Abstract
Objective
To assess the impact of a change from nurse to pharmacist instructors and a new curriculum intended to encourage students’ use of physical assessment skills.
Design
Pharmacist faculty members redesigned the physical assessment curriculum to focus on those assessment skills most likely to be performed by practicing pharmacists. The 5 focus areas were general assessment skills, gastrointestinal system, pulmonary system, central and peripheral nervous system, and cardiovascular system. Instructional methods used included prelaboratory assignments, brief introductory lectures, demonstration of assessment techniques, application of techniques with a laboratory partner, and demonstration of competence using a mannequin.
Assessment
A 16-item survey instrument was administered to determine students’ perceptions of the revised curriculum. Students who received instruction from pharmacist faculty members used their physical assessment skills more, especially during advanced pharmacy practice experiences (APPEs), than students who received instruction from nurse faculty members. Students instructed by pharmacist faculty members also felt more comfortable with their skills and rated the instruction as more practical.
Conclusion
A redesigned curriculum and pharmacist-led instruction resulted in improved pharmacy student comfort with and use of physical assessment skills.
Keywords: physical assessment, curriculum, pharmacist, nurse
INTRODUCTION
Physical assessment skills are necessary for health professionals to conduct complete and accurate patient evaluations. The information they are able to obtain is directly related to the type and quality of care they can provide. Traditionally, patient physical assessment has been performed by physicians, nurses, or physician assistants. However, as pharmacy services have become more directly related to patient outcomes, pharmacists have become more involved in conducting patient physical assessment.1,2
Jones defines patient assessment by pharmacists as the process by which information is gathered from the patient and other sources and evaluated in order to make decisions regarding: “(1) the health status of the patient; (2) drug therapy needs and problems; (3) interventions that will resolve identified drug problems and prevent future problems; and (4) follow-up to ensure that patient outcomes are being met.”3 To ensure pharmacy students receive instruction in such skills, the Accreditation Council for Pharmacy Education (ACPE) standards require that curriculums include a patient assessment laboratory addressing physical assessment techniques.4 Also, the educational outcomes of the Pharmacy Practice Supplement to the 2004 Center for the Advancement of Pharmaceutical Education (CAPE) call for students to be able to perform and evaluate aspects of patient physical assessment.5
Although instruction in physical assessment is required in colleges and schools of pharmacy, a 1995 survey of 55 colleges of pharmacy found that 29% of these courses were under the direction of physicians and/or physician assistants, and most used a combination of pharmacists, physicians, and/or nurses as instructors.6 A 2005 survey showed that more than two-thirds of programs continue to use physicians, nurses, and physician assistants as physical assessment instructors rather than pharmacist faculty members.7 Nurses also have been used to provide physical assessment instruction during advanced pharmacy practice experiences (APPE).8 Not all pharmacist faculty members are qualified to teach physical assessment skills.9 Two surveys of colleges of pharmacy found that the minority of pharmacist faculty members who did teach physical assessment had received formal training.6,7
Since 1996, students in the Nesbitt College of Pharmacy and Nursing at Wilkes University had received their physical assessment instruction from nurse faculty members. Students were instructed in traditional assessment techniques on several organ systems that medical or nursing students would be expected to perform. However, feedback from students and APPE preceptors indicated that pharmacy students were not being taught or encouraged to use physical assessment skills. Many of the assessment skills they were taught were not practical for a practicing pharmacist, and those that were, such as assessment of blood pressure and pulse, were not emphasized. Pharmacist faculty members felt this was directly related to the objectives and skills emphasized by nurse faculty members and decided that if they were directly involved in physical assessment instruction, they could draw on their pharmacy practice experience to bring relevance and practicality to the objectives and skills emphasized.
Although other authors have described efforts to redesign patient assessment instruction for pharmacy students,10 we are unaware of any report that describes a change from all nurse to all pharmacist instruction. The purpose of this report is to describe and evaluate our efforts in changing from nurse to pharmacist instruction of physical assessment. The goals of this curricular change were to emphasize and reinforce the practical physical assessment skills expected of practicing pharmacists who have direct patient contact. We hypothesized that by doing this students would use their physical assessment skills more frequently in practice settings.
DESIGN
Pharmacist faculty members assumed responsibility for providing patient physical assessment instruction to pharmacy students in fall 2006 and decided that physical assessment instruction would remain part of the Pharmacy Care Laboratory series. Pharmacy Care Laboratory is a 4-semester laboratory series that emphasizes the practical application of knowledge and skills gained in other portions of the curriculum to patient care scenarios. The series begins in the spring semester of the first year and occurs each semester thereafter, with the exception of the second-year spring semester. Each pharmacy class of 70 students is divided into 3 sections and students attend a 3-hour laboratory once weekly throughout the semester with the members of their section. Some of the skills emphasized throughout the course include patient counseling, pharmacokinetic assessment and pharmaceutical calculations, drug information, communication, critical thinking, literature evaluation, and patient assessment, including physical assessment. When taught by nurse faculty members, physical assessment instruction had been provided as part of the Pharmacy Care Laboratory course during the last 6 weeks of the fall semester in the second year. Pharmacist faculty members agreed that this was the most appropriate point in the curriculum to provide physical assessment instruction because of the skills-based emphasis of the course, but chose to teach the physical assessment portion during the first 6 weeks of the semester.
The 5 pharmacist faculty members who served as instructors for the physical assessment series were chosen based on their knowledge and experience using physical assessment skills and willingness to participate. One had completed a physical assessment certification program, but the others did not have any special certifications or qualifications in patient physical assessment. During initial redesign of the content for the physical assessment portion of the curriculum, the pharmacist faculty members met to develop general curricular outcomes, objectives, and necessary topics. The learning objectives that were established emphasized the application of practical physical assessment skills that were likely to be performed by pharmacists in various practice settings. The curricular outcome established was an increase in student use of their physical assessment skills in patient care settings.
Instruction by nurse faculty members had focused on the following areas: chest and pulmonary system, abdominal examination, cardiovascular system, neurological system, skin, and musculoskeletal system. The focus in the first 5 weeks was in these areas, with a practical examination given in the sixth week. Some of the physical assessment skills emphasized for the cardiovascular system during nurse instruction had included the auscultation of carotid bruits, valvular murmurs, and the S3 and S4 heart sounds, whereas assessment of blood pressure had not been a major focus. Similarly, nurse instruction in physical assessment of the neurological system did not review performance of the monofilament test, but did focus on assessment of several reflexes and all the cranial nerves. These were some of the skills that the students had considered impractical to pharmacy practice.
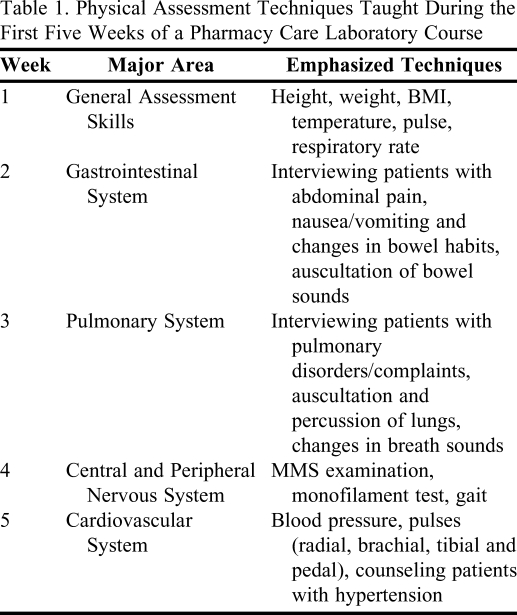
To meet our curricular objectives, the pharmacist faculty members focused instead on physical assessment skills in 5 major areas that they felt were the most practical for a pharmacist with direct patient contact: general assessment skills, gastrointestinal system, pulmonary system, central and peripheral nervous system, and cardiovascular system (Table 1). Each week students received instruction in these 5 areas and were taught to apply assessment techniques from the 5 different areas beginning with general assessment skills. The specific techniques emphasized in the 5 areas are provided in Table 1. These techniques were chosen because they were felt to be the most practical that a pharmacist with direct patient contact should be able to perform. The sixth week of the laboratory series consisted of a laboratory practical in which students had to demonstrate competence in techniques learned in the laboratory series. The assessed techniques included taking a patient's body temperature, questioning patients about common gastrointestinal and pulmonary complaints, performing a monofilament test, and taking a patient's blood pressure. Nurse faculty members had assessed similar techniques in the practical examination, including determining a patient's temperature, pulse, respiratory rate, and blood pressure, and performing a physical assessment of a randomly selected organ system.
Table 1.
Physical Assessment Techniques Taught During the First Five Weeks of a Pharmacy Care Laboratory Course
Abbreviations: BMI = body mass index; MMS = Mini Mental Status
To accomplish the curricular outcome, we incorporated mostly skills-based learning and assessment into the 5 weeks of the laboratory series. As an example, instruction in the assessment of blood pressure included a prelaboratory assignment, a brief introductory lecture, demonstration of the assessment technique, application of the technique with a laboratory partner, and demonstration of competence in the technique using a simulation mannequin. All of the laboratories used a similar combination of these instructional methods beginning with a prelaboratory assignment that counted as credit towards the overall/final laboratory grade and had to be turned in at the beginning of the laboratory. This usually involved a reading assignment from Patient Assessment in Pharmacy Practice,11 the required text for the series. The laboratories often incorporated a brief (usually no longer then 30 minutes) introductory lecture at the beginning of the laboratory to familiarize students with various terminology, applicable disease state information, and assessment techniques. Students were divided into smaller groups or pairs during the laboratory to practice the assessment techniques. The majority of laboratory time was devoted to similar methods of active learning. Finally, students’ competence in the techniques was assessed either by their peers or the instructor. Many of the instructors also used a full-size auscultation simulation mannequin to facilitate active learning and for demonstration of student competence with some of the assessment techniques. This study was granted exempt status by the university's Human Subjects Review Committee.
EVALUATION AND ASSESSMENT
A survey was conducted to determine curricular outcomes for the physical assessment instruction. The survey instrument was administered first in October 2007 to students of the class of 2008, who had received their physical assessment instruction from nurse faculty members. Pharmacist faculty members chose instead to survey students in the class of 2009 and 2010 at the end of their fourth year, during their final APPE, in order to gather data regarding use of physical assessment skills up to and during their APPEs. An invitation to complete the 16-item, anonymous, voluntary, electronic survey instrument on SurveyMonkey (SurveyMonkey Corporation, Portland, OR) was sent to students. Students who did not respond to the initial invitation were sent reminders at 2 weeks and 4 weeks.
After graduation of each class, the survey for that year was closed and data were downloaded into Microsoft Office Excel 2007. Only data from complete survey instruments were included in the analysis. Categorical variables were analyzed using the chi-square or Fisher exact test as appropriate. Survey variables assessed with Likert scales were analyzed using the independent-samples t test. All data analysis was conducted using SPSS, version 17.0 (SPSS Inc, Chicago, IL). All p values were 2-sided and considered significant if less than 0.05 for all results.
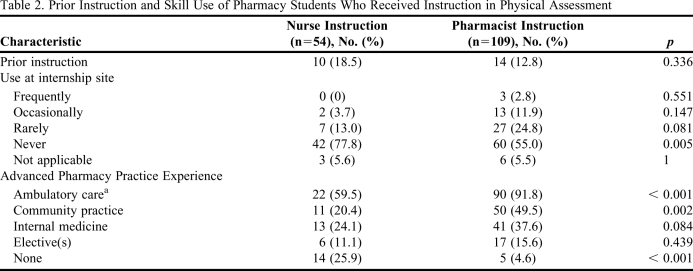
Two hundred four students were surveyed: 73 from the class of 2008, 62 from the class of 2009, and 69 from the class of 2010. Fifty-four students from the class of 2008, 49 from the class of 2009, and 60 from the class of 2010 completed the survey instrument, for an overall response rate of 80%. Prior instruction and skill use at baseline did not differ significantly overall between the groups (Table 2), although more students instructed by nurse faculty members reported they had never used their physical assessment skills at their internship site.
Table 2.
Prior Instruction and Skill Use of Pharmacy Students Who Received Instruction in Physical Assessment
a Analysis based on the number of students who completed their ambulatory care APPE at the time of the survey (n = 37 for nurse instruction; n = 98 for pharmacist instruction)
The percentage of students who reported involvement in performing physical examinations prior to instruction was 17.4% for those instructed by pharmacists compared to 22.2% for those instructed by nurses (p = 0.463). However, after instruction, 88.1% of students who had received pharmacist instruction reported being involved in performing physical examinations compared to 75.9% who had received nurse instruction (p = 0.046). Similarly, there was a significant increase in physical assessment skill use by students who received instruction from pharmacist faculty members compared to students who received instruction from nurse faculty members (Table 3).
Table 3.
Change in Use of Physical Assessment Techniques After Instruction
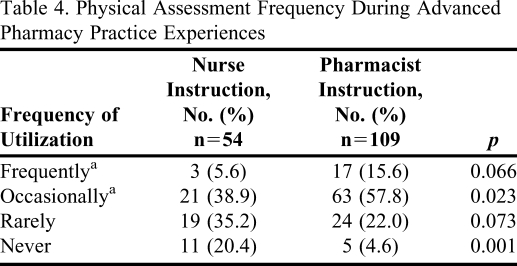
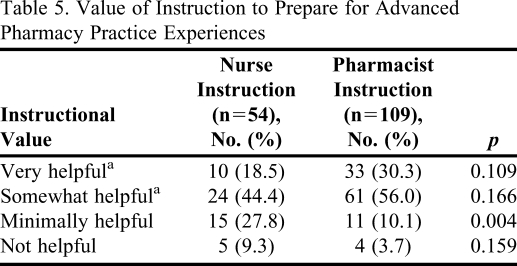
As for use of physical assessment skills during APPEs, significantly more students instructed by pharmacist faculty members felt they frequently or occasionally used their skills compared to students instructed by nurse faculty members (Table 4). Table 2 shows the use of physical assessment skills among APPE categories, with ambulatory care having the most prevalent use. However, significantly more students instructed by pharmacist faculty members used their skills during both their ambulatory and community APPEs than those instructed by nurses. The results in Table 5 also indicate that students instructed by pharmacist faculty members felt more prepared to perform physical assessments during their APPEs than those instructed by nurse faculty members.
Table 4.
Physical Assessment Frequency During Advanced Pharmacy Practice Experiences
a p < 0.001 for combined utilization frequency of “frequently/occasionally” for pharmacist compared to nurse instruction.
Table 5.
Value of Instruction to Prepare for Advanced Pharmacy Practice Experiences
a p = 0.001 for combined instructional value of “very/somewhat helpful” for pharmacist compared to nurse instruction.
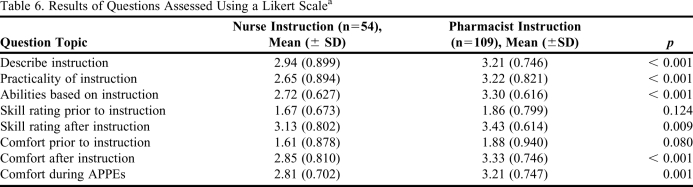
The results of survey questions that asked students to rank items on a Likert scale are summarized in Table 6. Compared to students who received nurse faculty instruction, those instructed by pharmacist faculty members consistently gave higher rankings to the instruction they received. In particular, they rated the quality of their instruction significantly higher and gave a higher rating to the practicality of the instruction. Students instructed by pharmacist faculty members also rated their physical assessment abilities higher than did students instructed by nurse faculty members. In addition, although students in both groups indicated improvement in their skills and comfort level after instruction, those instructed by pharmacist faculty members rated both their skills and comfort level significantly higher after instruction than did students instructed by nurse faculty members. Students instructed by pharmacist faculty members also rated their comfort level during APPEs as being significantly higher.
Table 6.
Results of Questions Assessed Using a Likert Scalea
Abbreviations: APPEs = advanced pharmacy practice experiences
Results reported are based on a Likert scale of 1 to 5, where 1 = poor, 2 = below average, 3 = average, 4 = above average, and 5 = excellent.
DISCUSSION
Our original hypothesis was that by emphasizing and reinforcing practical physical assessment skills performed by practicing pharmacists, students would use their skills more frequently in practice settings. Therefore, we redesigned the physical assessment portion of the Pharmacy Care Laboratory series to include both didactic instruction and application of the practical skills commonly used by pharmacists for assessing organ systems. Overall, students who received their instruction after the course redesign used their skills more often in providing patient care.
For most pharmacy students, the practice of physical assessment is quite foreign as it may not typically be performed in the pharmacies where they are employed. The exercises involving application of physical assessment skills using a partner allowed students to learn what is an unremarkable physical examination. At the same time, students gained experience in performing assessment techniques they could use in practice. The simulation mannequin provided students with additional experience and the opportunity to auscultate and evaluate abnormal findings that should be reported.
In addition to the experience provided in the Pharmacy Care Laboratory, introductory pharmacy practice experiences (IPPE) in the Nesbitt College of Pharmacy expose students to practitioners and various advanced clinical practices early in the curriculum. The IPPE curriculum offers students the opportunity to collaborate with other healthcare professionals and participate in interprofessional education settings. Therefore, the change to pharmacist faculty members teaching physical assessment gives doctor of pharmacy students a practical perspective for using these skills at the beginning of the second professional year. With their first interprofessional IPPE experiences occurring in the second professional year they then have time to practice and refine their skills soon after instruction.
The most notable finding from our study was that students who received instruction after the course redesign reported higher skill use than students taught by nurses. In addition, student satisfaction with instruction was significantly higher in the group that received the redesigned curriculum. Whether this greater use and satisfaction can be attributed to a perceived increase in relevance of the material to practice or variation among classes surveyed cannot be concluded as it was not formally assessed. Our evaluation also does not allow for definitive conclusions regarding whether these differences are due to instruction being provided by pharmacist instead of nurse faculty members or the revised course objectives and material.
APPE experiences provide students with greater frequency and opportunity to use their physical assessment skills than internships (paid work experiences). However, the significant difference reported between the groups for skill use during ambulatory and community APPEs may have been a function of survey timing rather than changes in the course or instructors. All students in the group instructed by nurse faculty members would not have completed their required ambulatory and community practice APPEs before the October 2007 survey date. We accounted for this in our analysis of skill use during ambulatory care APPEs by only basing it on the number of students who had completed that experience at the time of the survey.
Another factor that may have influenced student skill use during these APPEs was that one of the pharmacist instructors for the physical assessment portion of the Pharmacy Care Laboratory series also served as a preceptor for an ambulatory care APPE. Because the survey was conducted anonymously, we are unsure how many students had completed their Ambulatory Care APPE with this instructor at the time the surveys were administered. However, we do not feel this had a large influence on our results as this instructor would only have served as an ambulatory care APPE preceptor for a small portion of the students surveyed. Therefore, despite these 2 factors we believe our evaluation demonstrates an overall increase in student use of their physical assessment skills as a result of the course changes.
In each group assessed, a small portion of students reported that they had received instruction on physical assessment prior to this laboratory series. However, the effect of prior instruction was believed to be insignificant as most students indicated that they rarely or never had the opportunity to use their physical assessment skills at their internship sites. This is in contrast to the percentage of students who used their skills during their APPEs, where we found significantly more students who received instruction after redesign of the course reported they frequently or occasionally used their skills. This difference may be due to the lack of specific outcomes or learning objectives that need to be met for most pharmacy internships.
This study has a number of limitations. Two distinct, unmatched groups were compared in the analysis. Randomizing students from consecutive classes to a particular instructional group would have provided more robust results. Such a design also would have allowed for more definitive conclusions to be drawn regarding any influence of nurse compared to pharmacist faculty instruction on the results. However, the acute change in the curricular objectives did not allow for such a design. Another limitation was the use of a student survey for qualitative evaluation of the instructional redesign. In addition, the timing of survey administration may have influenced the results. The survey was administered to the class of 2008 in the fall semester (October 2007) prior to graduation, but for the classes of 2009 and 2010, the survey was not administered until their last APPE of the year, just prior to graduation. This resulted in fewer students in the class of 2008 having the opportunity to use their skills during APPEs compared to students in the classes of 2009 and 2010. It is unknown whether the greater time in which students had opportunities to use their physical assessment skills affected the survey results.
Although our evaluation appears to demonstrate consistent student learning and an increase in skill use, whether our curricular changes will continue to have any impact on eventual practice habits of our graduates is unknown. Whether similar curricular changes in other schools of pharmacy would produce similar results also is unclear. Our instructional redesign also does not account for any effect of interprofessional education in physical assessment. The curricular change we have described lacked coordinated input from and participation with nurse faculty members. A collaborative effort between both groups of instructors may have produced a curriculum that resulted in even greater student comfort with and use of physical assessment skills. Such collaboration between nurse and pharmacist faculty members during an ambulatory care APPE has been reported with favorable results.8 Finally, future areas for improvement in our instructional design may include developing the physical assessment practical into an objective structured clinical examination to assess student competence.
CONCLUSION
The goal of this curricular change was to teach students the practical physical assessment skills needed by a practicing pharmacist, and we hypothesized that this would lead to an increase in use of those skills by students. Students felt the instruction provided after the course redesign was more practical than that previously provided, and they used their skills more in various practice settings. However, it does not allow for conclusions regarding the influence of collaborative interprofessional instruction on students’ use of physical assessment skills. Patient physical assessment is a skill set that will become increasingly important to pharmacists as they continue to expand their professional roles. By focusing physical assessment curriculum on the practical skills a pharmacist will need to provide patient care, pharmacy students may be more confident in those abilities and use them more frequently.
REFERENCES
- 1.Irons BK, Seifert CF, Horton NA. Quality of care of a pharmacist-managed diabetes service compared to usual care in an indigent clinic. Diabetes Technol Ther. 2008;10(3):220–226. doi: 10.1089/dia.2007.0262. [DOI] [PubMed] [Google Scholar]
- 2.Rospond RM, Tice A, Tice B. Physical assessment for the community pharmacist, part 2. America's Pharm. 1999;121:47–53. [Google Scholar]
- 3.Jones RM. Patient assessment and the pharmacist's role in patient care. In: Jones RM, Rospond RM, editors. Patient Assessment in Pharmacy Practice. 2nd ed. Philadelphia, PA: Lippincott, Williams, & Wilkins; 2009. pp. 2–11. [Google Scholar]
- 4. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. January 15, 2006. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed January 27, 2011.
- 5. 2005 and 2006 AACP Pharmacy Practice Educational Outcomes and Objectives Supplements Task Force. Pharmacy Practice Supplemental Educational Outcomes Based on CAPE 2004. American Association of Colleges of Pharmacy. http://www.aacp.org/resources/education/Documents/PharmacyPracticeDEC006.pdf. Accessed January 27, 2011.
- 6.da Camara CC, D'Elia RP, Swanson LN. Survey of physical assessment course offerings in American colleges of pharmacy. Am J Pharm Educ. 1996;60(4):343–349. [Google Scholar]
- 7.Spray JW, Parnapy SA. Teaching patient assessment skills to doctor of pharmacy students: the TOPAS study. Am J Pharm Educ. 2007;(4):71. doi: 10.5688/aj710464. Article 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hilaire M, Snook M, Wozniak J. Implementation of physical assessment curriculum during a 4-week ambulatory care rotation [abstract] ASHP Midyear Clinical Meeting. 2007 [Google Scholar]
- 9.Longe RL. Teaching physical assessment to doctor of pharmacy students. Am J Pharm Educ. 1995;59(2):151–155. [Google Scholar]
- 10.Sobieraj DM, Mccaffrey D, Lee JJ. Redesign and evaluation of a patient assessment course. Am J Pharm Educ. 2009;(737):73. doi: 10.5688/aj7307133. Article 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones RM, Rospond RM. Patient Assessment in Pharmacy Practice. 2nd ed. Philadelphia, PA: Lippincott, Williams and Wilkins; 2009. [Google Scholar]