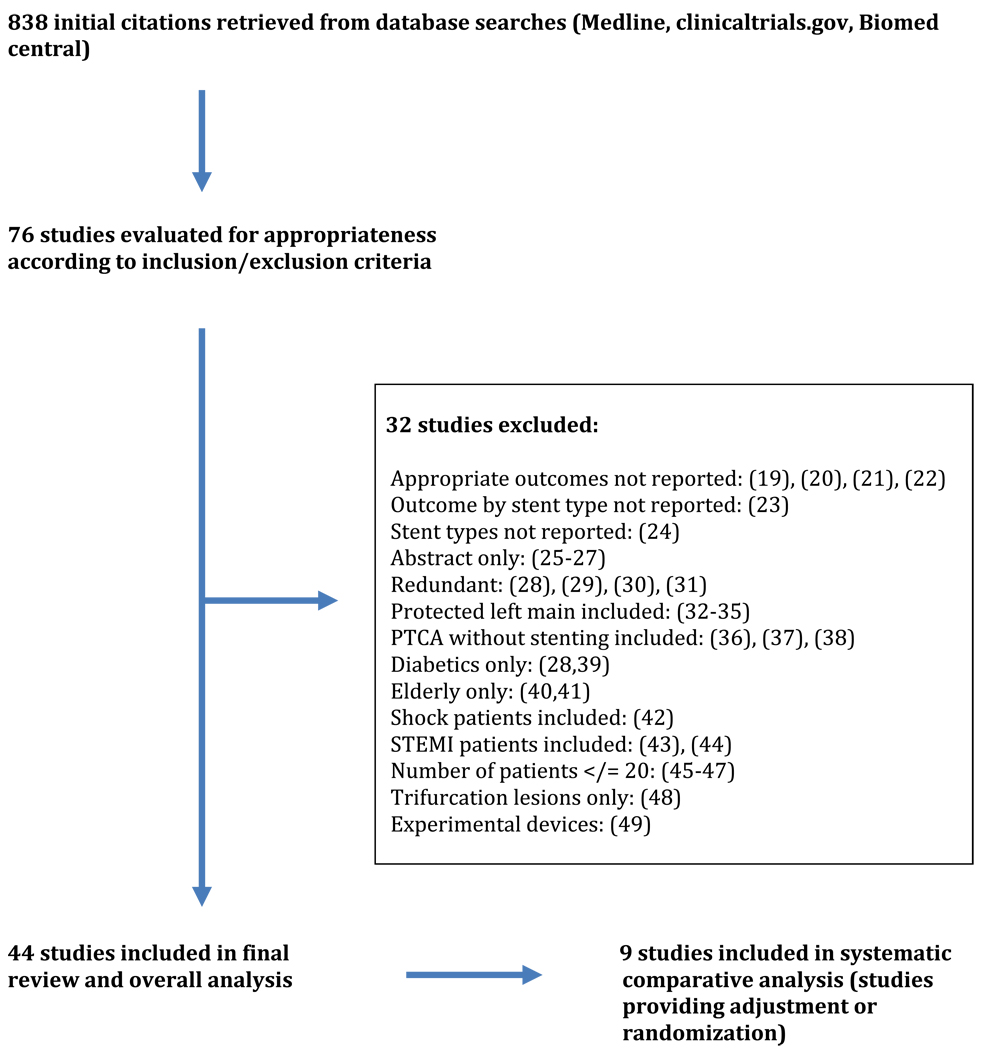
Database searches retrieved an initial 838 studies, of which 76 were deemed relevant; 32 of these studies were eventually excluded. A final 44 studies meeting inclusion/exclusion criteria were included in the analysis, consisting of 10,342 patients (see Figure 1). Studies fell into general categories involving a) use of only BMS, b) use of only DES, c) comparative studies of BMS versus DES, or d) comparison studies of PCI versus CABG (see Table 1).
Figure 1.
Methods
Table 1.
Included studies
| Study | Year | Design | Stent Type |
N | DES (N) |
BMS (N) |
Location | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|
| BMS only studies: 5 | ||||||||
| Black (50) | 2001 | Retrospective Cohort study | BMS | 92 | 0 | 92 | Europe | 7+/−5 |
| Kelley (51) | 2003 | Retrospective cohort study | BMS | 43 | 0 | 43 | US/Europe | 12 |
| Lee BK (52) | 2007 | Propective cohort study | BMS | 187 | 0 | 187 | Asia | 71+/26 |
| Silvestri (53) | 2000 | Prospective cohort study | BMS | 140 | 0 | 140 | Europe | 12 |
| Takagi (54) | 2002 | Prospective cohort study | BMS | 64 | 0 | 64 | Europe | 31+/−23 |
| DES only studies: 21 | ||||||||
| Agostini (55) | 2005 | Retrospective cohort study | DES | 58 | 58 | 0 | Europe | 15 |
| Arampatzis (56) | 2003 | Retrospective cohort study | DES | 31 | 31 | 0 | Europe | 5.1+/−1.8 |
| Chieffo (57) | 2007 | Retrospective cohort study | DES | 147 | 147 | 0 | US/Asia/Europe | 30+/−10 |
| Chieffo (58) | 2008 | Retrospective cohort study | DES | 731 | 731 | 0 | US/Asia/Europe | 29+/−13 |
| Cherradi (59) | 2008 | Prospective cohort study | DES | 101 | 101 | 0 | Europe | 12+/−3 |
| de Lezo(60) | 2004 | Prospective cohort study | DES | 52 | 52 | 0 | Europe | 12 |
| Ge L (61) | 2007 | Retrospective cohort study | DES | 70 | 70 | 0 | Asia/Europe | 12 |
| Khattab (62) | 2007 | Prospective cohort study | DES | 82 | 82 | 0 | Europe | 36 |
| Kim (63) | 2006 | Retrospective cohort study | DES | 116 | 116 | 0 | Asia | 18 |
| Kim (64) | 2008 | Retrospective cohort study | DES | 63 | 63 | 0 | US | 12+/−8 |
| Lee, SH (65) | 2005 | Nonrandomized study (SES vs PES) | DES | 54 | 54 | 0 | Asia | 6 |
| Lozano (66) | 2004 | Prospective cohort study | DES | 42 | 42 | 0 | Europe | 11 |
| Mehilli (67) | 2009 | Randomized controlled trial (SES vs PES) | DES | 607 | 607 | 0 | Europe | 24 |
| Meliga (68) | 2008 | Retrospective cohort study | DES | 358 | 358 | 0 | US/Europe | 36 |
| Migliorini (69) | 2006 | Prospective cohort study | DES | 101 | 101 | 0 | Europe | 10+/−6 |
| Price (70) | 2006 | Prospective cohort study | DES | 50 | 50 | 0 | US | 9 |
| Sanmartin (71) | 2007 | Prospective cohort study | DES | 100 | 100 | 0 | Europe | 12 |
| Sheiban (72) | 2007 | Prospective cohort study | DES | 85 | 85 | 0 | Europe | 20+/−7 |
| Vaquerizo (73) | 2009 | Prospective cohort study | DES | 291 | 291 | 0 | Europe | 24 |
| Vecchio (74) | 2007 | Prospective cohort study | DES | 114 | 114 | 0 | Europe | 17+/−9 |
| Wood (75) | 2008 | Retrospective cohort study | DES | 100 | 100 | 0 | US | 28 |
| BMS and DES studies: 12 | ||||||||
| Cheiffo (76) | 2005 | Nonrandomized study | DES vs BMS | 149 | 85 | 64 | Europe | 6 |
| Erglis (12) | 2007 | Randomized Controlled Trial | DES vs BMS | 103 | 53 | 50 | Australia | 6 |
| Gao (77) | 2008 | Nonrandomized study | DES vs BMS | 424 | 220 | 224 | Asia | 15 |
| Han (78) | 2009 | Nonrandomized study | DES vs BMS | 287 | 178 | 109 | Asia | 35+/−14 |
| Hertting (79) | 2008 | Nonrandomized study | DES vs BMS | 54 | 16 | 38 | Europe | 24 |
| Kim (80) | 2009 | Nonrandomized study | DES vs BMS | 1217 | 864 | 353 | Asia | 36 |
| Palmerini (81) | 2008 | Nonrandomized study | DES vs BMS | 1453 | 1111 | 342 | Europe | 24 |
| Park (63) | 2005 | Nonrandomized study | DES vs BMS | 123 | 102 | 121 | Asia | 12 |
| Schrale (82) | 2008 | Retrospective cohort study | DES and BMS | 100 | 55 | 45 | Europe | 21+/−14 |
| Tamburino (83) | 2009 | Nonrandomized study | DES vs BMS | 849 | 611 | 238 | Europe | 36 |
| Tamburino (84) | 2009 | Nonrandomized study | DES vs BMS | 479 | 334 | 145 | Europe | 36 |
| Wood (85) | 2005 | Nonrandomized study | DES vs BMS | 161 | 61 | 100 | US | 12 |
| PCI/CABG studies: 6 | ||||||||
| Buszman (86) | 2008 | Randomized controlled trial | CABG vs PCI | 52 | 18 | 34 | Europe | 28+/−10 |
| Chieffo (87) | 2006 | Nonrandomized study | CABG vs DES | 107 | 107 | 0 | Europe | 12 |
| Makikallo (88) | 2008 | Nonrandomized study | CABG vs DES | 49 | 49 | 0 | Europe | 12+/−6 |
| Palmerini (89) | 2006 | Nonrandomized study | CABG vs PCI | 157 | 94 | 63 | Europe | 14 |
| Sanmartin (90) | 2007 | Nonrandomized study | CABG vs DES | 96 | 96 | 0 | Europe | 13+/−8 |
| Seung (91) | 2008 | Randomized Controlled Trial | CABG vs PCI | 603 | 396 | 207 | Asia | 34 |
Patient demographics in the group undergoing BMS placement were generally similar to those undergoing DES placement (see Table 2). There was incomplete reporting of baseline demographics across studies. Medication profiles – including duration of antiplatelet drug therapy – were inconsistently reported.
Table 2.
Baseline Patient Demographics for Studies Included in the Overall Analysis
| DES | BMS | |||
|---|---|---|---|---|
| n | n | |||
| Age (years) | 4768 | 67.5 (65.8 – 69.3) | 1621 | 67.8 (66.0 – 69.7) |
| Percent (95% CI) | Percent (95% CI) | |||
| Male | 6464 | 74 (73 – 75) | 2091 | 61 (69 – 73) |
| Diabetes Mellitus (DM) | 6691 | 28 (27 – 29) | 2170 | 22 (20 – 23) |
| Insulin dependent DM | 85 | 11.0 (4.2 – 17.8) | 63 | 8.9 (1.9 – 15.9) |
| Hypertension | 6297 | 65 (64 – 67) | 2032 | 53 (51 – 55) |
| Hypercholesterolemia | 6111 | 57 (57 – 59) | 1892 | 39 (36 – 41) |
| History of Prior MI | 3036 | 23 (21 – 24) | 1165 | 12 (10 – 14) |
| History of PCI | 1912 | 19 (18 – 21) | 794 | 13 (10 – 15) |
| COPD | 1962 | 9.4 (7.9 – 10.9) | 996 | 1.6 (0.8 – 2.4) |
| Renal Insufficiency | 3570 | 7.7 (6.8 – 5.5) | 1241 | 4.5 (3.4 – 5.6) |
| Peripheral Arterial Disease | 1168 | 6.8 (5.5 – 8.2) | 560 | 0.9 (0.03– 1.9) |
n refers to the number of patients within the studies who contributed to the estimate of interest. Rates are the estimated percent of patients with the characteristic, and associated 95% confidence intervals.
Estimates of rates for mortality, MI, and TVR/ TLR at each of the three recorded time points are displayed in Table 3. The rates of events are numerically higher for patients treated with BMS for most endpoints, at most timepoints. However, without adjustment, the significance and/or relevance of the differences noted cannot be fully determined. As expected, the overall rates of events are higher in patients undergoing unprotected LMCA PCI than in conventional PCI patients.
Table 3.
Estimated Cumulative Event Rates by Stent Type in the Overall Analysis
| Stent Type |
6–12 Months | 2 years | 3 years | |
|---|---|---|---|---|
| Mortality | DES |
5.94% (4.73% – 7.44%) n = 2691 |
7.89% (6.07% – 10.20%) n = 4430 |
8.80% (6.20% – 12.34%) n = 2912 |
| BMS |
7.24% (3.51% – 14.33%) n = 763 |
14.14% (8.96% – 21.62%) n = 1266 |
12.71% (6.94% – 22.15%) n = 959 |
|
| MI | DES |
6.26% (4.71% – 8.27%) n = 2356 |
3.90% (1.98% – 7.55%) n = 2182 |
4.04% (2.33% – 6.91%) n = 2516 |
| BMS |
9.97% (6.09% – 15.90%) n = 157 |
3.06% (1.18% – 7.69%) n = 607 |
3.43% (1.87% – 6.21%) n = 752 |
|
| TVR/TLR | DES |
7.83% (5.95% – 10.24%) n = 2257 |
10.20% (8.55% – 12.13%) n = 4772 |
8.03% (5.62% – 11.37%) n = 2912 |
| BMS |
16.95% (12.92% – 21.92%) n = 985 |
16.15% (13.93% – 18.66%) n = 1241 |
16.40% (12.23% – 21.64%) n = 959 |
|
| MACE | DES |
15.87% (12.93%-19.32%) n=2593 |
18.99% (14.92%-23.86%) n=2623 |
21.43% (14.85%-29.91%) n=1652 |
| BMS |
39.31% (31.68%-47.50%) n=554 |
32.69% (17.72%-52.26%) n=441 |
31.60% (23.15%-41.47%) n=399 |
n refers to the number of patients within the studies who contributed to the estimate of interest. Rates are the estimated percent of patients with the event and associated 95% confidence intervals.
Subsequent analysis was performed on those studies comparing DES and BMS and providing either adjusted event rates, or randomization according to stent type. Of the 12 comparative studies, 9 studies reported relevant endpoints, consisting of 5,081 patients (see Table 4). Most utilized propensity scoring for adjustment. Comparative event estimates for DES versus BMS were calculated (see Table 5). At 6–12 months, the OR for mortality was 0.94 (95%CI 0.06 – 15.48, p=0.97) and for MI was (0.64, 95%CI 0.19 – 2.17, p = 0.47). The OR clearly favored DES for TVR/TLR (0.10, 95%CI 0.01 – 0.84, p=0.01) and MACE (0.34, 95%CI 0.15 – 0.78, p=0.01) at 6–12 months. At 2 years the OR favored DES for mortality (0.42, 95%CI 0.28 – 0.62, p<0.01) and MACE (0.31, 95%CI 0.15 – 0.66, p<0.01); the OR for MI did not reach statistical significance (0.16, 95%CI 0.01 – 3.53, p=0.13). The OR for TVR/TLR at 2 years could not be estimated due to a lack of reported data. Findings at 3 years favored DES for mortality (0.70, 95%CI 0.53 – 0.92, p=0.01), MI (0.49, 95%CI 0.26 – 0.92, p=0.03), and TVR/TLR (0.46, 95%CI 0.30 – 0.69, p<0.01); the OR for MACE did not reach statistical significance (0.78, 95%CI 0.57 – 1.07, p=0.12).
Table 4.
Comparative studies of DES versus BMS
| Design | Method of Adjustment |
DES (n) |
BMS (n) |
F/u (months) |
Adjusted Point Estimate Mortality at f/u |
Adjusted Point Estimate MI at f/u |
Adjusted Point Estimate TVR/TLR at f/u |
Adjusted Point Estimate MACE at f/u |
|
|---|---|---|---|---|---|---|---|---|---|
| Chieffo 2005 (76) | Nonrandomized study | Propensity score matching | 85 | 64 | 6 | N/A | N/A |
OR 0.28 (0.09–0.81) p=0.01 |
OR 0.27 (0.09–0.73) p=0.007 |
| Erglis 2007 (12) | Randomized Controlled trial | Randomization | 53 | 50 | 6 |
OR 0.94 (0.06–15.48) p=1.00 |
OR 0.64 (0.19–2.17) p= 0.47 |
OR 0.10 (0.01–0.84) p=0.01 |
OR 0.36 (0.13–0.96) p=0.04 |
| Gao 2008 (77) | Prospective Cohort study (DES compared to historical BMS cohort) | Propensity score matching | 220 | 224 | 15 | N/A | N/A | N/A |
OR 0.49 (0.26–0.94) p=0.032 |
| Han 2009 (78) | Prospective Cohort study | Propensity score matching | 178 | 109 | 35+/−14 |
OR 0.25 (0.08–0.81) p<0.01 |
OR 0.16 (0.01–3.53) p=0.13 |
OR 0.26 (0.08–0.83) p<0.001 |
OR 0.23 0.09–0.56) p<0.001 |
| Kim 2009 (80) | Prospective Cohort study | Weighting with propensity score | 864 | 353 | 36 |
HR 0.86 (0.50–1.47) p=0.569 |
N/A |
HR 0.32 (0.17–0.61) P<0.001 |
HR 0.81 (0.54–1.21) p=0.31 |
| Palmerini 2007 (40) | Nonrandomized study | Propensity score as a covariate | 1111 | 342 | 24 |
HR 0.48 (0.32–0.74) p=0.002 |
N/A | N/A | N/A |
| Schrale 2008 | Retrospective Cohort study | Multivariate Cox regression | 55 | 45 | 21+/14 |
HR 0.23 (0.06–0.91) p=0.034 |
N/A | N/A | N/A |
| Tamburino 2009 (83) | Nonrandomized study | Propensity score matching | 611 | 238 | 36 |
HR 0.75 (0.52–1.12) p=0.17 |
HR 0.49 (0.26–0.92) p=0.03 |
HR 0.46 (0.29–0.74) p=0.001 |
N/A |
| Tamburino 2009 (84) | Nonrandomized study | Propensity score matching | 334 | 145 | 36 |
HR 0.51 (0.30–0.86) p=0.01 |
N/A |
HR 0.79 (0.33–1.90) p=0.39 |
HR 0.73 (0.44–1.21) p=0.22 |
n refers to the number of patients within the studies who contributed to the estimate of interest. Odds ratios (OR) and Hazard ratios (HR) are reported with 95% confidence intervals.
Table 5.
Cumulative Odds Ratios for Comparative Studies (DES versus BMS)
| Time | Contributing studies | DES (n) |
BMS (n) |
OR (95% CI) |
P value | |
|---|---|---|---|---|---|---|
| Mortality | 6–12months | Erglis 2007(12) | 53 | 50 |
0.94 (0.06–15.48) |
p=0.97 |
| 2 years | Han 2009 (78) Palmerini 2007 (40) Schrale 2008 (82) |
1344 | 496 |
0.42 (0.28–0.62) |
p<0.01 | |
| 3 years | Kim 2009 (80) Tamburino 2009 (83) Tamburino 2009 (84) |
1809 | 736 |
0.70 (0.53–0.92) |
p=0.01 | |
| MI | 6–12 months | Erglis 2007(12) | 53 | 50 |
0.64 (0.19–2.17) |
p= 0.47 |
| 2 years | Han 2009 (78) | 178 | 109 |
0.16 (0.01–3.53) |
p=0.13 | |
| 3 years | Tamburino 2009 (83) | 611 | 238 |
0.49 (0.26–0.92) |
p=0.03 | |
| TVR/TLR | 6–12 months | Erglis 2007(12) | 53 | 50 |
0.10 (0.01–0.84) |
p=0.01 |
| 2 years | No studies | -- | -- | -- | -- | |
| 3 years | Kim 2009 (80) Tamburino 2009 (83) Tamburino 2009 (84) |
1809 | 736 |
0.46 (0.30–0.69) |
p<0.01 | |
| MACE | 6–12 months | Chieffo 2005 (76) Erglis 2007(12) |
138 | 114 |
0.34 (0.15–0.78) |
P=0.01 |
| 2 years | Gao 2008 (77) Han 2009 (78) |
398 | 333 |
0.31 (0.15–0.66) |
P<0.01 | |
| 3 years | Kim 2009 (80) Tamburino 2009 (84) |
1198 | 498 |
0.78 (0.57–1.07) |
P=0.12 |
n refers to the number of patients within the studies who contributed to the estimate of interest. OR are reported with 95% confidence intervals.
Discussion
PCI is increasingly being performed for lesions previously considered contraindicated, such as unprotected LMCA. Given the lower rates of restenosis reported with DES in PCI of standard coronary lesions, there has been a trend towards their use in unprotected LMCA PCI. However, the superiority of DES over BMS for unprotected LMCA has not been clearly established.
We reviewed the literature on unprotected LMCA PCI to compare outcomes between DES vs. BMS. We identified 44 studies involving PCI for unprotected LMCA as a source for crude event rates. Crude event rates were lower for DES than BMS for mortality, TVR/TLR and MACE at 6–12 months, 2 years, and 3 years, but appeared equivalent for MI at these same timeponts. However, these rates are unadjusted, rendering them prone to selection bias and confounding.
To address this, we performed a subsequent analysis involving studies that provided adjusted event rates or randomized patients according to stent type (DES vs. BMS). Although event rates at 6–12 months favored DES, the sample size was small, involving predominantly one study (12). At 2 and 3 years post-PCI, the sample size was larger and improved outcomes with DES over BMS were observed for mortality, MI, TVR/TLR, and MACE. Statistically significance differences were observed in most cases.
Although the finding of lower TVR/TLR rates is consistent with the known performance of DES, no study to date has shown a consistent mortality benefit with DES over BMS in unprotected LMCA PCI. The reason for the lower mortality rate in the DES group seen in our meta-analysis is unclear. It may be that DES, with known lower rates of restenosis, provides a true advantage over BMS. In the critical left main position a small or moderate degree of restenosis could theoretically precipitate critical ischemia. Alternatively, this finding could be due to methodological issues. Selection bias may have favored DES: patients with fewer medical comorbidities may have preferentially undergone DES placement. A review of overall patient demographics in our analysis does not support this, as similar rates of cardiac risk factors were found between both groups (see Table 2). An alternative explanation may relate to a procedural learning curve, as operators may have become more technically proficient at unprotected LMCA PCI by the time DES were favored. Finally, as medication profiles at baseline and follow-up were not consistently reported, it is possible that the benefit seen with DES could be due, in part, to a longer duration of dual antiplatelet drug therapy as compared to BMS. Similarly, patients deemed to be poor candidates for long-term dual or triple antiplatelet therapy may have been denied treatment with DES.
A recent meta-analysis of patients undergoing DES for unprotected LMCA by Biondi-Zoccai et al noted similar findings, reporting an adjusted OR of 0.34 for both MACE and TVR, favoring DES over BMS (13). This meta-analysis was performed through 2006 and included far fewer patients than our analysis (206 DES patients, 190 BMS patients). Since our analysis was performed, Buszman et al have reported on the long-term follow-up of a group of 252 patients from the LE-MANS registry (14). Their results mirror ours. Unmatched analysis showed a significantly lower rate of major adverse cardiovascular or cerebral events (MACCE) with DES as compared to BMS at four-year follow-up (14.9% vs. 25.9%, p=0.039); subsequent propensity matched analysis showed similar results. They noted that mortality rates favored DES, although this did not reach statistical significance (9.6% vs. 13.3%, p=NS). In a subgroup of patients with distal unprotected LMCA, however, DES was associated with a statistically significant lower mortality rate as compared to BMS (p=0.03). Results from the left main subset of the SYNTAX trial (15) were presented at TCT 2008. Reported 12 month DES event rates were similar to our cumulative crude estimates, with a rate of 4.2% for mortality, 4.3% for MI, and 15.8% for major cardiac or cerebrovascular adverse events (MACCE) (16). As these results have yet to be published they were not included in our analysis. SYNTAX did not include a BMS arm and thus would not impact our comparative analysis.
Currently there are no large, randomized controlled clinical trials comparing DES to BMS in unprotected LMCA. Two ongoing studies comparing PCI with DES to CABG for unprotected LMCA (PRE-COMBAT and REVASCULARIZE) do not include a comparison with BMS. Therefore our meta-analysis may offer evidence to guide clinical practice.
Study limitations
Our study has clear limitations. The limitations of the meta-analytical approach are well known and documented (17); the meta-analytical approach with observational data is even more fraught with limitations (18). The inclusion of only published studies makes our analysis prone to publication bias. Our results, particularly the crude event rates, are prone to confounding and selection bias and thus direct comparison of these overall rates was not performed. We did not have data for all studies at each time period; therefore this limits comparison of rates across time within a specific endpoint. Finally, we were unable to control for the specific type of DES or BMS used, as some studies suggest heterogenous outcomes within the stent types.
Conclusions
The results of this meta-analysis suggest that DES is associated with favorable outcomes as compared to BMS in unprotected LMCA PCI. The improved outcomes observed with DES compared to BMS support a continued re-evaluation of the role of PCI for the treatment of unprotected LMCA.
Bibliography
- 1.Caracciolo EA, Davis KB, Sopko G, et al. Comparison of surgical and medical group survival in patients with left main coronary artery disease. Long-term CASS experience. Circulation. 1995;91:2325–2334. doi: 10.1161/01.cir.91.9.2325. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf S, Zucker D, Peduzzi P, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994;344:563–570. doi: 10.1016/s0140-6736(94)91963-1. [DOI] [PubMed] [Google Scholar]
- 3.Eagle KA, Guyton RA, Davidoff R, et al. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery) J Am Coll Cardiol. 2004;44:e213–e310. doi: 10.1016/j.jacc.2004.07.021. [DOI] [PubMed] [Google Scholar]
- 4.Stertzer SH, Myler RK, Insel H, Wallsh E, Rossi P. Percutaneous transluminal coronary angioplasty in left main stem coronary stenosis: a five-year appraisal. Int J Cardiol. 1985;9:149–159. doi: 10.1016/0167-5273(85)90194-9. [DOI] [PubMed] [Google Scholar]
- 5.King SB, 3rd, Smith SC, Jr, Hirshfeld JW, Jr, et al. 2007 focused update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. J Am Coll Cardiol. 2008;51:172–209. doi: 10.1016/j.jacc.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Moses JW, Leon MB, Popma JJ, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003;349:1315–1323. doi: 10.1056/NEJMoa035071. [DOI] [PubMed] [Google Scholar]
- 7.Stone GW, Ellis SG, Cox DA, et al. One-year clinical results with the slow-release, polymer-based, paclitaxel-eluting TAXUS stent: the TAXUS-IV trial. Circulation. 2004;109:1942–1947. doi: 10.1161/01.CIR.0000127110.49192.72. [DOI] [PubMed] [Google Scholar]
- 8.Kushner FG, Hand M, Smith SC, Jr, et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205–2241. doi: 10.1016/j.jacc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 9.Beohar N, Davidson CJ, Kip KE, et al. Outcomes and complications associated with off-label and untested use of drug-eluting stents. JAMA. 2007;297:1992–2000. doi: 10.1001/jama.297.18.1992. [DOI] [PubMed] [Google Scholar]
- 10.Stettler C, Wandel S, Allemann S, et al. Outcomes associated with drug-eluting and bare-metal stents: a collaborative network meta-analysis. Lancet. 2007;370:937–948. doi: 10.1016/S0140-6736(07)61444-5. [DOI] [PubMed] [Google Scholar]
- 11.Comprehensive Meta Analysis, version 2.2.048. www.Meta-Analysis.com.
- 12.Erglis A, Narbute I, Kumsars I, et al. A randomized comparison of paclitaxel-eluting stents versus bare-metal stents for treatment of unprotected left main coronary artery stenosis. J Am Coll Cardiol. 2007;50:491–497. doi: 10.1016/j.jacc.2007.03.055. [DOI] [PubMed] [Google Scholar]
- 13.Biondi-Zoccai GG, Lotrionte M, Moretti C, et al. A collaborative systematic review and meta-analysis on 1278 patients undergoing percutaneous drug-eluting stenting for unprotected left main coronary artery disease. Am Heart J. 2008;155:274–283. doi: 10.1016/j.ahj.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 14.Buszman PE, Buszman PP, Kiesz RS, et al. Early and long-term results of unprotected left main coronary artery stenting: the LE MANS (Left Main Coronary Artery Stenting) registry. J Am Coll Cardiol. 2009;54:1500–1511. doi: 10.1016/j.jacc.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 15.Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–972. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 16.Data presented by Patrick W, Dr, Serruys M., PhD TCT. 2008
- 17.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 18.Egger M, Schneider M, Davey Smith G. Spurious precision? Meta-analysis of observational studies. BMJ. 1998;316:140–144. doi: 10.1136/bmj.316.7125.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang HW, Brent BN, Shaw RE. Trends in percutaneous versus surgical revascularization of unprotected left main coronary stenosis in the drug-eluting stent era: a report from the American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR) Catheter Cardiovasc Interv. 2006;68:867–872. doi: 10.1002/ccd.20886. [DOI] [PubMed] [Google Scholar]
- 20.Wu C, Hannan EL, Walford G, Faxon DP. Utilization and outcomes of unprotected left main coronary artery stenting and coronary artery bypass graft surgery. Ann Thorac Surg. 2008;86:1153–1159. doi: 10.1016/j.athoracsur.2008.05.059. [DOI] [PubMed] [Google Scholar]
- 21.Lee RJ, Shih KN, Lee SH, et al. Predictors of long-term outcomes in patients after elective stent implantation for unprotected left main coronary artery disease. Heart Vessels. 2007;22:99–103. doi: 10.1007/s00380-006-0948-7. [DOI] [PubMed] [Google Scholar]
- 22.White AJ, Kedia G, Mirocha JM, et al. Comparison of coronary artery bypass surgery and percutaneous drug-eluting stent implantation for treatment of left main coronary artery stenosis. JACC Cardiovasc Interv. 2008;1:236–245. doi: 10.1016/j.jcin.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Wu XM, Liu CP, Lin WC, Kao HL. Long-term outcome of percutaneous coronary intervention for unprotected left main coronary artery disease. Int J Cardiol. 2008 doi: 10.1016/j.ijcard.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 24.Cheng CI, Wu CJ, Fang CY, et al. Feasibility and safety of transradial stenting for unprotected left main coronary artery stenoses. Circ J. 2007;71:855–861. doi: 10.1253/circj.71.855. [DOI] [PubMed] [Google Scholar]
- 25.Carrie D, Eltchaninoff H, Lefevre T, et al. Twelve month clinical and angiographic outcome after stenting of unprotected left main coronary artery stenosis with paclitaxel-eluting stents--results of the multicentre FRIEND registry. EuroIntervention. 2009;4:449–456. doi: 10.4244/eijv4i4a78. [DOI] [PubMed] [Google Scholar]
- 26.Carrie D, Maupas E, Hmem M, Lhermusier T, Elbaz M, Puel J. Clinical and angiographic outcome of stenting of unprotected left main coronary artery bifurcation narrowing. Int J Cardiovasc Intervent. 2005;7:97–100. doi: 10.1080/14628840510011243. [DOI] [PubMed] [Google Scholar]
- 27.Peszek-Przybyla E, Buszman P, Bialkowska B, et al. Stent implantation for the unprotected left main coronary artery. The long-term outcome of 62 patients. Kardiol Pol. 2006;64:1–6. discussion 7. [PubMed] [Google Scholar]
- 28.Capodanno D, Di Salvo ME, Palmerini T, et al. Long-term clinical benefit of drug-eluting stents over bare-metal stents in diabetic patients with de novo left main coronary artery disease: results from a real-world multicenter registry. Catheter Cardiovasc Interv. 2009;73:310–316. doi: 10.1002/ccd.21845. [DOI] [PubMed] [Google Scholar]
- 29.Meliga E, Garcia-Garcia HM, Valgimigli M, et al. Impact of drug-eluting stent selection on long-term clinical outcomes in patients treated for unprotected left main coronary artery disease: The sirolimus vs paclitaxel drug-eluting stent for left main registry (SP-DELFT) Int J Cardiol. 2008 doi: 10.1016/j.ijcard.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Lee JY, Park DW, Yun SC, et al. Long-term clinical outcomes of sirolimus- versus paclitaxel-eluting stents for patients with unprotected left main coronary artery disease: analysis of the MAIN-COMPARE (revascularization for unprotected left main coronary artery stenosis: comparison of percutaneous coronary angioplasty versus surgical revascularization) registry. J Am Coll Cardiol. 2009;54:853–859. doi: 10.1016/j.jacc.2009.04.071. [DOI] [PubMed] [Google Scholar]
- 31.Gao RL, Xu B, Chen JL, et al. Prognosis of unprotected left main coronary artery stenting and the factors affecting the outcomes in Chinese. Chin Med J (Engl) 2006;119:14–20. [PubMed] [Google Scholar]
- 32.Valgimigli M, Malagutti P, Aoki J, et al. Sirolimus-eluting versus paclitaxel-eluting stent implantation for the percutaneous treatment of left main coronary artery disease: a combined RESEARCH and T-SEARCH long-term analysis. J Am Coll Cardiol. 2006;47:507–414. doi: 10.1016/j.jacc.2005.09.040. [DOI] [PubMed] [Google Scholar]
- 33.Valgimigli M, Malagutti P, Rodriguez Granillo GA, et al. Single-vessel versus bifurcation stenting for the treatment of distal left main coronary artery disease in the drug-eluting stenting era. Clinical and angiographic insights into the Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital (RESEARCH) and Taxus-Stent Evaluated at Rotterdam Cardiology Hospital (T-SEARCH) registries. Am Heart J. 2006;152:896–902. doi: 10.1016/j.ahj.2006.03.029. [DOI] [PubMed] [Google Scholar]
- 34.Valgimigli M, Malagutti P, Rodriguez-Granillo GA, et al. Distal left main coronary disease is a major predictor of outcome in patients undergoing percutaneous intervention in the drug-eluting stent era: an integrated clinical and angiographic analysis based on the Rapamycin-Eluting Stent Evaluated At Rotterdam Cardiology Hospital (RESEARCH) and Taxus-Stent Evaluated At Rotterdam Cardiology Hospital (T-SEARCH) registries. J Am Coll Cardiol. 2006;47:1530–1537. doi: 10.1016/j.jacc.2005.11.066. [DOI] [PubMed] [Google Scholar]
- 35.Valgimigli M, van Mieghem CA, Ong AT, et al. Short- and long-term clinical outcome after drug-eluting stent implantation for the percutaneous treatment of left main coronary artery disease: insights from the Rapamycin-Eluting and Taxus Stent Evaluated At Rotterdam Cardiology Hospital registries (RESEARCH and T-SEARCH) Circulation. 2005;111:1383–1389. doi: 10.1161/01.CIR.0000158486.20865.8B. [DOI] [PubMed] [Google Scholar]
- 36.Tan WA, Tamai H, Park SJ, et al. Long-term clinical outcomes after unprotected left main trunk percutaneous revascularization in 279 patients. Circulation. 2001;104:1609–1614. doi: 10.1161/hc3901.096669. [DOI] [PubMed] [Google Scholar]
- 37.Dubois C, Dens J, Sinnaeve P, et al. Results of percutaneous coronary intervention of the unprotected left main coronary artery in 143 patients and comparison of 30-day mortality to results of coronary artery bypass grafting. Am J Cardiol. 2008;101:75–81. doi: 10.1016/j.amjcard.2007.07.051. [DOI] [PubMed] [Google Scholar]
- 38.Brener SJ, Galla JM, Bryant R, 3rd, Sabik JF, 3rd, Ellis SG. Comparison of percutaneous versus surgical revascularization of severe unprotected left main coronary stenosis in matched patients. Am J Cardiol. 2008;101:169–172. doi: 10.1016/j.amjcard.2007.08.054. [DOI] [PubMed] [Google Scholar]
- 39.Sheiban I, Garrone P, Sillano D, et al. Impact of diabetes mellitus on early and long-term results of percutaneous drug-eluting stent implantation for unprotected left main coronary disease. J Cardiovasc Med (Hagerstown) 2008;9:1246–1253. doi: 10.2459/JCM.0b013e32830d8303. [DOI] [PubMed] [Google Scholar]
- 40.Palmerini T, Barlocco F, Santarelli A, et al. A comparison between coronary artery bypass grafting surgery and drug eluting stent for the treatment of unprotected left main coronary artery disease in elderly patients (aged > or =75 years) Eur Heart J. 2007;28:2714–2719. doi: 10.1093/eurheartj/ehm403. [DOI] [PubMed] [Google Scholar]
- 41.Rodes-Cabau J, Deblois J, Bertrand OF, et al. Nonrandomized comparison of coronary artery bypass surgery and percutaneous coronary intervention for the treatment of unprotected left main coronary artery disease in octogenarians. Circulation. 2008;118:2374–2381. doi: 10.1161/CIRCULATIONAHA.107.727099. [DOI] [PubMed] [Google Scholar]
- 42.Lee MS, Tseng CH, Barker CM, et al. Outcome after surgery and percutaneous intervention for cardiogenic shock and left main disease. Ann Thorac Surg. 2008;86:29–34. doi: 10.1016/j.athoracsur.2008.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tan CH, Hong MK, Lee CW, et al. Percutaneous coronary intervention with stenting of left main coronary artery with drug-eluting stent in the setting of acute ST elevation myocardial infarction. Int J Cardiol. 2008;126:224–228. doi: 10.1016/j.ijcard.2007.03.131. [DOI] [PubMed] [Google Scholar]
- 44.Lee MS, Sillano D, Latib A, et al. Multicenter international registry of unprotected left main coronary artery percutaneous coronary intervention with drug-eluting stents in patients with myocardial infarction. Catheter Cardiovasc Interv. 2009;73:15–21. doi: 10.1002/ccd.21712. [DOI] [PubMed] [Google Scholar]
- 45.Barlis P, Horrigan M, Elis S, et al. Treatment of unprotected left main disease with drug-eluting stents in patients at high risk for coronary artery bypass grafting. Cardiovasc Revasc Med. 2007;8:84–89. doi: 10.1016/j.carrev.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 46.Lee RJ, Lee SH, Shyu KG, et al. Immediate and long-term outcomes of stent implantation for unprotected left main coronary artery disease. Int J Cardiol. 2001;80:173–177. doi: 10.1016/s0167-5273(01)00478-8. [DOI] [PubMed] [Google Scholar]
- 47.Hsu JT, Chu CM, Chang ST, Kao CL, Chung CM. Percutaneous coronary intervention versus coronary artery bypass graft surgery for the treatment of unprotected left main coronary artery stenosis: in-hospital and one year outcome after emergent and elective treatments. Int Heart J. 2008;49:355–370. doi: 10.1536/ihj.49.355. [DOI] [PubMed] [Google Scholar]
- 48.Sheiban I, Gerasimou A, Bollati M, et al. Early and long-term results of percutaneous coronary intervention for unprotected left main trifurcation disease. Catheter Cardiovasc Interv. 2009;73:25–31. doi: 10.1002/ccd.21759. [DOI] [PubMed] [Google Scholar]
- 49.Hasegawa T, Ako J, Koo BK, et al. Analysis of left main coronary artery bifurcation lesions treated with biolimus-eluting DEVAX AXXESS plus nitinol self-expanding stent: intravascular ultrasound results of the AXXENT trial. Catheter Cardiovasc Interv. 2009;73:34–41. doi: 10.1002/ccd.21765. [DOI] [PubMed] [Google Scholar]
- 50.Black A, Cortina R, Bossi I, Choussat R, Fajadet J, Marco J. Unprotected left main coronary artery stenting: correlates of midterm survival and impact of patient selection. J Am Coll Cardiol. 2001;37:832–838. doi: 10.1016/s0735-1097(00)01176-1. [DOI] [PubMed] [Google Scholar]
- 51.Kelley MP, Klugherz BD, Hashemi SM, et al. One-year clinical outcomes of protected and unprotected left main coronary artery stenting. Eur Heart J. 2003;24:1554–1559. doi: 10.1016/s0195-668x(03)00314-2. [DOI] [PubMed] [Google Scholar]
- 52.Lee BK, Hong MK, Lee CW, et al. Five-year outcomes after stenting of unprotected left main coronary artery stenosis in patients with normal left ventricular function. Int J Cardiol. 2007;115:208–213. doi: 10.1016/j.ijcard.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 53.Silvestri M, Barragan P, Sainsous J, et al. Unprotected left main coronary artery stenting: immediate and medium-term outcomes of 140 elective procedures. J Am Coll Cardiol. 2000;35:1543–1550. doi: 10.1016/s0735-1097(00)00588-x. [DOI] [PubMed] [Google Scholar]
- 54.Takagi T, Stankovic G, Finci L, et al. Results and long-term predictors of adverse clinical events after elective percutaneous interventions on unprotected left main coronary artery. Circulation. 2002;106:698–702. doi: 10.1161/01.cir.0000024983.34728.5d. [DOI] [PubMed] [Google Scholar]
- 55.Agostoni P, Valgimigli M, Van Mieghem CA, e, et al. Comparison of early outcome of percutaneous coronary intervention for unprotected left main coronary artery disease in the drug-eluting stent era with versus without intravascular ultrasonic guidance. Am J Cardiol. 2005;95:644–647. doi: 10.1016/j.amjcard.2004.10.042. [DOI] [PubMed] [Google Scholar]
- 56.Arampatzis CA, Lemos PA, Tanabe K, et al. Effectiveness of sirolimus-eluting stent for treatment of left main coronary artery disease. Am J Cardiol. 2003;92:327–329. doi: 10.1016/s0002-9149(03)00640-4. [DOI] [PubMed] [Google Scholar]
- 57.Chieffo A, Park SJ, Valgimigli M, et al. Favorable long-term outcome after drug-eluting stent implantation in nonbifurcation lesions that involve unprotected left main coronary artery: a multicenter registry. Circulation. 2007;116:158–162. doi: 10.1161/CIRCULATIONAHA.107.692178. [DOI] [PubMed] [Google Scholar]
- 58.Chieffo A, Park SJ, Meliga E, et al. Late and very late stent thrombosis following drug-eluting stent implantation in unprotected left main coronary artery: a multicentre registry. Eur Heart J. 2008 doi: 10.1093/eurheartj/ehn270. [DOI] [PubMed] [Google Scholar]
- 59.Cherradi R, Ouldzein H, Zouaoui W, Elbaz M, Puel J, Carrie D. Clinical and angiographic results of angioplasty with a paclitaxel-eluting stent for unprotected left main coronary artery disease (a study of 101 consecutive patients) Arch Cardiovasc Dis. 2008;101:11–17. doi: 10.1016/s1875-2136(08)70249-3. [DOI] [PubMed] [Google Scholar]
- 60.de Lezo JS, Medina A, Pan M, et al. Rapamycin-eluting stents for the treatment of unprotected left main coronary disease. Am Heart J. 2004;148:481–485. doi: 10.1016/j.ahj.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 61.Ge L, Cosgrave J, Iakovou I, et al. Long-term outcomes following drug-eluting stent implantation in unprotected left main bifurcation lesions. Chin Med J (Engl) 2007;120:545–551. [PubMed] [Google Scholar]
- 62.Khattab AA, Hamm CW, Senges J, et al. Sirolimus-Eluting Stent Treatment for Unprotected versus Protected Left Main Coronary Artery Disease in the Widespread Clinical Routine: 6-Month and 3-Year Clinical Follow-up Results From The Prospective Multi-Centre German Cypher Registry. Heart. 2007 doi: 10.1136/hrt.2007.104703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim YH, Park SW, Hong MK, et al. Comparison of simple and complex stenting techniques in the treatment of unprotected left main coronary artery bifurcation stenosis. Am J Cardiol. 2006;97:1597–1601. doi: 10.1016/j.amjcard.2005.12.051. [DOI] [PubMed] [Google Scholar]
- 64.Kim YH, Dangas GD, Solinas E, et al. Effectiveness of drug-eluting stent implantation for patients with unprotected left main coronary artery stenosis. Am J Cardiol. 2008;101:801–806. doi: 10.1016/j.amjcard.2007.10.052. [DOI] [PubMed] [Google Scholar]
- 65.Lee SH, Ko YG, Jang Y, et al. Sirolimus- versus paclitaxel-eluting stent implantation for unprotected left main coronary artery stenosis. Cardiology. 2005;104:181–185. doi: 10.1159/000088106. [DOI] [PubMed] [Google Scholar]
- 66.Lozano I, Herrera C, Moris C, et al. Drug-eluting stents in patients with left main coronary lesions who are not candidates for surgical revascularization. Rev Esp Cardiol. 2005;58:145–152. [PubMed] [Google Scholar]
- 67.Mehilli J, Kastrati A, Byrne RA, et al. Paclitaxel- versus sirolimus-eluting stents for unprotected left main coronary artery disease. J Am Coll Cardiol. 2009;53:1760–1768. doi: 10.1016/j.jacc.2009.01.035. [DOI] [PubMed] [Google Scholar]
- 68.Meliga E, Garcia-Garcia HM, Valgimigli M, et al. Longest available clinical outcomes after drug-eluting stent implantation for unprotected left main coronary artery disease: the DELFT (Drug Eluting stent for LeFT main) Registry. J Am Coll Cardiol. 2008;51:2212–2219. doi: 10.1016/j.jacc.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 69.Migliorini A, Moschi G, Giurlani L, et al. Drug-eluting stent supported percutaneous coronary intervention for unprotected left main disease. Catheter Cardiovasc Interv. 2006;68:225–230. doi: 10.1002/ccd.20815. [DOI] [PubMed] [Google Scholar]
- 70.Price MJ, Cristea E, Sawhney N, et al. Serial angiographic follow-up of sirolimus-eluting stents for unprotected left main coronary artery revascularization. J Am Coll Cardiol. 2006;47:871–877. doi: 10.1016/j.jacc.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 71.Sanmartin M, Baz JA, Lozano I, et al. One-year results of unprotected left main disease treatment with paclitaxel-eluting stents: results of a multicenter registry. Catheter Cardiovasc Interv. 2007;69:372–377. doi: 10.1002/ccd.20960. [DOI] [PubMed] [Google Scholar]
- 72.Sheiban I, Meliga E, Moretti C, et al. Long-term clinical and angiographic outcomes of treatment of unprotected left main coronary artery stenosis with sirolimus-eluting stents. Am J Cardiol. 2007;100:431–435. doi: 10.1016/j.amjcard.2007.03.041. [DOI] [PubMed] [Google Scholar]
- 73.Vaquerizo B, Lefevre T, Darremont O, et al. Unprotected left main stenting in the real world: two-year outcomes of the French left main taxus registry. Circulation. 2009;119:2349–2356. doi: 10.1161/CIRCULATIONAHA.108.804930. [DOI] [PubMed] [Google Scholar]
- 74.Vecchio S, Chechi T, Vittori G, et al. Outlook of drug-eluting stent implantation for unprotected left main disease: insights on long-term clinical predictors. J Invasive Cardiol. 2007;19:381–387. [PubMed] [Google Scholar]
- 75.Wood FO, Saylors EK, Schneider JE, Jobe RL, Mann JT., 3rd Unprotected left main disease managed with drug-eluting stents: long-term outcome of 100 patients with increased surgical risk. Catheter Cardiovasc Interv. 2008;71:533–538. doi: 10.1002/ccd.21447. [DOI] [PubMed] [Google Scholar]
- 76.Chieffo A, Stankovic G, Bonizzoni E, et al. Early and mid-term results of drug-eluting stent implantation in unprotected left main. Circulation. 2005;111:791–795. doi: 10.1161/01.CIR.0000155256.88940.F8. [DOI] [PubMed] [Google Scholar]
- 77.Gao RL, Xu B, Chen JL, et al. Immediate and long-term outcomes of drug-eluting stent implantation for unprotected left main coronary artery disease: comparison with bare-metal stent implantation. Am Heart J. 2008;155:553–561. doi: 10.1016/j.ahj.2007.10.030. [DOI] [PubMed] [Google Scholar]
- 78.Han Y, Wang S, Jing Q, et al. Comparison of long-term efficacy of the paclitaxel-eluting stent versus the bare-metal stent for treatment of unprotected left main coronary artery disease. Am J Cardiol. 2009;103:194–198. doi: 10.1016/j.amjcard.2008.08.058. [DOI] [PubMed] [Google Scholar]
- 79.Hertting K, Harle T, Krause K, Reimers J, Boczor S, Kuck KH. Stenting of unprotected left main stem stenosis: Results from a German single-centre registry. Exp Clin Cardiol. 2008;13:37–41. [PMC free article] [PubMed] [Google Scholar]
- 80.Kim YH, Park DW, Lee SW, et al. Long-term safety and effectiveness of unprotected left main coronary stenting with drug-eluting stents compared with bare-metal stents. Circulation. 2009;120:400–407. doi: 10.1161/CIRCULATIONAHA.108.800805. [DOI] [PubMed] [Google Scholar]
- 81.Palmerini T, Marzocchi A, Tamburino C, et al. Two-year clinical outcome with drug-eluting stents versus bare-metal stents in a real-world registry of unprotected left main coronary artery stenosis from the Italian Society of Invasive Cardiology. Am J Cardiol. 2008;102:1463–1468. doi: 10.1016/j.amjcard.2008.07.030. [DOI] [PubMed] [Google Scholar]
- 82.Schrale RG, van Gaal W, Channon KM, Forfar JC, Ormerod OJ, Banning AP. Long-term outcomes of percutaneous coronary intervention for unprotected left main coronary artery disease. Int J Cardiol. 2008;130:185–189. doi: 10.1016/j.ijcard.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 83.Tamburino C, Di Salvo ME, Capodanno D, et al. Comparison of drug-eluting stents and bare-metal stents for the treatment of unprotected left main coronary artery disease in acute coronary syndromes. Am J Cardiol. 2009;103:187–193. doi: 10.1016/j.amjcard.2008.08.059. [DOI] [PubMed] [Google Scholar]
- 84.Tamburino C, Di Salvo ME, Capodanno D, et al. Are drug-eluting stents superior to bare-metal stents in patients with unprotected non-bifurcational left main disease? Insights from a multicentre registry. Eur Heart J. 2009 doi: 10.1093/eurheartj/ehp052. [DOI] [PubMed] [Google Scholar]
- 85.Wood F, Bazemore E, Schneider JE, Jobe RL, Mann T. Technique of left main stenting is dependent on lesion location and distal branch protection. Catheter Cardiovasc Interv. 2005;65:499–503. doi: 10.1002/ccd.20426. [DOI] [PubMed] [Google Scholar]
- 86.Buszman PE, Kiesz SR, Bochenek A, et al. Acute and late outcomes of unprotected left main stenting in comparison with surgical revascularization. J Am Coll Cardiol. 2008;51:538–545. doi: 10.1016/j.jacc.2007.09.054. [DOI] [PubMed] [Google Scholar]
- 87.Chieffo A, Morici N, Maisano F, et al. Percutaneous treatment with drug-eluting stent implantation versus bypass surgery for unprotected left main stenosis: a single-center experience. Circulation. 2006;113:2542–2547. doi: 10.1161/CIRCULATIONAHA.105.595694. [DOI] [PubMed] [Google Scholar]
- 88.Makikallio TH, Niemela M, Kervinen K, et al. Coronary angioplasty in drug eluting stent era for the treatment of unprotected left main stenosis compared to coronary artery bypass grafting. Ann Med. 2008;40:437–443. doi: 10.1080/07853890701879790. [DOI] [PubMed] [Google Scholar]
- 89.Palmerini T, Marzocchi A, Marrozzini C, et al. Comparison between coronary angioplasty and coronary artery bypass surgery for the treatment of unprotected left main coronary artery stenosis (the Bologna Registry) Am J Cardiol. 2006;98:54–59. doi: 10.1016/j.amjcard.2006.01.070. [DOI] [PubMed] [Google Scholar]
- 90.Sanmartin M, Baz JA, Claro R, et al. Comparison of drug-eluting stents versus surgery for unprotected left main coronary artery disease. Am J Cardiol. 2007;100:970–973. doi: 10.1016/j.amjcard.2007.04.037. [DOI] [PubMed] [Google Scholar]
- 91.Seung KB, Park DW, Kim YH, et al. Stents versus coronary-artery bypass grafting for left main coronary artery disease. N Engl J Med. 2008;358:1781–1792. doi: 10.1056/NEJMoa0801441. [DOI] [PubMed] [Google Scholar]