Abstract
The present investigation examined the mediating role of distress tolerance in the association between impulsivity and alcohol use coping motives among trauma-exposed individuals. Participants were 86 adults (64.3% women; Mage = 23.4, SD = 9.3) who met the DSM-IV-TR posttraumatic stress disorder (PTSD) criterion A for at least one traumatic life event and endorsed alcohol use in the past month. Distress tolerance at least partially mediated the association between impulsivity and alcohol use coping motives, after controlling for the variance explained by PTSD symptom severity and alcohol use problems. Clinical implications and future directions related to this line of inquiry are presented and discussed.
Keywords: Impulsivity, Alcohol, Coping, Distress Tolerance, PTSD
Introduction
Significant associations have been documented between posttraumatic stress disorder (PTSD) symptoms, includingPTSD diagnosis, and alcohol use disorders (e.g., McFarlane et al., 2009; Stewart, 1996). Recent efforts have focused on elucidating the mechanisms underlying the co-occurrence of these clinical problems. The examination of motivations for alcohol use is promising in understanding the association between PTSD and problematic alcohol use. Coping motives, in particular, are significantly related to alcohol consumption and alcohol use problems (Cooper, 1994).Emerging research has indicated that trauma-exposed individuals with or without PTSDare especially likely to demonstrate enhanced motivation to drink alcohol to cope with negative affective states (e.g., Dixon, Leen-Feldner, Ham, Feldner, & Lewis, 2009), and drinking to cope has been shown to mediate the relationship between alcohol consumption rate and PTSD symptoms (Kaysen et al., 2007).Given the associations between PTSD symptoms and alcohol use coping motives, it is pertinent to improve our understanding of cognitive-affective factors that may underlie this relationship to inform clinical interventions. Impulsivity and distress tolerance are two promising factors in this domain, as both possess associations to PTSD symptoms and problem alcohol use.
Impulsivity, the tendency to opt for immediate reward regardless of long-term consequences (Moeller, Barratt, Dougherty, Schmitz, & Swann, 2001), is associated with PTSD (Casada&Roache, 2005), binge drinking (James & Taylor, 2007), and shorter duration of alcohol abstinence (Charney, Zikos, & Gill, 2010). Impulsivity may function as a risk and maintenance factor for PTSD symptoms. Specifically, greater impulsivity may predispose individuals to engage in high-risk behaviors (e.g., substance use), which may lead to increased risk for trauma exposure (e.g., Stewart & Israeli, 2002). Moreover, greater impulsivity post-trauma theoretically may predispose individuals with PTSD symptoms to act upon their symptoms in a risky manner to alleviate the associated distress. Finally, theory and emerging empirical evidence suggest that individuals high in certain forms of impulsivity (e.g., “negative urgency,” or the tendency to “act rashly in response to distress,” Cyders et al., 2007) may more immediately select negative reinforcement opportunities, such as coping-oriented alcohol use, when faced with high levels of negative affect (Cyders& Smith, 2008).
Distress tolerance, the perceived or actual ability to withstand aversive physical or emotional stimuli (Simons &Gaher, 2005), is anotherpromisingexplanatory factor in the association between PTSD and alcohol use coping motives. Distress tolerance is a theoretically malleable factor (e.g., Linehan, 1993) that has been inversely related to PTSD symptoms (Marshall-Berenz, Vujanovic, Bonn-Miller, Bernstein, &Zvolensky, 2010), alcohol use problems (Buckner, Keough, & Schmidt, 2007), duration of substance use abstinence attempts (Daughters, Lejuez, Kahler, Strong, & Brown, 2005), and coping motives for alcohol use (Buckner et al., 2007). Trauma-exposed individuals with lower levels of distress tolerance may perceive their abilities to withstand emotional distress as compromised, and may be more motivated to use alcohol to regulate negative mood states.Consistent with this perspective, recent work has demonstrated that lower levels of distress tolerance partially mediated the association between PTSD symptoms and alcohol use coping motives among trauma-exposed adults (Vujanovic, Marshall-Berenz, &Zvolensky, in press).
To our knowledge, no studies have examined the association between impulsivity and distress tolerance, although extant models of impulsivity hypothesize key relationships between these constructs (Cyders& Smith, 2008).Further, no empirical work to date has examined the relationships among impulsivity, distress tolerance, and alcohol use coping motives among trauma-exposed adults in one overarching model. Among trauma-exposed individuals, lower levels of perceived distress tolerance (i.e., cognitive self-appraisals of one’s ability to tolerate distress) may help to explain the association between impulsivity and the tendency to opt for negative reinforcement (e.g., alcohol use) without regard for long-term consequences (Cyders& Smith, 2008). In so doing, these individuals may develop or maintain the perception that they cannot tolerate negative affective states without engaging in a behavior to alleviate those states. Lower perceived distress tolerance may thus partially mediate the relationship between impulsivity and coping motives for alcohol use, such that impulsive individuals may experience increased motivation to drink to cope by way of learning that they cannot tolerate episodes of negative affect but rather require immediate relief of the distressing affective state.
The aim of the current study was to investigate the mediating role of perceived distress tolerance in the relationship between self-reported impulsivity and coping-oriented alcohol use motives in a trauma-exposed community sample. Consistent with formal tests of mediation, it was hypothesized that: (1) impulsivity would be positively associated with alcohol use coping motives; (2) impulsivity would be negatively associated with distress tolerance; and (3) distress tolerance would mediatethe relationship between impulsivity and alcohol use coping motives (please see Figure 1).All proposed effects were examined after accounting for the variance contributed by alcohol use problems and PTSD symptomseverity.
Figure 1.
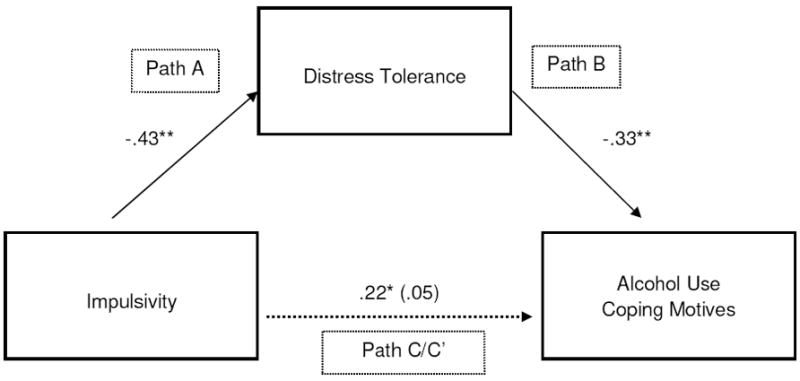
Proposed model: Distress tolerance as mediator of the association between impulsivity and alcohol use coping motives.
Note: *p< .05, **p< .01
Method
Participants
Participants were 86 adults (64.3% women; Mage = 23.4, SD = 9.3) who met the Diagnostic and Statistical Manual-IV(DSM-IV-TR)PTSD Criterion A1 and Criterion A2 (American Psychiatric Association [APA], 2000, p. 467) for at least one traumatic life event. Consistent with the Vermont state population (State of Vermont, Department of Health, 2007), approximately 94.0% of the sample identified as White/Caucasian, 2.4% as Hispanic/Latino, 1.2% as Asian, 1.2% as Biracial, and 1.2% as “other.” With regard to educational status, approximately 64.3% completed some college, 17.9% completed high school/GED, 9.5% completed college, 2.4% completed some graduate school, 4.8% completed a graduate degree, and 1.2% completed less than a high school degree.
Measures
Structured Clinical Interview for DSM-IV – Non-Patient Version (SCID-I/NP; First, Spitzer, Gibbon, & Williams, 1994)
The SCID-I/NP was administered to assess current (past month) axis I mood and anxiety disorders, current (past 6 months) substance use disorders, suicidal ideation, and psychotic-spectrum symptoms. Each SCID administration was reviewed by the PI (E.M.-B.) to ensure inter-rater agreement.No instances of diagnostic disagreement between the CAPS interviewers and the PI were noted.
Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995)
The CAPS was employed to assess the frequency and intensity of current (past month) PTSD symptoms and a PTSDdiagnosis. All individuals met the DSM-IV-TR PTSD Criterion A (APA, 2000, p. 467) for at least one traumatic event. The CAPS Life Events Checklist was used to index number of traumatic events. All events endorsed on the Life Events Checklist are not assessed for Criterion A status, only the target/worst event. Past work has found that the Life Events Checklist has good test-retest reliability and convergent validity (Gray, Litz, Hsu, & Lombardo, 2004).Consistent with prior research (Weathers, Ruscio, & Keane, 1999), symptom severity was defined as the sum of the frequency and intensity ratings.CAPS administrationswere conducted by trained clinical assessors and reviewed by the PI (E.M.-B.) to ensure agreement on PTSDsymptom ratings and diagnosis. No instances of diagnostic disagreement between the CAPS interviewers and PI were noted.
Alcohol Use Disorders Identification Test (AUDIT; Babor, de la Fuente, Sauders, & Grant, 1992)
The AUDIT is a 10-item self-report screening measure developed by the World Health Organization to identify individuals with alcohol problems (Babor et al., 1992). There is a large body of literature attesting to the psychometric properties of the AUDIT (e.g., Saunders, Aasland, Babor, de la Fuente, &Grant, 1993). The current study utilized: (1) a composite of the frequency item and quantity item (items 1 and 2) to index alcohol consumption; and (2) the total score to measure alcohol use problems (Babor et al., 1992). Individuals scoring an 8 or higher on the AUDIT total likely meet criteria for at least “moderate” alcohol problems (Babor et al., 1992).
Barratt Impulsiveness Scale (BIS-11; Patton, Stanford, & Barratt, 1995)
The BIS-11 is a 30-item self-report measure, on which respondents indicate, on a 4-point Likert-type scale (1 = rarely/never to 4 = almost always/always), the extent to which they behave impulsively (e.g., “I do things without thinking”). The BIS is a well-established measure of impulsive personality traits with good psychometric properties (Stanford et al., 2009). The total BIS-11 score (α = .83) was computed in the current study to index general levels of impulsivity.
Distress Tolerance Scale (DTS; Simons &Gaher, 2005)
The DTS is a 15-item self-report measure, on which respondents indicate, on a 5-point Likert-type scale (1 = “strongly agree” to 5 = “strongly disagree”), the extent to which they believe they can experience and withstand distressing emotional states (e.g., “I can’t handle feeling distressed or upset,” reverse-coded; Simons &Gaher, 2005). The total DTS score (α = .94) was employed as a global index of perceived distress tolerance.
Drinking Motives Questionnaire-Revised (DMQ-R; Cooper, 1994)
The DMQ-R is a 20-item self-report measure designed to index reasons why people might be motivated to drink alcoholic beverages. Participants rate, on a 5-point scale (1 = almost never/never to 5 = almost always/always), how frequently each of the listed reasons motivate them to drink alcoholic beverages. The DMQ-R demonstrates good structural and criterion validity, as well as internal consistency, with alpha’s for each subscale ranging from .81 to .94 (Cooper, 1994; MacLean & Lecci, 2000). The Coping motives subscale (e.g., “To forget your worries;” α = .88) was utilized in the current study.
Procedure
The current data are derived from a larger investigation focused on emotional reactivity processes. Individualswho responded to newspaper advertisements and community fliers for a study on emotion completed a brief phone screen andwere scheduled for a session in the laboratory to determine eligibility and collect study data. Upon arrival to the laboratory, participants provided informed consent and were administered the SCID-I/NP to determine eligibility. Eligible participants were administered the CAPS and a battery of self-report measures; they were compensated $30. Ineligible participants were compensated $10 for participating in the SCID-I/NP administration. Eligible participants completed a second laboratory session; however, all data in the current study were collected at the baseline session.Exclusionary criteria for the laboratory session of the larger study were: (1) limited mental competency and/or the inability to provide informed verbal and written consent, (2) current (past month) suicidal ideation, (3) evidence of current or past psychotic-spectrum symptoms, (4) current psychotropic medication use, and (5) lifetime panic disorder diagnosis. Inclusionary criteria were: (1) being between the ages of 18-65, and (2) endorsing either a recent(i.e., past 2-year) history of nonclinical, unexpected panic attacks or no lifetime history of panic attacks on the SCID-I/NP.
Data Analysis
First, a series of zero-order correlations was conducted to examine associations among key variables. Second, the mediating role of distress tolerance in the relation between impulsivity and alcohol use coping motives was examined, using Baron and Kenny’s (1986) recommended test of mediation. Specifically, the test requires the following series of multiple regressions: (1) the predictor variable (i.e., BIS – total score) must significantly predict the criterion variable (i.e., Coping motives), as depicted in Figure 1 – Path C; (2) the predictor variable (i.e., BIS – total score) must significantly predict the mediator (i.e., DTS - total score), as depicted in Figure 1 – Path A; and (3) when the predictor (i.e., BIS – total score) and mediator (i.e., DTS – total score) are entered simultaneously into a third multiple regression, the mediator must significantly predict the outcome, and the relation between the predictor and outcome is either diminished (partial mediation) or non-existent (full mediation). Per current recommendations, bootstrapping analyses were conducted as a test of indirect effects (see Preacher & Hayes, 2008). In the current mediational test, PTSD symptom severity (CAPS – total score) and alcohol use problems (AUDIT – total score) were entered as covariates in step one of all regression equations when Coping motives was the criterion variable.
Results
Sample Characteristics
46.4% of the sample met criteria for one or more current (past month) axis I disorders. Participants with current psychopathology met criteria for an average of 1.05 (SD = 1.57) diagnoses. 16.7% of the total sample met current (past month) criteria for Social Anxiety Disorder, 15.5% for Generalized Anxiety Disorder, 9.5% for Specific Phobia, 9.5% for Dysthymia, 8.3% for Major Depressive Disorder, 6.0% for Obsessive Compulsive Disorder, 4.8% for PTSD [assessed by the CAPS], 2.4% for Eating Disorder Not Otherwise Specified, and 1.2% for Bipolar II Disorder. 54.8% met criteria for nonclinical panic attacks in the past two years. With regard to current (past 6 months) substance use disorders, 7.1% of the total sample met criteria for alcohol abuse, 8.3% for alcohol dependence, 8.3% for cannabis abuse, 7.1%for cannabis dependence, and 1.2% for amphetamine dependence.
84.6% of the sample reported drinking alcohol at least 2-4 times per month. Participants scored an average of 10.35 (SD = 6.68) on the AUDIT. Approximately 59.5% of the sample met criteria for at least moderate alcohol problems on the AUDIT, defined as a total score of 8 or greater (Babor et al., 1992). [Note: AUDIT scores and alcohol use disorder diagnoses on the SCID-I/NP likely do not correspond given the differences in the time frames assessed (i.e., past year and past month, respectively).]
With regard to the Life Events Checklist of the CAPS (Blake et al., 1995), participants reported an average of 8.21 (SD = 6.24) lifetime traumatic events. With regard to participants’ “worst” Criterion A event, the most commonly endorsed events were sudden, unexpected death of a loved one (21.4%), transportation accident (14.3%) and sexual assault (14.3%). Participants scored an average of 13.96 (SD = 17.12; Range = 0-66) on CAPS severity ratings, indicating low levels of symptoms (Weathers, et al., 1999).
Zero-Order Correlations
See Table 1 for zero-order correlations and descriptive data for key variables1. Impulsivity was significantly associated with Coping alcohol use motives (r = .41, p< .01). Distress tolerance and PTSD symptom severity were significantly correlated with Coping alcohol use motives (r = -.46, r = .43, p’s< .01, respectively). Alcohol consumption was significantly associated with impulsivity (r = .36, p < .01) but not distress tolerance or Coping alcohol use motives (p’s> .05). The alcohol use problem index (AUDIT – total score) was significantly correlated with all variables except distress tolerance (p> .05).
Table 1.
Zero-Order Correlations and Descriptive Data among Theoretically-Relevant Variables
| Variablea | 1 | 2 | 3 | 4 | 5 | 6 | Mean (SD) |
|---|---|---|---|---|---|---|---|
| 1. Alcohol Consumption | - | .77** | .27* | .36** | .15 | .13 | 5.84 (4.22) |
| 2. AUDIT – Total | - | - | .41** | .41** | -.03 | .34** | 10.35 (6.68) |
| 3. CAPS – Total | - | - | - | .38** | -.39** | .43** | 13.96 (17.12) |
| 4. BIS – Total | - | - | - | - | -.39** | .41** | 66.16 (10.73) |
| 5. DTS – Total | - | - | - | - | - | -.46** | 46.73 (13.15) |
| 6. DMQ-R: Coping | - | - | - | - | - | - | 10.69 (5.12) |
Note:
p< .05;
p< .01;
Alcohol Consumption – Quantity * Frequency; AUDIT Total – alcohol use problems (Babor et al., 1992); CAPS – Total: Clinician Administered PTSD Scale total symptom severity score (Blake et al., 1995); BIS – Total: Barratt Impulsiveness Scale total score (Patton et al., 1995); DTS-Total: Distress Tolerance Scale score (Simons &Gaher, 2005); DMQ-R: Coping – Drinking Motives Questionnaire-Revised (Coping motives subscale; Cooper, 1994).
Mediation Analyses
The data met assumptions of normality with regard to skewness and kurtosis. See Table 2 for a summary of mediation analyses2. First, there was a significant association between the predictor (impulsivity; BIS-Total) and criterion (alcohol use coping motives; DMQ-R: Coping subscale) variables, after controlling for PTSD symptom severity (CAPS-total) and alcohol use problems (AUDIT - total; see Table 2 - analysis 2 and Figure 1 - Path C). Second, the predictor (impulsivity; BIS-Total) was significantly related to the proposed mediator, distress tolerance (DTS-Total; see Table 2 – analysis 1 and Figure 1 - Path A). Finally, the relation between impulsivity (BIS-Total) and alcohol use coping motives, the predictor and criterion variables, was reduced and rendered non-significant (β = 0.10 versus β = 0.22) by the inclusion of distress tolerance (DTS-Total) in the model (see Table 2 – analysis 3). Bootstrap analyses of 1,000 samples supported full mediation (estimate for indirect effects = .06; 95% confidence interval = .02-.12).
Table 2.
Test of Distress Tolerance as a Mediator in the Association between Impulsivity and Alcohol Use Coping Motivesa
| R2 | t (each predictor) | β | sr2 | p | |
|---|---|---|---|---|---|
| Criterion Variable: Distress Tolerance: Test of Path A | |||||
| Step 1 | .18 | < .001 | |||
| Impulsivity (BIS-Total) | -4.40 | -.43 | .18 | < .001 | |
| Criterion Variable: Alcohol Use Coping Motives: Test of Path C | |||||
| Step 1 | .24 | < .001 | |||
| CAPS-Total | 2.99 | .31 | .08 | < .01 | |
| AUDIT-Total | 2.58 | .27 | .06 | < .05 | |
| Step 2 | .04 | < .05 | |||
| Impulsivity (BIS-Total) | 2.00 | .22 | .04 | < .05 | |
| Criterion Variable: Alcohol Use Coping Motives: Test of Paths C’ and B | |||||
| Step 1 | .23 | < .001 | |||
| CAPS-Total | 3.03 | .33 | .09 | < .01 | |
| AUDIT-Total | 2.19 | .24 | .05 | < .05 | |
| Step 2 | .12 | < .01 | |||
| Impulsivity (BIS-Total) | .88 | .10 | .01 | .38 | |
| Distress Tolerance (DTS-Total) | -3.09 | -.33 | .08 | < .01 | |
Distress Tolerance: DTS-Total: Distress Tolerance Scale score (Simons &Gaher, 2005); Impulsivity: BIS – Total: Barratt Impulsiveness Scale total score (Patton et al., 1995); Alcohol Use Coping Motives: DMQ-R: Coping – Drinking Motives Questionnaire-Revised (Coping motives subscale; Cooper, 1994); CAPS – Total: Clinician Administered PTSD Scale total symptom severity score (Blake et al., 1995); AUDIT – Total: Alcohol Use Disorders Identification Test total score (Babor et al., 1992).
Per recommendations for cross-sectional meditational tests (e.g., Preacher & Hayes, 2004), a reverse mediation model was tested. Alcohol use coping motives did not mediate the relation between impulsivity (BIS-Total) and distress tolerance (DTS-Total), as impulsivity remained a significant predictor of distress tolerance (t = -2.53, β = -.28, p< .05) when entered concurrently with alcohol use coping motives (t = -3.09, β = - .34, p< .05).
Discussion
The present investigation evaluated the mediating role of distress tolerance in the association between impulsivity and alcohol use coping motives. Findings were consistent with hypotheses. First, impulsivity evidenced a significant positive association with alcohol use coping motives, even after accounting for the variance contributed by PTSD symptom severity and alcohol use problems. Although the effect size was small, this finding extends past work documenting significant associations between impulsivity and problem drinking outcomes. Thus, heightened levels of impulsivity, indexed post-trauma, might increase the likelihood that trauma-exposed individuals use alcohol in efforts to alleviate emotional distress. This finding is consistent with emerging evidence, suggesting that individuals with higher levels of impulsivity tend to seek more immediate negative reinforcement opportunities, such as alcohol use, when experiencing greater degrees of negative affect (Cyders& Smith, 2008).
Second, impulsivity was negatively associated with distress tolerance, such that trauma-exposed individuals with higher levels of impulsivity reported lower levels of distress tolerance. It is possible that individuals higher in impulsivity develop a belief that they cannot tolerate negative affective states, due to a propensity to prematurely opt for negative reinforcement opportunities; however, due to the cross-sectional design of the current study, causality cannot be inferred. It is also possible that lower levels of distress tolerance temporally predict higher levels of impulsivity over time (Cyders& Smith, 2008). Further research is needed to examine the differential and temporal associations among behavioral and self-report indices of distress tolerance, impulsivity, and alcohol use motives.
Finally, distress tolerance partially mediated the association between impulsivity and alcohol use coping motives, after controlling for the effects of PTSD symptom severity and alcohol use problems. It is possible that individuals high in impulsivity are more motivated to drink to avoid negative affective states due to a belief that they cannot tolerate such states. Due to the cross-sectional nature of the finding, the temporal order implicit to the mediational model cannot be ascertained. Therefore, prospective replication and extension of this finding is a necessary next step. Specifically, future studies addressing the temporal order of the observed associations are warranted.
Clinically, it may be worth investigating whether trauma-exposed individuals with alcohol use problems benefit from intervention strategies designed to target impulsivity and distress tolerance (e.g., distress tolerance component of Dialectical Behavior Therapy; Linehan, 1993). Such interventions may improve an individual’s ability to cope with PTSD symptoms and related negative mood states without using alcohol. Additionally, it may be useful to explore the role of impulsivity and distress tolerance inthe onset and maintenance of alcohol use problems among trauma-exposed individuals. If impulsivity and distress tolerance are fundamentally linked to emotional vulnerability, as implied by the alcohol coping motives effect observed here, these factors may similarly be associated with other emotionally-salient aspects of alcohol use (e.g., perception of withdrawal symptoms, abstinence duration) among trauma-exposed populations.
Several limitations of the current investigation warrant comment. First, the investigation was based on a racially homogeneous sample of community-recruited trauma-exposed participants who consumed alcohol to varying degrees and reported mostly subclinical levels of PTSD symptoms. It is important for future work to extend these findings with more diverse samples. Second, participantsreported a variety of types of trauma; therefore, the specificity of the documented distress tolerance-alcohol use coping motives association to specific forms of trauma cannot be determined. Replicating the current findings with samples recruited using a variety of strategies is warranted. Third, the study utilized a cross-sectional design and relied onself-report. Therefore, temporal order and causality cannot be inferred, and the potential influence of method-variance effects must be considered. This line of inquiry could be strengthened by the implementation of multi-method assessments. Fourth, it is likely that non-PTSD axis I psychopathology accounts for significant variance in coping-oriented alcohol use motives. Similarly, type of trauma, as well as the cumulative effects of multiple, related traumas, may impact individuals’ coping strategies. Future studies with larger sample sizes would benefit from exploring such relations among trauma-exposed samples. Fifth, the current investigation utilized one measure of impulsivity. Given that multiple behavioral and self-report measures of impulsivity exist (including measures of negative urgency), future work would benefit from investigating alternative impulsivity measures in relation to coping motives.Finally, although the present mediational test suggests that there may be explanatory merit for a distress tolerance mechanism linking PTSD symptoms and alcohol use coping motives, it is not necessarily mutually exclusive compared to other pathways. Future work may benefit from testing alternative models in efforts to better understand coping-oriented drinking among trauma exposed individuals.
Acknowledgments
This research was supported by a National Institute on Mental Health National Research Service Award (1 F31 MH080453-01A1) awarded to Erin C. Marshall-Berenz. The authors acknowledge the support of Dr. Michael J. Zvolensky, Ph.D., director of the Anxiety and Health Research Laboratory (AHRL) at the University of Vermont. The data presented in the manuscript were collected in the AHRL under direct supervision of Dr. Zvolensky. The views expressed here reflect those of the authors and do not necessarily represent those of the Department of Veterans Affairs.
Footnotes
Sex differences in variables studied were examined. There was not a significant correlation between participant sex and coping-oriented alcohol use motives. Similarly, although evidencing a slightly larger effect among men, correlations between impulsivity and coping motives were significant among men and women (r = .59 and .33, respectively, p’s< .05). Significant correlations were also found among men and women between impulsivity and distress tolerance scores (r = -.51 and -.40, respectively, p’s< .05).
The mediation model is not significant for non-coping alcohol use motives (i.e., enhancement, social, or conformity motives).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text revision. [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, Grant M. The alcohol use disorders identification test: Guidelines for use in primary care. Geneva: World Health Organization; 1992. WHO Publication No. 92.4. [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Keough ME, Schmidt NB. Problematic alcohol and cannabis use among young adults: The roles of depression and discomfort and distress tolerance. Addictive Behaviors. 2007;32:1957–1963. doi: 10.1016/j.addbeh.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casada JH, Roache JD. Behavioral inhibition and activation in posttraumatic stress disorder. Journal of Nervous and Mental Disease. 2005;193:102–109. doi: 10.1097/01.nmd.0000152809.20938.37. [DOI] [PubMed] [Google Scholar]
- Charney DA, Zikos E, Gill KJ. Early recovery from alcohol dependence: Factors that promote or impede abstinence. Journal of Substance Abuse Treatment. 2010;38:42–50. doi: 10.1016/j.jsat.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. doi: 10.1037/1040-3590.6.2.117. [DOI] [Google Scholar]
- Cyders MA, Smith GT. Emotion-based dispositions to rash action: Positive and negative urgency. Psychological Bulletin. 2008;134:807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment. 2007;19:107–118. doi: 10.1037/1040-3590.19.1.107. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Kahler CW, Strong DR, Brown RA. Psychological distress tolerance and duration of most recent abstinence attempt among residential treatment-seeking substance abusers. Psychology of Addictive Behaviors. 2005;19:208–211. doi: 10.1037/0893-164X.19.2.208. [DOI] [PubMed] [Google Scholar]
- Dixon LJ, Leen-Feldner EW, Ham LS, Feldner MT, Lewis SF. Alcohol use motives among traumatic event-exposed, treatment-seeking adolescents: Associations with posttraumatic stress. Addictive Behaviors. 2009;34:1065–1068. doi: 10.1016/j.addbeh.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM-IV Disorders. New York: Biometrics Research Department; 1994. [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- James LM, Taylor J. Impulsivity and negative emotionality associated with substance use problems and cluster B personality in college students. Addictive Behaviors. 2007;32:714–727. doi: 10.1016/j.addbeh.2006.06.012. [DOI] [PubMed] [Google Scholar]
- Kaysen D, Dillworth TM, Simpson T, Waldrop A, Larimer ME, Resick PA. Domestic violence and alcohol use: Trauma-related symptoms and motives for drinking. Addictive Behaviors. 2007;32:1272–1283. doi: 10.1016/j.addbeh.2006.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- MacLean MG, Lecci L. A comparison of models of drinking motives in a university sample. Psychology of Addictive Behaviors. 2000;14:83–87. doi: 10.1037/0893-164X.14.1.83. [DOI] [PubMed] [Google Scholar]
- Marshall-Berenz EC, Vujanovic AA, Bonn-Miller MO, Bernstein A, Zvolensky MJ. Multi-method study of distress tolerance and PTSD symptom severity in a trauma-exposed community sample. Journal of Traumatic Stress. 2010;23:623–630. doi: 10.1002/jts.20568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane AC, Browne D, Bryant RA, O’Donnell M, Silove D, Creamer M, Horsley K. A longitudinal analysis of alcohol consumption and the risk of posttraumatic symptoms. Journal of Affective Disorders. 2009;118:166–172. doi: 10.1016/j.jad.2009.01.017. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. The American Journal of Psychiatry. 2001;158:1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768∷AID-JCLP2270510607>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The distress tolerance scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. doi: 10.1007/s11031-005-7955-3. [DOI] [Google Scholar]
- Stanford MS, Mathias CW, Dougherty DM, Lake SL, Anderson NE, Patton JH. Fifty years of the Barratt impulsiveness scale: An update and review. Personality and Individual Differences. 2009;47:385–395. doi: 10.1016/j.paid.2009.04.008. [DOI] [Google Scholar]
- State of Vermont Department of Health. 2007 Retrieved June 30, 2007, from http://www.healthyvermonters.info/
- Stewart SH. Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin. 1996;120:83–112. doi: 10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Israeli AL. Substance abuse and co-occurring psychiatric disorders in victims of intimate violence. In: Wekerle C, Wall A, editors. The violence and addiction equation: Theoretical and clinical issues in substance abuse and relationship violence. New York: Brunner-Routledge; 2002. pp. 98–122. [Google Scholar]
- Vujanovic AA, Marshall-Berenz EC, Zvolensky MJ. Posttraumatic stress and alcohol use motives: The incremental and mediating role of distress tolerance. Journal of Cognitive Psychotherapy. doi: 10.1891/0889-8391.25.2.130. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11:124–133. doi: 10.1037/1040-3590.11.2.124. [DOI] [Google Scholar]


