Case Presentation
A 30-year-old female without structural heart disease was referred for electrophysiology study after 4 years of palpitations not controlled with medications. Baseline sinus cycle length was 765 ms, atrial-His (AH) interval 65 ms, and Hisventricular (HV) interval 46 ms. Atrial extrastimulus testing revealed evidence of antegrade dual AV nodal physiology with AH jump of 190 ms from 600/350 ms to 600/340 ms, but no sustained tachycardia. With infusion of isoproterenol, a regular, sustained, narrow-complex tachycardia, cycle length 340 ms, was repeatedly induced by atrial extrastimulus testing. Septal VA time was less than 50 ms, during and after spontaneous development of right-bundle-branch-block aberrancy. His-refractory premature ventricular extrastimuli did not affect the tachycardia. After cessation of overdrive ventricular pacing, the tachycardia continued with a V–A–V response, and the postpacing interval was 160 ms greater than tachycardia cycle length.
With these observations, a diagnosis of typical slow-fast AV nodal reentrant tachycardia (AVNRT) was made, and slow pathway modification was performed with radiofrequency (RF) catheter ablation anterior to the coronary sinus (CS) ostium. After slow junctional beats were observed during ablation, isoproterenol was again infused and testing was repeated. At this point, a second tachycardia was repeatedly induced by atrial and ventricular extrastimulus testing (Fig. 1). Ventricular overdrive pacing was performed at slightly faster than the shorter of the two R–R intervals during tachycardia (Fig. 2), resulting in termination of the tachycardia. Spontaneous change in the AV relationship was observed after cessation of isoproterenol infusion (Fig. 3).
Figure 1.

Intracardiac tracings of a regularly irregular narrow-complex tachycardia with QRS alternans and cycle length alternans. Cycle length variability results from alternating VA intervals. HIS = His bundle catheter; P = proximal; D = distal; CS = coronary sinus catheter.
Figure 2.

Diagnostic maneuver performed during tachycardia. During an attempt to entrain the tachycardia, ventricular pacing was performed at a rate slightly faster than the tachycardia's shorter cycle length. Tachycardia continues, but no effect on atrial cycle length was observed. After a few paced beats, the tachycardia terminates. HIS = His bundle catheter; P = proximal; D = distal; CS = coronary sinus catheter; RVA = RV catheter.
Figure 3.
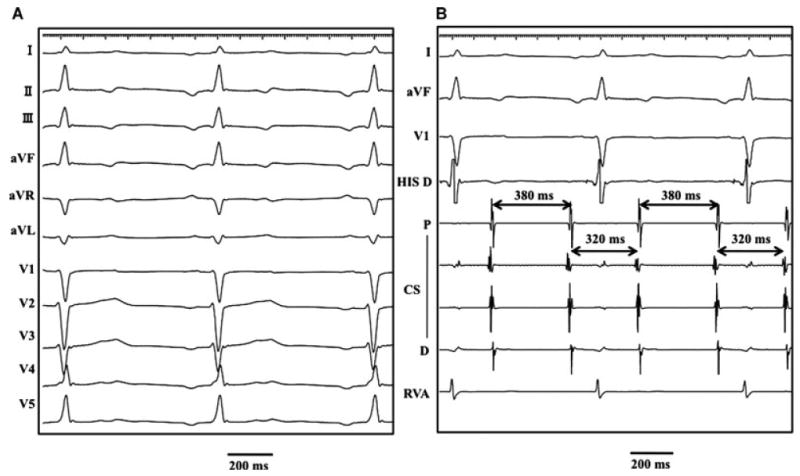
(A) Surface electrocardiogram of the second tachycardia after isoproterenol infusion stopped. 2:1 AV relationship is present. A–A intervals show cycle length alternans, while V–V intervals are constant. (B) Surface and intracardiac tracings of the same tachycardia depicted in A. 2:1 AV relationship is seen. HIS = His bundle catheter; P = proximal; D = distal; CS = coronary sinus catheter; RVA = RV catheter.
What is the most likely mechanism of this arrhythmia?
Commentary
The following pertinent findings are seen in Figure 1.
The tachycardia shows beat-to-beat variation in the RR interval (280 ms then 350 ms), with alternating QRS morphology.
The AV interval does not vary significantly, but the VA interval alternates between 140 ms and 210 ms, accounting for nearly all of the difference in the RR interval.
Atrial activation is similar in each beat, with earliest site near the coronary sinus ostium.
The differential diagnosis for this narrow-complex tachycardia includes a regularly irregular atrial tachycardia, orthodromic AV reciprocating tachycardia (AVRT) using 2 distinct retrograde accessory pathways,1 and atypical AVNRT with multiple retrograde AV nodal pathways. Another possibility is reentrant tachycardia with a single retrograde pathway (nodal or extranodal) displaying pronounced decremental conduction. In this case, oscillatory VA conduction time could result from each short VV interval causing slower retrograde conduction on the subsequent beat.
His-refractory ventricular extrastimuli failed to advance atrial activation, which does not rule out any mechanism of tachycardia. Ventricular overdrive pacing resulted in termination of the tachycardia without depolarizing the atria, excluding atrial tachycardia (Fig. 2). This maneuver also dissociated ventricular from atrial activation during tachycardia, excluding AVRT.
Confirmatory evidence was seen after isoproterenol infusion was stopped and the arrhythmia was reinduced, this time with ventricular cycle length 700 ms and a 2:1 AV relationship (Fig. 3A,B). Intracardiac recordings revealed similar atrial activation at a slower rate, with AA interval oscillating between 320 and 380 ms. Conduction block occurred at the level of the lower common pathway; no His bundle electrogram was recorded on the nonconducted beats. This is likely the same tachycardia with a different cycle length, due to less pronounced effect of isoproterenol. The lack of 1:1 AV relationship rules out orthodromic AVRT, and therefore atypical AVNRT is the most likely diagnosis. After further RF application in the slow pathway region, no tachycardia was inducible, with or without isoproterenol infusion.
Although the most common mechanism of irregular supraventricular tachycardia is atrial tachycardia, irregular variants of reentrant AVRT and AVNRT have been described. Orthodromic AVRT in patients with dual AV nodal physiology can result in oscillating cycle length due to alternating slow and fast AV nodal antegrade conduction.2 Less common is AVNRT with at least 3 distinct functional pathways, 1 retrograde and 2 antegrade, resulting in alternating fast and slow AV nodal antegrade conduction.3 In one study, 2% of 364 AVNRT cases showed significant variations in tachycardia cycle length, resulting from variable antegrade conduction and Wenckebach periodicity in the lower common pathway.4
The present case is unusual in several respects. First, alternating QRS morphology is more frequently seen in AVRT than in AVNRT,5 although it has been described in both arrhythmias.6 In this case, QRS changes were associated with cycle length oscillation, which may have altered ventricular geometry due to differential filling. Alternatively, conduction block in the His-Purkinje system may have resulted in an atypical left bundle-branch-block pattern on alternate beats. Second, beat-to-beat variation in cycle length during AVNRT usually results from changes in antegrade conduction, not retrograde conduction as shown here.7 Third, in most cases it is difficult to definitively establish whether the retrograde limb is within or outside the AV node, but here the observations of 2:1 AV relationship during tachycardia and VA dissociation during overdrive pacing rule out AVRT and establish AVNRT as the mechanism. However, it must be pointed out that this arrhythmia arose only after ablation, which may have modified the conduction properties of retrograde slow AV nodal fibers and resulted in the observed pattern of VA alternans.
Acknowledgments
Supported by American Heart Association, National Affiliate (grant number 0430287N) and the NHLBI, R01HL084261 grants to Dr. Shivkumar.
References
- 1.Buch E, Nakahara S, Shivkumar K. Diagnostic maneuver during narrow-complex tachycardia: What is the arrhythmia mechanism? Heart Rhythm. 2009;6:716–717. doi: 10.1016/j.hrthm.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Csanadi Z, Klein GJ, Yee R, Thakur RK, Li H. Effect of dual atrioventricular node pathways on atrioventricular reentrant tachycardia. Circulation. 1995;91:2614–2618. doi: 10.1161/01.cir.91.10.2614. [DOI] [PubMed] [Google Scholar]
- 3.Tai CT, Chen SA, Chiang CE, Lee SH, Chiou CW, Ueng KC, Wen ZC, Chen YJ, Chang MS. Multiple anterograde atrioventricular node pathways in patients with atrioventricular node reentrant tachycardia. J Am Coll Cardiol. 1996;28:725–731. doi: 10.1016/0735-1097(96)00217-3. [DOI] [PubMed] [Google Scholar]
- 4.Otomo K, Nagata Y, Uno K, Fujiwara H, Iesaka Y. Irregular atypical atrioventricular nodal reentrant tachycardia: Incidence, electrophysiological characteristics, and effects of slow pathway ablation. Heart Rhythm. 2007;4:1507–1522. doi: 10.1016/j.hrthm.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 5.Arya A, Kottkamp H, Piorkowski C, Schirdewahn P, Tanner H, Kobza R, Dorszewski A, Gerds-Li JH, Hindricks G. Differentiating atrioventricular nodal reentrant tachycardia from tachycardia via concealed accessory pathway. Am J Cardiol. 2005;95:875–878. doi: 10.1016/j.amjcard.2004.12.020. [DOI] [PubMed] [Google Scholar]
- 6.Maury P, Raczka F, Piot C, Davy JM. QRS and cycle length alternans during paroxysmal supraventricular tachycardia: What is the mechanism? J Cardiovasc Electrophysiol. 2002;13:92–93. doi: 10.1046/j.1540-8167.2002.00092.x. [DOI] [PubMed] [Google Scholar]
- 7.Richter S, Duray G, Israel CW, Groenefeld G, Hohnloser SH. Beat-to-beat cycle length variation during narrow QRS complex tachycardia: What is the mechanism? Pacing Clin Electrophysiol. 2005;28:1317–1319. doi: 10.1111/j.1540-8159.2005.00273.x. [DOI] [PubMed] [Google Scholar]


