Abstract
Objective
This study assessed the health effects of the 2003 Northeastern blackout, the largest one in history, on mortality and hospital admissions due to respiratory, cardiovascular, and renal diseases in New York City (NYC), and compared the disease patterns and sociodemographic profiles of cases during the blackout with those on control days.
Method
We investigated the effects of the blackout on health using incidence rate ratios to compare the disease on blackout days (August 14 and 15, 2003) with those on normal and comparably hot days (controls). Normal days were defined as summer days (June–August) between the 25th and 75th percentiles of maximum temperature during 1991–2004. Comparably hot days were days with maximum temperatures in the same range as that of the blackout days. We evaluated the interactive effects of demographics and the blackout using a case-only design.
Results
We found that mortality and respiratory hospital admissions in NYC increased significantly (two- to eightfold) during the blackout, but cardiovascular and renal hospitalizations did not. The most striking increases occurred among elderly, female, and chronic bronchitis admissions. We identified stronger effects during the blackout than on comparably hot days. In contrast to the pattern observed for comparably hot days, higher socioeconomic status groups were more likely to be hospitalized during the blackout.
Conclusions
This study suggests that power outages may have important health impacts, even stronger than the effects of heat alone. The findings provide some direction for future emergency planning and public health preparedness.
On August 14, 2003, a series of small disturbances in power generation and transmission triggered protective shutdowns of power plants that cascaded into a massive power outage affecting tens of millions of people throughout the Northeastern United States beginning at 4:11 p.m. on August 14 and lasting approximately 31 hours.1 The magnitude of the threat to human health and safety is illustrated by statistics from a U.S. Department of Transportation report on the effects of the blackout in New York City (NYC): 11,600 traffic signals went dark, 413 subway trains stopped with 400,000 passengers aboard, and 800 elevator rescues were made.2 In addition, high-rise apartment buildings were without water because they rely on electric pumps to move the water to the upper floors, and raw sewage was released into lakes and rivers as the loss of electric power shut down wastewater treatment plants.
Several studies have been published that detail some of the health-related issues posed by the blackout. Most of these studies focus on the increased use of various health-care sectors during the blackout. For example, an increase in calls to 9-1-1 and emergency services,3–5 including a poison control center, was noted.6 Klein et al. documented that while the power outage increased the utilization of hospitals' emergency services, the effective operation of hospitals was compromised by the loss of power.7 Beatty and colleagues described the public health responses in NYC to risks posed by the power outage, such as spoilage of food and contamination and/or lack of water.8
The increases in health service provider activity reported by these studies suggest an increase in health problems associated with the blackout, but only one study reported actual cases of illness. In a case-control investigation of diarrheal illness, Marx and colleagues found that cases were 2.7 times and 1.6 times more likely than controls to have eaten meat and seafood, respectively, during the period between the blackout and the onset of symptoms.9
Just as food spoilage caused by the blackout-induced loss of refrigeration posed a risk for gastrointestinal illness, it is hypothesized that the interruption of air conditioning and mechanized transportation and the resulting heat exposure and exertion may have posed a risk for other health problems. As no studies had been conducted in these areas, this study aimed to (1) assess the health effects of the 2003 blackout on mortality and hospital admissions for respiratory, cardiovascular, and renal diseases in NYC; (2) compare the pattern of health outcomes during the blackout with that during days of comparable temperatures and during normal summer days; and (3) identify the socioeconomic groups most susceptible to the combined effects of heat and power outage.
METHODS
Study population and data sources
The study population included all residents of NYC. Hospital discharge data in NYC from 1991 to 2004 for respiratory, renal, and cardiovascular diseases were obtained from the New York State Department of Health's Statewide Planning and Research Cooperative System (SPARCS).10 SPARCS is a legislatively mandated database that contains hospital discharge data for at least 95% of all acute care hospital admissions in New York State, excluding admissions to psychiatric and federal hospitals. The data included principal diagnoses, hospital admission date, sources of payment, date of birth, gender, race/ethnicity, and street address. Data from the 1990 and 2000 U.S. Census at the census block level were used to derive an indicator of socioeconomic status (SES).
We obtained mortality data from NYC Vital Records for the years 1995–2004. The data included principle diagnoses (International Classification of Diseases, Ninth Revision [ICD-9] code)11 for death causes, date and time of death, residential county, city and street information, ZIP code, gender, race/ethnicity, age, and birth date of decedent.
The Data Support Section of the Computational and Information Systems Laboratory at the National Center for Atmospheric Research provided hourly observations of temperature (T) and dew point (DP) from the National Weather Service (NWS) stations in NYC. Two NWS stations, LaGuardia Airport (LGA) and John F. Kennedy Airport (JFK), had complete data for the period of the study, June 1–August 31, 1991–2004. Because of its more central location compared with JFK, and the fact that more than 85% of NYC residents live within its buffer, the station at LGA was used as the T and DP data source for all of NYC.
Blackout and control definition
We classified August 14 and 15, 2003, as blackout days. We used two referent groups, “normal summer days” and “comparably hot days,” as the control (comparison) groups to assess the effects of the blackout and to compare/separate the effects of the blackout from those of temperature. We defined normal summer days as the summer days from June through August (1991–2004), after excluding the blackout days, and days on which the daily maximum temperature was <25th percentile or >75th percentile of daily maximum temperature in NYC during the summer months. The temperature range of the normal days in this study was between 78.1°F and 87.1°F (June 1–August 31, 1991–2004). Comparably hot days were days in the same period on which the maximum temperatures were in the same range as those of the blackout days (89.1°F to 91.0°F).
Health outcomes
The health outcomes examined were all-cause deaths and hospital admissions due to respiratory, renal, and cardiovascular diseases. For hospitalizations, a case was defined as a resident of NYC who was admitted to a hospital in the summer (i.e., June, July, and August) from 1991 to 2004 with a principal diagnosis of respiratory, renal, or cardiovascular disease. We used ICD-9 codes to classify cases.
Respiratory disease diagnoses included chronic bronchitis (491), emphysema (492), asthma (493), and chronic airway obstruction not elsewhere classified (496). For children aged 0–4 years, we included acute bronchitis and bronchiolitis (466) and bronchitis, not specified as acute or chronic (490), because these are common respiratory illnesses among very young children and their symptoms are difficult to distinguish from asthma in young children. Renal diagnoses included nephritis, nephrotic syndrome and nephrosis (580–589), other diseases of the urinary system (590–599), and symptoms involving the urinary system (788). Cardiovascular diagnoses included chronic rheumatic heart disease (393–396), hypertension (401–405), ischemic heart diseases (410–414), cardiac dysrhythmias (427), congestive heart failure (428), and cerebrovascular diseases (430–434, 436–438). Deaths from all causes were included in the mortality analyses.
Data processing and geocoding
To define the study population more precisely, the residential address from each hospital admission record due to respiratory diseases was geocoded and assigned a latitude and longitude using MapMarker Plus® 12.12 About 84% of the residential addresses were geocoded automatically, 15% were geocoded interactively, 94% were geocoded to street level, 5% were geocoded to ZIP code level, and fewer than 1% (about 6,110 records) could not be geocoded. Admission records for cardiovascular diseases, renal diseases, and mortality records were also geocoded to at least ZIP code level. The map of geocoded addresses was overlaid onto the map of exposure regions using MapInfo Professional® 8.5.13 We then calculated daily hospital admission counts for each outcome of interest between 1991 and 2004.
Statistical analysis
We used time-series plots to make time-based, within-community comparisons of mortality and morbidity during blackout and non-blackout periods. To control for the potential effect of high temperatures on hospital admissions, non-blackout days were partitioned into normal summer days and days that were as hot as the blackout (comparably hot days). We computed the mean daily rates of each outcome, and compared rates during blackout days, normal summer days, and comparably hot days using incidence rate ratios (IRRs). We calculated Wald 95% confidence intervals (CIs) assuming a Poisson distribution of daily admission counts.
To assess whether some people were more vulnerable than others to being hospitalized during the blackout, we examined several demographic characteristics: race/ethnicity, SES, gender, and age as potential modifiers of the effect of the exposure. We used a “case only” design, which, according to Armstrong and Schwartz,14,15 assesses the interaction between demographic variables and the exposure. Use of this method requires independence of the modifiers and the exposure, a condition met by these data. We calculated odds ratios (ORs) for each stratum to examine whether the proportion of a given demographic subgroup that was hospitalized during the blackout differed from the proportion hospitalized during normal summer days. For comparison, we conducted the same analyses to assess demographic modification of the effect of comparably hot days.
RESULTS
The blackout lasted for two days with maximum temperatures of 91.0°F and 89.1°F. There were 110 days with maximum temperatures comparable to those of the blackout days. A total of 703 days in June through August, 1991–2004, fell between the 25th and 75th percentiles of maximum temperature and were classified as normal summer days. We excluded 289 days having a maximum temperature <25th percentile (78.1°F) and 296 days having a maximum temperature >75th percentile (87.1°F).
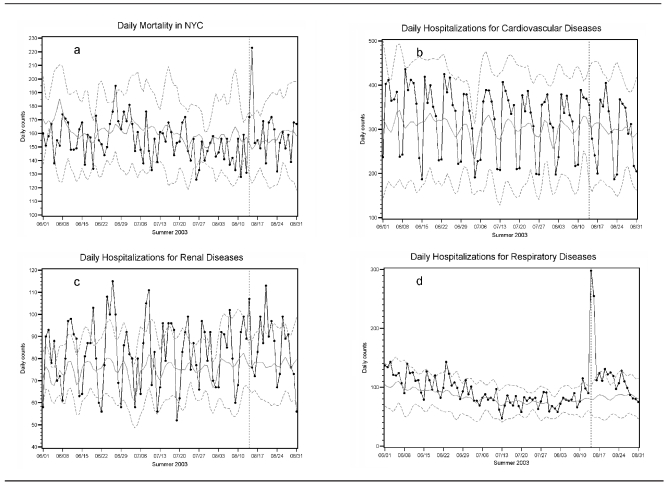
We conducted a preliminary examination of the effects of the blackout on hospital admissions and mortality by plotting the daily counts of these outcomes from June through August of 2003. Part “a” of the Figure shows daily mortality counts across summer 2003. A significant increase in deaths was seen on August 15, the day after the blackout. Figure part “b” shows no changes in the patterns of daily counts of cardiovascular admissions during the blackout period. For renal diseases (Figure part “c”), although the admissions count on August 14 was relatively high, it was not higher than days with very high temperatures (e.g., June 24–27, July 6, and August 20). In contrast, a large spike in hospital admissions for respiratory diseases occurred on the day of the blackout and continued on the day after the blackout (Figure part “d”). The increase in mortality will be explored in future work. Only the results for respiratory admissions are presented in this article.
Figure.
Daily mortality and morbidity counts in New York City during summer 2003
Note: The vertical reference lines point to the date of August 14, 2003; dots and black lines represent observed daily morbidity and mortality counts; gray curves are daily normals and their 95% confidence intervals. Daily normals are the mean daily mortality or morbidity counts for the same date in the years 1991–2004, with temperatures between 78.1°F and 87.1°F (the 25th and 75th percentile of the distribution of maximum temperature in New York City from June through August), excluding blackout days.
NYC = New York City
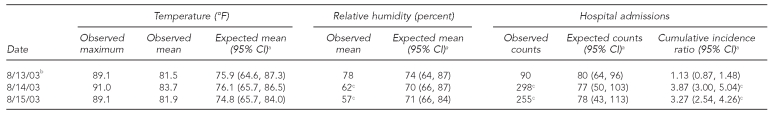
Table 1 presents data comparing the observed maximum temperatures and the observed and expected mean temperatures for the day before, the day of, and the day after the blackout, as well as the observed and expected values for humidity and respiratory admissions. Each expected value is the mean of the values on the same dates for all other years (1991–2002 and 2004). The observed mean temperatures for the three days did not differ from the expected temperatures. The relative humidity on the day before the blackout did not differ from expected, while on the day of the blackout (Day 0) and the day after the blackout (Day 1) it was lower than expected. The maximum temperatures for the three days were 89.1°F, 91.0°F, and 89.1°F, respectively. On the day before the blackout, there were 90 respiratory admissions in NYC, which did not differ significantly from the expected value of 80. However, on Day 0 and Day 1, hospital admissions for respiratory diagnoses were 298 and 255, respectively, each of which was more than three times higher than expected (IRR=3.87, 95% CI 3.00, 5.04; and IRR=3.27, 95% CI 2.54, 4.26, respectively).
Table 1.
Temperature, humidity, and hospitalizations for respiratory diseases during the Northeastern blackout: August 13–15, 2003, New York City
aBased on the daily admission counts, mean temperatures, and relative humidity on the same dates in 1991–2002 and 2004.
bAugust 13, 2003, is the day prior to the blackout, which began on August 14, 2003, at 4 p.m. and continued for 31 hours.
cSignificant at p<0.05
CI = confidence interval
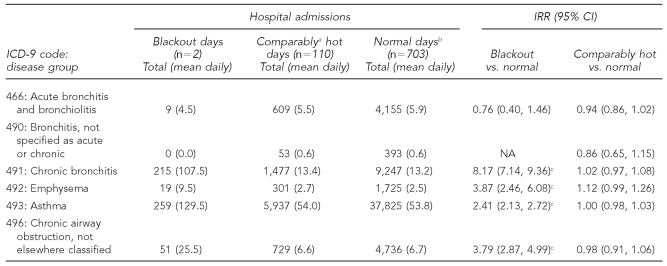
For all respiratory diagnoses combined, the rates of admissions were 276.5 per day during the blackout, 82.8 per day during comparably hot days, and 82.6 per day during normal days (data not shown). Within each diagnostic subgroup, the rates of admissions during each of the exposure types (blackout and comparably hot) were compared with the rates of admissions on normal days and reported as IRRs (Table 2). Of the diagnostic subgroups, chronic bronchitis admissions were most strongly affected by the blackout, showing a 717% increase compared with normal days (IRR=8.17, 95% CI 7.14, 9.36). Likewise, admissions for emphysema, chronic airway obstruction, and asthma were increased during the blackout, with IRRs of 3.87, 3.79, and 2.41, respectively. Comparably hot days did not have a similar effect on admissions; only one IRR approached statistical significance: emphysema admissions compared with normal days (IRR=1.12, 95% CI 0.99, 1.26).
Table 2.
Total hospitalizations and IRRs for respiratory admissions by disease subgroups during the Northeastern blackout: August 13–15, 2003, New York City
aComparably hot days are days with maximum temperatures between 89.1°F and 91.0°F (the maximum temperatures on August 14 and 15, 2003).
bNormal days are days with maximum temperatures between 78.1°F and 87.1°F (the 25th and 75th percentile of the distribution of maximum temperature in New York City) from June 1 through August 31, 1991–2004, excluding blackout days.
cSignificant at p<0.05
IRR = incidence rate ratio
CI = confidence interval
ICD-9 = International Classification of Diseases, Ninth Revision
NA = not applicable
During the blackout days, 52.1% of chronic bronchitis cases were ≥75 years of age compared with 39% during the comparably hot days. For chronic airway obstruction, the proportion of cases ≥75 years of age was 51% during the blackout and 40.7% during comparably hot days. Examination of the blackout effects in nearby areas of New York (e.g., Long Island, White Plains, and the Lower Hudson Valley) revealed significantly increased respiratory admissions (percentage increases of 1.61, 1.99, and 0.67, respectively) (data not shown).
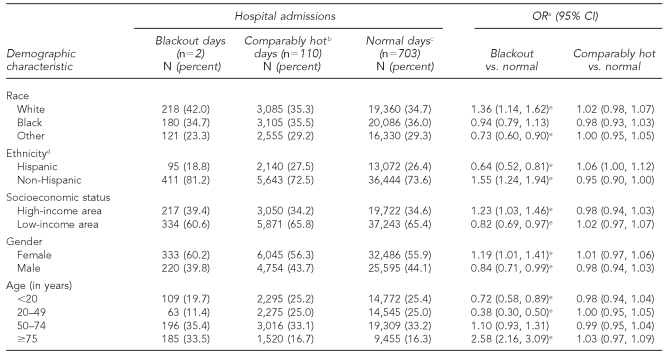
To assess whether some people were more vulnerable to being hospitalized for respiratory conditions during the blackout, we examined several SES variables, including race/ethnicity, socioeconomic factors, income, gender, and age, as potential modifiers of the effect of the exposure (Table 3). We calculated ORs for each stratum as a measure of how likely a demographic subgroup was to be hospitalized during the blackout compared with others not in that subgroup. For comparison, we conducted the same analyses to assess demographic modification of the effects of normal days and comparably hot days. Excess vulnerability to the effects of the blackout was found among the elderly (OR=2.58, 95% CI 2.16, 3.09), non-Hispanic people (OR=1.55, 95% CI 1.24, 1.94), white people (OR=1.36, 95% CI 1.14, 1.62), and those residing in higher socioeconomic areas (OR=1.23, 95% CI 1.03, 1.46). People of a race other than black or white (OR=0.73), Hispanic people (OR=0.64), and those <50 years of age (OR=0.38 for those aged 20–49 years and OR=0.72 for those aged <20 years) had reduced odds of being admitted to the hospital during the two blackout days. Gender, being black, or being aged 50–74 years had no differential effect on blackout-related hospitalizations.
Table 3.
Total hospitalizations and ORs for respiratory admissions by demographic characteristics during the Northeastern blackout: August 13–15, 2003, New York City
aORs are based on comparing the selected stratum with all other strata.
bComparably hot days are days with maximum temperatures between 89.1°F and 91.0°F (the maximum temperatures on August 14 and 15, 2003).
cNormal days are days with maximum temperatures between 78.1°F and 87.1°F (the 25th and 75th percentile of the distribution of maximum temperature in New York City) from June 1 through August 31, 1991–2004, excluding blackout days.
dMissing values are approximately 8% for blackout days, 15% for comparably hot days, and 15% for normal days.
eSignificant at p<0.05
OR = odds ratio
CI = confidence interval
Table 3 shows that most of the ORs for the interactions between demographic characteristics and exposure to comparably hot days were very close to 1.0, indicating that hospitalizations on these days were unaffected by demographics.
DISCUSSION
We found that respiratory hospital admissions and total mortality in NYC increased significantly during the 2003 Northeastern blackout relative to normal summer days, while hospitalization due to cardiovascular or renal diseases did not. The only previous study assessing a health effect was a case-control study examining diarrheal illness in NYC after the 2003 blackout.9 In that study, there was a significant increase in diarrhea cases identified through the NYC Syndromic Surveillance System; diarrhea cases occurring after the blackout were associated with eating meat (OR=2.7, 95% CI 1.2, 6.1) and seafood (OR=4.8, 95% CI 1.6, 14) that presumably had spoiled due to the power outage. No other studies of specific health endpoints after a massive power outage were available for comparison.
A question that might be asked is, what environmental factors changed due to the blackout and potentially contributed to the health effects we found? The blackout exposed people to a number of conditions that could have contributed to the surge in respiratory admissions, including heat, poor air quality, exertion, and psychological stress.
The heat effect during the blackout may have been an important contributor to the increase in admissions we observed. The ambient maximum temperature in NYC was 91.0°F on the day of the blackout and 89.1°F on the day after the blackout. In addition to the very high outdoor temperature, the loss of air conditioning and mechanical ventilation caused indoor temperatures to rise, leaving people with no respite from the outdoor heat. Previous studies have reported positive associations between very high temperatures and increased risk of mortality,16,17 respiratory diseases,18,19 and heat-related diseases.20
Poor air quality is a well-known risk factor for respiratory diseases21 and mortality.22 The 2003 blackout affected air quality on both the regional and local levels. The regional effect was due to the cascading electrical grid problems that caused power generation plants to shut down across the northeastern U.S. Evidence of large reductions in sulfur dioxide (SO2) (>90%), ozone (50%), and light scattering by particles (70%) was recorded by aircraft over central Pennsylvania on August 15, 2003, 24 hours after the blackout began. Similarly, nitrogen oxide and SO2 emissions from upwind power plants were down to 34% and 20%, respectively, of that normally found.23 Projections suggest that areas such as NYC may have experienced a reduction in pollution drift as a result of the power plant shutdowns.
On the local level, people's exposures to vehicular emissions were potentially higher than usual. With the loss of trains and subways, more people crowded the streets, walking or attempting to use buses or taxicabs. But vehicular traffic was snarled due to the absence of traffic signals, and it is likely that exhaust emissions were higher than usual on the streets as vehicles waited, with engines running, for the traffic jams to clear.
The increased need for physical exertion during the blackout would also be an important concern for the elderly, people with underlying diseases, and other vulnerable populations. With transit within NYC brought to a standstill, people were exerting themselves by walking longer distances under harsher conditions than they would have on a typical day. The U.S. Department of Transportation reported that 400,000 people were evacuated from stopped subway trains during the blackout.2 Many of these trains were stopped far from platforms and passengers had to walk on the train tracks in the dark tunnels that were now without ventilation. Similarly, people who ordinarily rode elevators now walked stairs in buildings without air conditioning or ventilation.
The effects of these three factors—heat, poor air quality, and exertion—were likely aggravated by a fourth factor: the psychological stress of not knowing what had happened, not knowing what else might happen, not knowing how to get home, and worrying about loved ones. The terrorist attacks on the World Trade Center had occurred less than two years previously, and many people feared that the blackout they were experiencing was the result of terrorism. In addition, home health aids for people with respiratory diseases (e.g., nebulizers and oxygen enrichers) would not be working during a blackout. Greenwald found that patients who were dependent on home electrical medical devices, mainly oxygen conservers, sought care in emergency departments and hospitals when the power failed.24 Due to the power outage, major municipal water pumping stations and fuel stations failed for 24 hours in NYC. The consequences of this series of problems after the blackout caused physical and emotional stress on local residents, especially those with existing chronic diseases.
This study demonstrates much stronger effects on respiratory diseases during the blackout than during heat wave days. These stronger effects were shown in almost all respiratory disease categories except for acute bronchitis, bronchiolitis, and non-specified bronchitis. The most striking increase during the blackout was in admissions due to chronic bronchitis, which were eight times the rate on normal days. Hospitalizations for emphysema, asthma, and chronic airway obstruction increased by 1.5- to threefold compared with normal days. The very large increase in risk for chronic bronchitis admissions could be due to the fact that there was a larger proportion of the elderly with this disease who were more susceptible to heat. Although there was also a large proportion of the elderly with chronic airway obstruction, the effect of the blackout on this disease is not as strong as the effect on chronic bronchitis for unknown reasons or unstable estimate due to small sample sizes. The stronger health effect during the blackout compared with comparably hot days may be due to the combined effects from heat and the additional risk factors, such as poor air quality, high exertion, psychological stress, and loss of access to electric medical devices, as mentioned previously.
In contrast to previous studies regarding heat effects,15,25 our study did not find increased susceptibility among the elderly during comparably hot days compared with normal summer days, which may be due to the temperature during the blackout being lower than that of a heat wave. However, our study found increased susceptibility among the elderly (those ≥75 years of age) during the blackout. Older people have a reduced biological capacity to acclimate to thermal extremes because of their higher sweating threshold.26 Thus, the loss of air conditioning and fans may have contributed to this increased effect. Furthermore, aging is often accompanied by chronic illness and social isolation.27 Finally, impaired cognitive function in older adults may affect their decision-making and make them less likely to avoid heat exposure or seek necessary medical assistance.28
Our study found that a greater proportion of women were hospitalized during the blackout compared with normal summer days, but gender had no effect during comparably hot days, which is consistent with other research.29 Because there are no other blackout studies for comparison, it is unclear why females would be more vulnerable.
One of the most interesting findings of the current study was that the demographic patterns of respiratory admissions during the 2003 blackout were quite different from those during comparably hot days. High sociodemographic (SES) groups such as white people, non-Hispanic people, and those living in higher income areas had a significantly increased risk of admission for respiratory diseases during the blackout. On the other hand, our previous studies in NYC found that lower SES populations were more susceptible to the heat's health effects during extremely hot days.18 Higher SES groups are more likely to use nebulizers or other electric home aids and air conditioners than lower SES groups in summer. Thus, they depend on electric equipment to manage disease and are adapted to living in cooler conditions, making them more susceptible to heat during a power outage.
We found that large increases in respiratory hospital admissions and mortality occurred in NYC during the 2003 blackout. This study may be the first epidemiologic study investigating the direct health effects of electrical power outages. To improve the design of an ecological study, we used individual-level demographic data and several strategies in controlling for time-varying confounders and selecting appropriate reference periods for comparison. For instance, the use of the summer days in the past 14 years and excluding the days with temperatures at the higher and lowest quartiles as the reference minimized the confounding effects of season, long-term trends, annual temperature/air pollution fluctuation, and extreme temperature outliers. Our use of population-based admission and mortality data with multiple outcomes (mortality and several morbidity diagnoses) and two reference time periods (normal summer days and comparably hot days to separate the effects of blackout from high temperature only) demonstrates the unique characteristics of this event and its potential health impact.
Limitations
Our study was limited to some extent, however, by the lack of individual-level or activity pattern information regarding the circumstances of hospitalization. For instance, we did not know where people were or what they were doing when they began having symptoms or whether they were accustomed to the use of air conditioning prior to the blackout. Such information would have allowed us to draw conclusions about the factors related to the blackout that were most responsible for triggering hospital admissions. Similarly, while we did not have information on people's preexisting conditions, it is tempting to speculate that people with preexisting respiratory disorders would be more susceptible to exacerbations during the conditions associated with a power outage.
As the current study design is an ecological study, which cannot illustrate the antecedent consequence effect, it is possible that the increase in respiratory admissions the day following the blackout was due to simple accumulation. However, we found that hospital admissions due to respiratory diseases and mortality significantly increased on both days of the blackout (August 14 and 15, 2003). These increases were the highest peaks of the entire summer without following secondary peaks. Additionally, unlike clinic visits, hospital admissions are very severe, and those cases may not be able to wait another one or two days. Therefore, it is less likely that the increased admissions we observed in this study were due to accumulation.
CONCLUSIONS
The results of this study suggest that power outages can pose a public health threat requiring preparedness planning. While an individual blackout cannot be anticipated, it is thought by experts in the power generation field that blackouts are an ever-present risk given that much of the nation's transmission grid is quite aged and there have been multiple smaller blackouts in summer and in winter snowstorms.1 Traffic authorities and public health officials need to be aware of the increased risk of respiratory disease and mortality, as well as the unique demographic composition of the potential cases. Hospitals need to anticipate surges in admissions. Future studies should focus on identifying the individual characteristics and circumstances linked to the increased risk of hospital admissions to plan emergency responses to a blackout.
Footnotes
The Data Support Section of the Computational and Information Systems Laboratory at the National Center for Atmospheric Research (NCAR) provided meteorologic data used in this study.
This work was supported in part by grants from the National Environmental Public Health Tracking Program, Centers for Disease Control and Prevention (CDC), #5U38EH000184. NCAR was supported by grants from the National Science Foundation (NSF).
No study sponsors were involved in the process of study design; the collection, analysis, and interpretation of data; the writing of the article; or the decision to submit the article. CDC, NCAR, and NSF have not officially endorsed this article and the views expressed herein may not reflect the views of CDC, NCAR, or NSF.
REFERENCES
- 1.U.S.-Canada Power System Outage Task Force. Final report on the August 14, 2003, blackout in the United States and Canada: causes and recommendations. Natural Resources Canada, Department of Energy (US) 2004 Apr [Google Scholar]
- 2.DeBlasio AJ, Regan TJ, Zirker M, Ficher K, Lovejoy K, Morin D. Effects of catastrophic events on transportation system management and operations: August 2003 Northeast blackout New York City. Cambridge (MA): Department of Transportation (US); 2004. May, No.: DOT-VNTSC-FHWA-04-04. [Google Scholar]
- 3.Freese J, Richmond NJ, Silverman RA, Braun J, Kaufman BJ, Clair J. Impact of a citywide blackout on an urban emergency medical services system. Prehosp Disaster Med. 2006;21:372–8. doi: 10.1017/s1049023x00004064. [DOI] [PubMed] [Google Scholar]
- 4.Kile JC, Skowronski S, Miller MD, Reissman SG, Balaban V, Klomp RW, et al. Impact of 2003 power outages on public health and emergency response. Prehosp Disaster Med. 2005;20:93–7. doi: 10.1017/s1049023x00002259. [DOI] [PubMed] [Google Scholar]
- 5.Prezant DJ, Clair J, Belyaev S, Alleyne D, Banauch GI, Davitt M, et al. Effects of the August 2003 blackout on the New York City healthcare delivery system: a lesson for disaster preparedness. Crit Care Med. 2005;33(1 Suppl):S96–101. doi: 10.1097/01.ccm.0000150956.90030.23. [DOI] [PubMed] [Google Scholar]
- 6.Klein KR, Herzog P, Smolinske S, White SR. Demand for poison control center services “surged” during the 2003 blackout. Clin Toxicol (Phila) 2007;45:248–54. doi: 10.1080/15563650601031676. [DOI] [PubMed] [Google Scholar]
- 7.Klein KR, Rosenthal MS, Klausner HA. Blackout 2003: preparedness and lessons learned from the perspectives of four hospitals. Prehosp Disaster Med. 2005;20:343–9. doi: 10.1017/s1049023x00002818. [DOI] [PubMed] [Google Scholar]
- 8.Beatty ME, Phelps S, Rohner MC, Weisfuse MI. Blackout of 2003: public health effects and emergency response. Public Health Rep. 2006;121:36–44. doi: 10.1177/003335490612100109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marx MA, Rodriguez CV, Greenko J, Das D, Heffernan R, Karpati AM, et al. Diarrheal illness detected through syndromic surveillance after a massive power outage: New York City, August 2003. Am J Public Health. 2006;96:547–53. doi: 10.2105/AJPH.2004.061358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.New York State Department of Health. The SPARCS Data System 2002 annual report. Albany (NY): NYSDOH; 2004. [Google Scholar]
- 11.Department of Health and Human Services (US). International classification of diseases, ninth revision, clinical modification. 6th ed. Washington: HHS; 1997. [Google Scholar]
- 12.Pitney Bowes Business Insight. MapMarker Plus®: Version 12. Troy (NY): Pitney Bowes Business Insight; 2007. [Google Scholar]
- 13.Pitney Bowes Business Insight. MapInfo Professional®: Version 8.5. Troy (NY): Pitney Bowes Business Insight; 2005. [Google Scholar]
- 14.Armstrong BG. Fixed factors that modify the effects of time-varying factors: applying the case-only approach. Epidemiology. 2003;14:467–72. doi: 10.1097/01.ede.0000071408.39011.99. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz J. Who is sensitive to extremes of temperature? A case-only analysis. Epidemiology. 2005;16:67–72. doi: 10.1097/01.ede.0000147114.25957.71. [DOI] [PubMed] [Google Scholar]
- 16.Naughton MP, Henderson A, Mirabelli MC, Kaiser R, Wilhelm JL, Kieszak SM, et al. Heat-related mortality during a 1999 heat wave in Chicago. Am J Prev Med. 2002;22:221–7. doi: 10.1016/s0749-3797(02)00421-x. [DOI] [PubMed] [Google Scholar]
- 17.Rey G, Jougla E, Fouillet A, Pavillon G, Bessemoulin P, Frayssinet P, et al. The impact of major heat waves on all-cause and cause-specific mortality in France from 1971 to 2003. Int Arch Occup Environ Health. 2007;80:615–26. doi: 10.1007/s00420-007-0173-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin S, Luo M, Walker RJ, Liu X, Hwang SA, Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20:738–46. doi: 10.1097/EDE.0b013e3181ad5522. [DOI] [PubMed] [Google Scholar]
- 19.Ye F, Piver WT, Ando M, Portier CJ. Effects of temperature and air pollutants on cardiovascular and respiratory diseases for males and females older than 65 years of age in Tokyo, July and August 1980–1995. Environ Health Perspect. 2001;109:355–9. doi: 10.1289/ehp.01109355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barrow MW, Clark KA. Heat-related illnesses. Am Fam Physician. 1998;58(749-56):759. [PubMed] [Google Scholar]
- 21.Lin S, Bell EM, Liu W, Walker RJ, Kim NK, Hwang SA. Ambient ozone concentration and hospital admissions due to childhood respiratory diseases in New York State, 1991–2001. Environ Res. 2008;108:42–7. doi: 10.1016/j.envres.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 22.Schwartz J. Air pollution and daily mortality: a review and meta-analysis. Environ Res. 1994;64:36–52. doi: 10.1006/enrs.1994.1005. [DOI] [PubMed] [Google Scholar]
- 23.Marufu LT, Taubman BF, Bloomer B, Piety CA, Doddridge BG, Stehr JW, et al. The 2003 North American electrical blackout: an accidental experiment in atmospheric chemistry. Geophys Res Lett. 2004;31(L13106) [Google Scholar]
- 24.Greenwald PW, Rutherford AF, Green RA, Giglio J. Emergency department visits for home medical device failure during the 2003 North America blackout. Acad Emerg Med. 2004;11:786–9. doi: 10.1197/j.aem.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 25.Vandentorren S, Bretin P, Zeghnoun A, Mandereau-Bruno L, Croisier A, Cochet C, et al. August 2003 heat wave in France: risk factors for death of elderly people living at home. Eur J Public Health. 2006;16:583–91. doi: 10.1093/eurpub/ckl063. [DOI] [PubMed] [Google Scholar]
- 26.Donoghue ER, Graham MA, Jentzen JM, Lifschultz BD, Luke JL, Mirchandani HG. Criteria for the diagnosis of heat-related deaths: National Association of Medical Examiners. Position paper. National Association of Medical Examiners Ad Hoc Committee on the Definition of Heat-Related Fatalities. Am J Forensic Med Pathol. 1997;18:11–4. doi: 10.1097/00000433-199703000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Ebi KL, Mills DM, Smith JB, Grambsch A. Climate change and human health impacts in the United States: an update on the results of the U.S. national assessment. Environ Health Perspect. 2006;114:1318–24. doi: 10.1289/ehp.8880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koken PJ, Piver WT, Ye F, Elixhauser A, Olsen LM, Portier CJ. Temperature, air pollution, and hospitalization for cardiovascular diseases among elderly people in Denver. Environ Health Perspect. 2003;111:1312–7. doi: 10.1289/ehp.5957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Neill MS, Zanobetti A, Schwartz J. Modifiers of the temperature and mortality association in seven US cities. Am J Epidemiol. 2003;157:1074–82. doi: 10.1093/aje/kwg096. [DOI] [PubMed] [Google Scholar]