The global burden of noncommunicable diseases is emerging as a major public health challenge in the world.1 Cardiovascular diseases (CVDs) account for half of noncommunicable disease deaths worldwide.2 Hypertension is a well-known risk factor for the development of CVD, heart attack, and stroke.3 The World Health Organization (WHO) estimates that one-half of CVDs are caused by elevated blood pressure (BP).4 Hypertension prevalence has been increasing, and an estimated 972 million people in the world suffer from this problem.5
Pre-hypertension is a new category of BP classification recommended by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) in 2003,6 in which people with a systolic BP of 120–139 millimeters of mercury (mmHg) and/or a diastolic BP of 80–89 mmHg are categorized as having pre-hypertension. The individuals with pre-hypertension are known to be at increased risk of developing hypertension.7,8 In addition, pre-hypertension is associated with increased risk of CVD, independent of other CVD risk factors.9,10
In China, the prevalence of hypertension has risen in the last decade. The International Collaborative Study of Cardiovascular Diseases in Asia indicates that the overall prevalence of hypertension in the Chinese adult population aged 35–74 years in 2001 was 27.2%,11 or 2.4 times higher than it was in 1991 (11%).12 However, there are few data on the epidemiology of pre-hypertension in China. Only a few studies estimate the prevalence of pre-hypertension in rural China, which ranges from 38.4% to 47.0%, and pre-hypertension has been found to be more common than hypertension.13–15
As in most traditional epidemiologic studies, investigations on the risk factors of pre-hypertension and hypertension have focused mainly on individual-level socioeconomic status (SES) variables such as income, education, and unemployment. Abundant evidence indicates that the individual SES is strongly associated with hypertension and other CVD risk factors.16–18 Hypertension has shown an inverse relationship with income, unemployment rate, and education level.19–22 Recently, researchers have become increasingly interested in examining the contextual SES effects on CVD risk factors.23,24 Several studies suggested that neighborhood SES characteristics are inversely associated with BP reactivity, and that individual and neighborhood SES may be independent predictors of BP.25–27
However, little is known about the association between both individual and contextual SES and pre-hypertension. A Chinese study indicated that individual education level was a protective factor for pre-hypertension.13 To date, however, there is still relatively little relevant research in China on the topic, and the association of contextual SES and both pre-hypertension and hypertension is still poorly understood. As such, there is a need to examine the association between SES and BP on multiple levels.
Yunnan Province in southwestern China is a relatively undeveloped province. It is a production and consumption hub for tobacco products, with the tobacco industry supporting a large portion of the local economy. Yunnan Province also has the country's largest concentration of ethnic minorities, with 25 of China's 56 state-recognized ethnicities living in the province. Ethnic minorities account for 38.1% of the region's total population of 41,440,000. The drinking and smoking habits seen in these cultures further increase the dangers of CVD in this ethnically diverse province.28
With this background in mind, the aim of this study was to estimate the prevalence rate of pre-hypertension and hypertension, and to apply multilevel regression analyses to simultaneously investigate the association between both individual and contextual SES (e.g., percent primary education [grades one to six] or higher, proportion of ethnic minorities, type of county, and mean yearly income) and pre-hypertension and hypertension among the rural adult population of southwest China from 2008 to 2009. The results may serve as a basis for further CVD research in this community.
METHODS
Study design, subjects, and sampling techniques
This study was a community-based, cross-sectional survey conducted in rural areas of Yunnan Province. We used multistage stratified random sampling methods to select the study sample. In the first stage, all of Yunnan Provinces' counties were divided into economically advantaged, middle economically advantaged, and economically disadvantaged populations, based on per capita gross domestic product. From each of these three groups we randomly selected one county, for a total of three counties.
In the second stage, to guarantee the representativeness of each sample, the groups selected for the study covered all of the township districts in the three chosen counties, for a total of 21 townships. In the third stage, each township was divided into three blocks based on the size of the population and adjacent geographical situation. In each of the 63 blocks, one village was chosen from the list of villages based on the probability proportional to size. In the final stage of sampling, we obtained a list of individuals aged ≥35 years from the village committee in each selected village, and we used simple random sampling to select eligible individuals from each village.
Data collection and measurement
Fifteen fifth-year medical students and three master's degree students from Kunming Medical University were selected as interviewers for data collection. Before the survey, they received training covering an introduction to hypertension, the use of the screening questionnaire, methods and skills of survey administration, and quality control. A workshop was conducted to teach interviewers anthropometric measurements.
Each participant who gave informed consent was personally interviewed by one of the interviewers using a pretested and structured questionnaire. Interviewers obtained information on demographic characteristics, behavioral practices, diagnosis, treatment, awareness and control of hypertension, and self-reported family history of CVDs, as well as the results from anthropometric measurements and BP.
Three BP measurements were made according to American Heart Association recommendations.29 After at least five minutes of rest in a sitting position, systolic and diastolic BPs were taken from the participant's right arm using standardized mercury sphygmomanometers. BP measures were based on the mean of three BP readings.
Body height and weight were measured using standard procedures to ensure the highest accuracy; weight was measured using a beam balance. Measurements of height and weight were conducted with the participants standing on the scale wearing indoor clothes and no shoes, with height measured to the nearest 0.2 centimeter, and weight to the nearest 0.2 kilogram (kg). Body mass index (BMI) was calculated as weight in kg divided by height in meters squared (kg/m2), which has been promulgated by WHO as the most useful epidemiologic measure of obesity.30
Definitions
We defined pre-hypertension as people with a systolic BP of 120–139 mmHg and/or a diastolic BP of 80–89 mmHg, which was recommended by JNC 7.6 We defined hypertension as a mean systolic BP ≥140 mmHg, a diastolic BP of ≥90 mmHg, and/or use of antihypertensive medications.
A current smoker was defined as a person who had smoked at least 100 cigarettes in his/her lifetime and smoked tobacco products during the survey period. A current drinker was defined as a person who drank alcohol regularly on 12 or more days during the past 12 months.
Outcome and independent variables
The outcome variables included a binary measure of pre-hypertension and hypertension. Independent variables included both individual and township characteristics. Individual characteristics included age, gender, ethnicity, yearly household income, education, smoking, drinking, family history of hypertension, and BMI. The township characteristics or contextual variables were percent primary (grades one to six) education or higher, percentage of ethnic minorities, type of county, and mean yearly income.
Statistical analysis
Mean yearly income of the township, percent of ethnic minorities, and percent primary education or higher were computed from each community for use as contextual variables. These contextual variables were then divided into two categories (high and low), with the median value as the cutoff.
We used descriptive analysis techniques and multilevel regression models in this study. We calculated the sampling weights based on data from the year 2000 China Population Census and our sampling scheme. However, we estimated the prevalence of pre-hypertension and hypertension based on weighted proportions. We calculated the age- and gender-standardized estimates of prevalence by a direct method using the year 2000 China adult population aged ≥35 years as the standard population.
We used multilevel logistic regression to analyze the association between contextual variables and dichotomous measures of pre-hypertension and hypertension. Individual characteristics were set at the first level and contextual characteristics at the second level. The association between contextual variables and pre-hypertension and hypertension were expressed in terms of odds ratios (ORs), and we computed their 95% confidence intervals (CIs). All decisions regarding statistical significance were based on two-tailed p-values. We conducted data analyses using R software.31
We fitted two models. First, we included the individual variables in the model (model 1) to investigate the extent to which township-level differences were explained by the individual composition of the townships. Second, we included the township variables (model 2) in addition to the variables already included in model 1 to investigate whether this contextual phenomenon was conditioned by specific township characteristics.
RESULTS
From the 21 townships, 11,700 individuals were invited to participate in the survey from the lists of eligible individuals, all of whom were at least 35 years of age. Of these, 11,061 (94.5%) individuals consented to participate. BP and anthropometric measurements were conducted on all of them.
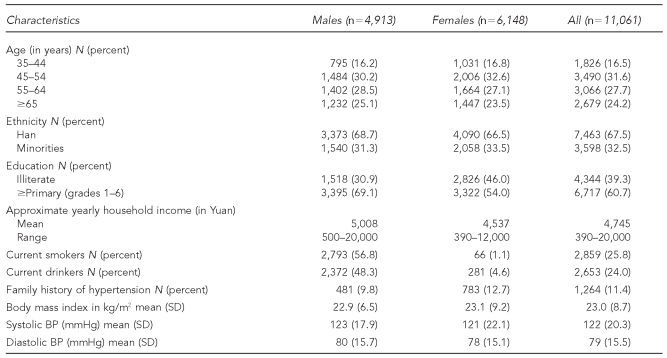
As shown in Table 1, participants in the study included 4,913 men and 6,148 women. The percentage of ethnic minorities was 32.5%, and the adult illiteracy rate was 39.3%. Female participants had a higher illiteracy rate than male participants (p<0.01). The mean annual household income was 4,745 Yuan (equal to $703 U.S. dollars), varying from 390 Yuan ($58) to 20,000 Yuan ($2,963). The overall prevalence of current smokers, current drinkers, and family history of hypertension in the study population was 25.8%, 24.0%, and 11.4%, respectively. Men had a remarkably higher prevalence of being current smokers and current drinkers than women, whereas women had a higher mean BMI and systolic BP than men (p<0.01).
Table 1.
Characteristics of subjects in a community-based, cross-sectional survey of rural adults in Yunnan Province, China: 2008–2009
Kg/m2 = kilograms/meter squared
SD = standard deviation
BP = blood pressure
mmHg = millimeters of mercury
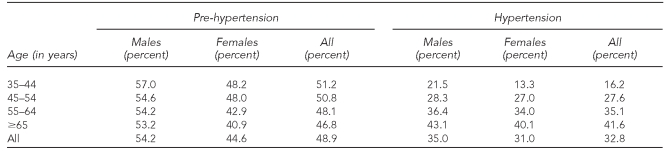
Table 2 presents weighted age- and gender-standardized prevalence of pre-hypertension and hypertension among study participants. Pre-hypertension and hypertension were more common in males than in females (p<0.01). With increasing age, the prevalence of pre-hypertension decreased, whereas the prevalence of hypertension increased for both men and women.
Table 2.
Weighted age- and gender-standardized prevalence of pre-hypertension and hypertension among participants in a community-based, cross-sectional survey of rural adults in Yunnan Province, China: 2008–2009
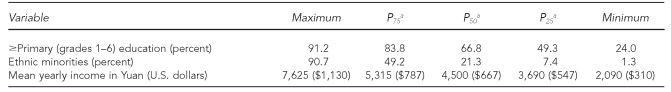
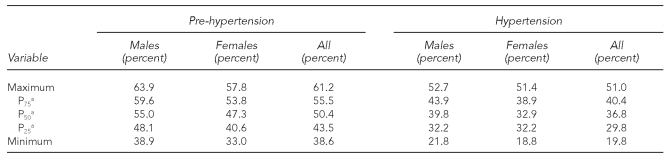
Table 3 summarizes the SES of townships. Overall, variations in percent primary education or higher, percentage of the minority, and mean income were high among the 21 townships. Table 4 shows the distribution of weighted age- and gender-adjusted prevalence of pre-hypertension and hypertension among the 21 townships. Men had a higher prevalence of pre-hypertension and hypertension than women.
Table 3.
Distribution of socioeconomic status for 21 townships in a community-based, cross-sectional survey of rural adults in Yunnan Province, China: 2008–2009
aP25 is the first quartile, P50 is the median quartile, and P75 is the third quartile.
Table 4.
Distribution of weighted age- and gender-adjusted prevalence of pre-hypertension and hypertension among 21 townships in a community-based, cross-sectional survey of rural adults in Yunnan Province, China: 2008–2009
aP25 is the first quartile, P50 is the median quartile, and P75 is the third quartile.
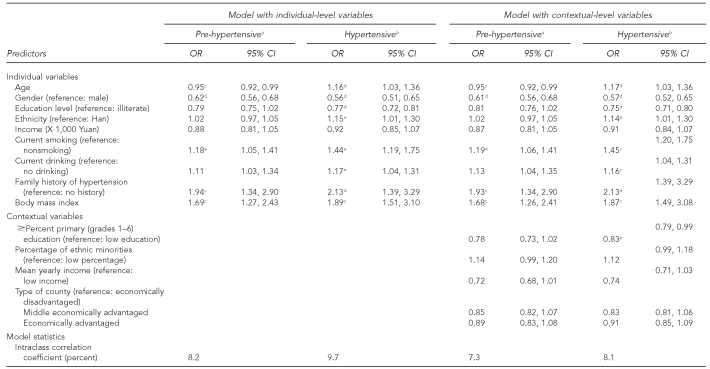
Table 5 shows the results of multilevel analyses. For individual demographic variables, females had a lower probability of being pre-hypertensive and hypertensive than males. The probability of being pre-hypertensive decreased with age but increased with BMI. In contrast, the probability of being hypertensive increased with age and BMI. Adults who were current smokers and those who had a family history of hypertension were more likely to be pre-hypertensive and hypertensive. Furthermore, individuals with a higher education level had a decreased probability of hypertension. Ethnic minority adults who were current drinkers were more likely to be hypertensive.
Table 5.
Multilevel logistic regression analysis of pre-hypertension and hypertension in a community-based, cross-sectional survey of rural adults in Yunnan Province, China: 2008–2009
aThe reference group is non-pre-hypertensive.
bThe reference group is non-hypertensive.
cp<0.01
dp<0.001
ep<0.05
OR = odds ratio
CI = confidence interval
Inclusion of township-level variables in model 2 did not affect the associations (ORs) estimated in model 1. Model 2 informed that townships with higher education levels had a decreased probability of hypertension. Both individual and contextual education levels showed no association with pre-hypertension. The intraclass correlation coefficients (ICCs) from the multilevel model were used to quantify the amount of variation in prevalence of pre-hypertension and hypertension resulting from differences among townships. The ICCs were reduced when information on township characteristics was introduced in the model. The ICCs in model 2 indicated that substantial proportions of the variation in prevalence of pre-hypertension (7.3%) and prevalence of hypertension (8.1%) were occurring at the contextual level.
DISCUSSION
The findings of this study indicate that the prevalence of pre-hypertension and hypertension was higher in males compared with females in all age categories, and pre-hypertension was more common than hypertension in rural southwest China. Both contextual and individual variables were associated with hypertension, whereas only individual demographic characteristics were shown to influence pre-hypertension.
This study demonstrates the high prevalence of pre-hypertension in rural adults of southwest China. In this study, the overall prevalence of pre-hypertension was greater than the prevalence of hypertension, and was higher than the prevalence rate observed in northeast China (47%);13 Taiwanese adults (31%);32 Asian people including Japanese,33 Indian,35 and Korean35 adults; and adults from other western countries.36,37
Pre-hypertension has been very prevalent in the Chinese rural adult population. Individuals with pre-hypertension have been known to progress to hypertension, and pre-hypertension is associated with an increased prevalence of CVD risk factors.14 The findings of this study suggest that pre-hypertensive adults need more positive strategies including lifestyle modifications, more frequent BP monitoring, and treatment for the early prevention of hypertension and CVD.
In the study population, the higher prevalences of pre-hypertension and hypertension in males was possibly due to the increased prevalence of metabolic risk factors for hypertension and pre-hypertension. This finding is in agreement with other studies in China,13,14 as well as studies from other developed and developing countries.33,34,36 In addition, the prevalence of pre-hypertension decreased with increasing age in both males and females, whereas the prevalence of hypertension increased with age for both genders. The opposite trend of these two categories of BP classification is likely a result of the progression of pre-hypertensive people to clinical hypertension.
In our study, BMI, current smoker, and family history of hypertension were positively associated with the probability of being pre-hypertensive and hypertensive. The finding that these factors are important contributors to both pre-hypertension and hypertension has been demonstrated in many previous studies,32,34,37,38 which indicates that smoking, overweight, and obesity increase the risk of elevated BP and overall mortality. In addition, being a current drinker was also an important contributor to hypertension but not pre-hypertension in this study. This finding differs from a previous Chinese study13 in which drinking was a risk factor for pre-hypertension. The reason for this dichotomy is not clear.
Ethnic minorities had an increased risk for hypertension in this study. Some previous Chinese studies15,40 also indicated that mean BP and prevalence of hypertension were significantly different among various ethnic groups. As ethnic populations living in the same area have differing BP levels, it seems that genetic factors, various diet-related factors, and lifestyles may be more important determinants for BP level.12,41 The results suggest that ethnicity is an important consideration in the management of BP, but further research is required to find out if this is true.
This study found that education level plays an important role in influencing hypertension. Both individuals' and townships' education levels were inversely associated with the probability of being hypertensive. This finding is consistent with other studies.22,25,26 The WHO MONICA project study42 showed that systolic BP was positively associated with low educational achievement. A Swedish study indicated that low educational achievement at the area level was independently associated with increased diastolic BP.43 The inverse association of township education level with hypertension suggests that the educated rural communities rather than the uneducated ones are still being targeted for future intervention programs.
Neither individual nor township education level influenced pre-hypertension in this study. Whereas a Chinese study conducted in Liaoning Province13 indicated that individual education level was a protective factor against pre-hypertension, the reason for the inconsistent effect of education on Chinese pre-hypertensive adults is unknown.
While several studies have demonstrated that individual income had a negative association with systolic and diastolic BP, and deprivation in low-income communities increases the probability of being hypertensive,16,20,26 our study yielded no evidence supporting any association between individual or contextual income and pre-hypertension or hypertension in rural Chinese adults. Income seemed to be the less important measure in relation to pre-hypertension and hypertension compared with other socioeconomic indicators in our study population.
Strengths and limitations
One strength of this study was the high response rate (more than 94%) in the community survey and the obtainment of measurements from health examinations to ensure the accuracy of data. One limitation of the study was that none of the lipid profiles were available due to financial restraints.
CONCLUSION
Pre-hypertension is more common than hypertension in rural southwest China. The identified risk factors provide important information for improving BP control among this population. The results of this study suggest that the study region should emphasize further control of pre-hypertension, and future contextual interventions on hypertension in parallel with those at the individual level are needed.
Acknowledgments
The authors thank Tom Fitzpatrick, a visiting student at Kunming Medical University School of Public Health, for reviewing the manuscript.
Footnotes
The study was supported by grants from the National Natural Science Funds of China (grant # 30960335) and Yunnan Provincial Natural Science Funds (grant # 2008CD115).
REFERENCES
- 1.Murray CJL, Lopez AD. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 projected to 2020. Cambridge (MA): Harvard School of Public Health; 1996. [Google Scholar]
- 2.World Health Organization. The world health report 2003—shaping the future. Geneva: WHO; 2003. [Google Scholar]
- 3.He J, Whelton PK. Elevated systolic blood pressure and risk of cardiovascular and renal disease: overview of evidence from observational epidemiologic studies and randomized controlled trials. Am Heart J. 1999;138(3 Pt 2):S211–9. doi: 10.1016/s0002-8703(99)70312-1. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. The world health report 2002—reducing risks, promoting healthy life. Geneva: WHO; 2002. [DOI] [PubMed] [Google Scholar]
- 5.Hajjar I, Kotchen JM, Kotchen TA. Hypertension: trends in prevalence, incidence, and control. Annu Rev Public Health. 2006;27:465–90. doi: 10.1146/annurev.publhealth.27.021405.102132. [DOI] [PubMed] [Google Scholar]
- 6.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 7.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–6. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 8.Greenlund KJ, Croft JB, Mensah GA. Prevalence of heart disease and stroke risk factors in persons with prehypertension in the United States, 1999–2000. Arch Intern Med. 2004;164:2113–8. doi: 10.1001/archinte.164.19.2113. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y, Lee ET, Devereux RB, Yeh J, Best LG, Fabsitz RR, et al. Prehypertension, diabetes, and cardiovascular disease risk in a population-based sample: the Strong Heart Study. Hypertension. 2006;47:410–4. doi: 10.1161/01.HYP.0000205119.19804.08. [DOI] [PubMed] [Google Scholar]
- 10.Liszka HA, Mainous AG, 3rd, King DE, Everett CJ, Egan BM. Pre-hypertension and cardiovascular morbidity. Ann Fam Med. 2005;3:294–9. doi: 10.1370/afm.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gu D, Reynolds K, Wu X, Chen J, Duan X, Muntner P, et al. InterASIA Collaborative Group. The International Collaborative Study of Cardiovascular Diseases in ASIA. Prevalence, awareness, treatment, and control of hypertension in China. Hypertension. 2002;40:920–7. doi: 10.1161/01.hyp.0000040263.94619.d5. [DOI] [PubMed] [Google Scholar]
- 12.People's Republic of China–United States Cardiovascular and Cardiopulmonary Epidemiology Research Group. An epidemiological study of cardiovascular and cardiopulmonary disease risk factors in four populations in the People's Republic of China: baseline report from the P.R.C.–U.S.A. Collaborative Study. Circulation. 1992;85:1083–96. doi: 10.1161/01.cir.85.3.1083. [DOI] [PubMed] [Google Scholar]
- 13.Sun Z, Zheng L, Wei Y, Li J, Zhang X, Liu X, et al. Prevalence and risk factors of the rural adult people prehypertension status in Liaoning Province of China. Circ J. 2007;71:550–3. doi: 10.1253/circj.71.550. [DOI] [PubMed] [Google Scholar]
- 14.Zhang M, Batu B, Tong W, Li H, Lin Z, Zhang X, et al. Prehypertension and cardiovascular risk factor clustering among Mongolian population in rural and animal husbandry area, Inner Mongolia, China. Circ J. 2009;73:1437–41. doi: 10.1253/circj.cj-09-0101. [DOI] [PubMed] [Google Scholar]
- 15.Sun Z, Zheng L, Xu C, Li J, Zhang X, Liu S, et al. Prevalence of prehypertension, hypertension, and associated risk factors in Mongolian and Han Chinese populations in Northeast China. Int J Cardiol. 2008;128:250–4. doi: 10.1016/j.ijcard.2007.08.127. [DOI] [PubMed] [Google Scholar]
- 16.Ezeamama AE, Viali S, Tuitele J, McGarvey ST. The influence of socioeconomic factors on cardiovascular disease risk factors in the context of economic development in the Samoan archipelago. Soc Sci Med. 2006;63:2533–45. doi: 10.1016/j.socscimed.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 17.Sharma S, Malarcher AM, Giles WH, Myers G. Racial, ethnic and socioeconomic disparities in the clustering of cardiovascular disease risk factors. Ethn Dis. 2004;14:43–8. [PubMed] [Google Scholar]
- 18.Roohafza HR, Sadeghi M, Kelishadi R. Cardiovascular risk factors in Iranian adults according to educational levels: Isfahan healthy heart program. Asia Pac J Public Health. 2005;17:9–14. doi: 10.1177/101053950501700103. [DOI] [PubMed] [Google Scholar]
- 19.Henriksson KM, Lindblad U, Agren B, Nilsson-Ehle P, Rastam L. Associations between unemployment and cardiovascular risk factors varies with the unemployment rate: the Cardiovascular Risk Factor Study in Southern Sweden (CRISS) Scand J Public Health. 2003;31:305–11. doi: 10.1080/14034940210164948. [DOI] [PubMed] [Google Scholar]
- 20.Walcott-McQuigg JA. Psychological factors influencing cardiovascular risk reduction behavior in low and middle income African-American women. J Natl Black Nurses Assoc. 2000;11:27–35. [PubMed] [Google Scholar]
- 21.Pereira MA, Kriska AM, Collins VR, Dowse GK, Tuomilehto J, Alberti KG, et al. Occupation status and cardiovascular disease in the rapidly developing, high-risk population of Mauritius. Am J Epidemiol. 1998;148:148–59. doi: 10.1093/oxfordjournals.aje.a009618. [DOI] [PubMed] [Google Scholar]
- 22.Yu Z, Nissinen A, Vartiainen E, Song G, Guo Z, Zheng G, et al. Associations between socioeconomic status and cardiovascular risk factors in an urban population in China. Bull World Health Organ. 2000;78:1296–305. [PMC free article] [PubMed] [Google Scholar]
- 23.Cubbin C, Sundquist K, Ahlen H, Johansson SE, Winkleby MA, Sundquist J. Neighborhood deprivation and cardiovascular disease risk factors: protective and harmful effects. Scand J Public Health. 2006;34:228–37. doi: 10.1080/14034940500327935. [DOI] [PubMed] [Google Scholar]
- 24.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21:171–92. doi: 10.1146/annurev.publhealth.21.1.171. [DOI] [PubMed] [Google Scholar]
- 25.Kapuku GL, Treiber FA, Davis HC. Relationships among socioeconomic status, stress induced changes in cortisol, and blood pressure in African American males. Ann Behav Med. 2002;24:320–5. doi: 10.1207/S15324796ABM2404_08. [DOI] [PubMed] [Google Scholar]
- 26.McGrath JJ, Matthews KA, Brady SS. Individual versus neighborhood socioeconomic status and race as predictors of adolescent ambulatory blood pressure and heart rate. Soc Sci Med. 2006;63:1442–53. doi: 10.1016/j.socscimed.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 27.Agyemang C, van Hooijdonk C, Wendel-Vos W, Ujcic-Voortman JK, Lindeman E, Stronks K, et al. Ethnic differences in the effect of environmental stressors on blood pressure and hypertension in the Netherlands. BMC Public Health. 2007;7:118. doi: 10.1186/1471-2458-7-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Le C, Chongsuvivatwong V, Geater A, Apakupakul N, et al. Contextual and individual demographic determinants of alcohol consumption and smoking: a comparative study in southwestern China and southern Thailand. Southeast Asian J Trop Med Public Health. 2009;40:370–9. [PubMed] [Google Scholar]
- 29.Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, et al. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88(5 Pt 1):2460–70. doi: 10.1161/01.cir.88.5.2460. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization. Obesity: preventing and managing the global epidemic: report of a WHO Consultation on Obesity. Geneva: WHO; 2000. [PubMed] [Google Scholar]
- 31.R Foundation for Statistical Computing. R: Version 2.9.1. Vienna (Austria): R Foundation for Statistical Computing; 2006. [Google Scholar]
- 32.Tsai PS, Ke TL, Huang CJ, Tsai JC, Chen PL, Wang SY, et al. Prevalence and determinants of prehypertension status in the Taiwanese general population. J Hypertens. 2005;23:1355–60. doi: 10.1097/01.hjh.0000173517.68234.c3. [DOI] [PubMed] [Google Scholar]
- 33.Ishikawa Y, Ishikawa J, Ishikawa S, Kayaba K, Nakamura Y, Shimada K, et al. Jichi Medical School Cohort Investigators Group. Prevalence and determinants of prehypertension in a Japanese general population: the Jichi Medical School Cohort Study. Hypertens Res. 2008;31:1323–30. doi: 10.1291/hypres.31.1323. [DOI] [PubMed] [Google Scholar]
- 34.Yadav S, Boddula R, Genitta G, Bhatia V, Bansal B, Kongara S, et al. Prevalence & risk factors of pre-hypertension & hypertension in an affluent north Indian population. Indian J Med Res. 2008;128:712–20. [PubMed] [Google Scholar]
- 35.Choi KM, Park HS, Han JH, Lee JS, Lee J, Ryu OH, et al. Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. J Hypertens. 2006;24:1515–21. doi: 10.1097/01.hjh.0000239286.02389.0f. [DOI] [PubMed] [Google Scholar]
- 36.Syamala S, Li J, Shankar A. Association between serum uric acid and prehypertension among US adults. J Hypertens. 2007;25:1583–9. doi: 10.1097/HJH.0b013e32813aeb6c. [DOI] [PubMed] [Google Scholar]
- 37.Greenlund KJ, Croft JB, Mensah GA. Prevalence of heart disease and stroke risk factors in persons with prehypertension in the United States, 1999–2000. Arch Intern Med. 2004;164:2113–8. doi: 10.1001/archinte.164.19.2113. [DOI] [PubMed] [Google Scholar]
- 38.Pitsavos C, Chrysohoou C, Panagiotakos DB, Lentzas Y, Stefanadis C. Abdominal obesity and inflammation predicts hypertension among prehypertensive men and women: the ATTICA Study. Heart Vessels. 2008;23:96–103. doi: 10.1007/s00380-007-1018-5. [DOI] [PubMed] [Google Scholar]
- 39.Goldstein IB, Shapiro D, Guthrie D. Ambulatory blood pressure and family history of hypertension in healthy men and women. Am J Hypertens. 2006;19:486–91. doi: 10.1016/j.amjhyper.2005.09.025. [DOI] [PubMed] [Google Scholar]
- 40.Liu L, Liu L, Ding Y, Huang Z, He B, Sun S, et al. Ethnic and environmental differences in various markers and dietary intake and blood pressure among Chinese Han and three other minority peoples of China: results from the WHO Cardiovascular Diseases and Alimentary Comparison (CARDIAC) study. Hypertens Res. 2001;24:315–22. doi: 10.1291/hypres.24.315. [DOI] [PubMed] [Google Scholar]
- 41.Zhao GS, Yuan XY, Gong BQ, Wang SZ, Cheng ZH. Nutrition, metabolism, and hypertension. A comparative survey between dietary variables and blood pressure among three nationalities in China. J Clin Hypertens. 1986;2:124–31. [PubMed] [Google Scholar]
- 42.Merlo J, Asplund K, Lynch J, Rastam L, Dobson A World Health Organization MONICA Project. Population effects on individual systolic blood pressure: a multilevel analysis of the World Health Organization MONICA Project. Am J Epidemiol. 2004;159:1168–79. doi: 10.1093/aje/kwh160. [DOI] [PubMed] [Google Scholar]
- 43.Merlo J, Ostergren PO, Hagberg O, Lindstrom M, Lindgren A, Melander A, et al. Diastolic blood pressure and area of residence: multilevel versus ecological analysis of social inequity. J Epidemiol Community Health. 2001;55:791–8. doi: 10.1136/jech.55.11.791. [DOI] [PMC free article] [PubMed] [Google Scholar]