Abstract
Objective
To develop, implement, and evaluate a new interprofessional learning module that focused on asthma health promotion called Taking Action Together for Asthma.
Design
Faculty members in medicine, nursing, and pharmacy courses recruited 10 students each to participate in a 3-day interprofessional learning module. Students received extensive materials including a workbook to document their expectations and experience; completed a 1-day interprofessional workshop; received training in the Triple A (Adolescent Asthma Action) program; and went into high schools and taught the Triple A program to students in interprofessional teams.
Assessment
Before and after participating in the module, students completed a questionnaire consisting of 3 previously validated instruments: the Asthma Knowledge for Health Professionals Scale, Attitudes Toward Health Care Teams Scale, and Readiness for Interprofessional Learning Scale (RIPLS). Seventeen students completed both the pre- and post-module scales and significant changes were seen only in means scores for the Attitude Toward Healthcare Teams (81.0 ± 4.7 to 85.2 ± 5.9) and the Teamwork and Collaboration subscale of the RIPLS (41.4 ± 2.7 to 43.2 ± 2.7).
Conclusion
Health promotion activities offer a viable mechanism for fostering interprofessional learning among health professions students.
Keywords: interprofessional learning, health professionals, teamwork, asthma
INTRODUCTION
Health care professions students share common core values, knowledge, and skills, yet in many universities, they are taught in isolation from one another, in what has been described as “professional silos.”1 Future health care service providers should have an opportunity to experience interprofessional education during their preparation for professional practice.2 Comprehensive reviews undertaken by health departments in Australia, New Zealand, Canada, and the United Kingdom emphasize the importance of interprofessional learning in providing quality health care.3-9 The European Interprofessional Education Network is trying to develop a network of universities across 6 countries to promote good practices in interprofessional learning and teaching in health sciences and social care.10
In the United States, there also are strong expectations for professional health care education in general,8 and pharmacy education specifically, to be interprofessional.11,12 The American Association of Colleges of Pharmacy (AACP) Center for the Advancement of Pharmaceutical Education (CAPE) clearly outline this in their Educational Outcomes, 2004.11 The Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree (effective July 2007)12 also strongly emphasize interprofessional learning.
The Centre for the Advancement of Interprofessional Education (CAIPE) defines interprofessional learning as “occasions when two or more professions learn from and about each other to improve collaboration and the quality of care.”4 The 1988 World Health Organization (WHO) document “Learning Together to Work Together for Health” 13 suggests that interprofessional learning is not an end, but rather a means to an end where interprofessional students can recognize the healthcare team's joint responsibility for prioritized community health goals.13
Interprofessional learning projects usually focus on practice experience training to place different health professions students together in the care of patients, particularly in a hospital setting.14,15 Only a few interprofessional learning projects have explored health promotion as a means of learning and teaching university students how to deliver health education messages in community settings, eg, schools, nurseries, community clubs, or prisons.16,17 However, most of these initiatives have not used evidence-based health education/health promotion programs, nor have any targeted a particular high-burden disease, such as asthma.
One of the responsibilities of health professionals is health promotion. This is reflected globally in professional pharmacy practice standards. In their revised educational outcomes in 2004, CAPE listed public health as a core competency for pharmacy practitioners of the future.11 Similarly, the 2010 edition of the Professional Practice Standards published by the Pharmaceutical Society of Australia states that pharmacists are expected to actively engage individual consumers and the community to promote health and wellbeing.18 Globally, the profession of pharmacy is evolving to include provision of services that require multidisciplinary health care input, such as pharmaceutical care and disease management. These service models require significant teamwork and collaboration among professionals.
Collaboration of pharmacists in the care process improves the quality of care and patient outcomes.19 Although collaborative care improves both clinical and economic outcomes, communication problems often occur between pharmacists and other members of the health care team and pharmacists’ recommendations often are not accepted by other providers.20
Most pharmacy curricula include references to service provision and provide pharmacy graduates with the clinical skills and competence to participate with other health care professionals as providers of high-quality patient services. However, pharmacy student training to work collaboratively with other health professionals is minimal in most colleges and schools. Public health and health promotion concepts are incorporated in some novel pharmacy curricula, 21,22 but the use of interprofessional learning concepts to emphasize that health promotion and health education is a role shared by all health professionals is minimal.
Australia has one of the highest prevalence rates of asthma in the world, and asthma is listed as a national health priority.23 Because a high proportion of asthma cases is managed at the community level, primary care health professionals have a key role in the management of this disease.24 The Australian National Asthma Strategy suggests that to change the face of asthma in Australia, it must be ensured that those without asthma and who do not have the tendency towards developing asthma remain so, and that this can be achieved by raising general awareness of asthma and asthma risk factors.24 Schools are considered good venues for health education because children are the future adult population and they will share health messages heard at school with their parents and other members of the community.
The Triple A program (Adolescent Asthma Action), is an evidence-based asthma education program that was developed to raise asthma awareness among school children with asthma.25 The program uses social modelling and supportive environments based on Bandura's Social Cognitive Theory26 and is inspired by Paolo Freire's empowering education philosophy.27 Triple A recruits senior school students who first learn from trained educators and then teach younger students. The program improves the asthma knowledge of school students with asthma and their peers.28 The research team has used the Triple A program as an educational tool in different disciplines including to train fourth-year pharmacy students as Triple A educators, who then went into schools and trained students. These pharmacy students rated the asthma learning experience higher than did their peers who completed regular asthma tutorials instead.29 Similarly, practicing community pharmacists were trained in and then delivered the Triple A program to local school students, resulting in significant increases in students’ asthma knowledge.30 In the US, a program similar to Triple A, called Open Airways, has been developed and delivered in schools with the help of undergraduate students in health care courses.31
Although the Triple A program had been used for asthma training of medical students at the University of Sydney, Australia, the program's potential as an interprofessional learning tool had not been explored.32 The aim of this project was to develop, implement, and evaluate a new interprofessional learning module for students enrolled within the university's Faculties of Health (Medicine, Nursing, and Pharmacy).
The learning module was named Taking Action Together for Asthma. Our study hypothesis was that participating in an interprofessional learning module with hands-on experience in providing asthma education to high school students would improve health care professional students’ knowledge about asthma and their readiness to undertake interprofessional learning and work in health care teams. As there was preexisting evidence for the effectiveness of the Triple A program in improving students’ knowledge of asthma and attitudes towards asthma in school students, this was not the aim of the project; the project focused instead on the attitudes and experiences of university students engaged in interprofessional learning.
DESIGN
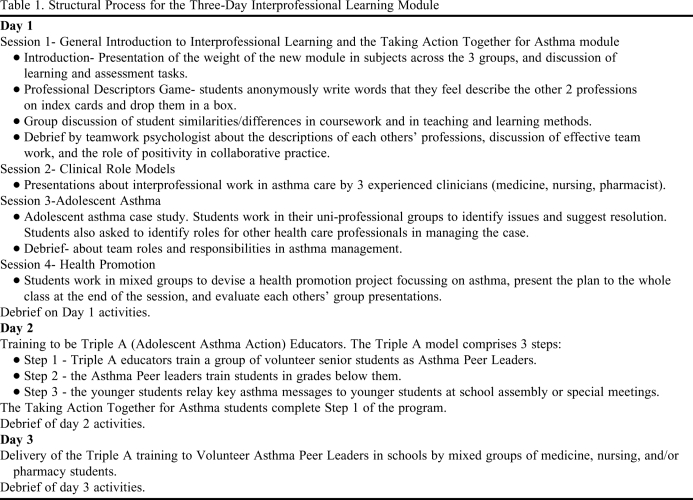
Health program students at the University of Sydney were the target participants for the Taking Action Together for Asthma module. The group included students in medicine (years 1 and 2 of a 4-year graduate-entry course), nursing (year 2 of a 2-year graduate-entry course,) and pharmacy (year 4 of a 4-year undergraduate course). The 3-day Taking Action Together for Asthma module (Table 1) was embedded as an option into an Independent Research and Learning Project for medical students and into clinical placement subjects for nursing and pharmacy students.
Table 1.
Structural Process for the Three-Day Interprofessional Learning Module
At the start of second semester in 2008, faculty members invited students through promotional flyers and during lectures. Students were accepted (n = 10 from each faculty member), until the study quota of 30 was reached. This quota was based on resource feasibility.
The Taking Action Together for Asthma module had 2 main components: a 1-day (7 hours) interprofessional learning in asthma workshop intended to encourage students to learn with and from each other about the role of each profession in asthma management (Table 1); and the training (day 2) for and actual delivery of the Triple A program to high school students (day 3).
The workshop and Triple A training (days 1 and 2) were held on-campus in October 2008. Students were assigned to seats so that during general discussions there were students from different disciplines at each table. Symbolism and imagery was used thematically across module activities and resources to enhance team formation between the different groups of health care students. For example, students were provided with name tags with their own faculty colors for sessions 1 and 2 on day 1, and then switched to having a uniform name tag with the project logo to symbolize the move from distinct entities to a single entity. In the introductory session on day 1, students were provided with a comprehensive student manual, readings, and activity sheets in resource folders. Reading the manual established the context and need for learning about asthma, and highlighted the immediate value of the learning -- an important fulcrum for adult learners.33 The manual included background information, learning objectives, information on course credit, and requirements for successful completion of the Taking Action Together for Asthma module; a workbook that needed completion prior to, during, and after participating in the module; and reference material about interprofessional learning and adolescent asthma. An eLearning Web site provided participating students with module information and allowed online discussion and submission of assessment tasks.
Case-based learning on day 1 used a problem-solving approach while the health promotion project design exercise on day 1 and the delivery of the Triple A program to school students on day 3 used experiential learning. These teaching approaches offered student participants the chance to undertake both exchange-based learning (discussions, problem-solving) and action-based learning (project work, experiential group work).34 The Taking Action Together for Asthma learning objectives included knowledge, attitude, and skill development34 and generally focused on: (1) learning from and about each other, (2) developing effective teamwork, (3) understanding and valuing team roles in asthma, (4) dealing with issues in adolescent asthma, and (5) learning to deliver key asthma education messages to an adolescent audience. Learning outcomes, activities, and assessments were aligned strategically, and different types of learning objectives were assessed using Bloom's Taxonomy of Learning Outcomes35 (Table 2). The students’ achievement of demonstrated prestructural, unistructural, multistructural, relational, and abstract learning outcomes were assessed using graded descriptors based on the Biggs’ SOLO (Structure of Observed Learning Outcomes) taxonomy.36 Students were provided with these descriptors and clearly explained about how these descriptors would be applied to their work.
Table 2.
Learning Outcomes and Learning Typology for the Taking Action Together for Asthma Module
a Brackets indicate classification by Bloom's Taxonomy35
b Participation in all module activities on days 1, 2 and 3 = 30%; completion of workbook items = 30%; reflective essay (group or individual) = 40%.
Following the training, the Taking Action Together for Asthma students formed interprofessional teams and delivered the Triple A program to high schools. The project received ethical approval from the University of Sydney's Human Research Ethics Committee.
EVALUATION AND ASSESSMENT
A multimethod research design that involved data collection before, during, and after completion of the 3-day module was adopted.34 The Barr (1996) typology 41 was used to ensure that several interprofessional learning outcome levels were being measured.
Three validated scales were incorporated into a pre- and post-module questionnaire to examine learning outcomes for asthma and interprofessional learning:
(1) Asthma Knowledge for Health Professionals scale, which consists of 18 true/false items.37
(2) Attitudes Towards Health Care Teams scale, which consists of 21 items scored on a 5-point Likert scale.38-40
(3) Readiness for Interprofessional Learning Scale, which consists of 19 items scored on a 5-point Likert scale.42-44
The following qualitative data also were collected:
Feedback from interviews conducted by a project officer with volunteer students after completion of the module.
Reflective essays in which students were required to critically reflect on their interprofessional learning experience.
Professional descriptors of the other 2 professions, which students wrote anonymously on index cards on day 1 and placed in a slotted box.
All data were entered into an SPSS Version 17.0 (Chicago, IL) database. Paired comparisons were made using student t tests for mean scores. Analyses of variance (ANOVAs, repeated measures) were conducted to test for differences among discipline groups. Analyses of Attitudes Towards Healthcare Teams and the Asthma Knowledge for Heath Professionals scales were run on means of the total scores. Analyses for the modified RIPLS were conducted on mean total scores and also means for each of the subscales.
Outcomes
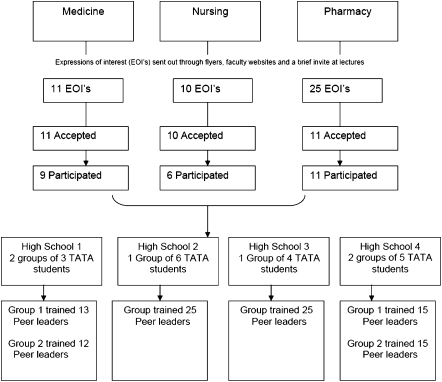
Twenty-six university students (9 medical students, 6 nursing students, and 11 pharmacy students) participated in and completed the Taking Action Together for Asthma module. Seventy-three percent of the students were female. The mean age of students was 26.5 ± 8.8 years. Six interprofessional learning groups of 3 to 6 university students from at least 2 professional groups conducted the Triple A peer leaders workshop at 4 participating high schools in New South Wales, Australia. Cumulatively, the university students trained 105 year high school students as Triple A peer leaders. The peer leaders trained by the health professions students went on to educate more than 250 younger students at their respective schools. A flowchart of the delivery of the health promotion to the school communities is outlined in Figure 1.
Figure 1.
Flow chart of health care students’ participation in the Taking Action Together for Asthma module (July-October 2008). Abbreviatins: EOI = expressions of interest; TATA = Taking Action Together for Asthma.
Questionnaire.
All Taking Action Together for Asthma students completed the questionnaires at baseline (prior to starting session 1 on day 1 of Taking Action Together for Asthma), and 17 completed the questionnaires and sent them back after completing the module (completers: 4 medical students, 23.5%; 4 nursing students, 23.5%; and 9 pharmacy students, 52.9%).
Of a possible total score of 17, the professional students’ mean asthma knowledge score at baseline was 13.8 ± 1.5 (n = 26). After completing the module, the mean score was 14.0 ± 2.0 (n = 17). Thus, no significant change in mean asthma knowledge scores occurred for either the overall group (p = 0.726), or within each of the 3 professions (p = 0.446).
The mean score on the Attitude Towards Healthcare Teams scale before completing the module was 81.0 ± 4.7 (n = 26). Postmodule, the mean score was 85.2 ± 5.9 (n = 17) of a maximum possible score of 105. This change was significant (p = < 0.003); however, there were no significant differences between professions for change in attitudes over time (p = 0.33). Mean scores for the overall modified RIPLS were high at both baseline (79.8 ± 5.7, n =26) and post-module (81.7 ± 5.7 n = 17) with no significant difference in scores before and after completing the module (p = 0.056); maximum possible score for the RIPLS was 95. Like the overall RIPLS score, the mean scores for both the Teamwork and Collaboration and Professional Identity subscales of the RIPLS also were high at baseline and postmodule; however, the change in scores on the Teamwork and Collaboration subscale (9 items, maximum score 45) from 41.4 ± 2.7 (n =26) to 43.2 ± 2.7 (n = 17) was significant (p = 0.047). Scores for the Roles and Responsibilities subscale of the RIPLS (3 items, maximum score 15) were low at commencement of the module (6.9 ± 2.1, n = 26) and remained low at completion of the module (6.0 ± 1.8, n = 17), with no significant changes found. No differences between pre- and post-module scores were found for total RIPLS or subscale scores between the 3 professional groups of students (repeated measures ANOVA).
Qualitative Results
The index cards with descriptors of other professions were removed from the box and read. Interviews were conducted over the telephone, audiotaped, and transcribed verbatim. Reflective essays were received electronically from students.45 Two researchers with experience in qualitative research coded these data sources. Emergent themes were shared with the wider research team and a consensus on how these themes added to an understanding of the results was reached.
Professional descriptor data.
All 26 students completed the professional descriptors data on day 1. A thematic analysis of phraseology used in the professional descriptors submitted on day 1 of the module suggested that many students held preconceived notions about the other 2 professional groups before initiating the Taking Action Together for Asthma module. Doctors were seen by nursing and pharmacy students as “intelligent,” “knowledgeable,” and “educated.” They also were seen as “professional.” Some students perceived doctors to be “decisions makers” and “community leaders.” However, several students perceived the doctors to be “arrogant,” “aloof,” or “paternalistic.”
Nurses were described by the pharmacy and medical students as “caring” and “kind.” They also were perceived to have a lot of “sympathy” and “compassion,” and to have “good patient communication skills.” Nurses were seen as “practical,” “hard-working,” “professional,” “dedicated,” and “reliable.” They also were seen to be “busy,” “rushed,” and “overworked.”
Like the doctors, pharmacists also were described as being “knowledgeable.” They were described as “professional,” as well as “precise,” and “meticulous.” Responses regarding interpersonal skills were mixed, with some students describing them as “helpful” and “approachable,” and others perceiving them as “nerdy,” “boring,” or “too serious.” A few students described pharmacists as “community focused.”
Interviews.
Seven students provided feedback on the Taking Action Together for Asthma module through qualitative interviews (2 medical, 2 nursing, and 3 pharmacy students). During the feedback interview, more than half the students expressed that they had few expectations about the module. The remaining students felt that the module either met or exceeded their expectations. With respect to the interprofessional learning aspects, 3 students expressed some initial concern about whether students from different faculties (ie, schools) would get along, but were pleased to find out that they “got along well.” Some students felt that the module allowed them to build on their knowledge about asthma management by learning how to use it in a health promotion setting.
When asked what they felt they learned about the 2 other professions, students stated they learned not only about the roles of the other health professionals and the settings where they worked, but also about their own actions. Most students observed that the knowledge bases required of the 3 disciplines were similar. Although problem-solving approaches differed and were influenced by discipline-specific training, the different approaches brought new ideas “to the table” and would enrich patient care.
Overall, the students felt that participation in the Taking Action Together for Asthma module had a positive influence on their perceptions of other health professions. Several students commented that the module helped them to better appreciate the importance of each profession's potential contribution to patient care. During the interviews, some students felt that the module helped to address some prior perceptions they had held. A female medical student observed: “I think that if you understand…what they can contribute, it's really useful because then you're not just guessing that they can do something and you're not excluding them from something, because you know they can do it.”
Most students enjoyed the training sessions and appreciated the opportunity to work with different people. Some students commented that they appreciated the opportunity to put interprofessional theory into practice and that they learned about teamwork “by doing it and not just by reading about it.”
Most students “really enjoyed” implementing the Triple A program in the high schools. A male pharmacy student commented: “…We were actually having to sit down as a team and work through how we were going to present it as a team…and I think it was really beneficial to get us to think about working together.”
Some students mentioned that it would be appropriate to include other allied health professionals, such as occupational therapists and physiotherapists, in such activities. Some students felt “confused” about fulfilling the module requirements within their own disciplines and expressed that this caused them some stress. They suggested that more information about module requirements be provided at the time of recruitment in the future. Students felt that the interprofessional learning module worked well with asthma, but also saw potential for the module to be used in the future with other chronic diseases, such as diabetes, because of the need for management by interprofessional patient care teams. They specifically mentioned the value of continuing the module in future years and that they would recommend it to future health care students.
Several students commented on the timing of the training sessions. The module was scheduled late in the semester when students had a heavy assessment load and students would have preferred it to be scheduled earlier in the semester.
Student Essays.
Student essays provided further insight into how the module had worked. Some students noted the importance of logistics and planning for smooth operation of the school-based activity. Most valued the opportunity to conduct education in non-clinical settings, and valued the interaction with school students. A key theme was the benefit of presenting a united front to the school students, so they viewed the University teams as a group of future health care professions rather than as a group of future doctors, nurses, or pharmacists. Students also reflected that the group based nature of the activity allowed them to be relaxed, knowing they could rely on each other for help and answers to any questions posed by the school students.
DISCUSSION
Taking Action Together for Asthma is an interprofessional learning initiative that was conceived by a team of researchers from different faculties of health (medicine, nursing, and pharmacy). The module for the program was developed based on principles of adult learning, and it was successfully embedded into existing units of study across the 3 faculties at The University of Sydney. A unique feature of the Taking Action Together for Asthma module included a health promotion activity completed by mixed teams of professional students. Our study hypothesis was that participating in an interprofessional learning module with hands-on experience in asthma education would improve students’ knowledge about asthma, and their readiness to undertake interprofessional learning and work in health care teams. A positive change occurred in students’ attitudes toward teamwork in health and toward teamwork and collaboration. Student feedback indicated that they had a greater understanding of the roles of each health professional in the management of asthma, and had learned about, with, and from each other.
In terms of planned outcomes, students’ asthma knowledge scores were high prior to participating in the module and remained high after completing the Taking Action Together for Asthma program. All students were either final-year undergraduate students or postgraduate students and had studied asthma and its management prior to completing the module. Additionally, the national asthma guidelines were placed on the list of recommended readings for students to review prior to participating in the module, perhaps affecting knowledge increases. Nonetheless, students’ comments during their feedback interviews indicated that contextualizing the interprofessional learning within the asthma management framework was effective in increasing their awareness of the roles of different health care professions in the care of this chronic condition. A clear clinical focus (instead of broad-scoped activities) for learners has been a recommendation for interprofessional learning planners,46 and the effectiveness of having this focus in an interprofessional learning activity is reflected in the students’ comments.
Another outcome was a significant positive shift in students’ attitudes after completing the module. Further, a significant change was found for the Teamwork and Collaboration subscale of the RIPLS, but there were no significant improvements for overall RIPLS score or for the other 3 subscales of the RIPLS. However, the mean score for overall RIPLS and 3 of the 4 subscales were high at commencement of the module and remained high at completion of the module; this trend has been reported for other interprofessional learning initiatives.1,47 In our study, students volunteered to participate and that may have affected the outcomes. Conducting studies with complete student cohorts rather than voluntary subsets in the future may shed more light on students’ readiness for interprofessional learning. The literature on the effect of interprofessional learning on participants’ attitudes towards health professionals and perceptions of other health professionals suggests that with a single intervention, mostly limited changes are seen.14,48 A Cochrane Review of the impact of interprofessional education49 also found mixed results regarding outcomes of interprofessional initiatives, partially attributed to the complexity of such educational interventions and the scarcity of sensitive instruments to measure their effect.
In our study, while no significant changes occurred in students’ scores on quantitative scales after completing Taking Action for Asthma, students’ feedback during the interview indicated that a change in attitudes toward other professionals had occurred, in some cases, resulting in the shedding of preconceived notions about them. These changes have been qualitatively described by interprofessional learning students in other studies.1,50,51 The inclusion of qualitative methodology in the evaluation of interprofessional learning initiatives may provide more detailed information about what is actually being achieved in such initiatives in terms of effect on participating individuals.14 Using student reflections as a data source was a unique feature of our evaluation of the module. Reflective essays provide students an opportunity to synthesize learning, enabling them to see linkages between experiences and learning goals and to provide summative evaluation of their own progress. This data set presented a rich tapestry of students’ thoughts and experiences, unprompted by framed questions.52
Overall the students highly valued the opportunity to participate in this interprofessional learning initiative and were satisfied with the module. It helped them to appreciate not only their own public health role but also the roles of other health professionals. The activities designed to illustrate the notion of differing professional approaches and the symbolism of coming from uniprofessional groups and moving towards interprofessional groups was particularly effective. In addition to learning together, the experience of working together as an interprofessional team was highly appreciated by the students. “The students’ feedback that the interprofessional learning module should be applied to other chronic diseases suggests that learning outcomes extended beyond the unistructural element to the relational elements in the SOLO framework.36
This study did have limitations including a small sample size, uneven participation levels from the 3 professions represented, and students’ self-selection into the module. Students who volunteered tended to have high asthma knowledge scores and positive attitudes regarding interprofessional teamwork before completing the module. No follow-up study was planned to examine how the interprofessional learning translates into practice once the students become practicing health professionals. Organizational issues, such as aligning the timetables of different courses and adding interprofessional learning into already crowded curriculum were the key challenges, and are fairly common to interprofessional learning initiatives.14,48 The voluntary nature of the course allowed for smaller numbers and therefore for sustainability of the module in future years. Although data were not collected, the module was conducted again successfully in 2009. Motivated students use creative ways to mange the logistics and time challenges that completing the module presents, making participation possible. Students’ comments about resource and course organization were overwhelmingly positive, and hence no changes to course materials have been made.
CONCLUSIONS
This study successfully pilot tested a new interprofessional learning module on asthma for medicine, nursing, and pharmacy students. Health education and health promotion offer a viable mechanism of fostering interprofessional learning, particularly as students focus more on the activity and learning with and about each other instead of on acquiring clinical skills. Interprofessional learning should be more widely used and tested by pharmacy educators.
ACKNOWLEDGEMENTS
The University of Sydney provided a Teaching Improvement Funding Grant to support this project. Dr. Murray Fisher, Associate Dean of Learning and Teaching, Faculty of Nursing and Midwifery, is acknowledged for his valuable time in attending and supporting staff meetings. Associate Professor Tania Gerzina, Institute of Teaching and Learning, University of Sydney, Australia, is acknowledged for her valuable feedback as an independent observer. Associate Professor Helen Reddel and Ms Jane Civitco, Royal Prince Alfred Hospital, Asthma Clinic, Camperdown, Sydney, are acknowledged for their presentations.
REFERENCES
- 1.Margalit R, Thompson S, Visovsky C, et al. From professional silos to interprofessional education: campuswide focus on quality of care. Qual Manag Health Care. 2009;18(3):165–173. doi: 10.1097/QMH.0b013e3181aea20d. [DOI] [PubMed] [Google Scholar]
- 2. L-TIPP (Aus). Interprofessional Health Education in Australia: The Way Forward. http://www.altc.edu.au/resource-learning-teaching-health-position-paper-uts-2009. Accessed February 10, 2011.
- 3. Bagot KL, Lawson M, Jolly B, et al. International approaches to undergraduate clinical training. 2005. Melbourne: Policy & Strategic Projects Division, Department of Human Services, Victoria. Australia. http://www.health.vic.gov.au/__data/assets/pdf_file/0019/306163/approaches_clintraining2007.pdf. Accessed January 27, 2011.
- 4.Centre for the Advancement of Interprofessional Education. Interprofessional Education: a Definition. London, UK: Centre for the Advancement of Interprofessional Education; 1997. [Google Scholar]
- 5.Department of Health. A Health Service of All the Talents: Developing the NHS Workforce. London, UK: Department of Health; 2000. [Google Scholar]
- 6.Hendry C, Emmerson H, Youngson R. Auckland: Clinical Leaders' Association of New Zealand; 2003. Report on strategies to support the development of collaborative health leadership and management within New Zealand healthcare services. [Google Scholar]
- 7. Romanow RJ. Building on values: the future of healthcare in Canada - final report. Saskatoon: 2002; Commission on the Future of Healthcare in Canada. dsp-psd.pwgsc.gc.ca/Collection/CP32-85-2002E.pdf. Accessed February 21, 2011.
- 8.Thistlethwaite J, Nisbet G. Interprofessional education: what's the point and where are we at. Clin Teach. 2007;4(2):67–72. [Google Scholar]
- 9.Liaskos J, Frigas A, Antypas K, Zikos D, Diomidous M, Mantas J. Promoting interprofessional education in health sector within the European Interprofessional Education Network. Int J Med Inform. 2009;78(Suppl 1):S43–47. doi: 10.1016/j.ijmedinf.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 10.O'Neil EH and the Pew Health Professions Commission. Recreating Health Professional Practice for a New Century. San Francisco, CA: Pew Health Professions Commission; 1998. [Google Scholar]
- 11. American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education. Educational Outcomes 2004. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed January 27, 2011.
- 12. Accreditation Council for Pharmacy Education Accreditation Standards and Guidelines For The Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree Adopted: January 15, 2006 Released: February 17, 2006 effective July 1 2007. Accreditation Council for Pharmacy Education Chicago, Illinois. at http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed January 27, 2011.
- 13. World Health Organization. Learning together to work together for health. Report of a WHO Study Group on Multi-professional Education of Health Personnel: The Team Approach. 1988; 5, Technical Report Series, No. 769. whqlibdoc.who.int/trs/WHO_TRS_769.pdf. Accessed February 21, 2011.
- 14.Nisbet G, Hendry GD, Rolls G, Field MJ. Interprofessional learning for pre-qualification health care students: an outcomes-based evaluation. J Interprof Care. 2008;22(1):57–68. doi: 10.1080/13561820701722386. [DOI] [PubMed] [Google Scholar]
- 15.Wilhelmsson M, Pelling S, Ludvigsson J, Hammar M, Dahlgren LO, Faresjo T. Twenty years experiences of interprofessional education in Linkoping-ground-breaking and sustainable. J Interprof Care. 2009;23(2):121–133. doi: 10.1080/13561820902728984. [DOI] [PubMed] [Google Scholar]
- 16.Anderson ES, Lennox A. The Leicester Model of Interprofessional Education: developing, delivering and learning from student voices for 10 years. J Interprof Care. 2009;23(6):557–573. doi: 10.3109/13561820903051451. [DOI] [PubMed] [Google Scholar]
- 17.Kapelus G, Karim R, Pimento BB, Ferrara G, Ross C. Interprofessional health promotion field placement: applied learning through the collaborative practice of health promotion. J Interprof Care. 2009;23(4):410–413. doi: 10.1080/13561820802432364. [DOI] [PubMed] [Google Scholar]
- 18.The Pharmaceutical Society of Australia. Australia: ACT; 2010. Professional Practice Standards. Version 4. [Google Scholar]
- 19.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 20.Monte SV, Slazak EM, Albanese NP, Adelman M, Rao G, Paladino JA. Clinical and economic impact of a diabetes clinical pharmacy service program in a university and primary care-based collaboration model. J Am Pharm Assoc. 2009;49(2):200–208. doi: 10.1331/JAPhA.2009.08160. [DOI] [PubMed] [Google Scholar]
- 21.Whitley HP. A public health discussion series in an advanced pharmacy practice experience. Am J Pharm Educ. 2010;74(6) doi: 10.5688/aj7406101. Article 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fuentes D, Deguire N, Patel R, Boyce E. A team public health research project for first year pharmacy students to apply content from didactic courses. Am J Pharm Educ. 2010;74(6) doi: 10.5688/aj740699. Article 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Asthma Council Australia. Melbourne: NAC Australia; 2006. Asthma management handbook. [Google Scholar]
- 24. Australian Centre for Asthma Monitoring, Glebe, NSW, Australia 2008. Asthma in Australia 2008. AIHW Asthma Series no. 3. Cat. no. ACM 14. Canberra: AIHW. http://www.aihw.gov.au/publications/index.cfm/title/10584. Accessed February 21, 2011.
- 25.Shah S, Mamoon H, Gibson P. Peer-led asthma education for adolescents: development and formative evaluation. Health Promot J Austr. 1998;8(3):177–182. doi: 10.1016/S1054-139X(97)00203-6. [DOI] [PubMed] [Google Scholar]
- 26.Bandura A. Human Agency in Social Cognitive Theory. Am Psychol. 1989;44(9):1175–1184. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- 27.Wallerstein N, Bernstein E. Empowerment education: Freire's ideas adapted to health education. Health Educ Behav. 1988;15(4):379–394. doi: 10.1177/109019818801500402. [DOI] [PubMed] [Google Scholar]
- 28.Shah S, Peat J, Mazurski E, et al. Effect of peer led programme for asthma education in adolescents: cluster randomised controlled trial. Br Med J. 2001;322(7286):583–585. doi: 10.1136/bmj.322.7286.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bosnic-Anticevich SZ, Krass I, Shah S, Saini B, Armour C. Comparison of two methods of training of undergraduate pharmacy students in asthma knowledge confidence and skills. Am J Crit Care Med. 2002;165(8):A709. [Google Scholar]
- 30.Kritikos V, Saini B, Bosnic-Anticevich SZ, Krass I, Shah S, Taylor S, Armour C. Innovative asthma health promotion by rural community pharmacists: a feasibility study. Health Promot J Austr. 2005;16(1):69–73. doi: 10.1071/he05069. [DOI] [PubMed] [Google Scholar]
- 31.Spencer GA, Atav S, Johnston Y, Harrigan JF. Managing childhood asthma: the effectiveness of the open airways for schools program. Fam Community Health. 2000;23(2):20–30. [Google Scholar]
- 32.Shah S, Roydhouse J, Sawyer SM. Medical students go back to school: the Triple A journey. Austr Fam Phys. 2008;37(11):952–954. [PubMed] [Google Scholar]
- 33.Brookfield SD. Adult learning: an overview. In: DeCorte E, Weinert FE, editors. International Encyclopedia of Developmental and Instructional Psychology. Oxford: Elsevier Science; 1996. [Google Scholar]
- 34.Reeves S, Freeth D, McCrorie P, Perry D. ‘It teaches you what to expect in the future.’ Interprofessional learning in a training ward for medical, nursing and physiotherapy students. Med Educ. 2002;36(4):337–344. doi: 10.1046/j.1365-2923.2002.01169.x. [DOI] [PubMed] [Google Scholar]
- 35.Bloom BS, editor. Taxonomy of Educational Objectives. The Classification of Educational Goals. Handbook1: Cognitive Domain. New York, NY: McKay; 1956. [Google Scholar]
- 36.Biggs JB, Collis KF. Evaluating the Quality of Learning – the SOLO Taxonomy. New York, NY: Academic Press; 1982. pp. 12–245. [Google Scholar]
- 37.Kritikos V, Krass I, Chan HS, Bosnic-Anticevich S. The validity and reliability of two asthma knowledge questionnaires. J Asthma. 2005;42(9):795–801. doi: 10.1080/02770900500308627. [DOI] [PubMed] [Google Scholar]
- 38.Heinemann G, Schmitt M, Farrell M, Brailler S. Development of an attitudes toward health care team scale. Eval Health Prof. 1999;22(1):123–142. doi: 10.1177/01632789922034202. [DOI] [PubMed] [Google Scholar]
- 39.Hyer K, Fairchild S, Abraham I, Mezey M, Fulmerr T. Measuring attitudes related to interdisciplinary training: revisiting the Heinemann Schmitt and Farrell Attitudes Toward Health Care Teams' scale. J Interprof Care. 2000;14(3):249–58. [Google Scholar]
- 40.Leipzig R, Hyer K, Ek K, et al. Attitudes toward working on interdisciplinary healthcare teams: a comparison by discipline. J Am Geriatr Soc. 2002;50(6):1141–1148. doi: 10.1046/j.1532-5415.2002.50274.x. [DOI] [PubMed] [Google Scholar]
- 41.Barr HL. Ends and means in interprofessional education: towards a typology. Educ Health. 1996;9(3):341–352. [Google Scholar]
- 42.McFadyen A, Webster V, Strachan K, Figgins E, Brown H, McKechnie J. The Readiness for Interprofessional Learning Scale: a possible more stable sub-scale for the original version of RIPLS. J Interprof Care. 2005;19(6):595–603. doi: 10.1080/13561820500430157. [DOI] [PubMed] [Google Scholar]
- 43.McFadyen A, Webster V, Maclaren W. The test-retest reliability of a revised version of the Readiness for Interprofessional Learning Scale (RIPLS) J Interprof Care. 2006;60(6):633–639. doi: 10.1080/13561820600991181. [DOI] [PubMed] [Google Scholar]
- 44.Parsell G, Bligh J. The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS) Med Educ. 1999;33(2):95–100. doi: 10.1046/j.1365-2923.1999.00298.x. [DOI] [PubMed] [Google Scholar]
- 45.Miers M, Rickaby C, Clarke B. Learning to work together: health and social care students' learning from interprofessional modules. Assess Eval High Educ. 2009;34(6):673–691. [Google Scholar]
- 46.Reeves S, Goldman J, Oandasan I. Key factors in planning and implementing interprofessional education in health care settings. J Allied Health. 2007;36(4):231–235. [PubMed] [Google Scholar]
- 47.Horsburgh M, Rain L, Williamson E. Multiprofessional learning: the attitudes of medical, nursing and pharmacy students to shared learning. Med Educ. 2001;35(9):876–883. doi: 10.1046/j.1365-2923.2001.00959.x. [DOI] [PubMed] [Google Scholar]
- 48.Hammick M, Freeth D, Koppel I, Reeves S, Barr H. A best evidence systematic review of interprofessional education: BEME Guide no.9. Med Teach. 2007;29(8):735–751. doi: 10.1080/01421590701682576. [DOI] [PubMed] [Google Scholar]
- 49.Reeves S, Zwarenstein M, Goldman J, et al. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database Systematic Reviews no. 1, CD002213. 2007 doi: 10.1002/14651858.CD002213.pub2. [DOI] [PubMed] [Google Scholar]
- 50.Anderson ES, Thorpe LN. Early interprofessional interactions: does student age matter? J Interprof Care. 2008;22(3):263–282. doi: 10.1080/13561820802054689. [DOI] [PubMed] [Google Scholar]
- 51.Leaviss J. Exploring the perceived effect of an undergraduate multiprofessional education intervention. Med Educ. 2000;36(6):483–486. doi: 10.1046/j.1365-2923.2000.00678.x. [DOI] [PubMed] [Google Scholar]
- 52.Pollard KC, Miers ME. From students to professionals: results of a longitudinal study of attitudes to pre-qualifying collaborative learning and working in health and social care in the United Kingdom. J Interprof Care. 2008;22(4):399–416. doi: 10.1080/13561820802190483. [DOI] [PubMed] [Google Scholar]