Abstract
Background
There is speculation that the volume of percutaneous coronary interventions (PCIs) has been decreasing over the past several years. Published studies of PCI volume have evaluated regional or hospital trends, but few have captured national data. This study describes the use of coronary angiography and revascularization methods in Medicare patients from 2001 to 2009.
Methods and Results
This retrospective study used data from the Centers for Medicare & Medicaid Services from 2001 to 2009. The annual number of coronary angiograms, PCI, intravascular ultrasound, fractional flow reserve, and coronary artery bypass graft (CABG) surgery procedures were determined from billing data and adjusted for the number of Medicare recipients. From 2001 to 2009, the average year-to-year increase for PCI was 1.3% per 1000 beneficiaries, whereas the mean annual decrease for CABG surgery was 5%. However, the increase in PCI volume occurred primarily from 2001 to 2004, as there was a mean annual rate of decline of 2.5% from 2004 to 2009; similar trends were seen with diagnostic angiography. The use of intravascular ultrasound and fractional flow reserve steadily increased over time.
Conclusions
This study confirms recent speculation that PCI volume has begun to decrease. Although rates of CABG have waned for several decades, all forms of coronary revascularization have been declining since 2004.
Keywords: angiography, catheterization, epidemiology, angioplasty, revascularization
Since the development of coronary angioplasty >3 decades ago, there have been several studies that have cited both an increase in percutaneous coronary intervention (PCI) and a decrease in coronary artery bypass graft (CABG) surgery volumes in the treatment of coronary artery disease within the United States and abroad.1–10 There has been speculation that the volume of PCIs has started to decline recently, however, in light of the increasing use of drug-eluting stents (DES), advances in medical therapy, and the publication of data from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial demonstrating that coronary revascularization does not reduce the risk of major cardiovascular events over and above optimal medical therapy in patients with stable angina.11,12 We analyzed Centers for Medicaid & Medicare Services procedure billing data from 2001 to 2009 to report trends in cardiac catheterizations (diagnostic and interventional), use of PCI (angioplasty and stents), CABG surgeries, and the use of intravascular ultrasound (IVUS) and fractional flow reserve (FFR) during angiography.
Methods
This retrospective study used data from the Centers for Medicare & Medicaid Services from 2001 to 2009 through the Medicare utilization statistics data set, Part B. Using billed American Medical Association Current Procedural Terminology (CPT) codes from that period, the total number of diagnostic catheterizations (CPT codes 93508 to 93529), PCIs, and CABG (CPT codes 33510 to 33536) surgeries were compiled. PCI was broken down into angioplasty (CPT codes 92982 and 92984; used as a primary treatment modality, not in combination with other therapies) and stenting (both single [CPT code 92980] and multivessel [CPT code 92981] stenting). Diagnostic catheterizations were defined as procedures in which only coronary angiography was performed; the angiographic component of PCI procedures was not included in this number. Diagnostic catheterization and PCI rates for a given year were then combined into a category called “total catheterizations.” The total CABG and PCI rates for a given year comprised the category “total coronary revascularizations.”
For reimbursement purposes, Medicare recognizes 3 coronary arteries: right coronary, left circumflex coronary, and left anterior descending coronary. In multivessel PCI, it is possible that a physician may report up to 3 percutaneous interventions if an intervention is performed in each of the 3 coronary arteries or their branches. The first reported procedure must use a primary code (CPT codes 92980 and 92982) corresponding to the most complex procedure performed. The procedures performed in the other 1 or 2 coronary arteries (including their branches) are reported with the CPT add-on codes (CPT codes 92981 and 92984). Therefore, multivessel PCI, as per Medicare billing guidelines, was defined as intervention in a vessel different from the vessel in which an initial stent was placed, billed separately and in addition to the initial vessel that received intervention. This definition differentiated multivessel stenting from both single-vessel stenting and multiple stents being placed within a single vessel (which was billed as single-vessel stenting).
The total number of annual fee-for-service Medicare beneficiaries during this period was gathered from the Annual Reports of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds during this period. Using these numbers as denominators, each procedure was reported per 1000 Medicare beneficiaries for each given year to account for annual changes in this population. Similar data on the use of IVUS (CPT codes 92978 and 92979) and FFR (CPT codes 93571 and 93572) during angiography also was collected on the basis of billing codes. Notably, data on IVUS use during 2004 was not available because Medicare only released data for high-volume procedures for that year; thus, IVUS did not qualify. Because this research used a limited data set with deidentified information, the University of Washington Institutional Review Board waived the formal application for approval to perform human subject research for this project.
Results
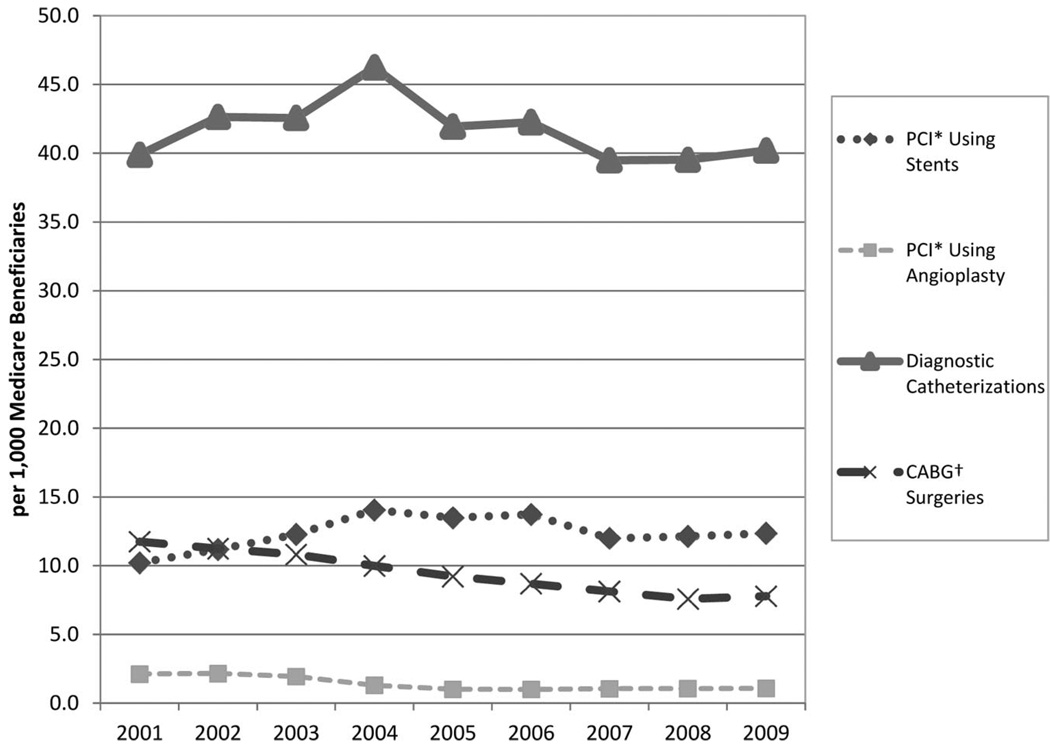
The total number of coronary procedures billed each year between 2001 and 2009 in the Medicare population are shown in the Table; procedures per 1000 Medicare beneficiaries are shown in Figure 1. The year-to-year percent change in procedures per 1000 beneficiaries is shown in Figure 2. Although the overall number of diagnostic catheterizations per 1000 Medicare beneficiaries increased by only 0.8% in 2009 compared to 2001, the year-to-year trends clearly demonstrate a marked increase in the number of catheterizations from 2001 to 2004, with an average increase of 5.1% per year per 1000 patients, followed by a mean decrease of 2.7% per year between 2004 and 2009 (Table).
Table.
Total Coronary Diagnostic and Treatment Procedures Billed in the Medicare Population From 2001 to 2009
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | |
|---|---|---|---|---|---|---|---|---|---|
| Diagnostic catheterizations | 1 075 623 | 1 180 899 | 1 201 590 | 1 315 515 | 1 193 200 | 1 166 972 | 1 063 429 | 1 040 274 | 1 047 945 |
| PCI using angioplasty | 57 114 | 59 830 | 54 659 | 36 972 | 28 564 | 27 492 | 28 134 | 27 790 | 28 100 |
| PCI using stents | 275 037 | 309 829 | 346 711 | 399 558 | 383 888 | 379 280 | 322 884 | 319 567 | 322 034 |
| Multivessel stenting | 32 034 | 36 915 | 39 952 | 47 320 | 49 738 | 50 088 | 38 128 | 37 609 | 38 053 |
| Total PCIs | 332 151 | 369 659 | 401 370 | 436 530 | 412 452 | 406 772 | 351 018 | 347 357 | 350 134 |
| Total catheterizations | 1 407 774 | 1 550 558 | 1 602 960 | 1 752 045 | 1 605 652 | 1 573 744 | 1 414 447 | 1 387 631 | 1 398 079 |
| CABG surgeries | 316 951 | 311 096 | 305 240 | 283 818 | 262 396 | 240 252 | 218 594 | 199 358 | 203 025 |
| Total coronary revascularizations | 649 102 | 680 755 | 706 610 | 720 348 | 674 848 | 647 024 | 569 612 | 546 715 | 553 159 |
| IVUS | N/A | N/A | 21 746 | N/A | 30 781 | 35 251 | 35 532 | 40 368 | 40 767 |
| FFR | N/A | N/A | N/A | N/A | 6 176 | 7 930 | 8 572 | 10 606 | 10 811 |
| Fee-for-service population | 26 959 000 | 27 686 000 | 28 232 000 | 28 440 000 | 28 443 000 | 27 614 000 | 26 933 000 | 26 319 000 | 26 064 000 |
Figure 1.
Trends in total coronary procedures per 1000 Medicare beneficiaries from 2001 to 2009.
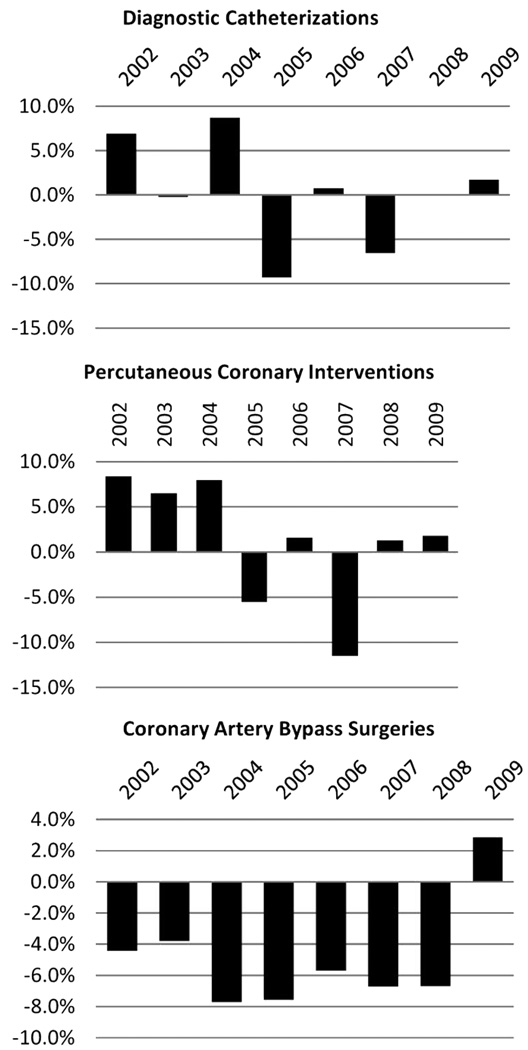
Figure 2.
Year-to-year percent change in coronary procedures per 1000 Medicare beneficiaries.
From 2001 to 2009, the use of PCI with stenting increased from 10.2 to 12.4 per 1000 beneficiaries. Similar to the temporal trend seen with diagnostic catheterizations between 2001 and 2004, the mean year-to-year change in coronary stenting increased 11.3% per year per 1000 patients, but from 2004 to 2009, there was a mean annual decrease of 2.4% (Figure 2). PCI using balloon angioplasty alone decreased steadily between 2002 and 2005 and remained at roughly 1 per 1000 beneficiaries for the remainder of the period (Figure 1). Overall, the average annual increase in PCI (stenting and angioplasty alone) per 1000 beneficiaries was 1.3% over the 9-year period. The increase in volume primarily was seen between 2001 and 2004, whereas a mean annual rate of decline of 2.5% was seen between 2004 and 2009 (Figure 2).
The use of coronary angiography and PCIs increased annually from 2001 and peaked in 2004, whereas there were notable percentage decreases in 2005 and 2007. In 2009, the number of diagnostic catheterizations and PCI procedures increased slightly compared to 2008, but were still well below the 2004 levels. In contrast, CABG procedures declined consistently from 2001 to 2008 by ≈4% to 7% per year followed by a slight increase in CABG procedures per beneficiary in 2009. The ratio of PCI to CABG procedures performed increased steadily from 1.05 in 2001 to 1.72 in 2009, demonstrating that the rate of decline in CABG was greater than PCI over the entire period. The number of multivessel stenting procedures remained relatively constant over time at ≈12% of PCIs using stents (Table).
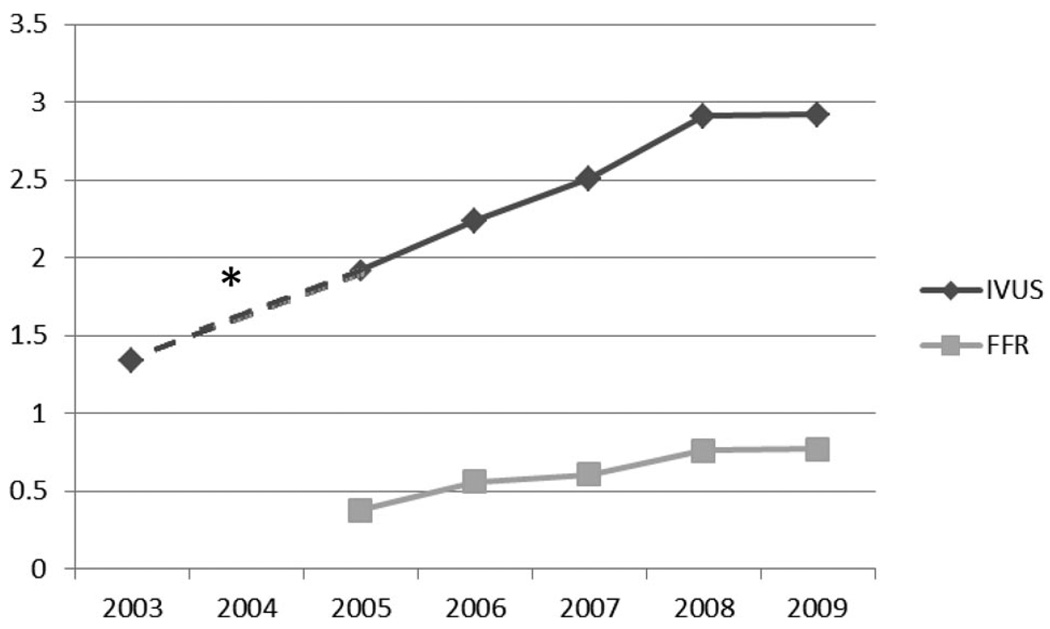
IVUS and FFR use per catheterization during this time period are shown in Figure 3. Data within the Medicare population was available starting in 2003 for IVUS and in 2005 for FFR. Total IVUS procedures doubled from 0.77 in 2003 to 1.53 per 1000 beneficiaries in 2009. FFR was used less frequently than IVUS during this time, but increased from 0.22 to 0.41 per 1000 beneficiaries (Table), with the percentage of catheterizations using FFR increasing by 101% from 2005 to 2009 (Figure 3).
Figure 3.
Percentage of total catheterizations in which IVUS and FFR were used in the Medicare population from 2003 to 2009. *2004 data were not available for IVUS.
Discussion
The most recent epidemiological data from 2007 showed that the overall death rate from cardiovascular disease in the United States was 204.3 per 100 000 persons, making it the leading cause of death in both men and women.13 However, the age-adjusted death rate for coronary heart disease has been steadily decreasing since the 1980s, likely as a result of improved risk factor modification and cardiovascular therapies. 14 The trends in coronary catheterization volumes observed in our study from 2001 to 2004 are consistent with previous reports that showed steady increases in PCI volumes during that period.15 Our data also show that the total and per-beneficiary numbers of diagnostic and interventional catheterizations in the Medicare population have been decreasing steadily since 2004. Although there was stabilization in the number of catheterizations in 2009, the overall trend from 2004 to 2009 remained in decline, with the total number of coronary revascularizations (PCI and CABG combined) declining over the 9-year period studied. The rate of decline in CABG surgeries continued to outpace that of the decline in PCI.
There are numerous possible explanations about why coronary catheterization rates have started to decline over the past several years. One explanation might be increased treatment of atherosclerotic risk factors over the past decade. It has been previously estimated that 44% of the reduction in US deaths due to coronary heart disease from 1980 to 2000 was due to risk factor modification.14 The Centers for Disease Control and Prevention recently published a report that showed that the prevalence of smoking among US adults decreased by 3.5% from 1998 to 2008.16 There also are data showing that an increasing percentage of the US population is achieving target blood pressure and cholesterol goals.17,18 The Medical Expenditure Panel Survey published a report in 2008 that showed nearly a doubling in statin prescriptions from 2000 to 2005 (89.7 versus 173.7 million) in the US population. 19 There is also evidence for increasing prescriptions for β-blockers among patients with known coronary artery disease.20
Another possible explanation for these trends could be the increasing use of DES during this period. After their initial approval by the US Food and Drug Administration in 2003, DES were used in as many as 90% of all PCIs in the United States by 2006.21 In a similar Medicare population, it was reported that the use of bare-metal stents in PCI decreased from 89% in 2001 to 19% in 2004. Similarly, the use of DES increased to 75% of all stents placed in this population in 2008. Concurrently, significant reductions were found in the need for repeat revascularization in this population over that period.15 The reduction of in-stent restenosis from the use of DES could have led to fewer repeat angiograms and repeat revascularization procedures. On the other hand, the concerns for increased stent thrombosis of DES in the latter part of this period also may have contributed to the decrease in PCI seen after 2004.22
Additionally, it is possible that more patients with stable angina are being primarily medically managed or evaluated with noninvasive imaging before diagnostic catheterization or coronary revascularization. In a recent single-center study, patients referred for angiography following publication of the COURAGE trial were more often treated with aggressive disease-modifying agents before referral for catheterization than were pre-COURAGE patients. In the same study, it also was noted that patients with stable angina and significant coronary artery disease on angiography were more likely to receive medical therapy rather than revascularization as initial treatment management post-COURAGE.20 An increased use of primary medical management along with an increasing use of noninvasive coronary imaging23 likely have contributed to decreasing catheterization and revascularization rates, although the COURAGE trial itself would not explain our results because it was not published until 2007.
During the same period in which PCI rates have been decreasing, the rates of IVUS and FFR use per catheterization have been steadily increasing within the Medicare population. This increased use could be related to the increased complexity of coronary artery disease being managed percutaneously. Conversely, the increased hemodynamic assessment of coronary lesions using FFR and anatomic assessment using IVUS could have contributed to the decrease in PCI. However, these changes in procedure volume were comparatively small, and their contribution to the overall changes in revascularization volumes was likely trivial.
There are several limitations to our study. First, patient-level data, the indication for each type of procedure, procedure priority (emergent versus nonemergent), and stent type (bare metal versus drug eluting) were not available for our study population, making it difficult to evaluate the contribution of these factors on the observed trends. Another limitation, inherent to studies based on physician billing codes, is that we were unable to account for the contribution of improper billing on our results. Underbilling due to accidental physician omission or overbilling for multivessel PCI (eg, billing for multivessel PCI when stenting the left anterior descending coronary artery plus a diagonal artery, which should be billed as single-vessel PCI) are 2 such examples. Finally, the older population within Medicare may not reflect the patient population of the United States as whole because trends in the use of diagnostic and interventional cardiac procedures may differ between older and younger patients. Nevertheless, Medicare is the largest insurance carrier in the United States and is likely representative of national trends.15
In summary, the use of diagnostic and interventional coronary catheterizations within the Medicare population has been steadily declining since 2004. Although there was some stabilization of these trends in 2009, they are reminiscent of the decline in CABG rates that started in the late 1980s, which was initially attributed to the expanding use of PCI. Given the declines in both CABG and PCI since 2004, the use of PCI does not appear to entirely explain the decline in CABG rates. Potentially, the decline in CABG surgery volume was simply the canary in the coal mine that signaled larger-scale reductions in the need for coronary revascularization as risk factor modification and cardiovascular therapeutics continue to improve.
WHAT IS KNOWN.
- In prior decades, diagnostic and interventional coronary catheterization rates have increased, whereas there has been a concurrent decrease in coronary artery bypass graft (CABG) surgery rates in the United States.
- Several factors, such as the publication of the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial, may have influenced rates of diagnostic and interventional coronary catheterization in recent years.
WHAT THE STUDY ADDS.
- Diagnostic and interventional coronary catheterization rates within the Medicare population have steadily declined since 2004.
- Rates of intravascular ultrasound and fractional flow reserve use per catheterization have steadily been increasing within the Medicare population over the past several years.
- Given the declines in both CABG surgery and percutaneous coronary intervention since 2004, the use of percutaneous coronary intervention does not appear to entirely explain recent declines in CABG surgery rates.
Acknowledgments
We thank Stephan D. Fihn, MD, for his contribution to this manuscript.
Sources of Funding
This publication was made possible by grant KL2 RR025015 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH). This publication was made possible by Grant Number KL2 RR025015 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Footnotes
Reprints: Information about reprints can be found online at http://www.lww.com/reprints
Disclosures
None.
References
- 1.Goodman S, Huang W, Yan A, Budaj A, Kennelly B, Gore J, Fox K, Goldberg R, Anderson FJ. The expanded global registry of acute coronary events: baseline characteristics, management practices, and hospital outcomes of patients with acute coronary syndromes. Am Heart J. 2009;158:193–201. doi: 10.1016/j.ahj.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Eagle K, Nallamothu B, Mehta R, Granger C, Steg P, Van de Werf F, López-Sendón J, Goodman S, Quill A, Fox K. Trends in acute reperfusion therapy for ST-segment elevation myocardial infarction from 1999 to 2006: we are getting better but we have got a long way to go. Eur Heart J. 2008;29:609–617. doi: 10.1093/eurheartj/ehn069. [DOI] [PubMed] [Google Scholar]
- 3.Gogo PJ, Dauerman H, Mulgund J, Ohman E, Patel M, Cohen D, Saucedo J, Harrington R, Gibler W, Smith SJ, Peterson E, Roe M. Changes in patterns of coronary revascularization strategies for patients with acute coronary syndromes (from the CRUSADE quality improvement initiative) Am J Cardiol. 2007;99:1222–1226. doi: 10.1016/j.amjcard.2006.12.037. [DOI] [PubMed] [Google Scholar]
- 4.Gerber Y, Rihal C, Sundt TR, Killian J, Weston S, Therneau T, Roger V. Coronary revascularization in the community. A population-based study, 1990 to 2004. J Am Coll Cardiol. 2007;50:1223–1229. doi: 10.1016/j.jacc.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 5.Movahed M, Ramaraj R, Jamal M, Hashemzadeh M. Nationwide trends in the utilization of multivessel percutaneous coronary intervention (MVPCI) in the United States across different gender and ethnicities. J Interv Cardiol. 2009;22:247–251. doi: 10.1111/j.1540-8183.2009.00467.x. [DOI] [PubMed] [Google Scholar]
- 6.Ulrich M, Brock D, Ziskind A. Analysis of trends in coronary artery bypass grafting and percutaneous coronary intervention rates in Washington state from 1987 to 2001. Am J Cardiol. 2003;92:836–839. doi: 10.1016/s0002-9149(03)00895-6. [DOI] [PubMed] [Google Scholar]
- 7.Sistino J. Epidemiology of cardiovascular disease in the last decade: treatment options and implications for perfusion in the 21st century. Perfusion. 2003;18:73–77. doi: 10.1191/0267659103pf661oa. [DOI] [PubMed] [Google Scholar]
- 8.Mack M, Brown P, Kugelmass A, Battaglia S, Tarkington L, Simon A, Culler S, Becker E. Current status and outcomes of coronary revascularization 1999 to 2002: 148,396 surgical and percutaneous procedures. Ann Thorac Surg. 2004;77:761–766. doi: 10.1016/j.athoracsur.2003.06.019. [DOI] [PubMed] [Google Scholar]
- 9.Lucas F, DeLorenzo M, Siewers A, Wennberg D. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation. 2006;113:374–379. doi: 10.1161/CIRCULATIONAHA.105.560433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weerasinghe D, Yusuf F, Parr N. Trends in percutaneous coronary interventions in New South Wales, Australia. Int J Environ Res Public Health. 2009;6:232–245. doi: 10.3390/ijerph6010245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boden W, O’Rourke R, Teo K, Hartigan P, Maron D, Kostuk W, Knudtson M, Dada M, Casperson P, Harris C, Chaitman B, Shaw L, Gosselin G, Nawaz S, Title L, Gau G, Blaustein A, Booth D, Bates E, Spertus J, Berman D, Mancini G, Weintraub W. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–1516. doi: 10.1056/NEJMoa070829. [DOI] [PubMed] [Google Scholar]
- 12.O’Neill W. A case against low-volume percutaneous coronary intervention centers. Circulation. 2009;120:546–548. doi: 10.1161/CIRCULATIONAHA.109.885269. [DOI] [PubMed] [Google Scholar]
- 13.Mininõ A, Xu J, Kochanek K, Tejada-Vera B. Death in the United States, 2007. NCHS Data Brief. 2009;26:1–8. [PubMed] [Google Scholar]
- 14.Ford E, Ajani U, Croft J, Critchley J, Labarthe D, Kottke T, Giles W, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 15.Ryan J, Linde-Zwirble W, Engelhart L, Cooper L, Cohen D. Temporal changes in coronary revascularization procedures, outcomes, and costs in the bare-metal stent and drug-eluting stent eras: results from the U.S. Medicare program. Circulation. 2009;119:952–961. doi: 10.1161/CIRCULATIONAHA.108.781138. [DOI] [PubMed] [Google Scholar]
- 16.Dube SR, Asman K, Malarcher A, Carabollo R. Cigarette smoking among adults and trends in smoking cessation—United States, 2008. MMWR. 2009;58:1227–1232. [PubMed] [Google Scholar]
- 17.Egan B, Zhao Y, Axon R. U.S. trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 18.Kuklina E, Yoon P, Keenan N. Trends in high levels of low-density lipoprotein cholesterol in the United States, 1999–2006. JAMA. 2009;302:2104–2110. doi: 10.1001/jama.2009.1672. [DOI] [PubMed] [Google Scholar]
- 19.Stagnitti MN. Trends in statins utilization and expenditures for the U.S. civilian noninstitutionalized population, 2000 and 2005 (Statistical brief #205) Medical Expenditure Panel Survey. 2008 May [Google Scholar]
- 20.Atwater B, Oujiri J, Wolff M. The immediate impact of the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial on the management of stable angina. Clin Cardiol. 2009;32:E1–E3. doi: 10.1002/clc.20524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thom T, Haase N, Rosamond W, Howard V, Rumsfeld J, Manolio T, Zheng Z, Flegal K, O’Donnell C, Kittner S, Lloyd-Jones D, Goff DJ, Hong Y, Adams R, Friday G, Furie K, Gorelick P, Kissela B, Marler J, Meigs J, Roger V, Sidney S, Sorlie P, Steinberger J, Wasserthiel-Smoller S, Wilson M, Wolf P. Heart disease and stroke statistics—2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85–e151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 22.Daemen J, Wenaweser P, Tsuchida K, Abrecht L, Vaina S, Morger C, Kukreja N, Jüni P, Sianos G, Hellige G, van Domburg R, Hess O, Boersma E, Meier B, Windecker S, Serruys P. Early and late coronary stent thrombosis of sirolimus-eluting and paclitaxel-eluting stents in routine clinical practice: data from a large two-institutional cohort study. Lancet. 2007;369:667–678. doi: 10.1016/S0140-6736(07)60314-6. [DOI] [PubMed] [Google Scholar]
- 23.Gershlick A, de Belder M, Chambers J, Hackett D, Keal R, Kelion A, Neubauer S, Pennell D, Rothman M, Signy M, Wilde P. Role of non-invasive imaging in the management of coronary artery disease: an assessment of likely change over the next 10 years. A report from the British Cardiovascular Society working group. Heart. 2007;93:423–431. doi: 10.1136/hrt.2006.108779. [DOI] [PMC free article] [PubMed] [Google Scholar]