Abstract
Objectives
To assess Croatian community pharmacists' patient care competencies using the General Level Framework (GLF).
Methods
The competencies of 100 community pharmacists working in 38 community pharmacies were evaluated using an adapted version of the GLF.
Results
Pharmacists demonstrated the best performance in the competency areas drug specific issues and provision of drug products; the poorest performance was in the competency areas evaluation of outcomes and monitoring drug therapy. Pharmacists' behavior varied the most in the following areas: ensuring that the prescription is legal, prioritization of medication management problems, and identification of drug-drug interactions.
Conclusions
Competencies were identified that need to be developed to improve pharmacist interventions in community settings. This study provides the first data on pharmacists' performance in Croatia and serves as a starting point for future studies and actions.
Keywords: competency, pharmacist, General Level Framework, Croatia, community pharmacy
INTRODUCTION
Development of competences in pharmacy is a basic prerequisite for providing pharmacy care and being responsible for patient treatment outcomes, especially when task- and behavior-related competencies are required to deliver quality care.1 The public health role of pharmacists using evidence-based practice to ensure patient safety and the best use of medicines, including individual patient and population outcomes, has been endorsed by the World Health Organization (WHO).2
Differences exist in pharmacy practice among countries.3 Discrepancies, omissions, and inconsistencies in providing pharmaceutical care at the national level are present in many countries.4-6 Assurance of quality and higher standards in professional performance are being sought by health professionals, patients, and regulators. Ways in which healthcare services and standards for healthcare delivery can be improved are being examined in many countries, such as systems to ensure the quality of education and training for pharmacy students and the ongoing competence of practitioners.7
In recent years, efficient programs for the evaluation and development of pharmacy competencies and education models promoting increased competence have been of the utmost interest to the International Pharmaceutical Federation (FIP).8,9 One such model has been supported via the General Level Framework (GLF) in Great Britain, developed by the Competency Development and Evaluation Group (CoDEG) in 2005.10
GLF studies of postgraduate students and pharmacists employed in hospital pharmacies have been conducted in Great Britain and Australia.11,12 Research studies also have been conducted of pharmacists delivering pharmaceutical care in community pharmacies in Great Britain.13 The extrapolation of discovered patterns in community pharmacies in Croatia as a new field of investigation is presented in this study.
General Level Framework (GLF)
The General Level Framework14 is a tool that allows for the defining, measuring, and developing of professional and scientific behavioral competencies in delivering pharmaceutical care among a selected group of pharmacists. The purpose of this document is to provide guidance on a competency framework that supports the development of pharmacists as safe, effective, general level practitioners. In primary care this general level is usually related to the services delivered by pharmacists working either full time or part time, providing audit support and/or medication review services, and pharmacists working in the community. Pharmacists working as a project or team leaders may want to consider the Advanced and Consultant Level Competency Framework (ACLF), as this may be more suitable to their needs.14 The GLF allows accurate determination of a precise described meanings and level of such competencies.10,11,15
There is a strong connection between competency and performance. Multiple-choice tests, oral examinations, or essays can be used to test factual knowledge, but more sophisticated methods are needed to assess performance, including observation, objective structured clinical examinations, and role play using standardized or real patients.16
Community Pharmacy in Croatia
In Croatia, an Eastern European country with a population of 4.5 million, pharmacies are a part of the primary health care system. Some pharmacies are state-owned (20.4%), and others are owned by 1 pharmacist (27.6%), but the majority are part of pharmacy chains owned by pharmacists and/or non-pharmacists (50%).17 Although pharmaceutical care and the new role of pharmacists in health care have been promoted in Croatia over the past few decades, the primary role of community pharmacists remains supplying and dispensing drugs and compounding medicines.18
Pharmacists' licences are renewed every 6 years via the competent authority (Croatian Chamber of Pharmacists) and based mostly on points earned through attendance at organized education events. Whether the educational event is a seminar, conference, congress, or organized course, it usually involves only passive listening, and with the exception of workshops, no active role on the part of the pharmacists is required to receive credit. To renew their pharmacy/practice license, some other activities may be required such as: participating in a pharmaceutical congress, mentoring students, publishing articles, teaching, etc.19 The average Croatian pharmacist does not engaged in self-directed learning to “diagnose their learning needs, identifying human and material resources for learning, formulating goals, choosing and implementing appropriate learning strategies, and evaluating learning outcomes.”20 Neither documenting consultations nor professional work is obligatory in the portfolio of a graduate pharmacist, so pharmacists' professional work cannot be assessed from written documents. Pharmacists in Croatia are not required to keep a learning portfolio and it is not a part of the licensing process yet. In countries like Croatia, development of an alternate evaluation system for assessing competencies is crucial. Since pharmaceutical care competencies in community pharmacy have previously not been tested, this study was conducted to assess current competencies among community pharmacists in Croatia.
METHODS
Instrument Validation
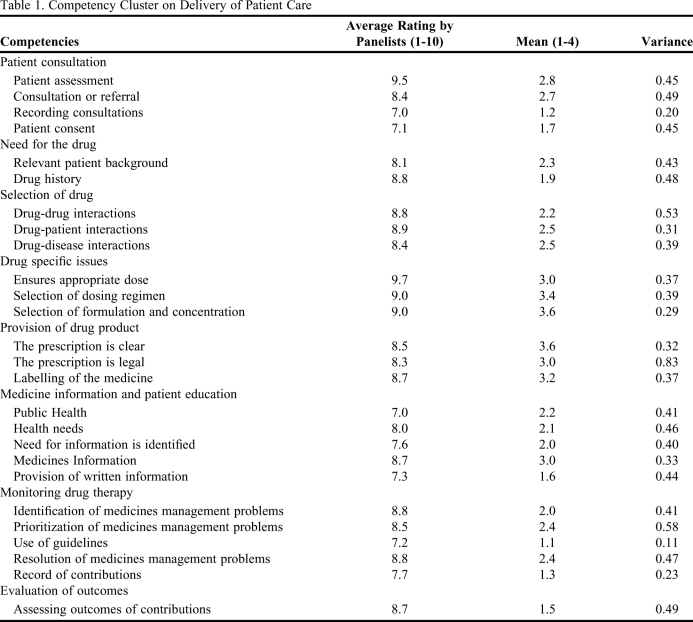
The GLF contains a detailed description of actions, skills, and knowledge that should be applied by a pharmacist in delivering competent pharmaceutical patient care. There are 4 competency clusters: delivery of patient care, problem-solving competencies, personal competencies, and management and organization competencies. The cluster Delivery of Patient Care, which comprises 8 different competencies (Table 1), was chosen by researchers and the expert panel group as the first one to use in scanning community pharmacists' professional performance in Croatia. Each of these competencies has 26 statements, known as behavioral statements, which define that competency (Table 1). All stated competencies can be evaluated through a monitoring method, ie, observation of performance in real situations involving the delivery of pharmaceutical care.
Table 1.
Competency Cluster on Delivery of Patient Care
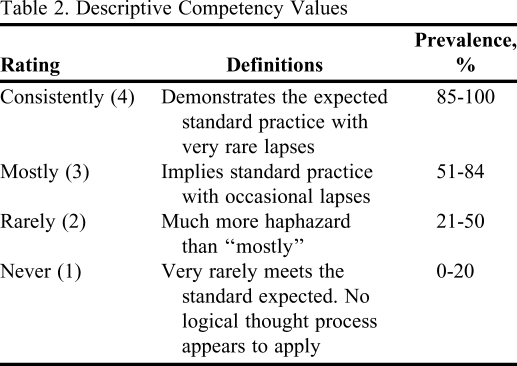
Competence is defined as the ability to carry out a job or task, whereas ability based on observed behavior is usually referred to as competency. In pharmaceutical practice, 1 the pharmacist's ability to do the job is the key area to be assessed.21 Behavior-related competencies are required to show a certain level of performance and deliver quality care to the patient.22 The level to which a pharmacist possesses the behavior described in each of the behavioral statements is validated by conducting an assessment, and rating the pharmacist's performance based on 4 different descriptive values assigned numbers from 1 to 4. In this way, an assessment rating for the pharmacist (Table 2) is obtained.
Table 2.
Descriptive Competency Values
For the purpose of this study, GLF was used to evaluate the patient care competencies of community pharmacists and to enable their further development. The delivery of patient care cluster was selected for this study. Based on self-reports from community pharmacists prior of this study and the lack of continuing education available for this area, we assumed that most of the pharmacists in Croatia were deficient in most of the competency areas on providing patient care. No patient-oriented continuing education courses existed in Croatia until 2006, and pharmaceutical care was not added in to the curricula until September 2009.
In Croatia, there are 2773 working community pharmacists registered by the Croatian Chamber of Pharmacists.23 Of these, 70% are employed in community pharmacies, 5% in hospital pharmacies, and the rest in industry and representative offices (11%), wholesale (5%), education (4%), health institutions (3%), and other (2%).22 Approximately 92.% of registered pharmacists in Croatia are female. Approximately 2-3 pharmacists work in each community pharmacy in Croatia. 23
To adapt the GLF for the Croatian setting, a double translation method was used, meaning that every item in English was translated into Croatian and then back-translated into English.24 Four translators were used and the translations most closely fitting the original questions were chosen. A panel of experts was used to validate the content.
A combination of the Delphi and nominal group process methods was employed.25 The 10-panel members chosen represented primary care, academia, policymakers, and public health, and included a sociologist and a psychologist. The competency framework was distributed to panel members by e-mail. Panel members were asked to provide written feedback on each competency and to grade the level of each behavioral statement on a 0-10 scale to determine the importance to patient care in community pharmacy in Croatia. Replies were collected and open-ended comments collated.
Anonymity of responses was maintained. Next, the panel met. Before the main score was calculated, all the behavioral statements were rated: above 1.0-3.0 indicated the behavioral statement was not relevant to community pharmacy practice in Croatia; 4.0-6.0 indicated the behavioral statement may or may not be relevant to community pharmacy practice in Croatia; and 7.0-10.0 indicated the behavioral statement was relevant to community pharmacy practice in Croatia. The mean score of each behavioral statement then was calculated (Table 1). All behavioral statements were rated above 7.0, so all were kept for further discussion.
Other than minor changes to formatting and wording, the panel approved all of the behavioral statements as written. Moreover, the criteria for evaluation of particular behavioral statements in pharmacists in Croatia were discussed and defined by the expert panel.
Pilot Study
The adopted framework was pilot tested with a sample of 10 pharmacists in 3 different pharmacies. The 3 assessors were all pharmacists with practice experience, education, and training, and all members of the research team.
The assessments for the pilot test were conducted in 1 visit through structural observation of participants in community pharmacies during regular working hours (shadowing14), using the behavioral statement checklist and a rating scale. This option was used because the assessors did not have the opportunity to observe the pharmacists' daily practice; hence, making arrangements to accompany the pharmacist in their work was required. No video or audio taping was used. Some interaction between the assessors and participants occurred, but it was limited (unless there was an issue of patient care to resolve). Feedback was reserved until the assessment was completed.
A consensus was reached by the assessors through the following process: the same pharmacist was assessed by all of the assessors at the same time. The performance of the pharmacist was evaluated by the main assessor, using a 1-4 scale to rate the 26 behavioral statements in the framework. The same process was followed by the control assessors. The data were compared, differences in ratings were discussed, and a final rating was made. Because the differences in the assessors' ratings were minor and easily reconsidered by all 3 assessors, no changes were made to the assessment process as a result of the pilot study. The data for the 10 pharmacists in the pilot study were included in the main study.
Description of Participants and Evaluation Process
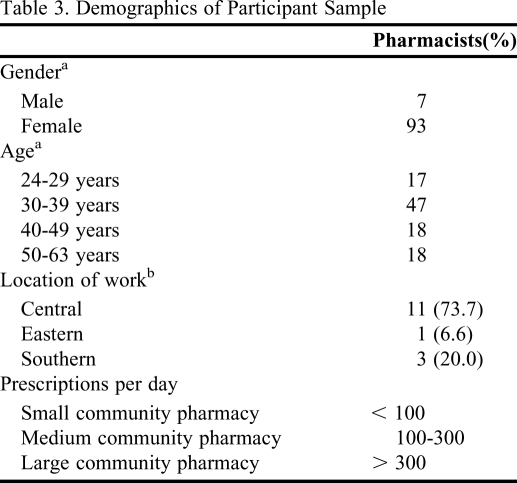
The 10 pharmacists in the pilot study and the other 90 participants in the main study worked in 38 community pharmacies that were part of Croatia's largest pharmacy chain, Atlantic Farmacia. This pharmacy chain was selected as its pharmacies had the sufficient diversity needed for this study. The 38 pharmacies ranged from small to large and were situated in different regions and in small and large towns throughout Croatia (Table 3).
Table 3.
Demographics of Participant Sample
a n=100
b n=15
The other 90 participants were evaluated by 1 assessor, the main researcher, who observed each of the pharmacists during regular working hours, as described above for the pilot project. The study was conducted over 3 months (March 2009-June 2009). Ethical approval was obtained from the Company Health Department Ethical Committee and written informed consent to participate was signed by all participants. Participation in the study was optional, but none of the pharmacists declined or asked that their data be excluded from the study. Participants were assured that confidentiality and anonymity would be maintained, and reassured that their employer would not have access to individual pharmacists' assessments. Although an employee of the company, the main assessor did not have an executive role or vertical type of authority over the participants.
There were occasions during the assessments when there were not enough patients in the pharmacy for the pharmacist to demonstrate a particular patient care behavior. In these circumstances, a hypothetical scenario was constructed by the assessor. The assessment was then based on the participant's response. Following instructions from the GLF original document,14 this alternative means of assessment had to be used most often in small pharmacies with an average of 3-4 assessment items per participant. The time needed for each evaluation varied depending on the number of patients coming into the pharmacy, but the average time required for each pharmacist assessment was 3 hours.
When the observation was complete, the assessor recorded a rating (1-4) for each of the 26 behavioral statements. The assessors immediately informed the pharmacists of their performance ratings. An assessor asked the pharmacist to confirm the level of every behavioral statement before the final rating. The assessors made only a few changes and these were limited to the following behavioral statements: drug history, drug-drug interactions, and recording consultation. The participants' agreement with the assessments was not measured, but their agreement was necessary to ensure the pharmacists' improvement on behavioral statements in the future.
Data were analyzed using SPSS, version 14 (SPSS, Inc, Chicago, IL). Descriptive statistics were used to report community pharmacists' behavioral statement measured by the framework. Results were subjected to frequency analysis, or cross tabulation with chi-square analysis, as appropriate.
RESULTS
Of the 100 pharmacists who participated in the study, 93% were female. Four percent held a postgraduate degree (specialization, master of science, or doctor of philosophy) or were still studying to obtain that degree. Fifteen towns, spread across central, eastern, and southern Croatia, were included in the geographic area of study, with 64% accounting for the Zagreb region, which is representative of the country profile (Table 3). Community pharmacies were divided by size into small (up to 100 prescriptions per day), medium (100-300 prescriptions per day), and large (more than 300 prescriptions per day), with more than half of the selected participants practicing in medium-sized community pharmacies (53%).
Participants performed best in the following behavioral areas: drug specific issues and provision of drug product competencies; selection of formulation and concentration; ensuring that the prescription is clear; selection of dosing regimen; labelling of the medicine; and ensuring appropriate dose (Table 1). The poorest performance was in the following patient care areas: evaluation of outcomes; monitoring drug therapy; use of guidelines; recording consultations and interventions; assessing outcomes of contributions; provision of written information; and obtaining patient consent (Table 1). Recording consultations and contributions was rare among the pharmacists observed, with only 25.6% of pharmacists taking notes, and then only rarely.
Assessment results for the delivery of patient care competency clearly showed the areas pharmacists are good at, but more importantly areas which need to be developed. A relationship was found between the size of the community pharmacy and the behavioral statement of ensuring that the prescription is clear, unambiguous, and legal, with participants working in medium and large community pharmacies more likely to ensure the legality of the prescription than their colleagues working in small ones (χ2 =13.1, p = 0.011). The highest variance in pharmacists' behavior was observed in the following areas: ensuring that the prescription is legal; prioritization of medicine management problems; identification of drug-drug interaction; assessing outcomes of interventions (contributions), consultation, or referral; taking drug history; and resolution of medicine management problems (Table 1).
DISCUSSION
Since the competence of Croatian community pharmacists previously had not been tested, the primary objective of this study was to assess the level of delivery of patient care competencies. By using GLF, the Global Pharmacy Education Action Plan has been joined to gather data in country studies on educational needs and competency assessment strategies. This Action Plan was developed by the Pharmacy Education Taskforce, established by FIP in association with the United Nations Educational, Scientific and Cultural Organization (UNESCO), and the World Health Organization (WHO) in 2007.9
The high mean value of the pharmacist behavioral statement evaluation associated with a selection of medicine form and concentration, dosage, and labeling was expected. During observation through assessments, the fact that pharmacists spend the majority of their work time in these activities was clearly noticed by the research team. Consequently, these behavioral statements have strongly been developed by these community pharmacists but limitations are present in Croatia in terms of a selection of medicine formulation. Acts by which a pharmacist also is limited or occasionally disabled to make his/her selection are adopted by the regulatory authorities.
The low mean assessment rating for the behavioral statement Use of Guidelines also was expected, as few therapeutic guidelines are available in the Croatian language, and those which circulate are recently dated and still not recognized by pharmacists. Also, education in the use of guidelines in pharmaceutical practice is not a part of formal pharmacy education in Croatia, and, other than written instructions, no education has been conducted among practicing pharmacists on how to use guidelines.
Documentation of pharmaceutical care in Croatia is not obligatory, and there are no official forms or computer programs that support this type of pharmaceutical care. Data on the impact of documenting clinical interventions has been shown in studies that favor the significance of documenting consultations.26 They have a significant impact on optimizing drug regimens and improving adherence to standards of care practices.27 The participants were challenged and encouraged by the company to document their work by keeping a portfolio.
One of goals of this study was to determine which behavioral statement levels vary among individual pharmacists. This information will serve for development of standard operating procedures (SOP) for delivering pharmaceutical care with specially detailed instructions provided for those procedures with the highest variance in performance. Large aberrations in levels of some behavioral statements, such as ensuring the prescription is legal, priority of medicine managing problems, resolution of medicine managing problems, assessing outcomes of contribution, identification of drug-drug interaction, and patient consent indicate the lack of SOPs in this domain and legal doubts. There are currently no official SOPs in the Croatian health system. However, an incentive to develop such procedures has been presented by the Croatian Chamber of Pharmacists. Development of a system in which these procedures can be evaluated and in which failure to adhere to them can have consequences on the professional status of pharmacists is important.
The most comprehensive variance and a mean assessment below 2.5 were comprised in behavioral statements that refer to medical interventions (Priority and Resolution of Medicine Managing Problems, Assessing Outcomes of Contributions). Since responsibility for the patient treatment outcome is assumed in pharmaceutical care, the high mean in these behavioral statements should be included in that process, especially in Assessing Outcomes of Contribution. Often, practices do not receive the feedback on patient outcomes. The reason for this is the varying levels of compliance by doctors and specialists, not all of whom feel positive about the involvement of pharmacists in pharmacotherapy. If pharmacists want to be recognized as an important link in the process of patient care, these competencies should be developed to the level of being recognizable by patients. Every licensed practicing pharmacist should be capable of determining priorities in treatment; observing and correcting irregularities such as polypharmacy, interactions, overdoses, and therapy inefficiency; and initiating resolution of drug-related problems, with the patient's informed consent.
Some pharmacists never develop these competencies because they feel they are unnecessary and that all responsibility for patient treatment rests in the hands of physicians. Additionally, regulatory surveillance authorities were rarely used to sanction the pharmacists' aberrations. During assessment, some pharmacists expressed lack of motivation for developing some competencies because patients cannot be charged for the additional services; thus, following the path of least resistance and taking a minimalist approach was often mentioned.
It is considered risky that the highest variance was shown for the behavioral statement the Prescription Is Legal. In that way, the pharmaceutical care provided at different pharmacies is inconsistent and impairs patients' trust in pharmacists. Moreover, compliance with professional guidelines is decreased as by their own admission, pharmacists act differently when pressured by patients or supervisors.
The illegal prescriptions found were: older than 12 months, were written without the original stamp or facsimile of the prescriber, did not include the full dosage regimen, or did not have the patient's name. Also, a few cases of dispensing medicines without a prescription were recorded, which was common behavior for some participants.
Identification of Interactions also is an important domain in which a key role should be played by the regulatory authority in terms of SOPs regarding sources of information, permitted interventions, and mechanisms for controlling the selection of prescribed drugs. Besides literature data on drug interactions themselves, 28 participants in our study believed that they needed to complete educational programs to be able to evaluate the clinical significance of potential interactions. They felt they not only should be capable of intervening when a clinically significant interaction was observed but they also should be able to make evidence based decisions when a potential interaction was noticed by a patient in the patient information leaflet.
This study has several strengths. An expert panel was formed to clarify in the Croatian language the basic and professional terms used in the study - something that had not been done previously. Moreover, the significance of behavioral statements in community pharmacy was evaluated for the first time in Croatia. In this way, key competencies were discussed in several meetings, and certain dilemmas regarding language barriers and differences in social environment in relation to the original text were clarified.
The study limitations are related to this being the first time that this type of investigation was conducted in Croatia, so some pharmacists felt uncomfortable, which surely resulted in some deviations from their regular behavior. Consequently, after the assessment process was finished, the results were presented to all participants in the Company Education Centre.
Some limitations of the study were in relation to participants' comments such as the lack of user programs for interaction observation. Other limitations were limited computer access, crowds in the pharmacy during competency testing and momentary absence of another pharmacist.
No significant differences were demonstrated in the assessment of a particular behavioral statement regarding the age and sex of a pharmacist, or regarding the size of the pharmacy, except in the behavioral statement ensuring the prescription is legal, where the lowest mean of behavioral statement was shown by pharmacists working in small pharmacies. Those prescriptions usually were prescribed by only one doctor, without any possibility to influence prescriber's usual prescribing modality.
Using virtual cases in the assessment process also could be considered a limitation. Disadvantages related to the use of virtual cases can be: the “textbook” scenarios may not reflect real-life situations, they may not allow assessment of complex skills, and participants may be less focused on solving virtual cases due to lack of empathy. There also are some advantages related to the use of virtual cases, including control and safety, feedback from the assessor (simulators), questions can be tailored to level of skill to be assessed, the patient scenario is uniform across participants.29
Because the data were collected during a 3-month period, pharmacists who participated early in the assessment may have passed on information to those who had not participated yet and this may have influenced their performance. Nevertheless, because the researcher assessed each pharmacist's performance based on unique, real-life patient situations that were not predictable, and posed questions to the pharmacist related to those situations, possible sharing of information among the participants was not considered a serious limitation.
The GLF was presented to participants as an evaluation instrument as well as an educational tool that could support their competency development in the future. We conducted this investigation in response to the 2006 World Health Report, which specifically has called for an individual approach to pharmacists' education and for investigating possibilities for the development of education programs for health care professionals.30 Therefore, there are initiatives in Croatia for developing an education program to teach pharmacists how to document their individual professional performance in a pharmacist's portfolio.
A pharmacist's performance is a clear indicator of professional competency, which in turn has a direct influence on patients' outcome and safety.31 Clarity of standards, personal control, and professional duty is significantly related to pharmacist responsibility for drug therapy outcomes.32 In order to improve their patient's health, pharmacists need to be competent in their daily work, regardless of the practice setting, country, or culture.33
CONCLUSIONS
We identified competencies that Croatian pharmacists need to develop to improve their interventions in community settings. Pharmacists need to improve in the following areas: monitoring drug therapy, patient consultation, and the evaluation of outcomes. Documenting pharmacy interventions and developing forms, templates, or computer programs to record them is essential. The greatest discrepancies among pharmacists were found in ensuring that the prescription is legal, prioritizing medicine management problems, and identifying drug-drug interactions, indicating the lack of SOPs in this area. A need to develop frameworks for collection of relevant patient background data and to provide more written information for patient safety was apparent from our findings. Pharmacists' best performance was in Drug Specific Issues and Provision of Drug Product competencies. The first data on pharmacist performance and current conditions in community pharmacy in Croatia are provided in these findings, and thus they serve as a starting point for future investigations and activities.
REFERENCES
- 1.McRobbie D, Webb D, Bates I, Wright J, Davies J. Assessment of clinical competence: designing a competence grid for junior pharmacists. Pharm Educ. 2001;1:67–76. [Google Scholar]
- 2.Developing Pharmacy Practice: A Focus on Patient Care [handbook] Geneva: World Health Organization and International Pharmaceutical Federation; 2006. [Google Scholar]
- 3.IMS Pharmaceutical Pricing & Reimbursement 2007. Concise Guide Series: Central & Eastern Europe, Western Europe. London: IMS Health; 2007. [Google Scholar]
- 4.Nickerson A, MacKinnon NJ, Roberts N, Saulnier L. Drug-therapy problems, inconsistencies and omissions identified during a medication - reconciliation and seamless care service. Health Care Q. 2005;8:65–72. doi: 10.12927/hcq..17667. [DOI] [PubMed] [Google Scholar]
- 5.Bergheim CM, Hudson S, Fenelon C, Loennechen T. Glasgow: University of Strathclyde; 2008. Clinical audit of structured pharmaceutical care plans recorded within a hospital pharmaceutical care service. [Google Scholar]
- 6.Taskforce on a Blueprint for Pharmacy. Blueprint for Pharmacy:The Vision for Pharmacy. Ottawa: Canadian Pharmacists Association; 2008. [Google Scholar]
- 7.Rouse M. A Global Framework for Quality Assurance of Pharmacy Education. Geneva: International Pharmacy Federation; 2008. [Google Scholar]
- 8.Anderson C, Bates I, Beck D, et al. FIP roundtable consultation on pharmacy education: developing a global vision and action plan. Int Pharm J. 2006;20(2):12–13. [Google Scholar]
- 9.Anderson C, Bates I, Beck D, et al. Action! Update on the global pharmacy education consultation. Int Pharm J. 2008;22(1):6–8. [Google Scholar]
- 10.Mills E, Farmer D, Bates I, Davies JG, Webb D, Mc Robbie D. Development of an evidence led competency framework for primary care and community pharmacists. Pharm J. 2005;275:48–52. [Google Scholar]
- 11.Antoniou S, Webb DG, McRobbie D, Davies JG, Wright J, Quinn J, Bates IP. A controlled study of the general level framework: results of the South of England competency study. Pharm Educ. 2005;5:201–207. [Google Scholar]
- 12.Coombes I. A Competency Framework for Pharmacy Practitioners to Provide Minimum Standard of Pharmaceutical Review - The General Level Framework Handbook. 2nd ed. Safe Medication Practice Unit Queensland Health. Adapted from NHS London and South East - CoDEG, Herston; 2009. [Google Scholar]
- 13.Laaksonen R, Mills E, Duggan C, Davies JG, Bates I, Mackie C. The effect of training and service provision on the self-assessed competence of community pharmacists. Int J Pharm Pract. 2007;15(2):141–147. [Google Scholar]
- 14.2nd ed. London: CoDEG; 2007. Competency Development Evaluation Group, GLF – General Level Framework. A Framework for Pharmacist Development in General Pharmacy Practice. [Google Scholar]
- 15.Mills E, Farmer D, Bates I, Davies G, Webb DG. The General Level Framework: use in primary care and community pharmacy to support professional development. Int J Pharm Pract. 2008;16:325–331. [Google Scholar]
- 16.Wass V, Van der Vleuten C, Shatzer J, Jones R. Assessment of clinical competence. Lancet. 2001;(9260)(357):945–949. doi: 10.1016/S0140-6736(00)04221-5. [DOI] [PubMed] [Google Scholar]
- 17.Croatian Chamber of Pharmacists. Registry of Community Pharmacies. Zagreb: 2009. [Google Scholar]
- 18.Zagreb: Croatian Government, Ministry of Health; 2006. Proposal of National Strategy in Developing Health System in Croatia 2006-2011. [Google Scholar]
- 19. Regulation on continuing education. Zagreb. Croatian Chamber of Pharmacists. June 2010.
- 20.Knowles M. Andragogy in Action, Applying Modern Principles of Adult Learning. 1st ed. San Francisco, CA: Jossey-Bass; 1985. [Google Scholar]
- 21.Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65:S63–S67. doi: 10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 22.Rethans JJE, Sturmans F, Drop R, et al. Assessment of the performance of general practitioners by the use of standardized (simulated) patients. Br J Gen Pract. 1991;41:97–99. [PMC free article] [PubMed] [Google Scholar]
- 23.Register of pharmacist. Zagreb: Croatian Chamber of Pharmacists; 2010. [Google Scholar]
- 24.Jones J, Hunter D. Consensus methods for medical and health services research. Br Med J. 1995;311(7001):376–380. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bowling A. Berkshire, UK: Open University Press; 2001. Research methods in health: investigating health and health services. [Google Scholar]
- 26.Meštrović A. Pharmacist's portfolio – written record of pharmaceutical care and competence development. Zagreb. Farm glasnik. 2010;66(8):403–405. [Google Scholar]
- 27.DiVall M, Zikaras B, Copeland D, Gonyeau M. School-wide clinical intervention system to document pharmacy students' impact on patient care. Am J Pharm Educ. 2010;74(1) doi: 10.5688/aj740114. Article 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vrhovac B, Reiner Z, Francetic I, et al. Reference Book of Pharmacotherapy. 5th ed. Zagreb: Medicinska naklada; 2007. p. 837. [Google Scholar]
- 29.Wallace J, Rao R, Haslam R. Simulated patients and objective structured clinical examinations:review of their use in medical education. Adv Psychiatr Treatment. 2002;8(5):342–348. [Google Scholar]
- 30.The World Health Report 2006 – Working Together for Health. Geneva: World Health Organization; 2006. [Google Scholar]
- 31.Newton D, Boyle M, Catizone AC. The NAPLEX – evolution, purpose, scope and educational implications. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720233. Article 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Planas GL, Kimberlin CL, Segal R, Brushwood DB, Hepler DC, Schlenker RB. A pharmacist model of perceived responsibility for drug therapy outcomes. Soc Sci Med. 2005;60(10):2393–2403. doi: 10.1016/j.socscimed.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 33.Bruno A, Bates I, Brock T, Anderson C. Towards a global competency framework. Am J Pharm Educ. 2010;74(1) doi: 10.5688/aj740356. Article 3. [DOI] [PMC free article] [PubMed] [Google Scholar]