Abstract
Objective
To evaluate the impact of a mental health elective on pharmacy students' perceptions and stigmatizing views of mental illness.
Design
An elective was designed that featured an advanced overview of psychopharmacology; student training in motivational interviewing; a presentation by the National Alliance on Mental Illness (NAMI) local chapter; introduction to pharmacy collaborations with peer support specialists, social workers, and psychiatrists; mock patient counseling sessions; and a required psychiatric patient interview at a local community mental health center.
Assessment
A survey instrument with 17 Likert-scale items was constructed to measure 2 distinct areas: social distance and stigmatizing views. The survey instrument was administered at the beginning and end of the spring 2010 semester to pharmacy students enrolled in the mental health elective course and to a control group of pharmacy students enrolled in an unrelated clinical elective. The course had a positive impact on pharmacy students' perceptions of mental illnesses. Students' social distance and stigmatizing views of mental illnesses improved, while no significant change in views occurred among students in the control group.
Conclusion
Advanced training in psychiatric medicine and exposure to mental health care are vital to prepare pharmacy students to provide unbiased, patient-centered care to this population.
Keywords: pharmacy student, mental health, elective course
INTRODUCTION
Patients with mental illness often encounter many barriers to recovery including stigma, poor insight, complex medication regimens, and serious adverse reactions, which may lead to poor treatment outcomes.1 Pharmacists are able to minimize some of these barriers to care by providing accessible medication and health education to patients with mental illness.2,3 Also, building a trusting patient-pharmacist alliance may prevent missed dosages and illness relapse. However, patients with mental illness may not be provided with adequate care by community pharmacists, due to stigma and perceived difficulty in communicating with individuals with mental illness.3,4 Pharmacists often are not as comfortable counseling and monitoring patients with mental health disorders compared to patients with other medical disease states such as cardiovascular disease or asthma.6,7
Furthermore, negative and stigmatizing attitudes are not confined to practicing pharmacists. Pharmacy students also may hold negative views.5,8,9 A survey completed at The University of Sydney School of Pharmacy assessed pharmacy students' and graduate students' attitudes toward people with schizophrenia and severe depression. They suggest that traditional teaching methods in pharmacy education may not improve social distance or stigmatizing views held by students. They also suggest that new models of pharmacy education surrounding communication between people with mental illness and pharmacists should be developed.9
Mental health electives that highlight patient recovery and barriers to recovery are not required in colleges or schools of pharmacy. Stigmatizing views toward individuals with mental illness may not be addressed adequately in pharmacy school curriculums, and graduating students must be trained to recognize these barriers to patient care, and be equipped to provide necessary care and support for these patients. In 2007, a survey of accredited pharmacy schools showed that while 100% of pharmacy curriculums included mental health topics, only 27% offered elective courses in psychiatric pharmacy.15 The lack of available services combined with negative views of pharmacy students indicate the need for further development of mental health education in pharmacy curriculums as well as evaluation of these educational methods.5,8,10-14
The purpose of this study was to determine the effect a mental health elective could have on students' perspectives and stigmatizing views. We predicted that completion of the mental health elective would increase students' familiarity with mental illness, thereby improving their attitude toward and beliefs about individuals with mental illness. Specifically, we believed that students who completed the mental health elective would show improvement on a measure of social distancing and stigmatization.
DESIGN
The Perspectives of Mental Health clinical elective course was offered to third-year (P3) pharmacy students at SIUE School of Pharmacy after completion of the required Psychiatry and Neurology Integrated Pharmacotherapy course. The elective was designed to provide students with further discussion about the treatment of mental illness as well as a variety of perspectives on the care of individuals with mental illness. The course used a variety of activities including: an advanced psychopharmacology overview; training in motivational interviewing; a presentation by the National Alliance on Mental Illness (NAMI) local chapter; introduction to pharmacy collaborations with peer support specialists, social workers, and psychiatrists; mock patient counseling sessions; and a required psychiatric patient interview at a local community mental health center. Psychiatric disorders discussed in this course included: schizophrenia, bipolar disorder, depression, anxiety disorders, personality disorders, and substance use/abuse disorders.
EVALUATION AND ASSESSMENT
A survey instrument was developed using previous research surrounding pharmacy student attitudes toward mental illness and was designed to measure 2 distinct features: social distance and stigmatizing views.8,9 The first section of the survey tool included questions to determine each student's social distance toward patients with mental illness. Social distance has been defined as the willingness of an individual to interact in varying degrees with patients with mental illness.16 This section included 7 statements with Likert scale responses (5 = definitely willing, 4 = willing, 3 = neutral, 2 = unwilling, and 1 = definitely unwilling). The sum of these 7 items was used as an index of overall social distance, with higher scores indicating a greater willingness to interact with patients with mental illness.
The second section of the survey instrument included questions to determine stigmatizing views held by students. Stigma is described as a negative view or attitude based on misinformation or prejudice toward someone with an illness.11 This section included 10 statements with Likert-scale responses (5 = strongly disagree, 4 = disagree, 3 = neutral, 2 = agree, 1 = strongly agree). The sum of these 10 items was used as an index of overall stigmatization, with higher scores indicating a more positive view toward individuals with a mental illness (ie, higher scores indicate lower stigmatization).
Demographic information also was gathered, including items pertaining to age, sex, political beliefs (ie, conservative, liberal, or undecided), and type of community (ie, urban or rural) where the participant spent the majority of childhood/young adulthood years, as these characteristics potentially can influence baseline views toward mental illness. Participants were asked to indicate whether they had taken any other courses that focused on mental illness. Participants also were asked to indicate whether they had ever known anyone with a mental illness, and subsequently to rate the extent to which they had been affected personally by their interaction with individuals with mental illness. A 10-point Likert scale was used with 1 indicating minimal affect and 10 indicating severe affect.
The survey instrument was administered to students enrolled in the Perspectives of Mental Health elective course in the spring semester of 2010. Simultaneously, the same survey instrument was administered to a control group of students enrolled in a different clinical elective not focused on the topic of mental illness. The survey instrument was administered at the beginning and end of the spring semester in both courses. Participation in this study was voluntary and all responses were provided anonymously.This study was approved by the SIUE Institutional Review Board.
All analyses were completed using SPSS, version 16.0. Exploratory analyses were run to determine whether the variables of interest (ie, social distance and stigmatization) were appropriate for use in parametric statistical analysis. Chi-squared analyses were used to determine whether the 2 groups were comparable with regard to demographic variables. Independent sample t tests were used for between-group comparisons to determine whether course enrollment (mental health elective versus control group) influenced student perspectives toward individuals with mental illness. Paired sample t tests were used to evaluate within-group changes in ratings that occurred between the initial survey and the follow-up survey at 15 weeks. One-way analysis of covariance (ANCOVA) was employed to evaluate the effect of group membership on social distance and social stigma ratings above and beyond individual differences measured at baseline. A 2-tailed alpha level of 0.05 was set as the criterion for statistical significance.
Twenty-two of 23 students completed both the precourse and postcourse survey instruments, for a 95.6% completion rate. Seventeen of 19 (89.5%) students in the control group completed both baseline and postcourse survey instruments.
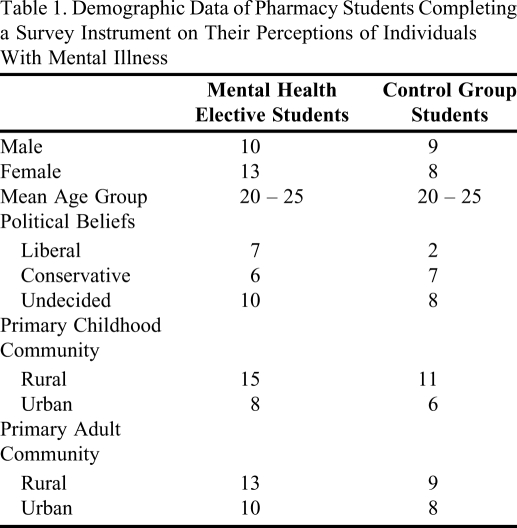
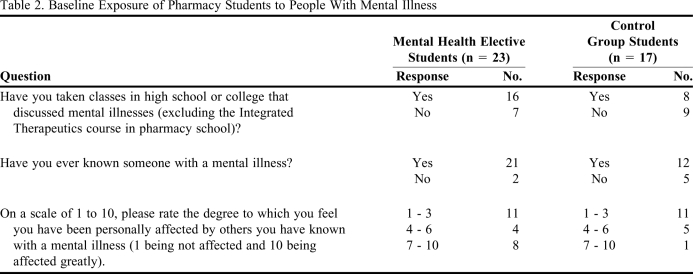
The study and control groups were comparable in age (p = 0.29), sex (p = 0.55), childhood community (p = 0.97), political beliefs (p = 0.33), previous education in mental health (p = 0.15), and previous experience with individuals with mental illness (p = 0.09). However, the 2 groups were found to be significantly different regarding the degree to which participants had been affected personally by their interactions with individuals with mental illness (p < 0.05). Individuals in the mental health elective had been more personally affected by individuals with mental illness (4.8 ± 2.9) than had individuals in the control group (2.9 ± 1.9). Tables 1 and 2 provide additional information regarding the relevant demographics and individual difference measures for the entire sample and by group.
Table 1.
Demographic Data of Pharmacy Students Completing a Survey Instrument on Their Perceptions of Individuals With Mental Illness
Table 2.
Baseline Exposure of Pharmacy Students to People With Mental Illness
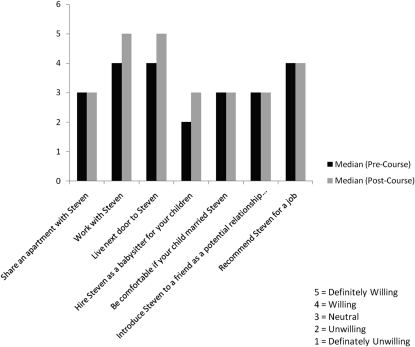
We hypothesized that the completion of the mental health elective would increase students' familiarity with mental illness, thereby improving their attitude toward and beliefs about individuals with mental illness. We predicted that, in comparison to a control group, students who completed the mental health elective would show improvement on a measure of social distancing and stigmatization. Regarding social distance, the 2 study groups were comparable in baseline ratings (p = 0.31). When comparing the ratings provided at follow-up, the 2 study groups were significantly different (p < 0.05). Within the mental health elective group, social distance ratings provided at follow-up (25.6 ± 4.9) were significantly higher than ratings provided at baseline (22.9 ± 4.6; p < 0.05). In contrast, individuals in the control group provided comparable social distance ratings at follow-up (21.7 ± 5.9) and at baseline (21.5 ± 3.6; p = 0.93).
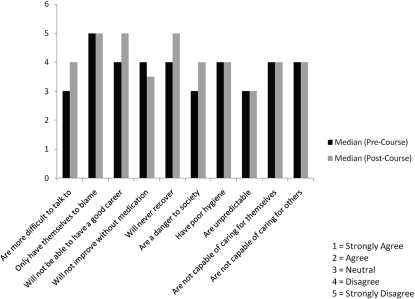
The 2 study groups were comparable in baseline ratings for stigmatization (p = 0.65). When comparing the ratings provided at follow-up, the ratings provided by the 2 study groups were significantly different (p < 0.05).Within the mental health elective group, stigmatization ratings provided at follow-up (40.1 ± 4.7) were significantly higher than ratings provided at baseline (37.1 ± 3.2; p < 0.05). In contrast, individuals in the control group provided comparable stigmatization ratings at follow-up (37.5 ± 4.5) and at baseline (36.3 ± 5.2; p = 0.38).
Given the observation at baseline that students in the mental health elective reported being more affected personally by their interactions with individuals with mental illness than did students in the control group, additional analyses were conducted to examine whether the observed changes in social distance and social stigma ratings could be better explained. One-way ANCOVAs were used to compare the 2 study groups' precourse and postcourse ratings of social distancing and social stigma, while controlling for degree of personal affect. Consistent with the results reported above, the 2 study groups were comparable in baseline ratings of social distance (p = 0.33) and social stigma (p = .47). After controlling for baseline degree of personal affect, the 2 study groups were significantly different regarding social distance (p < 0.05) and social stigma (p < 0.05).
On 3 of the 7 statements, students' perspectives improved following completion of the mental health elective (Figure 1). In the remaining 4 statements there was no change in student views. The 3 statements on which there was improvement were the students' willingness to work with, live next door to, and hire an individual with a mental illness as a babysitter for their children.
Figure 1.
Pharmacy students' responses to a scenario proposed to measure their social distance from people with mental illness. “Steven is a patient diagnosed with a mental illness. Would you…?”
In 4 of 10 statements, students' perspectives improved (less stigmatizing views were held) upon completion of the elective course (Figure 2). These statements included: patients with mental illness are more difficult to talk to; will not be able to have a good career; will never recover; and are a danger to society. Students' responses reflected a negative change in perspective on only 1 survey item: patients with mental illness will not improve without medication. Upon evaluation of the postcourse survey results, the changes in perspectives that occurred among students in the study group were not seen in students in the control group.
Figure 2.
Pharmacy students' responses to a scenario proposed to measure their stigmatizing views regarding people with mental illness. “Patients who are diagnosed with a mental illness…”
DISCUSSION
The students who participated in this survey held less stigmatizing views than those in similar studies.8 The social distance and stigmatization results in this study indicate that the pharmacy students enrolled in both the elective course and in the control group had mostly positive perceptions about patients with mental illness before participating in the study. At the end of the semester, students who had completed the mental health elective demonstrated significant and positive changes in their social distance and stigmatizing views that were not seen among students in the control group. Despite personal student experiences and exposure to mental illness prior to this elective, the reported findings suggest that the observed changes in social distance and social stigma ratings are related to completion of the mental health elective course.
Limited literature exists showing the impact of educational strategies on students' perspectives. Results of this study illustrate that enrollment and completion of a mental health elective at SIUE School of Pharmacy positively impacted pharmacy students' perspectives regarding mental illness, which is similar to findings from other studies in this area.14 Students' responses reflected a negative change in perspective on only 1 survey item: patients who are diagnosed with a mental illness will not improve without medication. This may reflect the students' pharmacy education, which is focused on medication management and pharmacotherapy. Although the clinical implications of the improvement in personal views seen in the overall survey results is unknown, having a more positive perception of patients with mental illness has the potential to enhance treatment outcomes and to build upon the therapeutic relationship between a pharmacist and patient.
Limitations of this study include the small sample size, despite the high survey response rate. The number of participants was limited to the course enrollment, capped at 30 students each year. Also, we were able to track student perspectives over only 1 semester. Following students into clinical practice after graduation would have been beneficial. A longer follow-up period has the potential to reveal how changes in perspectives translate to clinical practice, which would help reveal the clinical implications of our results. Also, as with any Likert-scale survey instrument, the survey tool introduced subjectivity to the study results. Identifying which component of the elective course had the biggest impact on students was difficult, due to the variety of student experiences. Another limitation to this study was not selecting a specific mental illness on which to focus. Social distance and stigmatizing views differ depending on the specific mental illness being discussed (eg, schizophrenia versus depression).4,9 However, we believe it would have been limiting to select a particular psychiatric illness, and by making the survey items applicable to all mental illness, our results will be more applicable to a wider range of patients.
Further studies should be completed to examine specific educational experiences within the curriculum and particular courses to determine which are most effective in influencing students' perspectives. Following these students during their experiential education clerkships and again after graduation also would be beneficial.
CONCLUSIONS
Our study showed that advanced mental health education has the potential to influence positively the perspectives of pharmacy students about mental illness. Providing quality education and experiences related to mental illness is an important part of the pharmacy curriculum. Because all pharmacists encounter patients with mental illness throughout their careers, advanced training in psychiatric medicine and mental health care exposure is vital in preparing pharmacy students to provide unbiased, patient-centered care.
REFERENCES
- 1.Compton MT, Rudisch BE, Weiss PS, West JC, Kaslow NJ. Predictors of psychiatrist-reported treatment-compliance problems among patients in routine US psychiatric care. Psychiatry Res. 2005;137(1-2):29–36. doi: 10.1016/j.psychres.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 2.Wahl OF. Mental health consumers' experience of stigma. Schizophr Bull. 1999;25(3):467–478. doi: 10.1093/oxfordjournals.schbul.a033394. [DOI] [PubMed] [Google Scholar]
- 3.Crisp AH, Gelder MG, Rix S, Meltzer H, Rowlands OJ. Stigmatization of people with mental illnesses. Br J Psychiatry. 2000;177(1):4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- 4.Phokeo V, Sproule B, Raman-Wilms L. Community pharmacists' attitudes toward and professional interactions with users of psychiatric medication. Psychiatric Serv. 2004;55(12):1434–1436. doi: 10.1176/appi.ps.55.12.1434. [DOI] [PubMed] [Google Scholar]
- 5.Vainio KK, Airaksinen M, Hyykky TT, Enlund KH. Effect of therapeutic class on counseling in community pharmacies. Ann Pharmacother. 2002;36(5):781–786. doi: 10.1345/aph.1A374. [DOI] [PubMed] [Google Scholar]
- 6.Hare SK, Kraenow K. Depression screenings: developing a model for use in a community pharmacy. J Am Pharm Assoc. 2008;48(1):46–51. doi: 10.1331/JAPhA.2008.07010. [DOI] [PubMed] [Google Scholar]
- 7.Cates ME, Burton A, Woolley TW. Attitudes of pharmacists toward mental illness and providing pharmaceutical care to the mentally ill. Ann Pharmacother. 2005;39(9):1450–1455. doi: 10.1345/aph.1G009. [DOI] [PubMed] [Google Scholar]
- 8.Volmer D, Maesalu M, Bell SJ. Pharmacy students' attitudes toward and professional interactions with people with mental disorders. Int J Soc Psychiatry. 2008;54(5):402–413. doi: 10.1177/0020764008090427. [DOI] [PubMed] [Google Scholar]
- 9.Bell JS, Johns R, Chen T. Pharmacy students' and graduates' attitudes towards people with schizophrenia and severe depression. Am J Pharm Educ. 2006;70(4) doi: 10.5688/aj700477. Article 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scheerder G, De Coster I, Van Audenhove C. Pharmacists' role in depression care: a survey of attitudes, current practices, and barriers. Psychiatric Serv. 2008;59(10):1155–1161. doi: 10.1176/ps.2008.59.10.1155. [DOI] [PubMed] [Google Scholar]
- 11.Bell JS, Aaltonen SE, Bronstein E, et al. Attitudes of pharmacy students toward people with mental disorders, a six country study. Pharm World Sci. 2008;30(5):595–599. doi: 10.1007/s11096-008-9211-x. [DOI] [PubMed] [Google Scholar]
- 12.Bell JS, Aaltonen SE, Airaksinen MS, et al. Determinants of mental health stigma among pharmacy students in Australia, Belgium, Estonia, Finland, India, and Latvia. Int J Soc Psychiatry. 2010;56(1):3–14. doi: 10.1177/0020764008097621. [DOI] [PubMed] [Google Scholar]
- 13.Zolezzi M, Blake A. Principles-based learning design for an online postgraduate psychiatric pharmacy course. Am J Pharm Educ. 2008;(5):72. doi: 10.5688/aj7205107. Article 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buhler AV, Karimi RM. Peer-level patient presenters decrease pharmacy students' social distance from patients with schizophrenia and clinical depression. Am J Pharm Educ. 2008;(5):72. doi: 10.5688/aj7205106. Article 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cates ME. Mental health and psychiatric pharmacy instruction in US colleges and schools of pharmacy. Am J Pharm Educ. 2007;(711):71. doi: 10.5688/aj710104. Article 04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lauber C, Nordt C, Falcato L, Roessler W. Factors influencing social distance toward people with mental illness. Community Ment Health J. 2004;40(3):265–274. doi: 10.1023/b:comh.0000026999.87728.2d. [DOI] [PubMed] [Google Scholar]