Abstract
Objectives
Occupation has been linked to cardiovascular disease (CVD) incidence and mortality, but few studies have investigated occupation in relation to early atherosclerotic disease. This study examined associations between various occupational characteristics and carotid artery intima-media thickness (IMT) in a multi-ethnic sample.
Methods
The Multi-Ethnic Study of Atherosclerosis (MESA) recruited 6814 adults aged 45e84 years and free of clinical CVD (response rate 60%, 51% female). Questionnaire data were used to determine occupational group (managerial/professional, sales/office, service, blue-collar), psychosocial job characteristics (ie, job demands, job control) and other sociodemographic information.
Results
Common carotid artery (CCA)-IMT was greater for blue-collar jobs than for management/professional jobs (mean difference=0.012 mm, p=0.049) after adjustment for age, sex, race, place of birth (US or foreign born) and CVD risk factors. Compared to management/professional jobs, internal carotid artery (ICA)-IMT was greater for sales/office, service and blue-collar jobs (mean difference=0.071 mm, p<0.001; 0.057 mm, p=0.009; and 0.110 mm, p<0.001, respectively) after adjustment for age, sex, race and place of birth. The difference between blue-collar jobs and management/professional jobs remained significant after additional adjustment for CVD risk factors, income and education (mean difference=0.048 mm, p=0.045). Higher levels of control at work were associated with thinner CCA-IMT (mean difference=‒0.009 mm, p=0.016, adjusted for age, sex, race and place of birth) but not with ICA-IMT. Job demands had no significant association with IMT.
Conclusions
Blue-collar jobs and low levels of job control were associated with the development of subclinical atherosclerosis.
INTRODUCTION
Various studies have linked occupational exposures to cardiovascular disease (CVD) incidence and mortality.1 In one estimation, CVD accounts for nearly a third of all mortality attributed to occupation.2 After a few decades of research on occupational characteristics and CVD events,1 several large-scale studies have started to investigate the relationship between job characteristics and intima-media thickness (IMT),3–10 a non-invasive measure of early atherosclerosis. IMT is associated with CVD risk factors11 12 and also predicts clinical CVD events.13 14 Identifying associations between occupation and subclinical disease will facilitate early interventions for CVD.
Most previous studies on occupation and IMT focussed on job characteristics such as job strain (a combination of high job demands and low job control)15 and stress caused by various job demands (eg, complexity of work, physical demands, irregular work schedules). The Atherosclerosis Risk in Communities Study and the Kuopio Ischaemic Heart Disease Risk Factor Study both reported significant associations between job stress and increased IMT, but these associations were attenuated to non-significance after traditional CVD risk factors were included in the analysis.6 7 The Cardiovascular Risk in Young Finns Study, on the other hand, reported that among men, job strain was associated with increased IMT even after adjustments were made for other CVD risk factors.3–5 While these results suggest that certain job characteristics are associated with IMT, at least two issues remain relatively unexplored.
First, these studies did not address occupational category in relation to IMT; therefore, it is not known if an occupational gradient exists regarding IMT. Occupational category is often used as an individual-level indicator of socioeconomic status (SES). Several studies have reported significant associations of IMT with educational attainment or income,10 16 17 but few have examined associations of IMT with occupational category. One exception is the Malmö Diet and Cancer Study, which found that IMT was significantly greater for unskilled manual workers than for high-level non-manual workers.8 10 The Malmö study results suggest an occupational gradient associated with IMT; however, it is not clear if this persists beyond the effects of income and education because these SES indicators were not included in the analyses.
A second point that needs clarification is IMT's segment-specific associations with occupation. The research on IMTas an indicator of early atherosclerosis has identified that the IMTs of different segments have different associations with CVD risk factors.18–20 More specifically, the IMT of the common carotid artery (CCA-IMT) is more strongly associated with blood pressure,19 20 while the IMT of the internal carotid artery (ICA-IMT) is more strongly associated with cholesterol.20 CCA- and ICA-IMT are also reported to have different associations with clinical outcomes.21 Because most previous studies on occupation and IMT either used only CCA-IMT3–6 8 or took the average of IMTs from different carotid artery segments,7 it is not well understood whether occupation has segment-specific associations with IMT. The Malmö study, which did report segment-specific IMT outcomes, found no significant associations of CCA-IMT with occupational status or job strain9 10; however,the IMT of the carotid bifurcation area was associated with job strain9 and occupational category.10 Different associations of occupational status and/or job characteristics with the IMT of different carotid artery segments would provide detailed information about the role of occupation in early atherosclerosis development; however, such research is still scarce.
The current study examined IMT in relation to both occupational category and job strain. Based on prior work,3–5 10 we hypothesised that (1) IMT would be greater for people in lower status jobs than for those in higher status jobs, (2) IMTwould be positively associated with job demands and negatively associated with job control, and (3) people in high strain jobs (a combination of high demands and low control) would have greater IMT than those in low strain jobs. We investigated these hypotheses with CCA- and ICA-IMT separately in order to explore segment-specific associations.
METHODS
Study participants
We used data from the Multi-Ethnic Study of Atherosclerosis (MESA), a multi-centre cohort study of 6814 adults designed to investigate the prevalence and progression of subclinical CVD.22 Participants were recruited from six US communities (Forsyth County, North Carolina; Northern Manhattan and the Bronx, New York; Baltimore City and Baltimore County, Maryland; St. Paul, Minnesota; Chicago, Illinois; and Los Angeles, California). At the time of enrolment between 2000 and 2002, the participants were 45e84 years of age and free of clinical CVD. The participation rate was 60% among those eligible, and women accounted for 51% of the participants. The cohort includes a wide range of occupations and four racial/ethnic groups, with minorities oversampled: whites (38%), Chinese American (11%), blacks (28%), and Hispanics (23%). This study uses data from the baseline medical exam with the exception of job characteristics variables, which were collected 1.5–2 years later. The MESA study protocol was approved by the Institutional Review Board in each field centre as well as in the National Heart, Lung, and Blood Institute; written informed consent was obtained from each participant. The current analysis was approved by the Human Subject Review Board of the National Institute for Occupational Safety and Health.
Subclinical CVD measurements
Carotid IMT measurements were obtained from high-resolution B-mode ultrasonography (Logiq 700 ultrasound machine; GE Medical Systems, Waukesha, Wisconsin). At each of the six field centres, trained technicians scanned the left and right near and far walls of the carotid arteries. CCA-IMT was measured over a distance of 10 mm proximal to the common carotid bulb, and ICA-IMT was measured at the level of the carotid bifurcation (common carotid artery bulb and proximal internal carotid artery). The images were then sent to a central ultrasound reading centre (Department of Radiology, Tufts-New England Medical Center, Boston, Massachusetts), where carotid IMTwas measured by six trained readers. For each carotid artery segment, IMT was defined as the mean of the maximal IMT of the near and far walls on both the left and right sides. In order to assess intra- and inter-reader reproducibility, a 5% random sample was re-read by either the same or a different reader without any knowledge of the previous reading. Intra-class correlation coef-ficients for intra-reader reproducibility of CCA- and ICA-IMT both exceeded 0.98 and for inter-reader reproducibility were 0.87 and 0.94, respectively.
Occupation
Occupational information was collected in a self-administered questionnaire. Four open-ended questions modelled on the US Census occupation questions were asked to determine the respondent's current occupation. Of the 6814 MESA participants, 308 (4.5%) had never worked outside the home, and 146 (2.1%) did not provide occupational information. These respondents were excluded from the analyses, leaving 6360 participants. In this older cohort (45–84 years old), about half of the respondents (n=3213, 50.5%) were no longer working. In such a case, they were asked to report their main occupation before they stopped working.
The responses were coded using Census 2000 Occupation Codes and then categorised into six categories according to the census system: (1) management/professional, (2) service, (3) sales/office, (4) farming, fishing and forestry, (5) construction, extraction and maintenance, and (6) production, transportation and material moving. Because the last three categories included only a small number of participants in this sample, they were combined into one category of `blue-collar jobs'.
Job control and job demands
A subsample of participants who were working at the time of data collection provided data on job demands and job control using the Job Content Questionnaire.23 More details of the subsample are provided in the data analysis section below. Previous studies have found that job strain and low job control are both associated with CVD.1 The job demands scale had five items (eg, `have to work fast', `have to work hard'), and the job control scale had nine items (eg, `have a lot of say in my job'). All items had a 4-point response scale, ranging from `never/almost never' to `often'. The average scores were calculated for individuals. Both scales had an acceptable level of internal consistency (Cronbach's α=0.70 for job demands, 0.84 for job control).
In addition to examining job demands and job control separately, we explored the association between IMT and job strain, a combination of high job demands and low job control.15 Several ways of formulating job strain have been proposed.24 In this study, we compared the following five formulations. The quadrant term was formed by dichotomising the job demands and job control scores at the sample median and defining the four combinations as follows: high strain (high demands/low control), passive (low demands/low control), active (high demands/high control) and low strain (low demands/high control). Tertiles were formed by trichotomising the job demands and job control scores and defining various combinations as follows: high strain (control tertile lower than demands tertile), intermediate strain (control and demand have the same tertile) and low strain (control tertile higher than demands tertile). The quotient term was calculated as demands divided by control. The linear term was calculated as control subtracted from demands. Finally, the multiplicative interaction term was created as a product of demands and control.
Confounders
Additional covariates included established risk factors for CVD.22 Height and weight were measured with light clothes on and shoes off at each field centre, and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Smoking status was determined by self-report as current smoker, former smoker and never smoker. Resting blood pressure was measured with an automated sphygmomanometer (Dinamap model Pro 100; Critikon, Tampa, Florida) three times at 5 min intervals, and the average of the last two measurements was used. Through review of medications, hypertension medication use was identified. Diabetes was determined by fasting serum glucose being greater than 125 mg/dl, self-reported physician diagnosis or diabetes medication use. Total and HDL cholesterol levels were obtained from fasting blood samples, and the total-to-HDL cholesterol ratio was calculated. Other socio-demographic information was also collected on the questionnaire: age, household income (less than US$20 000, US $20 000–US$49 999, and US$50 000 or more), educational level (less than high school diploma, high school diploma or some college, college degree or higher) and place of birth (one of the 50 states in the USA, Puerto Rico or another country).
Data analysis
All analyses were performed with SAS v 9.2. Multiple linear regression was used to assess associations between IMT and occupational category, job demands, job control and various formulations of job strain. Associations between these occupational characteristics and IMT were examined in sequential models. We first adjusted for age, sex, race/ethnicity and place of birth (model 1), then traditional CVD risk factors (ie, smoking, diabetes, BMI, total/HDL cholesterol ratio, systolic blood pressure, hypertension medication) were added (model 2) and finally income and education were included (model 3). As there was no evidence of statistical interaction between sex and occupational variables in the IMT regression models adjusted for age, no sexstratified analysis was conducted. Occupational category, job demands and job control had no significant interaction with race/ethnicity on IMT; therefore, we analysed data without stratification by race/ethnicity.
Full-sample analysis
We examined the association between occupational category and IMT with the full sample with occupational information (n=6360), which included both current and retired workers, under the assumption that the current or main occupation before retirement is a reasonable proxy for SES and the long-term occupational exposures most likely to be relevant to the development of atherosclerosis. This is a reasonable assumption because the US Bureau of Labour Statistics (BLS) reported that for individuals over 45 years of age, the median job tenure was about 10 years in 1998.25 The BLS also reported little difference in job tenure across white and African American workers, but those of Hispanic origin tended to have a shorter job tenure than whites or African Americans.25 The analysis was adjusted for current working status (ie, employed vs retired). We also ran the models with current workers as sensitivity analysis.
Subsample analysis
For the analysis of job strain and IMT, the same sequential models (models 1, 2 and 3) were run with a subsample of the participants. The job strain measures were restricted to current workers because assessments of the job the respondent no longer has will be subject to various biases. The job strain variables (job control, job demands) were collected from current workers 1.5–2 years after all other data were collected. At the time of the job strain data collection, 3066 respondents were working. Of those, 15 (0.5%) did not provide current occupation, and 250 (8.2%) had changed jobs after IMT data collection. These respondents were excluded from the subsequent analysis. The subsample for job strain analysis consisted of 2801 respondents (91.4% of current workers) who held the same job at the time of IMT and job strain data collection. We assumed that job characteristics had remained relatively stable over 1.5–2 years.26
RESULTS
The descriptive statistics for both the full and subsample are presented in table 1. The average age was 62 years for the full sample, and 56 years for the subsample of current workers. The full sample consisted of 49% males, 40% white workers and 30% immigrants; in the subsample of current workers, the proportions of males (53%) and white participants (43%) were slightly higher than the full sample. The largest occupational group was management/professional for both the full and subsamples (44% and 50%). Compared to the full sample, the subsample of current workers tended to be younger, with higher household income and more education. Current workers had thinner mean IMT than the full sample.
Table 1.
Characteristics of study participants included in the full sample and the subsample (current workers)
| Characteristic | Full sample (n = 6360) | Subsample for job strain analysis (n = 2801) |
|---|---|---|
| Demographics | ||
| Age (years), mean (SD) | 61.9 (10.2) | 56.4 (8.2) |
| Male, n (%)* | 3110 (48.9) | 1487 (53.1) |
| Race/ethnicity | ||
| White, n (%) | 2521 (39.6) | 1193 (42.6) |
| Chinese American, n (%) | 694 (10.9) | 303 (10.8) |
| Black, n (%) | 1805 (28.4) | 753 (26.9) |
| Hispanic, n (%) | 1340 (21.1) | 552 (19.7) |
| Foreign born, n (%) | 1834 (29.8) | 834 (29.8) |
| Employment status | ||
| Employed, n (%) | 3147 (49.5) | 2801 (100.0) |
| Retired, unemployed or on leave, n (%) | 3213 (50.5) | - |
| Occupational group,† n (%) | ||
| Management/professional | 2765 (43.5) | 1393 (49.7) |
| Sales and office | 1360 (21.4) | 568 (20.3) |
| Service | 1006 (15.8) | 416 (14.9) |
| Blue-collar | 1229 (19.3) | 424 (15.1) |
| Psychosocial job characteristics | ||
| Job control, mean (SD) | - | 28.6 (7.5) |
| Psychological job demands, mean (SD) | - | 74.6 (15.1) |
| Socioeconomic indicators | ||
| Gross household income, n (%) | ||
| <US$20000 | 1412 (22.5) | 310 (11.1) |
| $US20000–US$49000 | 2305 (36.7) | 990 (35.5) |
| ≥US$50000 | 2559 (40.8) | 1489 (53.4) |
| Education, n (%) | ||
| Less than high school diploma | 1039 (16.4) | 285 (10.2) |
| High school diploma or some college | 2980 (46.9) | 1243 (44.4) |
| College degree or higher | 2336 (36.8) | 1271 (45.4) |
| Traditional risk factors for cardiovascular disease | ||
| Smoking status, n (%) | ||
| Never smoker | 3142 (49.4) | 1423 (50.8) |
| Former smoker | 2375 (37.4) | 995 (35.6) |
| Current smoker | 838 (13.2) | 381 (13.6) |
| Diabetes, n (%) | 700 (11.0) | 223 (8.0) |
| Body mass index, n (%) | ||
| <25.0 | 1795 (28.2) | 780 (27.9) |
| 25.0–29.9 | 2505 (39.4) | 1122 (40.0) |
| ≥30.0 | 2060 (32.4) | 899 (32.1) |
| HDL cholesterol level (mg/dl), mean (SD) | 50.9 (14.8) | 50.3 (14.6) |
| Total cholesterol level (mg/dl), mean (SD) | 193.9 (35.8) | 193.2 (34.9) |
| Systolic blood pressure (mm Hg), mean (SD) | 126.2 (21.3) | 121.6 (19.1) |
| Hypertension medication use, n (%) | 2358 (37.1) | 788 (28.2) |
| CCA-IMT (mm), mean (SD) | 0.87 (0.19) | 0.82 (0.17) |
| ICA-IMT (mm), mean (SD) | 1.07 (0.60) | 0.96 (0.51) |
CCA-IMT, common carotid artery intima-media thickness; ICA-IMT, internal carotid artery intima-media thickness.
All percentages are calculated as column percentage.
For retired or unemployed workers, the main job before they stopped working was reported.
Occupational category and IMT: full sample analysis
The associations between IMT and occupational category are presented in table 2. Mean CCA-IMT was greater for blue-collar jobs than management/professional jobs (mean difference=0.022 mm, p<0.001) after adjustment for age, sex and race/ethnicity (model 1). This association was slightly attenuated when traditional CVD risk factors were added to the model (model 2) but was still statistically significant (mean difference=0.012 mm, p=0.049). After income and education were adjusted for (model 3), the mean difference between management/professional and blue-collar jobs was no longer statistically significant.
Table 2.
Mean differences (95% CIs) in CCA-IMT and ICA-IMT (mm) by occupational group (full sample, n=6360)
| Model 1: adjusted for age, sex, race/ethnicity, place of birth |
Model 2: additional adjustment for traditional CVD risk factors* |
Model 3: additional adjustment for education, household income |
||||
|---|---|---|---|---|---|---|
| Occupational group | Mean difference | (95% CI) | Mean difference | (95% CI) | Mean difference | (95% CI) |
| Outcome: CCA-IMT | ||||||
| Management/ professional (reference) | - | - | - | - | - | - |
| Sales/office | 0.008 | (−0.003 to 0.019) | 0.002 | (−0.009 to 0.013) | −0.004 | (−0.016 to 0.008) |
| Service | 0.011 | (−0.002 to 0.024) | 0.004 | (−0.009 to 0.017) | −0.004 | (−0.019 to 0.011) |
| Blue-collar | 0.022 | (0.010 to 0.034) | 0.012 | (0.000 to 0.024) | 0.004 | (−0.010 to 0.018) |
| Outcome: ICA-IMT | ||||||
| Management/ professional (reference) | - | - | - | - | - | - |
| Sales/office | 0.071 | (0.034 to 0.109) | 0.051 | (0.015 to 0.088) | 0.026 | (−0.016 to 0.066) |
| Service | 0.057 | (0.014 to 0.100) | 0.038 | (−0.005 to 0.080) | 0.005 | (−0.043 to 0.054) |
| Blue-collar | 0.110 | (0.070 to 0.150) | 0.083 | (0.044 to 0.122) | 0.048 | (0.011 to 0.094) |
CCA-IMT, common carotid artery intima-media thickness; ICA-IMT, internal carotid artery intima-media thickness.
Smoking status, diabetes, body mass index, total/HDL cholesterol ratio, systolic blood pressure and hypertension medication.
Occupational category was more strongly associated with ICA-IMT. Sales/office, service and blue-collar jobs all had a significantly higher mean ICA-IMT than management/professional jobs after adjustment for age, sex, race/ethnicity and place of birth (model 1). After traditional CVD risk factors were adjusted for, service jobs were no longer significantly different from management/professional jobs; however, sales/office and blue-collar jobs continued to have significantly higher ICA-IMT than management/professional jobs (model 2). The significant difference between blue-collar jobs and management/professional jobs persisted after income and education were added to the model (mean difference=0.048 mm, p 0.045). As sensitivity analyses, we ran the same models with the currently employed participants only (n=3147). The results followed a similar pattern as the full sample analyses. The association between occupational category and IMT was greater for ICA than for CCA, and the difference in ICA-IMT between management/professional and blue-collar workers remained nearly significant even in model 3 (mean difference=0.053 mm,p=0.067).
Job control, job demands and IMT: analysis of current workers
Analyses of job control and job demands were restricted to the subsample of participants (n=2801) who held the same job at the time of IMT data collection and job characteristics measurement. The job control score was significantly higher for management/professional jobs (80.5) than for all other groups (p<0.001), and service jobs had a significantly lower score (66.5) than any other group (p<0.001). The job control scores for sales/office (70.6) and blue-collar jobs (68.5) did not differ significantly. Management/professional jobs had the highest mean job demands score (29.1), followed by sales/office (28.4), service (28.3) and blue-collar jobs (27.6). The only statistically significant difference was between management/professional and blue-collar jobs (p=0.003).
Table 3 shows associations of carotid IMT with job control and job demands in the subsample. Job control had a statistically significant association with CCA-IMT: a 1 SD increase in job control was associated with a 0.009 mm thinner CCA-IMT after adjustment for age, sex, race/ethnicity and place of birth (model 1). After the traditional CVD risk factors were added to the model (models 2), the association was slightly attenuated but still statistically significant. In model 3, when additional SES indicators were included in the model, a 1 SD increase in job control was associated with a 0.007 mm thinner CCA-IMT with a p value of 0.053. Greater job control was also associated with a thinner ICA-IMT, but the association did not reach statistical significance even in model 1 (b=−0.017, p=0.079). Job demands were not associated with IMT in either location.
Table 3.
Mean differences (95% CIs) in CCA-IMT and ICA-IMT (mm) associated with job control and job demands before and after adjustment for covariates (current workers only, n=2801)
| Model 1: adjusted for age, sex, race/ethnicity, place of birth |
Model 2: additional adjustment for traditional CVD risk factors* |
Model 3: additional adjustment for education, household income |
||||
|---|---|---|---|---|---|---|
| Job characteristic | Mean difference | (95% CI) | Mean difference | (95% CI) | Mean difference | (95% CI) |
| Outcome: CCA-IMT | ||||||
| Job control† | −0.009 | (−0.016 to −0.003) | −0.007 | (−0.013 to −0.003) | −0.007 | (−0.014 to 0.000) |
| Job demands† | −0.000 | (−0.007 to 0.006) | −0.001 | (−0.008 to 0.005) | −0.001 | (−0.007 to 0.005) |
| Outcome: ICA-IMT | ||||||
| Job control† | −0.017 | (−0.037 to 0.002) | −0.008 | (−0.027 to 0.011) | −0.001 | (−0.022 to 0.020) |
| Job demands† | 0.005 | (−0.014 to 0.024) | 0.005 | (−0.014 to 0.024) | 0.057 | (−0.013 to 0.025) |
CCA-IMT, common carotid artery intima-media thickness; ICA-IMT, internal carotid artery intima-media thickness.
Smoking status, diabetes, body mass index, total/HDL cholesterol ratio, systolic blood pressure and hypertension medication.
Regression coefficients were calculated for a 1 SD difference.
Finally, we examined five formulations of job strain with the same multivariate regression models (table 4). Three formulations of job strain (ie, tertiles, quotient term and linear term) had a statistically significant association with CCA-IMT when covariates were limited to demographic characteristics (model 1). These associations did not remain significant when CVD risk factors were added to the model. There were no significant associations between job strain (in any formulation) and ICA-IMT. For both CCA-IMT and ICA-IMT, there was suggestive evidence of an interaction between job demands and control in the form of the multiplicative term, although it did not reach statistical significance at the 0.05 level (p=0.073–0.078 for CCA-IMT, p=0.064–0.091 for ICA-IMT). Figure 1 illustrates the nature of the interaction between job demands and job control on CCA-IMT. For those who reported low levels of job demand, job control was not associated with IMT; however, for those who reported high levels of job demand, high levels of job control were strongly associated with thinner IMT. The magnitude of associations was unaffected by adding traditional CVD risk factors or SES indicators (ie, income, education, occupational category).
Table 4.
Mean differences (95% CIs) in CCA-IMT and ICA-IMT (mm) associated with job strain before and after adjustment for covariates (current workers only, n=2801)*
| Model 1: adjusted for age, sex, race/ethnicity, place of birth |
Model 2: additional adjustment for traditional CVD risk factors† |
Model 3: additional adjustment for education, household income |
||||
|---|---|---|---|---|---|---|
| Job strain formulation | Mean difference | (95% CI) | Mean difference | (95% CI) | Mean difference | (95% CI) |
| Outcome: CCA-IMT | ||||||
| Quadrant term (ref: low strain) | ||||||
| High strain | 0.011 | (−0.006 to 0.029) | 0.005 | (−0.012 to 0.022) | 0.004 | (−0.014 to 0.021) |
| Passive | 0.000 | (−0.017 to 0.017) | −0.007 | (−0.023 to 0.010) | −0.008 | (−0.025 to 0.009) |
| Active | −0.007 | (−0.024 to 0.009) | −0.011 | (−0.026 to 0.005) | −0.010 | (−0.026 to 0.005) |
| Tertiles (ref: low strain) | ||||||
| High | 0.015 | (0.000 to 0.031) | 0.009 | (−0.006 to 0.023) | 0.009 | (−0.007 to 0.024) |
| Intermediate | 0.006 | (−0.009 to 0.021) | 0.001 | (−0.013 to 0.015) | 0.001 | (−0.014 to 0.015) |
| Quotient term‡ | 0.007 | (0.001 to 0.014) | 0.005 | (−0.001 to 0.011) | 0.005 | (−0.001 to 0.011) |
| Linear term‡ | 0.006 | (0.000 to 0.012) | 0.003 | (−0.003 to 0.010) | 0.003 | (−0.003 to 0.009) |
| Multiplicative term§ | −0.006 | (−0.012 to 0.001) | −0.005 | (−0.011 to 0.001) | −0.005 | (−0.011 to 0.001) |
| Outcome: ICA-IMT | ||||||
| Quadrant term (ref: low strain) | ||||||
| High strain | 0.013 | (−0.041 to 0.066) | −0.003 | (−0.055 to 0.050) | −0.016 | (−0.070 to 0.038) |
| Passive | 0.001 | (−0.050 to 0.052) | −0.024 | (−0.075 to 0.026) | −0.038 | (−0.090 to 0.014) |
| Active | −0.030 | (−0.080 to 0.020) | −0.038 | (−0.087 to 0.011) | −0.038 | (−0.087 to 0.011) |
| Tertiles (ref: low strain) | ||||||
| High | 0.009 | (−0.007 to 0.024) | −0.022 | (−0.066 to 0.022) | −0.022 | (−0.068 to 0.025) |
| Intermediate | 0.001 | (−0.014 to 0.015) | −0.031 | (−0.075 to 0.013) | −0.034 | (−0.078 to 0.010) |
| Quotient term‡ | 0.017 | (−0.002 to 0.037) | 0.013 | (−0.006 to 0.032) | 0.011 | (−0.008 to 0.030) |
| Linear term‡ | 0.015 | (−0.004 to 0.035) | 0.009 | (−0.010 to 0.028) | 0.005 | (−0.014 to 0.025) |
| Multiplicative term§ | −0.014 | (−0.030 to 0.002) | −0.015 | (−0.030 to 0.001) | −0.015 | (−0.031 to 0.001) |
CCA-IMT, common carotid artery intima-media thickness; ICA-IMT, internal carotid artery intima-media thickness.
Each formulation was tested separately.
Smoking status, diabetes, body mass index, total/HDL cholesterol ratio, systolic blood pressure and hypertension medication.
Regression coefficients were estimated for a 1 SD increase.
Additionally adjusted for job control and job demands in all models.
Figure 1.
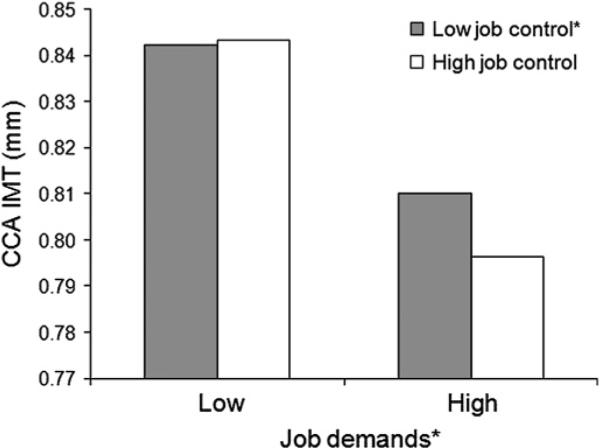
Interaction between job demands and job control on predicted common carotid artery intima-media thickness (CCA-IMT; mm). * Sample median (78 for job control, 28 for job demands) was used to define high and low groups.
DISCUSSION
This study examined associations of occupational groups and job characteristics with CCA-IMT and ICA-IMT in a multi-ethnic community sample. We found that two aspects of the job (occupational category, job characteristics) had different associations with two segments of carotid IMT. Overall, our results provide evidence that blue-collar jobs and low levels of job control are associated with early stages of atherosclerosis.
Carotid IMT, occupational category and job characteristics: segment-specific associations
We examined the two segments of carotid IMT separately. Occupational groups were more strongly associated with ICA-IMT than with CCA-IMT. Our results are similar to the findings from the Malmö study, which documented that unskilled manual jobs were associated with greater yearly progression of carotid IMT in the bifurcation area but not in the CCA.10 The British Regional Heart Study also found that manual (vs non-manual) occupations were associated with plaques and bifurcation IMT but not with CCA-IMT.27 The ICA and bifurcations are likely to have plaque accumulation, while plaques in the CCA are rare.28 Because IMT measurements in our study included plaque with the wall thickness, the stronger association between occupational groups and ICA-IMT may in fact reflect an association between occupational groups and plaques.
Job control, on the other hand, was more strongly associated with CCA-IMT than with ICA-IMT in our analysis, but the significant association was attenuated when traditional CVD risk factors were adjusted for. CCA-IMT is more strongly associated with blood pressure than the IMT of other carotid segments.19 29 The significant association between low job control and high blood pressure has been well established.24 26 30 Taken together with these findings, our results suggest that low job control may affect CCA-IMT through its associations with CVD risk factors such as high blood pressure.
Several studies have reported that CCA-IMT, which rarely includes plaques,28 and plaques in other areas in carotid arteries have different associations with clinical CVD.21 Ebrahim et al reported that CCA-IMT was associated with stroke while plaques were associated with angina and ischaemic heart disease.27 Combined with this information, our findings of job control suggest that the association between a lack of job control and stroke mortality31 may be mediated by increased CCA-IMT. Blue-collar jobs, on the other hand, may be associated with plaque development and higher risks for angina and ischaemic heart disease . Different aspects of the job may affect vascular health differently, and thus considering occupation from multiple perspectives is important in order to better understand occupational impacts on health.
Differences in IMT across occupational categories
This study adds to the relatively few reports on associations between IMT and occupational category. The four occupational groups we used in this study (management/professional, office/sales, service and blue-collar) are often considered as ordinal in the socioeconomic spectrum. Our results showed that the ICA-IMT difference between management/professional and blue-collar jobs was significant after controlling for traditional CVD risk factors. In a meta-analysis, Lorenz et al reported that a 0.1 mm difference in ICA-IMT was associated with a 4% increase in myocardial infarction incidence and a 6% increase in stroke incidence after adjustments were made for age, sex and CVD risk factors.14 Since our result for blue-collar jobs was only slightly smaller (0.083 mm) than the unit (0.1 mm) Lorenz et al used, the clinical significance of the difference between management/professional and blue-collar jobs is likely to be slightly less than the Lorenz et al results.
We also found that the significant difference was sustained even after adjustments were made for other individual level SES indicators (ie, household income, education). This suggests that blue-collar jobs may pose CVD risks through mechanisms other than their associations with socioeconomic disadvantage. In the USA, occupational status is strongly patterned by race/ethnicity,32 and racial/ethnic minorities are over-represented in blue-collar jobs in general.33 Therefore, our findings indicate that racial/ethnic disparities in CVD may be partly explained by disparities in occupation. Further analysis is needed to test such a hypothesis.
Job strain and IMT
Job strain (a combination of high job demands and low job control) in general did not have strong associations with IMT in our study. The quadrant term, the original and frequently used formulation of job strain, had no significant associations with IMT, which is consistent with the Young Finns study.3 4 9 The quadrant term of job strain, which is based on dichotomised variables, may be limited in its ability to capture meaningful variability in job strain. In contrast to results for the quadrant term, and consistent with results from the Young Finns study, we found that quotient and linear terms (both continuous variables) had a significant association with CCA-IMT, although in our analysis the associations were attenuated once traditional CVD risk factors and SES variables were included in the model.
The multiplicative interaction term, however, had somewhat promising results. Consistent with the demande–control model's prediction, the association between high job control and thinner IMT was stronger for those with high job demands after accounting for traditional CVD risk factors and SES variables (figure 1). While this interaction between job control and job demands on IMT did not reach statistical significance at the 0.05 level (p=0.06–0.09), Pedhazur34 suggests increasing the threshold for statistical significance when a product term is used to ascertain interaction in cross-sectional analysis. This interaction suggests that intervention efforts to prevent atherosclerosis through enhanced job control should be focused on those who are in high demand jobs.
One reason for the lack of a strong association between job strain and IMT in our study could be that job characteristics data were only available 1.5–2 years after IMT data had been collected. Even though we restricted the analysis to those who held the same job, potential changes in job characteristics during that time may have resulted in exposure misclassification, which could bias the results toward the null. Using the same job control and job demands scales with the same response options in a wide range of workers, Schnall et al reported that for those who stayed in the same company, the mean scores changed very little over 3 years: 0.24 for job control and −1.16 for job demands (calculated from table 2 in Schnall et al).26 In our study, the magnitude of these changes represents less than 1% of the mean job control score (28.6) and 1.6% of the mean job demands score (74.6). Therefore, it is unlikely that potential misclassification would have had a major impact on our findings.
Study strengths and limitations
Major strengths of this study include a large, multi-ethnic, community-based sample with a wide array of occupations and the use of well established measures of job characteristics. However, several limitations should be acknowledged in interpreting the findings. All occupational information was obtained through self-report, and therefore is subject to various biases (ie, recall, social desirability, acquiescence). For those who were still working, we had information on the current job. If the reported job was different from the main job in life (ie, the longest held job), this may have resulted in misclassification of the relevant occupational exposures. Those who were not working at the time of data collection provided their main job before stopping working, but no information was available on the number of years worked in the main job or the time since the job was left. This lack of information made the main job an imperfect proxy for long-term occupational exposure, especially for Hispanic workers because the US national data indicate that they tend to have a shorter job tenure than white or African American workers.25
CONCLUSION
This study examined associations of occupational category and job characteristics with subclinical CVD. The results showed that blue-collar jobs were associated with greater ICA-IMT even after adjustments were made for traditional CVD risk factors and SES. We also found that job control was associated with thinner CCA-IMT. These results highlight the potential strategies for workplace interventions in preventing the early stages of atherosclerosis, such as targeting blue-collar workers and addressing lack of job control among those with high job demands. In addition, our results suggest segment-specific associations of IMT with occupational category and job control: CCA-IMT was more strongly associated with job control, whereas ICA-IMT had a stronger association with occupational category. These different associations help us better understand the role of occupation in CVD development.
What this paper adds.
-
▶
Current literature is scarce on the relationship between occupation and segment-specific carotid intima-media thickness (IMT) and between IMT and occupational category as a socioeconomic status (SES) indicator.
-
▶
Blue-collar workers had greater internal carotid artery (ICA)-IMT than managers/professionals after adjustments were made for traditional cardiovascular disease risk factors and SES, suggesting that blue-collar jobs carry additional risk.
-
▶
Occupational category was more strongly associated with ICA-IMT, whereas job control was more strongly associated with common carotid artery (CCA)-IMT.
-
▶
Low job control was associated with greater CCA-IMT, with the association being stronger for those in high-demand jobs than in low-demand jobs.
Acknowledgements
We thank David Jacobs for his valuable comments on the discussion section. We also thank the other MESA investigators, staff and study participants for their contribution. A full list of participating MESA investigators and institutions can be found at http:www.mesa-nhlbi.org.
Funding MESA is supported by contracts N01-HC-95159 through N01-HC-95165 and N01-HC-95169 from the National Heart, Lung, and Blood Institute. Occupational coding was supported by the National Institute for Occupational Safety and Health (NORA FY08 CRN SLB8). Joel Kaufman was supported by NIEHS (K24ES013195).
Footnotes
Publisher's Disclaimer: The findings and conclusion in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
Competing interests None.
Ethics approval This study was conducted with the approval of the National Heart, Lung and Blood Institute, Columbia University, Johns Hopkins University, the National Institute for Occupational Safety and Health, the University of Minnesota, the University of California, Los Angeles, Northwestern University and Wake Forest University.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
- 1.Schnall PL, Belkic̀ K, Landsbergis PA, et al. The workplace and cardiovascular disease. Occup Med. 2000;15:1–334. [PubMed] [Google Scholar]
- 2.Nurminen M, Karjalainen A. Epidemiologic estimate of the proportion of fatalities related to occupational factors in Finland. Scand J Work Environ Health. 2001;27:161–213. doi: 10.5271/sjweh.605. [DOI] [PubMed] [Google Scholar]
- 3.Hintsa T, Kivimaäki M, Elovainio M, et al. Is the association between job strain and carotid intima-media thickness attributable to pre-employment environmental and dispositional factors? The Cardiovascular Risk in Young Finns Study. Occup Environ Med. 2008;65:676–82. doi: 10.1136/oem.2007.037622. [DOI] [PubMed] [Google Scholar]
- 4.Hintsanen M, Kivimaäki M, Elovainio M, et al. Job strain and early atherosclerosis: the Cardiovascular Risk in Young Finns Study. Psychosom Med. 2005;67:740–7. doi: 10.1097/01.psy.0000181271.04169.93. [DOI] [PubMed] [Google Scholar]
- 5.Kivimaäki M, Hintsanen M, Keltikangas-Jaärvinen L, et al. Early risk factors, job strain, and atherosclerosis among men in their 30s: The Cardiovascular Risk in Young Finns Study. Am J Public Health. 2007;97:450–2. doi: 10.2105/AJPH.2005.078873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lynch J, Krause N, Kaplan G, et al. Workplace demands, economic reward, and progression of carotid atherosclerosis. Circulation. 1997;96:302–7. doi: 10.1161/01.cir.96.1.302. [DOI] [PubMed] [Google Scholar]
- 7.Muntaner C, Nieto J, Cooper L, et al. Work organization and atherosclerosis: Findings from the ARIC Study. Am J Prev Med. 1998;14:9–18. doi: 10.1016/s0749-3797(97)00018-4. [DOI] [PubMed] [Google Scholar]
- 8.Rosvall M, Östergren P-O, Hedblad B, et al. Occupational status, educational level, and the prevalence of carotid atherosclerosis in a general population sample of middle-aged Swedish men and women: Results from the Malmö Diet and Cancer Study. Am J Epidemiol. 2000;152:334–46. doi: 10.1093/aje/152.4.334. [DOI] [PubMed] [Google Scholar]
- 9.Rosvall M, Östergren P-O, Hedblad B, et al. Work related psychosocial factors and carotid atherosclerosis. Int J Epidemiol. 2002;31:1169–78. doi: 10.1093/ije/31.6.1169. [DOI] [PubMed] [Google Scholar]
- 10.Rosvall M, Östergren P-O, Hedblad B, et al. Socioeconomic differences in the progression of carotid atherosclerosis in middle-aged men and women with subclinical atherosclerosis in Sweden. Soc Sci Med. 2006;62:1785–98. doi: 10.1016/j.socscimed.2005.08.037. [DOI] [PubMed] [Google Scholar]
- 11.Sharrett AR, Ding J, Criqui MJ, et al. Smoking, diabetes, and blood cholesterol differ in their associations with subclinical atherosclerosis: The Multiethnic Study of Atherosclerosis (MESA) Atherosclerosis. 2006;186:441–7. doi: 10.1016/j.atherosclerosis.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 12.Urbina EM, Srinivasan SR, Tang R, et al. Impact of multiple coronary risk factors on the intima-media thickness of different segments of carotid artery in health young adults (The Bogalusa Heart Study) Am J Cardiol. 2002;90:953–8. doi: 10.1016/s0002-9149(02)02660-7. [DOI] [PubMed] [Google Scholar]
- 13.Folsom AR, Kronmal RA, Detrano R, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: The Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168:1333–9. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lorenz MW, Markus HS, Bots M, et al. Prediction of clinical cardiovascular events with carotid intima-madia thickness: A systematic review and meta-analysis. Circulation. 2007;115:459–67. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 15.Karasek RA. Job demands, job decision latitude, and mental strain: Implications for job redesign. Adm Sci Q. 1979;24:285–308. [Google Scholar]
- 16.Din-Dzietham R, Liao D, Diez Roux AV, et al. Association of educational achievement with pulsatile arterial diameter change of the common carotid artery. Am J Epidemiol. 2000;152:617–27. doi: 10.1093/aje/152.7.617. [DOI] [PubMed] [Google Scholar]
- 17.Lemelin ET, Diez Roux AV, Franklin TG, et al. Life-course socioeconomic positions and subclinical atherosclerosis in the Multi-Ethnic Study of Atherosclerosis. Soc Sci Med. 2009;68:444–53. doi: 10.1016/j.socscimed.2008.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Espeland MA, Tang R, Terry JG, et al. Associations of risk factors with segment-specific intimal-medial thickness of the extracranial carotid artery. Stroke. 1999;30:1047–55. doi: 10.1161/01.str.30.5.1047. [DOI] [PubMed] [Google Scholar]
- 19.Polak JF, Person SD, Wei GS, et al. Segment-specific associations of carotid intima-media thickness with cardiovascular risk factors the coronary artery risk development in young adults (CARDIA) study. Stroke. 2010;41:9–15. doi: 10.1161/STROKEAHA.109.566596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schott LL, Wildman RP, Brockwell S, et al. Segment-specific effects of cardiovascular risk factors on carotid artery intima-medial thickness in women at midlife. Arterioscler Thromb Vasc Biol. 2004;24:1951–6. doi: 10.1161/01.ATV.0000141119.02205.6b. [DOI] [PubMed] [Google Scholar]
- 21.Terry JG, Tang R, Espeland MA, et al. Carotid arterial structure in patients with documented coronary artery disease and disease-free control subjects. Circulation. 2003;107:1146–51. doi: 10.1161/01.cir.0000051461.92839.f7. [DOI] [PubMed] [Google Scholar]
- 22.Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 23.Karasek RA, Brisson C, Kawakami N, et al. the job content questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–55. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 24.Landsbergis PA, Schnall PL, Shchwartz JE, et al. The association of ambulatory blood pressure with alternative forms of job strain. Scand J Work Environ Health. 1994;20:349–63. doi: 10.5271/sjweh.1386. [DOI] [PubMed] [Google Scholar]
- 25.Bureau of Labor Statistics . Employee tenure in 1998. U.S. Department of Labor; Washington, DC: 1998. [Google Scholar]
- 26.Schnall PL, Schwartz J, Landsbergis P, et al. A longitudinal study of job strain and ambulatory blood pressure: results from a three-year follow-up. Psychosom Med. 1998;60:697–706. doi: 10.1097/00006842-199811000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Ebrahim S, Papacosta O, Whincup P, et al. Carotid plaque, intima media thickness, cardiovascular risk factors, and prevalent cardiovascular disease in men and womendThe British Regional Heart Study. Stroke. 1999;30:841–50. doi: 10.1161/01.str.30.4.841. [DOI] [PubMed] [Google Scholar]
- 28.Zureik M, Ducimetière P, Touboul P-J, et al. Common carotid intima-media thickness predicts occurrence of carotid atherosclerotic plaques: Longitudinal results from the Aging Vascular Study (EVA) Study. Arterioscler Thromb Vasc Biol. 2000;20:1622–9. doi: 10.1161/01.atv.20.6.1622. [DOI] [PubMed] [Google Scholar]
- 29.O'Leary DH, Polak JF, Kronmal RA, et al. Thickening of the carotid wall: A marker for atherosclerosis in the elderly? Cardiovascular Health Study Collaborative Research Group. Stroke. 1996;27:224–31. doi: 10.1161/01.str.27.2.224. [DOI] [PubMed] [Google Scholar]
- 30.Steptoe A, Willemsen G. The influence of low job control on ambulatory blood pressure and perceived stress over the working day in men and women from the Whitehall II cohort. J Hypertens. 2004;22:915–20. doi: 10.1097/00004872-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Toivanen S, Hemström O. Is the impact of job control on stroke independent from socioeconomic status? A large-scale study of the Swedish working population. Stroke. 2008;39:1321–3. doi: 10.1161/STROKEAHA.107.495523. [DOI] [PubMed] [Google Scholar]
- 32.Tomaskovic-Devey D, Stainback K, Taylor T, et al. Documenting desegregation: Segregation in American workplaces in race, ethnicity, and sex, 1966–2003. Am Sociol Rev. 2006;71:565–88. [Google Scholar]
- 33.Bureau of Labor Statistics . Household data annual averages: Employed persons by detailed occupation, sex, race, and Hispanic or Latino ethnicity. US Department of Labor; Washington, DC: 2007. [Google Scholar]
- 34.Pedhazur EJ. Multiple regression in behavioral research: explanation and prediction. Harcourt Brace College Publishers; Fort Worth, TX: 1997. [Google Scholar]


