Abstract
Objectives
We tested whether positive selection on childhood predictors of adult mental and physical health contributed to health advantages of Mexican-born immigrants to the United States relative to U.S.-born Mexican Americans.
Methods
We combined data from surveys conducted during 2000–2003 in Mexico and the U.S. with the same structured interview. We examined retrospective reports of childhood (i.e., <16 years of age) predictors of adult health—education, height, childhood physical illness, childhood mental health, early substance use, and childhood adversities—as predictors of migration from Mexico to the U.S. at ≥16 years of age. We estimated overall selection by comparing migrants to all non-migrants. We also examined selection at the family (members of families of migrants vs. members of families without a migrant) and individual (migrants vs. non-migrants within families of migrants) levels.
Results
Distinguishing between family and individual selection revealed evidence of positive health selection that is obscured in the overall selection model. In particular, respondents in families with migrants were more likely to have ≥12 years of education (odds ratio [OR] = 1.60) and be in the tallest height quartile (OR=1.72) than respondents in families without migrants. At both the family and individual levels, migrants are disadvantaged on mental health profiles, including a higher prevalence of conduct problems, phobic fears, and early substance use.
Conclusions
Positive health selection may contribute to physical health advantages among Mexican immigrants in the U.S. relative to their U.S.-born descendants. Mental health advantages likely reflect a lower prevalence of psychiatric disorders in Mexico, rather than protective factors that distinguish migrants.
Mexican-born immigrants in the United States are in better health than U.S.-born Mexican Americans with respect to a broad range of physical and mental health conditions, including overweight and obesity,1 asthma,2 cardiovascular risk factor profiles,3,4 substance use,5 and psychiatric disorders.6,7 One proposed explanation for these findings is positive health selection8 (i.e., that compared with the non-migrating population of Mexico, migrants are predisposed pre-migration to better health), an advantage that is lost due to environmental influences on the second generation. Understanding the contribution of pre-migration factors to intergenerational differences in health in the Mexican-origin population in the U.S. is limited by the lack of information on pre-migration health of migrants, relative to the non-migrant population of Mexico.
Ecological comparisons based on population averages estimated separately in the U.S. and Mexico provide indirect evidence of better health among migrants with respect to life expectancy,9 height,10 and educational attainment.11 However, because many migrants arrive in the U.S. as children, ecological comparisons reflect differences that might have risen after arrival in the U.S. Rubalcava et al.,12 in the only prospective study of migrant health selection, followed a nationally representative sample of the Mexican population assessed in 2001 and identified individuals who migrated to the U.S. during the following three years. Baseline assessments included height, body mass index (BMI), blood pressure, hemoglobin, and self-rated health. In that study, migrants had been in slightly better-than-average health prior to migration with respect to some indicators of physical health (e.g., blood pressure and height).
Two recent studies have examined selection on mental health by combining data from surveys in Mexico and the U.S. collected retrospectively with the same structured interview. Both studies used information on age at migration to identify mental health problems that began prior to migration. Breslau et al.13 found that anxiety disorders were associated with a higher likelihood of subsequent migration, suggesting negative selection (i.e., worse mental health among migrants prior to migration than non-migrants). However, the migrant sample in that study was small (n=75) and limited to proficient English speakers. Borges et al.,14 using a larger sample of migrants interviewed in both English and Spanish, found no association between suicidality and subsequent likelihood to migrate to the U.S.
This study used a large epidemiologic dataset from surveys in Mexico and the U.S. to examine whether childhood predictors of adult health prior to age 16 were associated with migration to the U.S. at ≥16 years of age. We examined a broader range of mental health conditions than previous studies have done and covered, for the first time, early substance use and childhood family adversities, both of which are predictive of poor physical and mental health in adulthood.15–17 In addition, data from the Mexican survey identify those respondents who had previously been to the U.S. as labor migrants and those with an immediate family member living in the U.S. These data allowed for two additional methodological innovations.
First, we identified and grouped return migrants (i.e., people living in Mexico who have previously lived in the U.S.) with other migrants. Previous studies have misclassified return migrants as non-migrants. Second, in addition to estimating overall selection (i.e., differences between all migrants and all non-migrants), we also distinguished between selection at the family level (i.e., differences between families with and without migrants) and selection at the individual level (i.e., differences within families of migrants between those who migrate and those who remain in Mexico). Previous studies have not distinguished these two levels at which selection might occur, despite sociological evidence suggesting that migration is influenced by familial as well as individual factors.18 Health selection might occur at the family level because migrants tend to come from families with sufficient material and social resources to facilitate migration,18 including ties to cross-national migrant networks.19,20 Families with more resources are also likely to enjoy better health. Selection at the individual level would occur if decisions about migration take into account individual characteristics related to health. For instance, among family members, those less likely to succeed in the local vs. U.S. labor market due to lower educational attainment21 may be more likely to migrate.
Estimation of each of these two levels of selection was possible in this study because the sampling design in the U.S. and the Mexico surveys involved random selection of households and random selection of one respondent within each household. Because of this design, the sample included subsamples of respondents who were representative of the relevant comparison groups. We estimated family-level selection by comparing respondents from families without a migrant with respondents from families with a migrant (migrants in the U.S., return migrants in Mexico, and non-migrants in Mexico with a family member in the U.S.). We estimated individual-level selection within the subsample of respondents from families of migrants by comparing respondents who were themselves migrants (migrants in the U.S. and return migrants in Mexico) with respondents from families of migrants who were not migrants (non-migrants in Mexico with a family member in the U.S.). Countervailing migrant selection processes at the family and individual levels may be obscured when only overall selection is examined.
METHODS
Data sources
Data came from three surveys: one conducted in Mexico and two conducted in the U.S. The Mexico National Comorbidity Survey (M-NCS) was based on a stratified, multistage area probability sample of the Mexican adult household population living in communities of at least 2,500 people between September 2001 and May 2002.22 The response rate was 76.6%, with 5,826 completed interviews. To minimize respondent burden, a long-form interview containing additional risk factor batteries was administered to a subsample of 2,362 respondents, selected with known probabilities on the basis of initial diagnostic assessments.
The National Comorbidity Survey Replication (NCSR)23 and the National Latino and Asian American Survey (NLAAS)24 are based on representative samples of the U.S. adult household population. The NCSR, conducted during 2001–2003 with a response rate of 70.9%, is based on a stratified multistage area probability sample of the English-speaking adult household population of the continental U.S.25 The NLAAS is based on the same sampling frame as the NCSR, with special supplements to increase representation of Hispanic and Asian American populations (including Spanish-language interviews).26 The NLAAS was conducted during 2002–2003 and had a 75.5% response rate for the Latino sample. A total of 1,442 respondents in the NCSR and NLAAS were Mexican American.
Analysis sample and comparison groups
The analysis sample includes respondents to any of the three surveys who lived in Mexico from birth through age 15 (Table 1). This sample includes the Mexican-born respondents to the U.S. surveys who arrived in the U.S. at ≥16 years of age and the entire M-NCS sample. The U.S. respondents (Group 1a) and the return migrants from the M-NCS (Group 1b) together form the migrant sample (Group 1). Return migrants are M-NCS respondents who reported having traveled to the U.S. for employment or education. Return migrants are assumed to have immigrated to the U.S. at ≥16 years of age, a reasonable assumption given that younger migrants are more likely to be joining established families in the U.S. and, therefore, are less likely to return to live in Mexico. The remaining M-NCS respondents were divided into two groups: non-migrant respondents who had a member of their immediate family living in the U.S. (Group 2) and non-migrant respondents with no migrant in their family (Group 3).
Table 1.
Number of respondents of three groups of Mexican-born individuals to short- and long-form surveys: combined Mexico-U.S. sample, 2001–2003a
aData on the Mexican population come from the M-NCS, a nationally representative sample of the Mexican population. Data on the Mexican-born population in the U.S. come from the two nationally representative samples, the NCSR and NLAAS. All data were collected during 2001–2003.
M-NCS = Mexico National Comorbidity Survey
NCSR = National Comorbidity Survey Replication
NLAAS = National Latino and Asian American Survey
NA = not applicable
The three groups shown in Table 1 were used to estimate three migrant selection models. First, we examined overall selection (i.e., differences between all migrants and all non-migrants) by comparing migrants in the U.S. and return migrants in Mexico with all non-migrants in Mexico (Group 1 vs. Groups 2 and 3 combined). The overall selection model corresponds to models estimated in previous migrant selection studies.11,12 Second, we examined family selection (i.e., differences between individuals from families with migrants and those from families without migrants) by comparing migrants and non-migrants with a migrant in their immediate family against non-migrants without a migrant in their immediate family (Groups 1 and 2 combined vs. Group 3). Third, we examined individual selection (i.e., differences within families of migrants between those who migrate and those who do not) by comparing migrants with non-migrant family members of migrants in Mexico (Group 1 vs. Group 2).
Assessments
All three surveys were conducted with the World Mental Health version of the Composite International Diagnostic Interview (WMH-CIDI), a fully structured interview schedule designed for computer-assisted in-home administration by a trained non-clinician interviewer.27 The Spanish version of the instrument was developed following World Health Organization instrument translation procedures involving translation, back-translation, and pilot testing in the target population. Both the M-NCS and the NLAAS used the same Spanish version of the instrument, though some modules of the instrument were excluded in the NLAAS. Interviewer training for all three surveys was conducted by instructors certified by the Institute for Social Research at the University of Michigan. Study procedures were approved by the Institutional Review Boards of Harvard Medical School, the University of Michigan, and the National Institute of Psychiatry Ramon de la Fuentes.
Measures were selected for this study if (1) they were assessed in all three surveys, (2) they referred specifically to childhood conditions or included age-at-onset information, and (3) they were either indicators of childhood health or known childhood predictors of adult health.
Education.
Educational attainment was classified as (1) 0–5 years, (2) 6–8 years, (3) 9–11 years, and (4) ≥12 years of schooling.
Height.
Height was categorized according to quartiles of the gender-specific distribution in the sample. Height reflects cumulative investments in well-being during childhood and is predictive of health status in adulthood.10
Chronic physical illness (long-form only).
Chronic physical illness was defined as self-reported onset prior to age 16 of (1) pain disorder (e.g., arthritis, rheumatism, headache, backache, and other chronic pain); (2) physician diagnosis of allergy or asthma; or (3) other serious chronic condition or life-threatening illness.
Mental health conditions.
These included:
Mood and anxiety disorders: Diagnoses according to Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV)28 criteria of mood disorders (i.e., major depressive episode and dysthymia) and anxiety disorders (i.e., generalized anxiety disorder, panic disorder, social phobia, and posttraumatic stress disorder) with onset prior to age 16. Clinical re-interview studies have found adequate to good agreement with clinical diagnoses in the U.S.29 and in cross-national studies.30
Conduct problems: During childhood or adolescence, people had frequent problems getting into trouble with adults for one of the following: (1) frequent lying, stealing, or breaking rules; (2) fire-setting or other destruction of property; or (3) running away from home or cutting school.
Phobic fears: Respondents were asked a series of six items regarding specific fears that commonly occur in childhood: fear of animals, water, doctors or blood, closed spaces, high places, and airplanes. Respondents who indicated at least one fear were then asked a series of three questions about impairment resulting from the fear. A four-level scale was constructed with the following categories: no impairment (regardless of number of fears), impairment with one to two fears, impairment with three to four fears, and impairment with five to six fears.
Early substance use: Initiation of use of tobacco, alcohol, or illicit drugs prior to age 16.
Phobias and conduct problems in childhood are associated with elevated risk for psychiatric disorders in adulthood.31 Early initiation of substance use is associated with elevated risk for persistent substance use and disorders of abuse and dependence,32–36 as well as physical health problems.
Childhood family adversities (long-form only).
These included:
Family disruption: Did not live with both biological parents up to age 16.
Physical abuse: Was being badly beaten up by an adult caregiver prior to age 16.
Family violence: Witnessed serious physical fights at home prior to age 16.
Childhood family adversities are associated with a range of physical16 and psychiatric15 disorders in adulthood.
Statistical analysis
We conducted all statistical analyses using SUDAAN® to properly account for the complex survey design.37 The sample design specification variables for the combined sample relied on the primary stratum and primary sampling unit identification codes and the sampling weight variables developed by the sample design team at the Institute for Social Research, including the integrated sampling design and weight variable they developed to account for the overlapping coverage of Mexican Americans by the NCSR and NLAAS.26,38,39 Sampling stratification variables were modified to ensure that codes used for the NCSR, NLAAS, and M-NCS components did not overlap.40
Sampling weights reflected adjustments for unequal selection and response probabilities as well as poststratification adjustments to enhance the representativeness of weighted inferences with respect to contemporaneous national census estimates of target population sizes. We applied an additional rescaling factor to the sampling weights in the cross-national dataset so that the weighted sample sizes would reflect the relative sizes of the Mexican-origin target populations in Mexico and the U.S., thereby enhancing the suitability of the weights for use in design-based analyses involving the full population, as well as population subgroups.39,41 We used the Taylor series linearization method for variance estimation and survey-adjusted Wald-type test statistics for hypotheses tests of association in multivariable logistic regression analyses.
We estimated associations between childhood conditions and migration at each level in multivariable logistic regression models with main effects for gender and age. Preliminary model testing found that the interaction between gender and age did not improve model fit after adjusting for model complexity. Results are presented as adjusted odds ratios (AORs) and 95% confidence intervals (CIs). The percentage of observations with missing information on any of the variables used for particular analyses was small (<1.5%); such observations were excluded from particular analyses, resulting in slight variations in sample sizes among the analyses reported in this article.
RESULTS
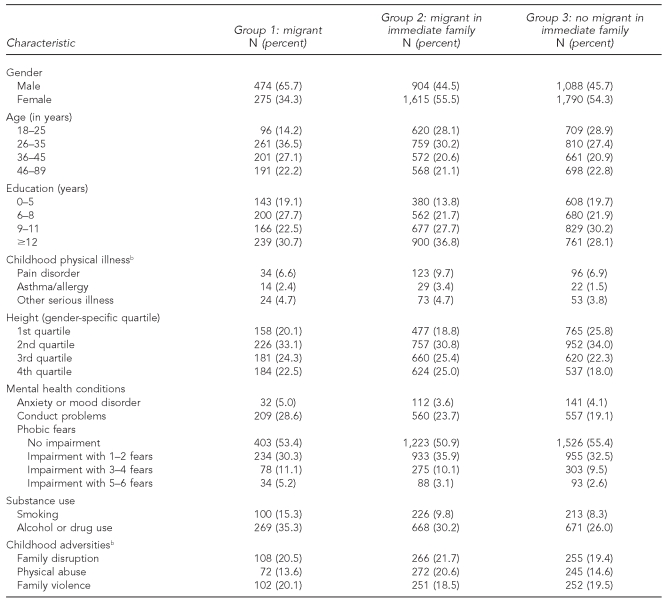
Table 2 shows the demographic characteristics and prevalence of childhood health conditions across the three groups compared in the migrant selection models. Migrants were more likely to be male and were slightly older than both non-migrant groups. Educational attainment was highest among family members of migrants. The prevalence of the three physical conditions ranged from 6.6% to 9.7% for pain disorder, from 1.5% to 3.4% for asthma/allergy, and from 3.8% to 4.7% for other serious illness. The prevalence of DSM-IV anxiety or mood disorder ranged narrowly from 3.6% to 5.0%, while the prevalence of conduct problems ranged from 19.1% to 28.6%. About half (50.9% to 55.4%) of each group reported no fear-related impairment. Smoking and alcohol or drug use were more common among migrants (15.3% and 35.3%, respectively) than among either of the two non-migrant groups. Among childhood adversities, family disruption and family violence were both reported by about one-fifth of respondents in all three groups, while physical abuse was reported more commonly by non-migrant family members of migrants (20.6%) than by respondents in the other two groups (13.6% among migrants and 14.6% among those with no migrant in their family).
Table 2.
Demographic characteristics and prevalence of childhood health conditions among a combined Mexico-U.S. sample, 2001–2003a
aData on the Mexican population come from the Mexico National Comorbidity Survey (M-NCS), a nationally representative sample of the Mexican population. Data on the Mexican-born population in the U.S. come from the two nationally representative samples, the National Comorbidity Survey Replication and the National Latino and Asian American Survey. All data were collected during 2001–2003.
bChildhood physical illness and childhood adversities were assessed in the long-form interview, which was administered to a subsample of the M-NCS respondents (n=2,362).
Results from the overall, family, and individual selection models, with statistical adjustment for age and gender, are shown in Table 3.
Table 3.
Association of childhood health with migration from Mexico to the U.S. at the overall, family, and individual levelsa
aData on the Mexican population come from the Mexico National Comorbidity Survey (M-NCS), a nationally representative sample of the Mexican population. Data on the Mexican-born population in the U.S. come from the two nationally representative samples, the National Comorbidity Survey Replication and the National Latino and Asian American Survey. All data were collected during 2001–2003.
bThe overall selection model compares all migrants with all non-migrants (Group 1 vs. Groups 2 and 3). The family selection model compares members of families with a migrant (including migrants themselves) with members of families with no migrant (Groups 1 and 2 vs. Group 3). The individual selection model compares migrants with non-migrant members of families in which there is a migrant (Group 1 vs. Group 2). All models include statistical controls for age and gender.
cChildhood physical illness and childhood adversities were assessed in the long-form interview, which was administered to a subsample of the M-NCS respondents (n=2,362)
AOR = adjusted odds ratio
CI = confidence interval
Ref. = referent group
Overall selection
In limited respects, there were differences between migrants and non-migrants in childhood predictors of adult health that favored migrants. Compared with non-migrants, migrants were slightly taller (though this figure did not reach statistical significance at p=0.05) and were less likely to have been physically abused. However, with respect to education, anxiety or mood disorder, conduct problems, phobic fears, and early substance use, the findings suggested that migrants were predisposed to worse health than non-migrants.
Family and individual selection
Results of the family and individual selection models revealed important selection effects that were obscured in the overall selection model. First, with respect to education, there was selection at the family and individual levels in opposing directions. The family selection model showed that respondents from families with migrants had significantly higher educational attainment compared with respondents with no migrant in their family, while the individual selection model showed that migrants themselves had significantly lower educational attainment compared with non-migrants from families with migrants.
Second, height was strongly associated with migration in the family selection model, with AORs increasing across quartiles from 1.22 to 1.72 (all statistically significant). However, height was not associated with migration in the individual selection model, with AORs ranging from 0.93 to 1.01, all non-significant.
Third, asthma was associated with migration in the family selection model (AOR=2.13), but not in the individual selection model. The finding of higher odds of asthma at the family level appears to be an isolated finding among chronic physical conditions included in the study; there was no evidence of selection for pain disorder or other serious illness.
Fourth, physical abuse was significantly associated with migration in the family and individual selection models in opposing directions. Respondents from families with migrants were slightly more likely to report physical abuse than respondents from families without migrants (AOR=1.37), but migrants were less likely to report physical abuse than non-migrant family members of migrants (AOR=0.52). There was no evidence of selection on other family adversities.
Conduct problems, phobic fears, and smoking were all significantly associated with migration, with AORs of similar magnitude, at both the family and individual levels. Anxiety or mood disorder was associated with migration at the individual level only, and alcohol or drug use was associated with migration at the family level only.
In summary, there was evidence of positive health selection at the family level with respect to two important predictors of adult health: education and height. There was also evidence of negative selection at the family level with respect to asthma and physical abuse. However, there was not a pattern of negative selection across multiple physical health conditions or childhood family adversities. Selection was consistently negative for mental health conditions at both the family and individual levels. The evidence of health selection at the family level has implications for migrants' health status in adulthood, apart from the migrants' own health predictors, a topic we return to later in this article.
DISCUSSION
Results of the overall selection model in this study were similar to the results of the one previous study that made this comparison in finding only weak evidence that migrants enjoy a physical health advantage due to selection on pre-migration health status.12 Although migrants were slightly more likely to be in the tallest gender-specific height quartile and less likely to have been physically abused than non-migrants, neither of these findings constitutes a clear advantage with implications for health status of Mexican migrants in the U.S. The advantage in height was small and not statistically significant and the difference with respect to history of physical abuse did not extend to other aspects of adverse early family environment, such as family disruption or family violence. Moreover, results directly contradicted the healthy migrant hypothesis with respect to education, childhood behaviors predictive of adult psychiatric disorder—conduct problems and phobic fears—and early initiation of substance use (both tobacco and alcohol or other drugs). Previous studies have also found a weak association11 between lower education and migration, but no previous studies of migrant selection have examined childhood behaviors or early substance use.
When selection at the family and individual levels were examined separately, which this study was the first to do, stronger evidence in support of the healthy migrant hypothesis emerged. First, despite apparent negative selection on education in the overall model, there was positive selection on education at the family level: individuals in families of migrants had significantly more education than individuals in families without migrants. The apparent negative selection on education resulted entirely from selection at the individual level: lower levels of education among migrants relative to non-migrants within the subpopulation of people in families of migrants. The education advantage of families of migrants, compared with Mexican families with no migrants, has important implications for migrants' health selection. If migrants originate in families that have, on average, more education than the general Mexican population, they are likely to have enjoyed a better early life environment than others with the same level of educational attainment. Therefore, their prospects for health in adulthood are more favorable than their own educational attainment alone would suggest.
Second, members of families of migrants were significantly taller, on average, than members of families without a migrant. This evidence also suggests that the potential of a positive influence of early family environment on adult physical health of migrants is larger than previous studies have suggested. Differences in height are particularly informative because they reflect the cumulative impact of nutritional status throughout childhood and have associations with a broad range of adult health conditions.10,42 No difference in height existed between migrants and non-migrant members of families of migrants.
Third, selection on childhood physical abuse also differed between the family and individual models. Families with a migrant were more likely to have had a member who was physically abused, but migrants were less likely to have been abused compared with non-migrants from families of migrants. However, no associations of migration with other childhood adversities approached statistical significance in either the family or individual models. There is evidence from epidemiologic studies suggesting that there are both specific effects of individual adversities and nonspecific effects of family environments on adult health when multiple adversities cluster.43 Migrants do not come from families in which multiple adversities cluster more than non-migrants, and they are less exposed to physical abuse than others in families of migrants. The implication of the observed difference in physical abuse alone in the absence of a cluster of family adversities is unclear.
With respect to mental health and early substance use, evidence directly contradicted the healthy migrant hypothesis at both the family and individual levels, as migrants were more likely to have had conduct problems, higher levels of phobic fear, and early use of tobacco and other drugs. This finding suggests that the observed low prevalence of psychiatric and substance use disorder among Mexican-born immigrants in the U.S., relative to U.S.-born Mexican Americans,6,7 was not a result of factors specific to the migrant population. The most likely explanation for the Mexican “immigrant advantage” with respect to psychiatric disorders is the low prevalence of these disorders among the general Mexican population relative to the general U.S. population, which the U.S.-born Mexican American population comes to resemble.44 The cross-national difference is so large45 that despite the adverse effects of acculturative stressors6 and the negative selection reported in this article for the first time, immigrants have a much lower risk for psychiatric disorders than the U.S.-born Mexican American population.6,7
Limitations
The contribution of this study should be examined in light of four data limitations. First, the analysis dataset involved the combination of multiple national surveys. Although these surveys were part of a multinational project specifically designed to yield survey content and sampling designs well-suited for cross-national comparisons, between-survey differences in measurement and response patterns may add potential sources of confounding bias not present in single-survey studies. The design-based estimation strategy we used allows variance estimates and 95% CIs to reflect some sources of between-survey variation.
Second, the data were retrospective and, thus, the assessments relied on respondent recall and self-report. While recall is imperfect and is likely to result in underreporting of symptoms and life events for all groups, there is no basis for suspecting that the accuracy of recall differs across the groups in a way that would bias the results. It is possible that there are cultural differences between Mexico and the U.S. in knowledge of height. Also, the analysis was limited by the available survey content and did not include comprehensive information on health during childhood. Decisions to include assessments in this study were made to cover the broadest possible range of health using available data specific to child health.
Third, the sample included only one respondent per household. Despite this limitation, we were able to identify the appropriate subsamples to estimate family and individual selection models thanks to the random selection at both the household and individual levels. Future studies that include multiple respondents within households would allow for more detailed specification of hypothesized selection processes.
Fourth, we were unable to distinguish selection at geographic or demographic units above the level of the family. This means that our estimates of family selection combine differences across regions within Mexico with differences between families within regions. For instance, family selection with respect to height might arise from differences in average height in regions where migration is common compared with regions where migration is uncommon.
CONCLUSIONS
This study suggests that health selection among migrants from Mexico to the U.S. is more complex than previous studies have suggested, with distinct and sometimes countervailing contributions at the family and individual levels. Accounting for these distinct contributions reveals stronger evidence of positive selection with respect to important childhood predictors of adult physical health than previous studies have found. These differences may partially account for the positive health profile of the Mexican-origin immigrant population in the U.S. The evidence also suggests negative selection of Mexican migrants to the U.S., relative to the Mexican general population, on predictors of adult mental health. The findings lend support to the suggestion that the low risk for psychiatric disorders among Mexican immigrants compared with U.S.-born Mexican Americans, reported consistently in previous studies,6,7,44 is due to cross-national differences in the prevalence of disorder rather than protective factors that distinguish the migrant population from the general population of Mexico.
REFERENCES
- 1.Crosnoe R, Lopez-Gonzalez L. Immigration from Mexico, school composition, and adolescent functioning. Soc Perspect. 2005;48:1–24. [Google Scholar]
- 2.Eldeirawi KM, Persky VW. Associations of acculturation and country of birth with asthma and wheezing in Mexican American youths. J Asthma. 2006;43:279–86. doi: 10.1080/0277090060022869. [DOI] [PubMed] [Google Scholar]
- 3.Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97:1305–10. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sundquist J, Winkleby MA. Cardiovascular risk factors in Mexican American adults: a transcultural analysis of NHANES III, 1988–1994. Am J Public Health. 1999;89:723–30. doi: 10.2105/ajph.89.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson TP, VanGeest JB, Cho YI. Migration and substance use: evidence from the U.S. National Health Interview Survey. Subst Use Misuse. 2002;37:941–72. doi: 10.1081/ja-120004160. [DOI] [PubMed] [Google Scholar]
- 6.Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:1226–33. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- 7.Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, et al. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008;165:359–69. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41:385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- 9.Jasso G, Massey DS, Rosenzweig MR, Smith JP. Immigrant health: selectivity and acculturation. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical perspectives on racial and ethnic differences in health in late life. Washington: National Academies Press; 2004. pp. p. 227–66. [PubMed] [Google Scholar]
- 10.Crimmins EM, Soldo BJ, Kim JK, Alley DE. Using anthropometric indicators for Mexicans in the United States and Mexico to understand the selection of migrants and the “Hispanic paradox”. Soc Biol. 2005;52:164–77. doi: 10.1080/19485565.2005.9989107. [DOI] [PubMed] [Google Scholar]
- 11.Feliciano C. Educational selectivity in U.S. immigration: how do immigrants compare to those left behind? Demography. 2005;42:131–52. doi: 10.1353/dem.2005.0001. [DOI] [PubMed] [Google Scholar]
- 12.Rubalcava LN, Teruel GM, Thomas D, Goldman N. The healthy migrant effect: new findings from the Mexican Family Life Survey. Am J Public Health. 2008;98:78–84. doi: 10.2105/AJPH.2006.098418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Breslau J, Aguilar-Gaxiola S, Borges G, Castilla-Puentes RC, Kendler KS, Medina-Mora ME, et al. Mental disorders among English-speaking Mexican immigrants to the US compared to a national sample of Mexicans. Psychiatr Res. 2007;151:115–22. doi: 10.1016/j.psychres.2006.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borges G, Breslau J, Su M, Miller M, Medina-Mora ME, Aguilar-Gaxiola S. Immigration and suicidal behavior among Mexicans and Mexican Americans. Am J Public Health. 2009;99:728–33. doi: 10.2105/AJPH.2008.135160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med. 1997;27:1101–19. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- 16.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults—the adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14:245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 17.Case A, Fertig A, Paxson C. The lasting impact of childhood health and circumstance. J Health Econ. 2005;24:365–89. doi: 10.1016/j.jhealeco.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 18.Massey DS, Espinosa KE. What's driving Mexico-U.S. migration? A theoretical, empirical, and policy analysis. Am J Sociol. 1997;102:939–99. [Google Scholar]
- 19.Palloni A, Massey DS, Ceballos M, Espinosa K, Spittel M. Social capital and international migration: a test using information on family networks. Am J Sociol. 2001;106:1262–98. [Google Scholar]
- 20.Orrenius PM. The role of family networks, coyote prices and the rural economy in migration from Western Mexico: 1965–1994. Dallas: Federal Reserve Bank of Dallas; 1999. [Google Scholar]
- 21.Ibarraran P, Lubotsky D. Mexican immigration and self-selection: new evidence from the 2000 Mexican census. In: Borjas GJ, editor. Mexican immigration to the United States. Chicago: University of Chicago Press; 2007. pp. p. 159–92. [Google Scholar]
- 22.Medina-Mora ME, Borges G, Lara C, Benjet C, Blanco J, Fleiz C, et al. Prevalence, service use, and demographic correlates of 12-month DSM-IV psychiatric disorders in Mexico: results from the Mexican National Comorbidity Survey. Psychol Med. 2005;35:1773–83. doi: 10.1017/S0033291705005672. [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13:60–8. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alegria M, Takeuchi D, Canino G, Duan N, Shrout P, Meng XL, et al. Considering context, place and culture: the National Latino and Asian American Study. Int J Methods Psychiatr Res. 2004;13:208–20. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, et al. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) Int J Methods Psychiatr Res. 2004;13:221–40. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: American Psychiatric Association; 2000. [Google Scholar]
- 29.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication [published erratum appears in Arch Gen Psychiatry 2005;62:768] Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 30.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006;15:167–80. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Arch Gen Psychiatry. 2009;66:764–72. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse. 1997;9:103–10. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- 33.Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: age at onset, duration, and severity. Arch Pediatr Adolesc Med. 2006;160:739–46. doi: 10.1001/archpedi.160.7.739. [DOI] [PubMed] [Google Scholar]
- 34.Chen CY, Storr CL, Anthony JC. Early-onset drug use and risk for drug dependence problems. Addict Behav. 2009;34:319–22. doi: 10.1016/j.addbeh.2008.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Breslau N. Daily cigarette consumption in early adulthood: age of smoking initiation and duration of smoking. Drug Alcohol Depend. 1993;33:287–91. doi: 10.1016/0376-8716(93)90114-6. [DOI] [PubMed] [Google Scholar]
- 36.Breslau N, Fenn N, Peterson EL. Early smoking initiation and nicotine dependence in a cohort of young adults. Drug Alcohol Depend. 1993;33:129–37. doi: 10.1016/0376-8716(93)90054-t. [DOI] [PubMed] [Google Scholar]
- 37.Research Triangle Institute. SUDAAN®: Version 10.0. Research Triangle Park (NC): Research Triangle Institute; 2005. [Google Scholar]
- 38.Kessler RC, Haro JM, Heeringa SG, Pennell BE, Ustun TB. The World Health Organization World Mental Health Survey Initiative. Epidemiologia Psichiatr Soc. 2006;15:161–6. doi: 10.1017/s1121189x00004395. [DOI] [PubMed] [Google Scholar]
- 39.Heeringa SG, Berglund P National Institutes of Mental Health (NIMH) Collaborative Psychiatric Epidemiology Survey Program (CPES) data set. Integrated weights and sampling error codes for design-based analysis. Ann Arbor (MI): Inter-University Consortium for Political and Social Research; 2007. [cited 2010 Jul 29]. Also available from: URL: http://www.icpsr.umich.edu/cocoon/cpes/using.xml?section=Weighting. [Google Scholar]
- 40.Korn EL, Graubard BI. Analysis of health surveys. New York: Wiley Interscience; 1999. [Google Scholar]
- 41.Kish L. Cumulating/combining population surveys. Surv Methodol. 1999;25:129–38. [Google Scholar]
- 42.Steckel RH. Heights and human welfare: recent developments and new directions. Explorations in Economic History. 2009;46:1–23. [Google Scholar]
- 43.McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychopathology in the National Comorbidity Survey Replication (NCS-R) II: associations with persistence of DSM-IV disorders. Arch Gen Psychiatry. 2010;67:124–32. doi: 10.1001/archgenpsychiatry.2009.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Breslau J, Borges G, Hagar Y, Tancredi D, Gilman S. Immigration to the USA and risk for mood and anxiety disorders: variation by origin and age at immigration. Psychol Med. 2009;39:1117–27. doi: 10.1017/S0033291708004698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Degenhardt L, Chiu WT, Sampson N, Kessler RC, Anthony JC, Angermeyer M, et al. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the WHO World Mental Health Surveys. Plos Med. 2008;5:e141. doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]