Abstract
Clinical accounts of depression underscore its relation to negative emotional experiences; yet few empirical studies examine emotional experiences in adults with depression, with even less work on depression and emotion in children. Using a nonclinical sample of school-aged children (n = 89) ages 8–12, this study evaluated whether greater mood symptoms were associated with more or less intense emotional reactions (measured via psychophysiology, subjective report, and behavior) in response to a threat paradigm. Results indicated that increased negative mood symptoms were associated with larger startle magnitude responses during threat, increased self-reports of negative emotion, and greater likelihood of crying and stopping the paradigm prematurely.
Keywords: depression, emotion, psychophysiology, dysphoria, middle childhood
Disturbance in mood and emotional experience are the hallmarks of depression in adults and children (American Psychiatric Association, 2000; Clark, Watson, & Mineka, 1994; Gross & Munoz, 1995). The precise nature of the association between depressed mood and emotion reactivity, however, is poorly understood, partly due to the lack of conceptual clarity in emotion-related constructs (Durbin & Shafir, 2008). Consistent with an affective science model (Rottenberg & Gross, 2003), we consider emotions to be coordinated reactions that involve changes in physiology, behavior, and feelings (Keltner & Gross, 1999), whereas moods are longer-lasting feeling states that have significant influence on cognitive patterns but are less clearly tied to external events. In order to adequately measure emotional reactions, investigations must probe these events using multiple methods of measurement, indexing emotion at the level of subjective experience, behavior, and psychophysiology (Mauss & Robinson, 2009). Following others (Rottenberg, Gross, & Gotlib, 2005), we assume that depressive symptoms are related to changes in mood states. However, the way in which this translates into patterns of emotional experiences is far from clear.
It is natural to expect that greater depressive symptoms would be related to altered patterns of emotional experience. Indeed, several hypotheses regarding the association between depression and emotion have been posited. The negative potentiation hypothesis (NP; Rottenberg et al., 2005) predicts that depressed people experience more negative emotion when confronted with negative situations than nondepressed individuals. This resonates with the clinical truism that depressed patients exhibit intense negative emotion and self-criticism, and that people who are depressed are more likely to cry and express distress (Rottenberg, Gross, Wilhelm, Najmi, & Gotlib, 2002). In contrast, the emotion context insensitivity hypothesis (ECI; Rottenberg & Gotlib, 2004; Rottenberg et al., 2005) suggests that depressed people show a restricted range of responding to emotional events, and specifically that they show reduced responses to both positive and negative events. Based on evolutionary formulations of depression, the ECI purports that depressed moods function to enable the individual to disengage from their environment during times when this would be evolutionarily adaptive (Rottenberg & Gotlib, 2004). Therefore, according to the ECI, depression involves a lack of emotional engagement or responding to both positive and negative stimuli (Rottenberg & Gotlib, 2004). This model of disengagement, or the absence of response during adverse circumstances, fits with the learned helplessness model of depression (Seligman, 1975; Seligman & Maier, 1967).
Importantly, both the NP and the ECI hypotheses were initially developed to explain emotional responding among adults with depressive disorders. However, they may also provide useful frameworks for understanding the link between depression and emotion in children. Beyond providing a developmental contribution to the ECI/NP debate, middle childhood is a particularly important period for examining the presence of risk factors related to the development of clinically-significant mood disturbances. The transition to adolescence represents a critical period associated with sharp increases in the prevalence of depression, particularly among girls (Hankin & Abramson, 2001; Nolen-Hoeksema & Girgus, 1994). Consistent with a diathesis-stress model of psychopathology, certain profiles of emotion reactivity under stress may heighten youths’ risk of developing worsening depressive symptoms during the transition to adolescence, constituting a pre-existing diathesis that enhances risk in the presence of additional stressors (Kovacs, Joormann, & Gotlib, 2008). Therefore, late middle childhood, the developmental period preceding adolescence, may represent an ideal window for studying emotion reactivity profiles to negative stimuli (Hankin et al., 1998). Further, consistent with a developmental psychopathology framework, an important first step in identifying emotional response profiles that may enhance risk for future depressive disorders is to evaluate concurrent associations among emotional response and mood symptoms in individuals who are not currently depressed. If cross-sectional research documents an association between emotional response profiles and mood symptoms, this will position future work to examine emotional responding as a potential risk factor for the development of depression in longitudinal designs. In sum, examination of emotional response in both nonclinical and clinical samples will be important in order to better understand risk for dysphoria and depression in children (Cole, Luby, & Sullivan, 2008; Kovacs et al., 2008).
Research Evidence for the Link between Depression and Emotion in Adults
Despite its phenotypic fit with clinical observations of depressed individuals (Rottenberg et al., 2002), the NP hypothesis has not garnered universal research support. Clinically depressed adults and adults with remitted clinical depression show greater galvanic skin response when hearing vignettes describing negative social scenes (Sigmon & Nelson-Gray, 1992). In addition, college students with greater depressive symptoms show greater physiological arousal in terms of galvanic skin responses following receipt of negative feedback (Golin, Hartman, Klatt, Munz, & Wolfgang, 1977) and during the presentation of mild electric shock (Lewinsohn, Lobitz, & Wilson, 1973). In turn, a large and growing literature documents increased amygdala activation in depressed adults in response to the presentation of negative emotional information (Mayberg et al., 1999; Sheline et al., 2001; Siegle, Steinhauer, Thase, Stenger, & Carter, 2002; Siegle, Thompson, Carter, Steinhauer, & Thase, 2007). However, substantial evidence suggests that rather than potentiation of negative emotion, depression is related to attenuated negative emotion, which contradicts the NP. For instance, depressed adults show smaller startle responses to negative images (Allen, Trinder, & Brennan, 1999).
Although the ECI may seem inconsistent with clinical perception about depression, it is consistent with depressed individuals’ experience of the world as empty and dull (Healy, 1993), as well as with the symptoms of anhedonia and social withdrawal, known to characterize many depressed individuals’ experiences. The ECI also explains the observation that depressed adult inpatients show less variability in their emotionally expressive behavior across situations (Rottenberg & Gotlib, 2004). In terms of subjective reports, depressed adults report smaller increases in positive and negative emotion in response to pleasant and unpleasant films, respectively (Kaviani et al., 2004; Rottenberg et al., 2002b). In terms of physiological indicators of emotion reactivity, depressed adults show less modulation of their electromyographical (EMG) responses than nondepressed controls in response to emotionally evocative images (Gehricke & Shapiro, 2000; Greden, Genero, Price, Feinberg, & Levine, 1986), and less modulation of brain activity in response to previously-seen positive images (Deldin, Keller, Gergen, & Miller, 2001) and to facially expressive images (Gotlib, Sivers, Canli, Kasch, & Gabrieli, 2001). Further, patients with high depression and/or anhedonia fail to show affective modulation of the startle response when watching pleasant and unpleasant film clips (Kaviani et al., 2004). In addition, preliminary evidence suggests that even among nonclinical samples, adults with greater depressive symptoms have less affective startle modulation (Mneimne, McDermut, & Powers, 2008). Finally, in contrast to clinical lore, research indicates that depressed adults are not more likely to cry after watching a film depicting themes of loss and abandonment (Rottenberg et al., 2002).
Research Evidence for the Link between Depression and Emotion in Children
Research examining the link between depressed states and emotion in children is less well-developed and findings to date are mixed with regard to context insensitivity in depressed children (Durbin & Shafir, 2008). Compared to healthy controls one study found depressed children (n = 5) show a blunted amygdala response when viewing fear faces (Thomas et al., 2001). In contrast, another study found that depressed children showed greater amygdala activation than control children when presented with fear faces (Beesdo et al., 2009). An investigation of pupil dilation, a physiological indicator of cognitive and emotional processing (Beatty, 1982; Siegle, Steinhauer, Carter, Ramel & Thase, 2003), reported that depressed children showed diminished dilation relative to controls in response to negative words (Silk et al., 2007). Further, a study examined startle response during contextual threat among children with parents with Major Depressive Disorder (MDD), who presumably would be at risk for internalizing disorders (Grillon et al., 2005), and found that, as compared to the control group, children of depressed parents have greater startle magnitude across the paradigm. Given the inconsistencies in findings across investigations, further research involving both clinical and nonclinical samples needs to be conducted on this topic. If ECI is a risk factor for the development of depression, it should have a trait-like quality, and be associated with greater mood symptoms within normative samples of children. Alternatively, if ECI is a marker of clinical depression itself (Rottenberg et al., 2005), it should not be present among individuals who are not clinically depressed.
Emotional Responsiveness to Threat: The Fear-potentiated Startle Paradigm
An important dimension of emotion reactivity is the ability to launch emotional responses of varying intensities depending on the stimuli in question (Keltner & Gross, 1999). The ability to use context cues to gauge one’s reaction to emotionally-evocative situations is central to adaptive functioning, and according to the ECI, it is this capacity that is impaired in depressed individuals (Rottenberg et al., 2005). A paradigm that lends itself well to the evaluation of emotional modulation based on context cues is fear-potentiated startle. The startle reflex is an amygdala-mediated defensive response that occurs in reaction to intense, abrupt stimuli (Bradley, 2000; Lee & Davis, 1997), is measured using the eye blink response, and is heightened in the presence of frightening contexts (Bradley, Cuthbert, & Lang 1990; Campeau & Davis, 1992; Davis, Falls, Campeau, & Kim, 1993; Lang, 1995; Lang, Greenwald, Bradley, & Hamm, 1993). Fear-potentiated startle uses anticipation of mildly aversive stimuli (e.g., air puffs) and permits the comparison of individuals’ startle responses under experimentally-induced conditions of “threat” and “safety” (Grillon et al., 1999). The use of these separate conditions enables researchers to compare individuals’ responses across conditions. Fear-potentiated startle response is increased among patients with anxiety symptoms and disorders (Grillon, Ameli, Foot, & Davis, 1993; Grillon, Ameli, Goddard, Woods, & Davis, 1994; Grillon & Morgan, 1999), as well as among children of individuals with MDD (Grillon et al., 2005), and is also sensitive to emotion reactivity manipulations (Lissek, et al., 2007).
Although the threat paradigm was initially developed to probe emotion reactivity among anxious individuals, anxiety and depressive disorders are highly comorbid conditions (Anderson, Williams, McGee, & Silva, 1987; Brown, Campbell, Lehman, Grisham, & Mancill, 2001), leading some to suggest that depression and anxiety should both be considered to be disturbances in negative affect and should be treated using unified protocols (Ehrenreich, Goldstein, Wright, & Barlow, 2009; Moses & Barlow, 2006). Therefore, since research shows that anxiety disorders and states are related to startle response using the fear-potentiated paradigm (e.g., Grillon & Morgan, 1999), response to threat may also be important to examine for its relation to depressive states in children. Further, given that individuals with greater depressive symptoms show heightened sensitivity to threats of rejection within the social sphere (Ayduk, Downey, & Kim, 2001; Borelli & Prinstein, 2003; Downey, Lebolt, Rincon, & Freitas, 1998), it also may be important to examine the association between mood symptoms and generalized threat, or threat that exists outside of the social sphere1. Finally, an accumulating body of evidence indicates amygdala hyperactivity in depressed adults and children (e.g., Beesdo et al., 2009), suggesting that psychophysiological paradigms indexing amygdala-driven responses may provide important information about mood symptoms.
The Present Study
This study investigated the association between school-aged children’s self-reported mood symptoms and their emotional response. Based on recent suggestions that assessment of emotional response ought to involve measurements of subjective, physiological and experiential manifestations of emotion (Mauss & Robinson, 2009), perhaps particularly in terms of evaluating risk for depressive disorders (Kovacs et al., 2008), we adopt a multimethod assessment strategy, sampling participants’ psychophysiological, subjective, and behavioral responses to a fear-potentiated startle paradigm. Specifically, we examined children’s startle magnitude during conditions of “threat” (relative to their response during “safety”), their self-reported changes in negative emotion from pre- to post-startle paradigm, and behavioral signs of negative affectivity, such as crying and stopping the paradigm prematurely. Given the recent suggestion that support for the ECI is found in the affective startle responses of a nonclinical sample of adults (Mneimne et al., 2008), an additional goal of the current investigation was to evaluate whether children’s emotional responses can be interpreted as supportive of the extant theories of emotion and depression in adults (the ECI and the NP hypotheses). Specifically, we hypothesized that if mood symptoms were related to decreased responsiveness to negative emotional stimuli (such that higher mood symptoms are associated with lesser startle magnitude during threat, smaller increases in negative emotion, and lesser likelihood of crying or stopping the paradigm early), this would provide evidence for the ECI model. Conversely, if we found that children’s mood symptoms were positively associated with negative emotional response (greater startle magnitude during threat, greater increases in self-reported negative emotion, and a greater likelihood of crying and stopping the paradigm early), this would provide evidence for the NP model.
Method
Participants
Ninety-seven 8 to 12-year-old children participated in this study and were recruited from the community through a variety of means, including internet postings, flyers, and a mass mailing. A total of 131 parents initially contacted the research team expressing interest in the study, only 103 (79%) could be recontacted for participation. Ninety-four percent (n = 97) of these enrolled in the study. Two children (2%) failed to complete the second study session due to schedule conflicts, and an additional 6 (6%) children’s startle data was unusable due to equipment malfunction during the time of their lab visit. Thus, eighty-nine children provided sufficient data for the startle analyses reported here.
The final sample included 56.6% boys and 43.3% girls with a mean age of 10.01 years old (SD = 1.52), with 86.6% Caucasian, 3.1% Hispanic, 3.1% African American, and 7.2% biracial children. Educational background data were collected on a subset of the sample (25%) randomly selected from the larger sample. These data indicated that the sample was moderately educated (M = 1.85, SD = .67, where 1 = high school education, 2 = some college, 3 = postgraduate).
Procedure
Prior to beginning data collection, approval from the Human Investigation Committee was obtained for the protocol. The data reported here were part of a larger study examining 8 to 12 year-old children’s socioemotional development. The goal of the larger investigation was to examine the interrelations between children’s mental representations of attachment relationships, clinical symptoms, and emotional response to threat. The cross-sectional design involved two sessions approximately one week apart, each of which lasted 1.5 hours. All children completed the protocol in a fixed order.
Participants and their parents completed informed consent and assent forms upon arrival at the laboratory. Experimenters informed children that they could refuse to participate in any part of the study if they wished. Parents also completed a short demographic form. During the remainder of the first session children completed an attachment interview, the results of which are discussed elsewhere (Borelli et al., 2010). During the second session child participants first completed a measure of state affect (Positive and Negative Affective Scale for Children, PANAS-C), then the fear-potentiated startle paradigm, followed by another PANAS-C measure. Children then completed the Children’s Depression Inventory (CDI; Kovacs, 1992) and the Penn State Worry Questionnaire for children (Chorpita, Tracey, Brown, Collica, & Barlow, 1997). In order to minimize the impact of reading ability on participants’ responses, all questionnaires were delivered via computer (one item per screen, text plus audio, repeatable, female voice)(Fisher & Mayes, 2001). Children used a computer touchscreen to input their desired response choice.
Measures
Children’s Depression Inventory
The Children’s Depression Inventory (CDI; Kovacs, 1992) consists of 27-items designed to assess the behavioral, cognitive, emotional, and physiological features of depression in children aged 7 to 17. Participants choose one of three statements which best describes their symptoms over the past two weeks (e.g., “I am sad once in a while, ”“I am sad many times,” “I am sad all the time”). Responses are coded on a scale of 0 to 2, with higher scores indicating more severe mood symptoms. In the current sample, eleven children (12.36%) reported mood symptoms exceeding Kovac’s mild depression cut-off score of 13 (Kovacs, 1992). The psychometric properties of the CDI have been reported in past work (Kovacs, 1992; Saylor, Finch, Spirito, & Bennett, 1984). Cronbach’s alpha in this sample was .82.
Penn State Worry Questionnaire for Children
The PSWQ-C (Chorpita, Tracey, Brown, Collica, & Barlow, 1997) is a 14-item self-report questionnaire that is designed to assess symptoms of worry and generalized anxiety disorder in children aged 8 to 12. Participants rate how true the items are for them on a 4 point scale (e.g., “Many things make me worry), with a score of 0 signifying “not at all true” and a score of 3 signifying “always true”. The reliability and validity of the measure have been demonstrated in clinical and non-clinical samples (Chorpita et al., 1997; Muris, Meesters, & Gobel, 2001). Cronbach’s alpha in this sample was .77.
Positive and Negative Affect Scale for Children
The PANAS-C (Laurent et al., 1999) is a 30-item self-report measure of affect for children between the ages of 8 and 13. Children rate the degree to which they feel emotion words (e.g., “nervous”) on a scale of 1 to 5, with a score of 1 signifying “very slightly or not at all” and a score of 5 signifying “extremely.” Reliability and validity data for the measure suggest that it is an appropriate measure for state affect in children (Laurent et al., 1999). In the current investigation, children were asked to rate how they felt “right now”. Cronbach’s alpha in this sample was excellent (.90 and above for both scales).
Fear-potentiated Startle
In the fear-potentiated startle paradigm, children watched pictures come on a computer screen while headphones delivered auditory probes designed to elicit a startle reaction (Grillon, Dierker, & Merikangas, 1998). They were told that they may receive a puff of air to the neck (threat condition), which was delivered through a collar fastened around the neck, when a certain picture is displayed on the computer screen. Participants were also told that when another picture was on the computer screen (safe condition), they would not receive puffs of air. The entire paradigm consisted of 64 auditory startle probes delivered at different times following the onset of a safety or threat picture (i.e., at 1, 3, 7, and 9 seconds, the order of which was held constant across participants). Startle probes did not occur during the period of time between each trial, or the inter-trial intervals.
The startle assessment took place in a quiet, dimly lit room (60 watt bulb). The child sat in a comfortable chair facing a color monitor at a distance of 50 cm and a visual angle of approximately 4 degrees. The threat and safety signals appeared as 15 cm × 22 cm colored images green/yellow and blue/purple against a black background. Signal identity color was counterbalanced across subjects. For each participant, this color-signal mapping was held constant throughout the course of the paradigm. Images were presented at random positions on the screen (random number generation of x, y coordinates in Eprime software).
The aversive stimulus (air puff) was an 80 psi burst of breathable air with variable duration (50ms, 100 ms, 150 ms) directed at the larynx through rigid 8 mm nylon 11 tubing. The duration of the air puff varied across the experiment to influence the child’s perceived intensity of the puff (5 puffs in total), but the pattern was consistent across subjects. Instructions conveyed that some puffs would be stronger than others. Acoustic startle probes were 40 ms long, 103 dB white noise bursts, with instantaneous rise time, presented binaurally through AERO ear-canal conforming earplugs.
After a four startle probes (baseline), the experimental portion of the task began. The paradigm consisted of five blocks of signals. Within each block, there were four safe and four threat signals, for a grand total of twenty safe and twenty threat signals. Each signal (picture on the computer screen) lasted 11 s, during which time one startle probe was presented (at 1s, 3s, 7s, and 9s). The inter-trial interval (ITI), during which a black screen was presented, occurred between each signal and varied from 3 to 19s (mean = 12s). Air puffs were administered randomly on five of the 20 threat signals. In each block, only one air puff was given under one of five threat trials. If an air puff occurred during a threat trial, it always occurred between 2 and 10 seconds into the threat signal and after the startle probe for that trial had been presented. Startle sessions were videotaped and displayed on a screen behind a barrier in the startle lab room so that the experimenter could watch the child unobtrusively.
Electromyographic (EMG) activity of the left orbicularis oculi muscle was recorded via two miniature (contact area <4 mm) Ag/AgCl electrodes filled with Grass electrode cream. After exfoliation (using Nuprep), one electrode was positioned below the eyelid in line with the pupil in forward gaze. A second electrode was placed ~2 cm lateral to the first. A ground (reference) electrode was placed on the inner side of the left forearm. The startle system recorded EMG activity for 500 ms (sample interval 1 ms) beginning 200 ms prior to the onset of the startle stimulus. The amplification gain control for the EMG signal was kept constant for all subjects. Recorded EMG activity was band-pass filtered before digitizing; cut-off frequencies were set at 100 hz and 1 kHz. A 60-Hz notch filter was used to eliminate the 60-Hz interference. Data were scored offline for response amplitude and magnitude (in arbitrary analog to- digit units) and latencies to response peak (in ms). The scoring program contained a rolling average routine that smoothed the rectified EMG response. Latency to response peak was determined as the point of maximal amplitude that occurred within 120 ms from the startle stimulus (20 ms baseline). For the purposes of these analyses, we use measures of startle magnitude, which includes 0 startle responses. Startle magnitude was standardized using a t-transformation.
Behavioral Markers of Distress
The experimenter administering the startle paradigm was asked to identify whether the child began crying during the paradigm and/or requested to stop the paradigm early. The experimenter was separated from the child by a partition but was able to view the child’s face as it was displayed on a large television monitor adjacent to the experimenter seat. Experimenters were instructed to record that the child was crying only if they could see tears on their faces. All children who asked to terminate the paradigm early were allowed to do so. These two variables were coded dichotomously (present/absent) for the purpose of data analyses. Eight children (9%) cried and 7 (8%) stopped early (see Table 2).
Table 2.
Behavioral Responses by Sex
| Total (N = 89) | Boys (n = 50) | Girls (n =39) | Sex Differences Pearson Chi-Square |
|
|---|---|---|---|---|
| Crying During Startle | ||||
| Didn’t Cry | 81 | 45 | 36 | |
| Cried | 8 | 5 | 3 | |
| 0.14 | ||||
| Stopping Startle Early | ||||
| Finished Paradigm | 82 | 47 | 35 | |
| Stopped Early | 7 | 3 | 4 | |
| 0.12 | ||||
Note.
p < .05;
p < .01;
p < .001.
Data Analytic Plan
Empirical inquiries involving continuous dependent variables were evaluated using hierarchical linear regression. Previous research has indicated that anxiety disorders are related to startle response in adults (e.g., Grillon, 2002) and in children with a history of inhibited temperament (Reeb-Sutherland et al., 2009). However, these studies reveal that individuals with anxiety disorders show greater increases in startle reactivity from baseline to safe but did not reveal differences from baseline to threat. This fits with the idea that anxiety is a sense of insecurity or fear in the absence of frightening stimuli (Reeb-Sutherland et al., 2009). In order to attempt to isolate the unique association of mood symptoms with negative emotion (rather than broad negative affect), we first conducted all study analyses without statistically controlling for children’s anxiety symptoms. We then reran the analyses including children’s self-reported generalized anxiety symptoms as a covariate. The findings remained unchanged; we present the full models here.
Child age and sex were included as statistical covariates in the model and were entered on the first step of the equation. The second step of the equation included child-reported generalized anxiety symptoms, and the third step was comprised of child-reported mood symptoms. For analyses involving dichotomous dependent variables (crying during startle paradigm, stopping paradigm early), logistic regression analyses were used to evaluate hypotheses.
Results
Descriptive Statistics
Table 1 reports means and standard deviations for all continuous dependent variables by sex. T-tests revealed no significant sex differences in these variables. Results of a chi-square analysis revealed no statistically significant differences in behavioral responses to startle by sex (see Table 2). Table 3 reports all means and standard deviations for the behavioral, subjective, and physiological emotion variables by mood symptom group (high versus low mood symptoms based on a median split). We present these data to facilitate interpretation of descriptive statistics only, but do not utilize median splits in subsequent analyses. Preliminary analyses did not reveal an association between mood symptoms and startle during baseline, r = 0.14, p = 0.37, or safe, r = −0.15, p = 0.18, but indicated a correlation between mood symptoms and startle during threat, r = 0.31, p < .01.
Table 1.
Means (Standard Deviations) of Main Study Variables.
| Measures | Total (N =89) | Boys (n = 50) | Girls (n = 39) | Sex Differences | |
|---|---|---|---|---|---|
| df | t | ||||
| Depressive Symptoms | 5.78 (5.32) | 6.31 (5.37) | 5.08 (5.23) | 87 | 1.09 |
| Generalized Anxiety | 27.19 (6.22) | 27.54 (6.27) | 26.72(6.19) | 87 | 0.62 |
| T1 Negative Emotion | 20.53 (8.38) | 19.75 (7.57) | 21.60 (9.37) | 87 | −1.07 |
| T2 Negative Emotion | 20.59 (8.97) | 19.51 (8.06) | 22.03 (9.98) | 87 | −1.33 |
| Startle Magnitude/Baselinea | 12.11(5.66) | 13.17 (6.31) | 10.74 (4.48) | 87 | 1.47 |
| Startle Magnitude/Safea | −0.25 (0.33) | −0.22 (0.34) | −0.28 (0.31) | 87 | 0.91 |
| Startle Magnitude/Threata | 0.05 (0.28) | 0.04 (0.32) | 0.06 (0.21) | 87 | −0.44 |
Note.
p < .05;
p < .01;
p < .001.
Startle magnitude is reported in Hz units; all data were standardized using t-transformations prior to analysis and all values reflect mean responses across condition.
Table 3.
Means (Standard deviations) of Measures of Emotion by Depression Group.
| Measures | Total (N =89) | Low CDIa(n = 40) | High CDIa(n = 49) | Differences | |
|---|---|---|---|---|---|
| df | t | ||||
| Behavioral Variables: | |||||
| Number who Cried | 8 | 3 | 5 | — | — |
| Number who Stopped | 7 | 3 | 4 | — | — |
| Subjective Reports: | |||||
| T1 Negative Emotion | 20.53 (8.38) | 19.44 (6.28) | 23.37 (9.85) | 87 | −2.20* |
| T2 Negative Emotion | 20.59 (8.97) | 18.98 (7.13) | 21.86 (9.29) | 87 | −1.68 |
| Physiological Variables: | |||||
| Startle Magnitude/Baselineb | 12.11(5.66) 11.66(5.43) | 12.57 (6.08) | 87 | −0.60 | |
| Startle Magnitude/Safeb | −0.25 (0.33) | 48.09(3.49) | 47.09 (3.13) | 87 | 1.33 |
| Startle Magnitude/Threat | 0.05 (0.28) | 49.47 (2.54) | 51.23 (2.77) | 87 | −2.96** |
Note.
p < .05;
p < .01;
p < .001.
Groups derived based on a median split. Data are presented using this dichotomy for ease of inspection, but study hypotheses are addressed using continuous CDI scores.
Startle magnitude is reported in Hz units; all data were standardized using t-transformations prior to analysis and all values reflect mean responses across condition.
Mood Symptoms and Startle Magnitude During Threat
A hierarchical regression analysis was conducted to evaluate the association between child mood symptoms and startle response during threat. In order to provide a more conservative test of the hypothesis that mood symptoms are associated with greater startle potentiation during threat, we included startle magnitude during safe as a covariate. The regression revealed that after controlling for child age and sex in the first step, R2 = .08, p < .05, startle magnitude during the safe condition in the second step, ΔR2 = .27, p < .001, and child anxiety symptoms in the third step, ΔR2 = .02, p = .11, child mood symptoms added to the prediction of startle magnitude during threat, ΔR2 = .04, p < .05. Children reporting greater dysphoria evidenced increased startle response to threat cues relative to response during safety cues (see Figure 1).
Figure 1.
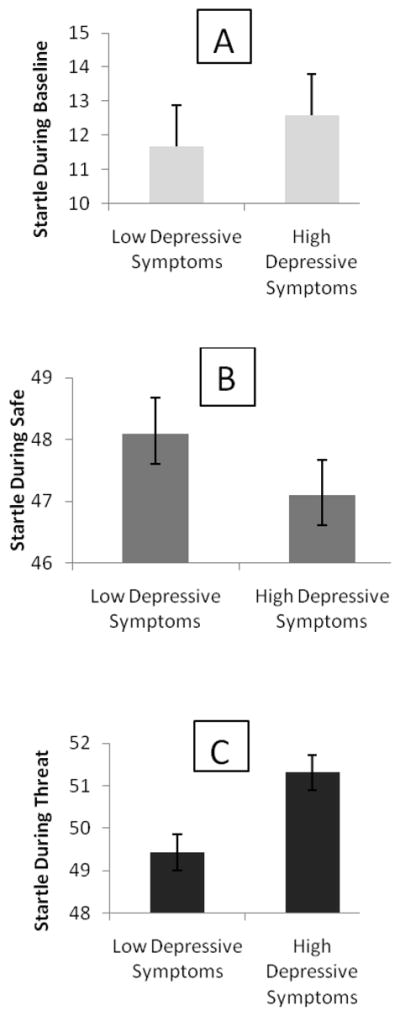
Children’s Depressive Symptoms and Their Startle Magnitude During Baseline (Panel A; N = 89), Safe (Panel B; N = 89), and Threat (Panel C; N = 89).
Note: Error bars represent standard errors. The sample was divided into the two groups (“high” and “low” depressive symptoms) using a median split. Startle data is reported in Hz units and was t-transformed prior to analysis. Values presented here reflect mean startle magnitude across condition (baseline, safe, threat).
Mood Symptoms and Changes in Negative State Emotion
A hierarchical regression analysis was conducted to evaluate the association between child mood symptoms and changes in state-level negative emotion from pre- to post-startle paradigm. The regression revealed that after controlling for child age and sex in the first step, R2 = 0.05, p = 0.12, pre-startle negative state emotion in the second step, ΔR2 = 0.76, p < .001, and child anxiety symptoms in the third step, ΔR2 = .01, p = 0.18, child mood symptoms added to the prediction of startle magnitude during threat, ΔR2 = 0.04, p < .001. Children reporting greater dysphoria showed increases in reports of negative emotion from pre- to post-startle.
Mood Symptoms and Distress-related Behavioral Response
After controlling for child sex and age, mood symptoms significantly predicted crying during the startle paradigm, Wald χ2(1, 87) = 6.59, p < .01. As mood symptoms increased, the odds of crying also increased, B = 1.17 (95% Confidence Interval = 1.04–1.32), p < .01. Similarly, after controlling for sex and age, mood symptoms significantly altered the likelihood a child would stop the startle paradigm early, χ2(1, 87) = 6.38, p < .01; as mood symptoms increased, the odds of stopping the paradigm early also increased, B = 1.19 (95% Confidence Interval = 1.04 – 1.36), p < .01.
Discussion
Despite considerable advances in affective science, much remains to be learned about the link between depression and emotional experience, especially in children. The ECI and NP models are contradictory and have yet to be studied in children. In a nonclinical sample of school-aged children, we found that greater dysphoria was associated with signs of greater negative emotional experience, as manifested in terms of larger startle magnitude during threat, greater increases in self-reported negative emotion, and greater likelihood of exhibiting behavioral markers of distress (stopping the paradigm early and crying). The findings remained after controlling for children’s self-reported generalized anxiety symptoms. The results provide preliminary support for the NP model, which states that depression is related to potentiated negative emotional reactions.
Mood Symptoms and Startle Magnitude During Threat
The threat paradigm employed here enabled us to measure children’s modulation of startle response to environmental cues (“safety” versus “threat”), which arguably is one of the most important aspects of emotion reactivity (Keltner & Gross, 1999), and one that according to the ECI model, ought to be impaired in depression (Rottenberg et al., 2005). Although researchers have examined emotional reactions to threat for their association with anxiety (e.g., Grillon et al., 1994), little research has examined this for its association with mood symptoms. However, given the high comorbidity between anxiety and depression (e.g., Anderson et al., 1987), in order to fully understand the emotional responding of dysphoric individuals, it is important to examine reactions to threat. In contrast to research findings on affect-modulated startle in nonclinical adults (Mneimne et al., 2008), we found that mood symptoms were associated with greater negative psychophysiological signs of emotion in children, or with a greater increase in startle magnitude from “safety” to “threat.” Rather than showing less sensitivity to the threat cue, as the ECI model would predict, children with greater mood symptoms showed greater reactivity than children with fewer mood symptoms, which is consistent with the NP model. Further, unlike previous research with adults (Dichter et al., 2004; Iacono et al., 1984), the results of this study fail to support the trait perspective of ECI insofar as ECI is not concurrently associated with greater mood symptoms among children. Future research should examine whether ECI in this paradigm predicts subsequent depressive episodes among children.
Mood Symptoms and Subjective and Behavioral Indices of Negative Emotion
In addition to these startle effects, children with greater mood symptoms reported greater increases in subjective negative emotion and showed greater signs of behavioral distress. Importantly, and unlike many multimethod investigations of emotion (e.g., Kring & Neale, 1996; Mauss & Robinson, 2009), evidence of greater negative emotional experience is apparent across multiple domains of measurement. This increases confidence in the belief that children with greater mood symptoms experience greater levels of negative emotion in response to the startle paradigm. It is possible that the reason for the consistency across domains of measurement is because children, whose emotion regulation skills are less well honed, may be less skilled in masking their distress to the outside world than adults or may have a lesser understanding of display rules (Garrett-Peters & Fox, 2007; Gnepp & Hess, 1986; Saarni, 1979, 1984; Underwood, Coie, & Herbsman, 1992; Zeman & Garber, 1996), and, therefore, may show greater congruence of emotional experience and expression.
Limitations
It is important to interpret the findings of this study in the context of its limitations. We conceive of this study as a first step in identifying whether emotional response to threat may be a risk factor for the development of depression, and we accomplished this by using a cross-sectional, correlational study, which means that the results cannot speak to the temporal association between emotion and mood symptoms. Future research should examine these associations using a prospective design in order to further evaluate if emotional response profiles are related to risk for the future development of depressive disorders in children and adolescents. Further, these hypotheses were examined among a normative sample of children as a function of mood symptoms as opposed to a diagnosis of major depressive disorder. The mean level of mood symptoms in the sample was low, and even the children endorsing many symptoms of depression could be better classified as dysphoric than depressed. Although we attempted to isolate the association between wmood symptoms and emotional response by first statistically controlling for children’s reports of generalized anxiety symptoms, it is possible that response on the CDI better reflects broad negative affect than depressive symptoms per se. Following Rottenberg and colleagues (2005), the best examination of this hypothesis is to measure ECI within a clinical sample depressed children using stimuli with person-specific themes. Therefore, a better test of these hypotheses would involve examining response to fear-potentiated startle in a clinical sample, or in a community sample with greater mood symptoms. Finally, according to the ECI, depressed individuals exhibit attenuated responses to both negative and positive stimuli (Rottenberg et al., 2005), whereas this study only evaluated children’s responses to negative stimuli. A more complete evaluation of the link between depression and emotion will assess children’s reactions to both negative and positive stimuli.
Implications for Research, Policy, and Practice
Within the context of these limitations, this study contributes to the literature on depression and emotion in childhood (Durbin & Shafir, 2008). Use of a multimethod approach enabled us to study various manifestations of emotional experience. The results from different modalities were convergent, indicating that children with greater mood symptoms experience more intense negative emotion during a threatening task. In the context of this paradigm, greater mood symptoms are related to increased context sensitivity and greater reactivity.
How do we understand these findings in light of theory and data in support of the ECI model among adults? On one hand, the lack of support for context insensitivity could be evidence of developmental differences in the link between mood symptoms and emotion. It is well-known that children’s mood symptoms manifest differently than adults’ (American Psychiatric Association, 2000), and it may be that ECI is a feature of depression specific to the manifestation of the disorder in adults. Specifically, children with depression are more likely to experience and express their symptoms as irritability and somatic complaints, and are less likely to have symptoms of motor retardation, hypersomnia, and anhedonia (American Psychiatric Association, 2000). Context insensitivity may have its origins in a sense of numbing known to be attendant to depression in adults (Healy, 1993), but depressed children may not experience this sense of numbing, making it unlikely that they would show signs of ECI. Given that this investigation focused on late middle childhood, however, it will be important for future research to examine these questions in younger children and in adolescents. For example, given the changes in phenomenology of depression that occur from childhood to adulthood (APA, 2000; Healy, 1993), it would be interesting to evaluate if depression is linked to NP in childhood and to ECI from adolescence onward.
On the other hand, perhaps context insensitivity develops only after an individual has experienced elevated depressive symptoms for a prolonged period of time, making it unlikely that mood symptoms in children, or in a non-clinical sample, would be associated with ECI. In addition, based on the fact that different studies have shown inconsistencies across measurements of ECI in the behavioral, subjective, and physiological domains (Gehricke & Shapiro, 2000; Rottenberg et al., 2002b), researchers typically recommend assessing ECI across domains and by using person-specific or idiographic stimuli (Rottenberg et al., 2005). Although in the current study we incorporated multi-domain assessments, the stimulus employed to evaluate ECI was not person-specific or idiographic. Further, the fear-potentiated startle paradigm tapped children’s emotional reactions to threat, or to the anticipation of an aversive stimulus, which arguably may be produce different results than the paradigm that has been used with adults (e.g., Mneime et al., 2008), which involves examining the modulation of startle response by affective pictures. It is quite likely that individuals’ emotional reactions to threat differ from their reactions to negative, but non-threatening, stimuli, and this difference in procedure used in the study may account for the discrepant findings. Therefore, future research with adults should also examine startle response in the fear-potentiated startle paradigm (Grillon et al., 1999) for its association with depression and dysphoria. Finally, it is possible that the context insensitivity observed in both adult clinical populations and adults with greater levels of depressive symptoms is only evident among children with clinically-significant levels of mood symptoms. Future research should evaluate whether the reactions observed in the current study pertain to negative, but non-threat-oriented, stimuli, as well as to children with clinical depression.
Beyond informing the understanding of ECI and NP models in children, findings from the present study also provide valuable new evidence on the link between mood symptoms and negative emotional experience in school-aged children, an area deserving of further inquiry (Durbin & Shafir, 2008; Cole et al., 2008; Kovacs et al., 2008). Converging evidence from multiple modes of assessment suggests that children with greater mood symptoms experience greater negative emotion reactivity when exposed to threat. Based on research documenting increased startle reactivity among children of depressed parents, Grillon and colleagues (2005) suggested that increased startle during threat may constitute a risk factor for the development of depression. The data from this study provide further support for this hypothesis. Specifically, children’s current levels of mood symptoms are positively associated with greater startle reactivity to threat, and greater subjective and behavioral signs of distress. Identifying potential risk factors for the development of depression may be particularly important during middle childhood and preadolescence due to the marked increases in prevalence rates during adolescence (Hankin et al., 1998). Although significant research has examined social cognitive risk factors for the development of depression in this age group (Abela, 2001; Joiner & Wagner, 1995), future research should examine deficits in emotion reactivity and regulation as potential risk factors leading to the development of depression (Kovacs et al., 2008).
An emerging body of research has examined the role of youths’ peer relationships in contributing to the development of and maintaining depression, with findings generally suggesting that depressed adolescents’ peer relationships suffer as a consequence of their depressive symptoms (Borelli & Prinstein, 2006; Prinstein, Borelli, Cheah, Simon, & Aikins, 2005; Stevens & Prinstein, 2005; Stice, Ragan, & Randall, 2004). Researchers have implicated various interpersonal behaviors (e.g., excessive feedback seeking, negative feedback seeking) as potential causes of this deterioration in relationship quality. However, it is also possible that children with depressive symptoms alienate peers based on displays of negative emotion. Our findings suggest that children with greater depressive symptoms were more likely to cry and stop the task prematurely, behaviors which, if replicated among peers, might lead to alienation from the broader social group and/or deterioration in friendship quality, known risk factors for the development and worsening of depression in adolescents (Boivin & Hymel, 1997). Future research ought to examine the interpersonal consequences of negative emotionality among children with greater depressive symptoms, as it is easy to imagine that peer rejection or deterioration in friendship quality could interact with initial reactivity and depressive symptoms to precipitate a depressive episode.
Finally, future research should address what remains unknown about the proximal causes of negative emotion reactivity among children with greater mood symptoms in this sample. Specifically, what caused the children to react with more negativity to the threat paradigm? Were they more fearful to begin with, and the cues of threat just exacerbated this fearful state? Were they making negative attributions about the threat cues during the paradigm, which resulted in exacerbations in negative emotional state? In line with a learned helplessness model of depression (Seligman, 1975; Seligman & Maier, 1967), did they feel more out of control than other children, and did these feelings exacerbate their initial emotional reactions to the stimuli?2 It would be interesting to identify whether depressed children are less likely to use emotion regulation strategies during difficult tasks, or whether they are as likely to use emotion regulation strategies but are less successful in their attempts to regulate.
Acknowledgments
This research was supported by grants from National Science Foundation, the Center for Mental Health Promotion, and by NIH Grant 1-F32AG032310-01 awarded to the first author. Special thanks are due to Daryn David, Nicki Hunter, and Eric Langlois for their assistance with the project. Finally, thanks are due to all of the children and families who participated in this study.
Footnotes
Although we have characterized the threat presented in the fear-potentiated startle paradigm as being non-social, for some children it may actually present a social threat. For example, after hearing the instructions for the paradigm, one male participant responded, “I don’t believe you you’re going to puff me when the safe guy is on the screen.” Despite multiple reassurances from the experimenter, this child persisted in his assertion that the experimenter was going to trick him.
Anecodotal observations of the experimenter indicated that several of the children used active emotion regulation strategies throughout the startle task, such as talking aloud throughout the task, (e.g., “Oh, it’s the safe guy. No puff of air for this one”; “Here’s the threat one the puff wasn’t very scary last time, though.”), counting the number of puffs they received, or using deep breathing during the task. The children were not given any instructions about using techniques during the paradigm, so any reliance on emotion regulation techniques was self-motivated.
References
- Abela JRZ. The hopelessness theory of depression: A test of the diathesis-stress and causal mediation components in third and seventh grade children. Journal of Abnormal Child Psychology. 2001;29:241–254. doi: 10.1023/a:1010333815728. [DOI] [PubMed] [Google Scholar]
- Allen NB, Trinder J, Brennen C. Affective startle modulation in clinical depression: Preliminary findings. Biological Psychiatry. 1999;46:542–550. doi: 10.1016/s0006-3223(99)00025-6. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- Anderson JC, Williams S, McGee R, Silva PA. DSM-III disorders in preadolescent children. Archives of General Psychiatry. 1987;44:69–76. doi: 10.1001/archpsyc.1987.01800130081010. [DOI] [PubMed] [Google Scholar]
- Ayduk O, Downey G, Kim M. Rejection sensitivity and depressive symptoms in women. Personality and Social Psychology Bulletin. 2001;27:868–877. [Google Scholar]
- Barlow DH. Disorders of emotion. Psychological Inquiry. 1988;2:58–71. [Google Scholar]
- Beatty J. Task-evoked pupillary responses processing load and the structure of processing resources. Psychological Bulletin. 1982;91:276–292. [PubMed] [Google Scholar]
- Boivin M, Hymel S. Peer experiences and social perceptions: A sequential model. Developmental Psychology. 1997;33:135–145. doi: 10.1037//0012-1649.33.1.135. [DOI] [PubMed] [Google Scholar]
- Borelli JL, Crowley MJ, David DH, Sbarra DA, Anderson GM, Mayes LC. Attachment and emotion in school-aged children. Emotion. doi: 10.1037/a0018490. in press. [DOI] [PubMed] [Google Scholar]
- Borelli JL, Prinstein MJ. Rejection Sensitivity and Internalizing Distress among Adolescents; Poster presented at the Association for the Advancement of Behavior Therapy; Boston. Nov. 20–23.2003. [Google Scholar]
- Borelli JL, Prinstein MJ. Reciprocal, Longitudinal Associations Among Adolescents’ Negative Feedback-Seeking, Depressive Symptoms, and Peer Relations. Journal of Abnormal Child Psychology. 32:159–169. doi: 10.1007/s10802-005-9010-y. [DOI] [PubMed] [Google Scholar]
- Bradley MM. Emotion and motivation. In: Cacioppo JT, Tassinary LG, Bernston GG, editors. Handbook of Psychophysiology. New York: Cambridge University Press; 2000. pp. 602–642. [Google Scholar]
- Bradley MM, Cuthbert B, Lang PJ. Startle reflex modification: Attention or emotion? Psychophysiology. 1990;27:513–522. doi: 10.1111/j.1469-8986.1990.tb01966.x. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Campeau S, Davis M. Fear potentiation of the acoustic startle reflex using noises of various spectral frequencies as conditioned stimuli. Animal Learning & Behavior. 1992;20:177–186. [Google Scholar]
- Chorpita BF, Tracey SA, Brown TA, Collica TJ, Barlow DH. Assessment of worry in children and adolescents: An Adaptation of the Penn State Worry Questionnaire. Behaviour Research & Therapy. 1997;35:569–581. doi: 10.1016/s0005-7967(96)00116-7. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103:103–116. [PubMed] [Google Scholar]
- Cole PM, Luby J, Sullivan MW. Emotions and the development of childhood depression: Bridging the gap. Child Development Perspectives. 2008;2:141–148. doi: 10.1111/j.1750-8606.2008.00056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis M, Falls WA, Campeau S, Kim M. Fear-potentiated startle: A neural and pharmacological analysis. Behavioural Brain Research. 1993;58:175–198. doi: 10.1016/0166-4328(93)90102-v. [DOI] [PubMed] [Google Scholar]
- Deldin PJ, Keller J, Gergen JA, Miller GA. Cognitive bias and emotion in neuropsychological models of depression. Cognition &Emotion. 2001;15:787–802. [Google Scholar]
- Dichter GS, Tomarken AJ, Shelton RC, Sutton S. Early and late-onset startle modulation in unipolar depression. Psychophysiology. 2004;41:433–440. doi: 10.1111/j.1469-8986.00162.x. [DOI] [PubMed] [Google Scholar]
- Downey G, Lebolt A, Rincon C, Freitas AL. Rejection sensitivity and children’s interpersonal difficulties. Child Development. 1998;69:1074–1091. [PubMed] [Google Scholar]
- Durbin CE, Shafir DM. Emotion regulation and risk for depression. In: Abela JRZ, Hankin BL, editors. Handbook of depression in children and adolescents. New York, NY: Guilford; 2008. pp. 149–176. [Google Scholar]
- Ehrenreich JT, Goldstein CR, Wright LR, Barlow DH. Development of a unified protocol for the treatment of emotional disorders in youth. Child & Family Behavior Therapy. 2009;31:20–37. doi: 10.1080/07317100802701228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher S, Mayes LC. Computerized assessment and presentation engine. (Version 3.0) [Computer software] New Haven, CT: Yale University; 2001. [Google Scholar]
- Garrett-Peters PT, Fox NA. Cross-cultural differences in children’s emotional reactions to a disappointing situation. International Journal of Behavioral Development. 2007;31:161–169. [Google Scholar]
- Gehricke JG, Shapiro D. Reduced facial expression and social context in major depression: Discrepancies between facial muscle activity and self-reported emotion. Psychiatry Research. 2000;95:157–167. doi: 10.1016/s0165-1781(00)00168-2. [DOI] [PubMed] [Google Scholar]
- Gnepp J, Hess DL. Children’s understanding of verbal and facial display rules. Developmental Psychology. 1986;22:103–108. [Google Scholar]
- Golin S, Hartman SA, Klatt EN, Munz K, Wolfgang GL. Effects of self-esteem manipulation on arousal and reactions to sad models in depressed and nondepressed college students. Journal of Abnormal Psychology. 1977;86:435–439. doi: 10.1037//0021-843x.86.4.435. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Sivers H, Canli T, Kasch KL, Gabrieli JDE. Neural activation in depression in response to emotional stimuli. In: Gotlib IH Chair, editor. New directions in the neurobiology of affective disorders; Symposium presented at the Annual Meeting of the Society for Research in Psychopathology; Madison, WI. 2001. Nov, [Google Scholar]
- Greden JF, Genero N, Price HL, Feinberg M, Levine S. Facial electromyography in depression. Archives of General Psychiatry. 1986;43:269–274. doi: 10.1001/archpsyc.1986.01800030087009. [DOI] [PubMed] [Google Scholar]
- Grillon C, Ameli R, Foot M, Davis M. Fear-potentiated startle: Relationship to the level of state/trait anxiety in healthy subjects. Biological Psychiatry. 1993;33:566–574. doi: 10.1016/0006-3223(93)90094-t. [DOI] [PubMed] [Google Scholar]
- Grillon C, Ameli R, Goddard A, Woods SW, Davis M. Baseline and fear-potentiated startle in panic disorder patients. Biological Psychiatry. 1994;35:431–439. doi: 10.1016/0006-3223(94)90040-x. [DOI] [PubMed] [Google Scholar]
- Grillon C, Dierker L, Merikangas KR. Fear-potentiated startle in adolescent offspring of parents with anxiety disorders. Biological Psychiatry. 1998;44:990–997. doi: 10.1016/s0006-3223(98)00188-7. [DOI] [PubMed] [Google Scholar]
- Grillon C, Merikangas KR, Dierker L, Snidman N, Arriaga RI, Kagan J, Donzella B, Dikel T, Nelson C. Startle potentiation by threat of aversive stimuli and darkness in adolescents: A multi-site study. International Journal of Psychophysiology. 1999;32:63–73. doi: 10.1016/s0167-8760(99)00002-1. [DOI] [PubMed] [Google Scholar]
- Grillon C, Morgan CA., III Fear-potentiated startle conditioning to explicit and contextual cues in Gulf War veterans with posttraumatic stress disorder. Journal of Abnormal Psychology. 1999;108:134–142. doi: 10.1037//0021-843x.108.1.134. [DOI] [PubMed] [Google Scholar]
- Grillon C, Warner V, Hille J, Merikangas KR, Bruder GE, Tenke CE, Nomura Y, Leite P, Weissman MM. Families at high and low risk for depression: A three-generation startle study. Biological Psychiatry. 2005;57:953–960. doi: 10.1016/j.biopsych.2005.01.045. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Munoz RF. Emotion regulation and mental health. Clinical Psychology: Science and Practice. 1995;2:151–164. [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: An elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin. 2001;127:773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, Mcgee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;10:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Healy D. Dysphoria. In: Costello CG, editor. Symptoms of depression. NewYork: Wiley; 1993. pp. 23–42. [Google Scholar]
- Iacono WG, Lykken DT, Haroian KP, Peloquin LH, Valentine RH, Tuason VB. Electrodermal activity in euthymic patients with affective disorders: One-year retest stability and the effects of stimulus intensity and significance. Journal of Abnormal Psychology. 1984;93:304–311. doi: 10.1037//0021-843x.93.3.304. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Wagner KD. Attribution style and depression in children and adolescents: A meta-analytic review. Clinical Psychology Review. 1995;15:777–798. [Google Scholar]
- Kaviani H, Gray JA, Checkley SA, Raven PW, Wilson GD, Kumari V. Affective modulation of the startle response in depression: influence of the severity of depression, anhedonia, and anxiety. Journal of Affective Disorders. 2004;83:21–31. doi: 10.1016/j.jad.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Keltner D, Gross JJ. Functional accounts of emotions. Cognition and Emotion. 1999;13:467–480. [Google Scholar]
- Kovacs M. Children’s Depression Inventory Manual. Los Angeles: Western Psychological Services; 1992. [Google Scholar]
- Kovacs M, Joormann J, Gotlib IH. Emotion (dys)regulation and links to depressive disorders. Child Development Perspectives. 2008;2:149–155. doi: 10.1111/j.1750-8606.2008.00057.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM, Neale JM. Do schizophrenic patients show a disjunctive relationship among expressive, experiential, and psychophysiological components of emotion? Journal of Abnormal Psychology. 1996;105:249–257. doi: 10.1037//0021-843x.105.2.249. [DOI] [PubMed] [Google Scholar]
- Lang PJ, Greenwald MK, Bradley MM, Hamm AO. Looking at pictures: Affective, facial, visceral, and behavioral reactions. Psychophysiology. 1993;30:261–273. doi: 10.1111/j.1469-8986.1993.tb03352.x. [DOI] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, Joiner TE, Jr, Rudolph KD, Potter KI, Lambert S, Osborne L, Gathright T. A measure of positive and negative affect for children: Scale development and preliminary validation. Psychological Assessment. 1999;11:326–338. [Google Scholar]
- Lee Y, Davis M. Role of the Hippocampus, the Bed Nucleus of the Stria Terminalis, and the Amygdala in the Excitatory Effect of Corticotropin-Releasing Hormone on the Acoustic Startle Reflex. The Journal of Neuroscience. 1997;17:6434–6446. doi: 10.1523/JNEUROSCI.17-16-06434.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Lobitz WC, Wilson S. Sensitivity” of depressed individuals to aversive stimuli. Journal of Abnormal Psychology. 1973;81:259–263. doi: 10.1037/h0034529. [DOI] [PubMed] [Google Scholar]
- Lissek S, Orme K, McDowell DJ, Johnson LL, Luckenbaugh DA, Baas JM, et al. Emotion regulation and potentiated startle across affective picture and threat-of-shock paradigms. Biological Psychology. 2007;76:124–133. doi: 10.1016/j.biopsycho.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauss IB, Robinson MD. Measures of emotion: A review. Cognition and Emotion. 2009;23:209–237. doi: 10.1080/02699930802204677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayberg HS, Liotti M, Brannan SK, McGinnis S, Mahurin RK, Jerabek PA, et al. Reciprocal limbic cortical function and negative mood: Converging PET findings in depression and normal sadness. American Journal of Psychiatry. 1999;156:675–682. doi: 10.1176/ajp.156.5.675. [DOI] [PubMed] [Google Scholar]
- Mneimne M, McDermut W, Powers AS. Affective ratings and startle modulation in people with nonclinical depression. Emotion. 2008;8:552–559. doi: 10.1037/a0012827. [DOI] [PubMed] [Google Scholar]
- Moses EB, Barlow DH. A new unified treatment approach for emotional disorders based on emotion science. Current Directions in Psychological Science. 2006;15:146–150. [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological Bulletin. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Borelli JL, Cheah CSL, Simon VA, Aikins JW. Adolescent girls’ interpersonal vulnerability to depressive symptoms: A longitudinal examination of reassurance-seeking and peer relationships. Journal of Abnormal Psychology. 2005;114:676–688. doi: 10.1037/0021-843X.114.4.676. [DOI] [PubMed] [Google Scholar]
- Reeb-Sutherland BC, Helfinstein SM, Degnan KA, Perez -Edgar K, Henderson HA, Lissek S, Chronis-Tuscano A, Grillon C, Pine DS, Fox NA. Startle response in behaviorally inhibited adolescents with a lifetime occurrence of anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48:610–617. doi: 10.1097/CHI.0b013e31819f70fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberson-Nay R, McClure EB, Monk CS, Nelson EE, Guyer AE, Fromm SJ, Charney DS, Leibenluft E, Blair J, Ernst M, Pine DS. Increased amygdala activity during successful memory encoding in adolescent major depressive disorder: an fMRI study. Biological Psychiatry. 2006;60:966–973. doi: 10.1016/j.biopsych.2006.02.018. [DOI] [PubMed] [Google Scholar]
- Rottenberg J, Gotlib IH. Socioemotional functioning in depression. In: Power M, editor. Mood disorders: A handbook of science and practice. New York: Wiley; 2004. pp. 61–77. [Google Scholar]
- Rottenberg J, Gross JJ. When emotion goes wrong: Realizing the promise of affective science. Clinical Psychology: Science and Practice. 2003;10:227–232. [Google Scholar]
- Rottenberg J, Gross JJ, Gotlib IH. Emotion context insensitivity in major depressive disorder. Journal of Abnormal Child Psychology. 2005;114:627–639. doi: 10.1037/0021-843X.114.4.627. [DOI] [PubMed] [Google Scholar]
- Rottenberg J, Gross JJ, Wilhelm FH, Najmi S, Gotlib IH. Crying threshold and intensity in major depressive disorder. Journal of Abnormal Psychology. 2002;111:302–312. [PubMed] [Google Scholar]
- Rottenberg J, Kasch KL, Gross JJ, Gotlib IH. Sadness and amusement reactivity differentially predict concurrent and prospective functioning in major depressive disorder. Emotion. 2002;2:135–146. doi: 10.1037/1528-3542.2.2.135. [DOI] [PubMed] [Google Scholar]
- Saarni C. Children’s understanding of display rules for expressive behavior. Child Development. 1979;15:424–429. [Google Scholar]
- Saarni C. An observational study of children’s attempts to monitor their expressive behavior. Child Development. 1984;55:1504–1513. [Google Scholar]
- Saylor CF, Finch AJ, Spirito A, Bennett B. The Children’s Depression Inventory: A systematic evaluation of psychometric properties. Journal of Consulting & Clinical Psychology. 1984;52:955–967. doi: 10.1037//0022-006x.52.6.955. [DOI] [PubMed] [Google Scholar]
- Seligman M. Helplessness: On depression, development and death. San Francisco: Freeman; 1975. [Google Scholar]
- Seligman MEP, Maier SF. Failure to escape traumatic shock. Journal of Experimental Psychology. 1967;74:1–9. doi: 10.1037/h0024514. [DOI] [PubMed] [Google Scholar]
- Siegle GJ, Steinhauer SR, Carter CS, Ramel W, Thase ME. Do the seconds turn into hours? Relationships between sustained pupil dilation in response to emotional information and self-reported rumination. Cognitive Therapy and Research. 2003;27:365–382. [Google Scholar]
- Siegle GJ, Steinhauer SR, Thase ME, Stenger VA, Carter CS. Can’t shake that feeling: fMRI assessment of sustained amygdala activity in response to emotional information in depressed individuals. Biological Psychiatry. 2002;51:693–707. doi: 10.1016/s0006-3223(02)01314-8. [DOI] [PubMed] [Google Scholar]
- Sigmon ST, Nelson-Gray RO. Sensitivity to aversive events in depression: Antecedent, concomitant, or consequent? Journal of Psychopathology and Behavioral Assessment. 1992;14:225–246. [Google Scholar]
- Stevens EA, Prinstein MJ. Peer contagion of depressogenic attributional styles among adolescents: A longitudinal study. Journal of Abnormal Child Psychology. 2005;33:25–37. doi: 10.1007/s10802-005-0931-2. [DOI] [PubMed] [Google Scholar]
- Stice E, Ragan J, Randall P. Prospective relations between social support and depression: Differential direction of effects for parent and peer support? Journal of Abnormal Psychology. 2004;113:155–159. doi: 10.1037/0021-843X.113.1.155. [DOI] [PubMed] [Google Scholar]
- Thomas KM, Drevets WC, Dahl RE, Ryan ND, Birmaher B, Eccard CH, et al. Amygdala response to fearful faces in anxious and depressed children. Archives of General Psychiatry. 2001;58:1057–1063. doi: 10.1001/archpsyc.58.11.1057. [DOI] [PubMed] [Google Scholar]
- Underwood MK, Coie JD, Herbsman CR. Display rules for anger and aggression in school-age children. Child Development. 1992;63:366–380. [PubMed] [Google Scholar]
- Zeman J, Garber J. Display rules for anger, sadness, and pain: It depends on who is watching. Child Development. 1996;67:957–973. [PubMed] [Google Scholar]


