Abstract
Objective
This article reports findings from a one-year longitudinal study examining the impact of change in PTSD symptoms following combat deployment on National Guard soldiers’ perceived parenting, and couple adjustment one year following return from Iraq.
Method
Participants were 468 Army National Guard fathers from a Brigade Combat Team (mean age 36 years; median deployment length 16 months; 89% European American, 5% African American, 6% Hispanic American). Participants completed an in-theater survey one month before returning home from OIF deployment (Time 1), and again, one year post-deployment (Time 2). The PTSD Checklist-Military Version (PCL-M; Weathers, Litz, Herman, Huska, & Keane, 1993) was gathered at both times, and two items assessing social support were gathered at baseline only. At Time 2, participants also completed self-report measures of parenting (Alabama Parenting Questionnaire—Short Form; Elgar, Waschbusch, Dadds, & Sigvaldason, 2007), couple adjustment (Dyadic Adjustment Scale-7; Sharpley & Rogers, 1984; Spanier, 1976), parent-child relationship quality (4 items from the Social Adjustment Scale-Self Report; Weissman & Bothwell, 1976), alcohol use (Alcohol Use Disorders Identification Test; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001), and items assessing injuries sustained while deployed.
Results
Structural equation modeling analyses showed that increases in PTSD symptoms were associated with poorer couple adjustment and greater perceived parenting challenges at Time 2 (both at p<.001). Furthermore, PTSD symptoms predicted parenting challenges independent of their impact on couple adjustment.
Conclusions
Findings highlight the importance of investigating and intervening to support parenting and couple adjustment among combat-affected National Guard families.
Keywords: parenting, couple adjustment, military personnel, posttraumatic stress symptoms
The current conflicts in Afghanistan (Operation Enduring Freedom; OEF) and Iraq (Operation Iraqi Freedom; OIF) have resulted in the highest rates of military troop mobilization and deployment since the Vietnam War, with an unprecedented reliance on National Guard/Reserve (NG/R) troops. Combat deployment is particularly stressful for NG/R “civilian soldiers,” who tend to be older, partnered with dependent children and less prepared for prolonged separations from family than active duty service members (Browne et al., 2007). Moreover, NG/R troops appear to be at risk for post-deployment mental health problems: a large-scale screening of service members returning from OIF revealed self-reports of mental health problems (depression, PTSD, and relationship problems) among NG/R troops (42.4%) to be more than double those of active duty service members (20.3%). Moreover, rates of positive screening for PTSD symptoms more than doubled among NG/R soldiers between immediate post-deployment screening (12.7%) and re-evaluation 6 months later (24.5%); in contrast, the PTSD screening rate increased by only 4.9% in active duty troops in the same time frame (Milliken, Auchterlonie, & Hoge, 2007). PTSD is a key risk factor for family distress following deployment (for a review of this literature, see Galovski & Lyons, 2004), yet no studies have examined these relationships among NG/R troops or in the context of current military conflicts.
Conceptual Framework
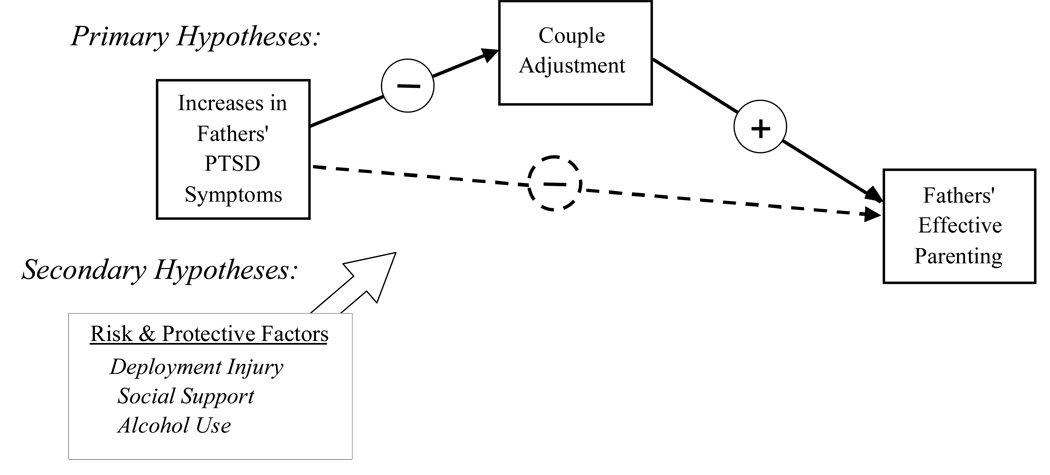
This study uses a developmental-ecological framework to examine associations among combat-related PTSD symptoms, parenting behaviors, and couple adjustment among National Guard soldiers recently returned from Iraq. A developmental-ecological framework (e.g., Bronfenbrenner, 1979; Caspi, Bolger, & Eckenrode, 1987) seeks to explain the cumulative and reciprocal influences of person and context on adjustment and development at multiple levels of influence. This framework is particularly relevant for understanding the impact of traumatic events; for example, several authors have noted the profound ways in which trauma affects the individual’s social/family context (e.g., Solomon et al., 1992). Similarly, prior research has shown how parental psychopathology (specifically, depression) impairs marital adjustment, parenting practices, and child adjustment (e.g., Downey & Coyne, 1990; Gartstein & Fagot, 2003), with marital adjustment mediating associations between family stressors and parenting (Conger, Ge, Elder, Lorenz, & Simons, 1994). As illustrated in Figure 1, in this study we are interested in direct and indirect effects of PTSD symptoms on National Guard veterans’ adjustment in two key family roles: partner and parent. Several primarily cross-sectional studies have examined relationships between PTSD symptoms and general family functioning variables; ours is the first longitudinal study to examine these relationships within a developmental ecological framework. Below, we briefly review extant research.
Figure 1.
Conceptual Model of Change in Fathers’ Posttraumatic Stress Symptoms and Family Functioning.
Impact of PTSD on Couple Relationships and Parenting
Prior literature has linked PTSD with marital disruption and spousal abuse (McCarroll et al., 2000; Prigerson, Maciejewski, & Rosenheck, 2001) reduced intimacy, sexual dysfunction, and lower marital satisfaction (Carroll, Rueger, Foy, & Donahoe, 1985; Riggs, Byrne, Weathers, & Litz, 1998). Few published studies of OEF/OIF deployed military personnel have examined the effects of PTSD symptoms on couple relationships. In a sample of 45 families, soldier-rated PTSD symptoms correlated negatively with self-, and partner-reported relationship satisfaction ratings (Goff, Crow, Reisbig, & Hamilton, 2007). Renshaw, Rodrigues, & Jones (2008), sampling 49 National Guard soldiers and their spouses, found partner-reported marital satisfaction to be negatively associated with soldier self-reports of psychological symptoms only when spouses perceived that the soldier had experienced low combat exposure during deployment; when high combat exposure was perceived, there was no association between soldiers’ symptoms and spouses’ marital satisfaction.
Several studies have examined relationships between PTSD and family functioning variables, but only one study has examined associations with parenting behaviors specifically. Studies of male Vietnam veterans have found PTSD symptoms to be associated with decreased parenting satisfaction (Samper, Taft, King, & King, 2004), impaired attachment with children (Fuls, 1995), child behavior problems (Caselli & Motta, 1995) and family violence (Solomon et al., 1992). A nationally representative sample of 1200 male Vietnam veterans and 376 spouses indicated significantly more child behavior problems, family violence, lower parenting satisfaction, and lower family cohesion, among the group with PTSD (Jordan et al., 1992).
Davidson and Mellor (2001) examined child reports of parenting behaviors in a cross-sectional study of 50 children of Australian Vietnam veterans with and without PTSD and 33 children of civilians. Having a father with PTSD was associated with poorer parent-child problem-solving, communication, and affective involvement (compared with veteran and civilian families without PTSD), although PTSD was not associated with poorer parent-child behavioral control. No published empirical studies have examined the impact of PTSD symptoms on parent reports of parenting, which may be quite different from children’s perceptions. The current study addresses this gap by examining the impact of PTSD symptoms on self-reported parenting behaviors and couple adjustment in a large sample of OIF deployed National Guard soldiers.
Contextual factors associated with PTSD, parenting, and couple adjustment
A developmental-ecological framework requires assessment of contextual risk and protective factors (i.e. those associated with deployment and combat) in adjustment. Combat-related PTSD and alcohol abuse commonly co-occur (Bremner, Southwick, Darnell, & Charney, 1996), and two recent studies have shown alcohol abuse to be problematic among NG/R members recently returned from Iraq. Milliken et al., (2007) reported that 15% of NG/R soldiers compared with 11.8% of active duty soldiers endorsed alcohol problems in a 2-item screening measure included in the Post-Deployment Health Re-Assessment. In a sample of 48,481 participants from the Millenium Cohort Study, Jacobson and colleagues (2008) found increased risk of new-onset binge drinking (odds ratio [OR], 1.46; 95% confidence interval [CI], 1.24–1.71), heavy weekly drinking (OR, 1.63; 95% CI, 1.36–1.96), and alcohol-related problems (OR, 1.63; 95% CI, 1.33–2.01) among combat-deployed NG/R troops, compared with non-deployed NG/R personnel. In addition, reports of mental health symptoms (including PTSD) were associated with risk for new-onset alcohol-related problems in NG/R personnel. Thus, we predicted in this study that PTSD symptoms would be associated with alcohol use, which would directly affect parenting behavior and couple adjustment.
Deployment-related injury, in combination with, or independent of PTSD symptoms, may also contribute to impaired post-deployment couple adjustment and parenting behaviors. Just one pilot study of 41 families with OEF/OIF combat-injured parents has been conducted, yielding associations between spouse reports of family disruption and child distress; no measures of couple adjustment or parenting behaviors were gathered (Cozza et al., 2010). Further investigations are needed to determine the influence of combat injury for both parenting and partner/couple adjustment roles, in association with PTSD symptoms.
Finally, PTSD also has been associated with less perceived social support, and more perceived social support, has, in turn, been identified as a protective factor in the development of PTSD. Two meta-analyses have identified low perceived social support following trauma exposure as one of the most robust correlates of PTSD incidence and severity (Brewin, Andrews, & Valentine, 2000; Ozer, Best, Lipsey, & Weiss, 2003). The relationship between social support and PTSD appears complex: some investigations have found that PTSD leads to deteriorating social support over time, perhaps through processes of altered social orientation (e.g., Clapp & Beck, 2009) or simple deterioration of social resources (e.g., King, Taft, Hammond, & Stone, 2006). However, a recent multi-wave longitudinal study of a natural disaster found that social support immediately following trauma serves as a protective factor for PTSD symptoms in the short term but that persisting PTSD symptoms may erode social support over time (Kaniasty & Norris, 2008). No studies have examined associations between combat-related PTSD symptoms, social support, parenting or couple adjustment in OIF or NG/R samples. Examining social support is particularly important for civilian soldiers, who do not live within the military command and support structures of active duty personnel.
Addressing gaps in the literature: the present study
The body of extant literature regarding the impact of PTSD on families provides support for the association of PTSD symptoms with impairments in family functioning, broadly speaking. However, the literature is limited by descriptive, cross-sectional studies and (particularly for OEF/OIF studies) small sample sizes that limit explanatory power in estimating effects. Much of the existing military family literature is based on retrospective studies of Vietnam veterans; to our knowledge, no prospective longitudinal studies have examined the impact of change in PTSD symptoms on specific elements of family functioning (couple adjustment and perceived parenting behaviors) among OEF/OIF veterans. This is an important area of study, given data indicating an increase in PTSD symptoms following return from deployment (Milliken et al., 2007). There is a critical need for research on NG/R civilian soldiers, a subset of the military more likely to be partnered and parenting, and more vulnerable to mental health and substance use problems than active duty personnel (Jacobson et al., 2008).
To address these gaps in the literature, the present study examined the impact of change in PTSD symptoms following combat deployment on National Guard soldiers’ perceived parenting and couple adjustment one year following return from Iraq. The present study was part of a larger study of NG/R soldiers who were initially assessed (in-theater) one month prior to returning home (Ferrier-Auerbach, Erbes, Polusny, Rath, & Sponheim, 2010). Ferrier-Auerbach et al. (2010) reported significant associations between soldiers’ reports of emotional distress and perceptions of social support from home during deployment. We extend these findings by examining soldiers’ reports of functioning in the roles of parent and partner. Thus, consistent with a developmental-ecological framework, the primary hypothesis of the present study was that increases in PTSD symptoms over time would be associated with lower levels of perceived effective parenting and couple adjustment after deployment, controlling for alcohol use, social support, deployment injury, and socio-demographics. Further, couple adjustment was expected to mediate the relationship between change in PTSD symptoms and effective parenting.
Secondary hypotheses predicted the influence of contextual factors: Increases in PTSD symptoms were expected to be associated with greater alcohol use, which, in turn, would be associated with lower levels of couple adjustment and effective parenting following return from deployment. Deployment injury was conceptualized as an additional stressor with direct and indirect influences on parenting through the increased likelihood of PTSD symptoms at both time points. On the other hand, perceived social support was expected to provide a buffer to parenting, as well as to reduce the likelihood of increase in PTSD symptoms following return home (Kaniasty & Norris, 2008).
Method
Participants
Data for this study were from a sample of 468 male National Guard soldiers who were deployed to Iraq, endorsed being the father of at least one or more children and self-identified as either European American (89%), African American (5%), or Hispanic American (6%), and completed in-theater (Time 1) and follow-up (Time 2) questionnaires. The current sample came from a larger, longitudinal study of 2,677 soldiers from the 1st Brigade Combat Team, 34th Infantry (1/34 BCT) who were deployed to Iraq from March 2006 to July 2007 (Ferrier-Auerbach et al., 2010). At Time 2, one year following the return from deployment, 49.3% of respondents who had agreed to be contacted for follow-up (n = 953), returned questionnaires. Although Time 2 responders were significantly older (mean years = 31.47, SD = 8.31) than non-responders (mean years = 29.06, SD = 7.70) and more likely to be married (48.8% of responders vs. 37.7% of non-responders), there were no differences between responders and non-responders at Time 1 on gender, ethnicity, or baseline PTSD symptoms.
Of the 953 respondents completing surveys at both time points, 516 soldiers endorsed having one or more children and 468 also met the criterion of being European American, African American, or Hispanic American males (1.4% were Native American, 1% Asian, and 1.6% other, and were excluded from analyses because numbers were too small for estimates of meaningful racial and ethnic contrasts in the hypothesized adjustment model). Given that 97% of the sample was male, we restricted the sample to fathers for the present report. Mean age of the analysis sample was 36.36 years (SD=8.04). Ranging from 1 to 39 months, the duration of this deployment was, on average, 16.56 months (SD = 3.24). The median and modal number of months deployed was 16. Sixty percent of the sample was previously deployed one or more times. Seventy-four percent were married, and the average number of minor children living at home was 1.35 (SD = 1.14). Respondents could report the ages for up to at least 6 children. For minor children, the youngest reported child age ranged from 0 to 17 years (M = 6.45, SD = 4.53) and oldest reported age ranged from 0 to 17 years (M = 9.63, SD = 5.11). One item assessed whether respondents had sustained any injury while deployed, requiring those responding in the affirmative to check the type of injury sustained. Over half of the sample (n = 273; 52.9%) reported sustaining at least one injury in Iraq, with 8.9% reporting a head injury, 1.9% reporting a fragment injury, 8.3% reporting a vehicular injury, 13.5% reporting a fall injury, and 23.1% reporting a blast injury. Three items assessed whether participants had received VA care since returning from Iraq. Overall, 70.8% of the study sample reported receiving VA care of some kind since returning from Iraq, with 36.5% reporting VA care for physical problems and 28.6% for “reintegration problems”.
Procedures
For the larger study, soldiers (N=2677) completed a survey one month prior to their return home (Time 1). One year following soldiers’ return from Iraq (Time 2), 1,935 soldiers (72.3% of the original sample) who provided contact information and who expressed interest in participating in future follow up studies were sent a mailed survey to assess the impact of deployment and PTSD symptoms on reintegration concerns including parenting and family functioning. While the survey method enabled access to a larger sample, resource limitations prevented us from gathering multi-informant data (i.e. data from spouses or children), or from gathering additional, parenting-related information (i.e. a child behavior questionnaire). Mailed survey procedures used a modified Dillman (2007) protocol with repeated mailings, a postcard reminder, and $20 incentive to enhance the response rate, which was 49.3%.
Measures
PTSD symptomatology was assessed at both time-points using the PTSD Checklist-Military Version (PCL-M; Weathers, Litz, Herman, Huska, & Keane, 1993), a widely used self-report questionnaire of the presence and severity of PTSD symptoms as defined by the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV; American Psychiatric Association, 1994). Respondents were asked to rate the extent to which they were bothered by each of 17 PTSD symptoms in the past month using a 5-point scale ranging from 1 (Not at all) to 5 (Extremely). Items are summed to yield a total PTSD symptom severity score and three subscale scores: Re-experiencing, Avoidance, and Arousal. The PCL has demonstrated excellent internal consistency (Ruggiero, Rheingold, Resnick, Kilpatrick, & Galea, 2006). Convergent validity of the PCL is supported by positive correlation with other measures of PTSD (e.g., Mississippi Scale for PTSD; Ruggiero et al., 2003). Three subscales derived from the PCL were used as manifest indicators in the latent variable models for Time 1 and Time 2. Participants were determined to have probable PTSD if they met DSM-IV criteria on the PCL-M (reporting at least of one intrusion symptom, three avoidance symptoms, and two hyperarousal symptoms at moderate levels) and obtained a total score of at least 50 (Hoge et al., 2004). In this study, Cronbach's alpha for the three subscales ranged from .81–.92 (alpha reliabilities for specific scale and time listed in Table 1).
Table 1.
Time 1 In-theater and Time 2 Post Deployment Means and Standard Deviations for Study Scale Scores and Latent Variable Indicators (n=468)
| Time 1 | Time 2 | Paired Sample |
||||||
|---|---|---|---|---|---|---|---|---|
| M | SD | α | M | SD | α | t | η2 | |
| Total PCL PTSD symptoms | 30.54 | 11.33 | .92 | 34.57 | 14.82 | .95 | 6.89*** | .09 |
| Re-experiencing Scale | 8.16 | 3.60 | .86 | 9.10 | 4.44 | .92 | 5.04*** | .05 |
| Avoidance Scale | 11.47 | 4.77 | .83 | 13.55 | 6.37 | .90 | 7.71*** | .11 |
| Hyper Arousal Scale | 10.90 | 4.49 | .81 | 11.94 | 5.08 | .87 | 4.59*** | .04 |
| Social Support | 4.01 | .83 | .68 | |||||
| Alcohol Use | 6.57 | 6.24 | .85 | |||||
| Couple Adjustment | ||||||||
| Brief DAS Total | 21.97 | 6.57 | .88 | |||||
| Closeness | 2.74 | 1.09 | .70 | |||||
| Perceived Parenting Behaviors | ||||||||
| Positive Parenting APQ | 12.03 | 2.36 | .91 | |||||
| Inconsistent Discipline APQ | 6.56 | 2.26 | .65 | |||||
| Poor Supervision APQ | 4.96 | 2.31 | .74 | |||||
| Parent-Child Involvement | 3.81 | 0.79 | .75 | |||||
Note: Time 1 is in-theater data, surveyed one month prior to return home. Time 2 is one year post deployment. η2 = eta squared measure of effect size.
p < .001;
p < .01;
p < .05
The perceived parenting behaviors latent variable was measured at Time 2, by four scale indicators. The first three were from the Alabama Parenting Questionnaire—Short Form (APQ-9; Elgar, Waschbusch, Dadds, & Sigvaldason, 2007), a shortened version of the widely-used Alabama Parenting Questionnaire (Frick, 1991) measuring parenting practices. The APQ-9 contains nine items and yields three subscales: Positive Parenting, Inconsistent Discipline, and Poor Supervision. Participants are asked to rate the typical frequency of various parental and child behaviors on a 5-point Likert scale with options ranging from 1 (Never) to 5 (Always), for example: “You praise your child if he/she behaves well”, and “You threaten to punish your child and then do not actually punish him/her”. Possible scores range from 9–45. Internal consistency of the three subscales has been shown to be moderate (Elgar et al., 2007) (α ranged from .57–.61, Table 1). The APQ-9 has demonstrated strong criterion validity as evidenced by moderate correlations with child symptoms (Elgar et al., 2007) (α ranged from .64–.90). The fourth indicator was positive parent-child involvement measured from four items on the Social Adjustment Scale-Self Report (SAS-SR; Weissman & Bothwell, 1976) and one additional item. The following SAS-SR items were rated by respondents on 5-point scale ranging from 1 (Not at all) to 5 (All of the time): “In the past two weeks have you, 1) Been interested in your children’s activities, 2) Been able to talk to and listen to your children, 3) Been shouting at or arguing with your children (reverse coded), and 4) Been feeling affectionate towards your children.” Additionally, respondents were asked to provide an overall rating of their connection with their children on a 5-point scale ranging from 1 (A lot less connected) to 5 (A lot more connected). Specifically, respondents were asked: “Compared to before you were deployed to Iraq (2006–2007), how connected do you feel with your children?” (α = .75 for 5-item scale).
Post-deployment couple adjustment was measured at Time 2, using total scores from the 7-item short form of the widely used Dyadic Adjustment Scale (DAS-7; Sharpley & Rogers, 1984; Spanier, 1976). Participants are asked to rate each of 6 items assessing domains of relationship functioning on a 6-point scale and one item assessing overall happiness, with higher ratings indicating better adjustment. The DAS-7 has demonstrated good internal consistency (Hunsley, Pinsent, Lefebvre, James-Tanner, & Vito, 1995; Sharpley & Rogers, 1984). Evidence for the criterion validity of the DAS-7 is demonstrated by studies showing the scale correlates with other measures of marital functioning (Hunsley et al., 1995) and discriminates between distressed and adjusted couples (Hunsley, Best, Lefebvre, & Vito, 2001) (α = .89).
Closeness, a second indicator of couple adjustment, was taken from the mean of two items. The first item was “Compared to before you were deployed to Iraq, how would you describe your physical intimacy with your partner?” rated from 1 (a lot less intimate) to 5 (a lot more intimate). The second item was “Compared to before you were deployed to Iraq, how emotionally connected do you feel with your partner?” rated from 1 (a lot less connected) to 5 (a lot more connected). The two closeness items were correlated .54 (p < .001, α = .70).
Problematic alcohol use following deployment was measured, at Time 2, with the 10-item Alcohol Use Disorders Identification Test (AUDIT: Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). Using a 5-point scale ranging from 0 to 4, participants are asked to rate the quantity and frequency of drinking on a typical day, frequency of binge drinking (defined as six or more drinks), and problem behaviors associated with drinking. Scores for the ten items are summed, with higher scores indicating more problematic drinking. The AUDIT has demonstrated high internal consistency and excellent test-retest reliability, and correlates with other self-report instruments of alcohol use and alcohol problems (Babor et al., 2001). A cut score of 8 or greater was used to identify those reporting problematic drinking (Conigrave, Hall, and Saunders, 1995) (α = .86).
At Time 2, respondents were asked whether they sustained any physical injury during deployment coded 1 (yes) and 0 (no); severity of the injury was not assessed.
Two items assessed at Time 1 measured soldiers’ perceptions of social support while deployed in-theater: “I have had sufficient contact with my family and friends back home during my deployment,” and “The contact I have had with my family and friends back home has helped me to feel better about my mission and more focused on my duties”. Each item was rated on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree), and the mean of the items was used as an exogenous indicator. Items were correlated .50 (p <.001); α = .68.
Several control variables were entered in the multivariate analyses. Previous deployment status was assessed at Time 2 by a yes/no question asking whether the individual had, other than the recent deployment, been previously deployed to OEF/OIF and was coded 1 (yes) and 0 (no). Racial/ethnic status was assessed at Time 1 and entered using dummy coded contrast variables created for African American and Hispanic Americans coded 1 (yes) and 0 (no). Number of minor children in the home was assessed at Time 2 and entered as a continuous variable.
Analytic Strategy
The analysis plan included two basic analyses, (a) examination of sample descriptive data and a paired sample t test to compare the change between the Time 1 and Time 2 PTSD scores, and, (b) structural equation path models for the effects of change in PTSD on couple adjustment and perceived parenting behaviors, specified as an auto-regressive latent variable model. More specifically, the present study employed structural equation path modeling (SEM) to examine the hypothesized model and hypothesized mediation (MacKinnon, 2008). SEM simultaneously estimates a measurement model for the latent variable factor structures and estimates the specified predictive associations among the latent variables using multivariate regression analysis. We employed the MPlus5.2 program (Muthén & Muthén, 2007) because of its ability to incorporate missing data using full-information maximum likelihood (FIML) estimation, which provides more statistically reliable standard errors compared to mean-imputation, list-wise, or pair-wise SEM models (Wothke, 2000).
Results
Means, standard deviations, and alpha reliabilities of the key study variables are provided in Table 1. Bivariate correlations among all study variables are provided in Table 2. The total PCL scale score and the three subscales each showed a marked increase in PTSD symptoms from the Time 1 data gathered in-theater to the Time 2 data gathered one-year following return from deployment. The repeated measures (η2) indicated by the effect sizes for the changes in PTSD were in the medium to large ranges for the total score and sub scales, .09, .05, .11 and .04. Cohen (1988) characterizes η2 of .01 as small, .06 as medium, and .14 as large. Using Hoge and colleagues’ strict criteria, defined as meeting DSM-IV criteria on the PCL (reporting at least one intrusion symptom, three avoidance symptoms, and two hyperarousal symptoms at the moderate level) and total score of at least 50 (Hoge et al., 2004), 6% had probable PTSD at Time 1 and 15% at Time 2.
Table 2.
Pearson Correlations Among Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Prior Deployed | --- | ||||||||||||||||||
| 2. Injured | −.04 | --- | |||||||||||||||||
| 3. Number of children | −.04 | −.01 | --- | ||||||||||||||||
| 4. Social Support | .00 | −.03 | .04 | --- | |||||||||||||||
| 5. African American | −.03 | −.03 | −.06 | .06 | --- | ||||||||||||||
| 6. Hispanic American | −.08 | .09 | −.06 | .01 | −.06 | --- | |||||||||||||
| 7. Alcohol Use | .00 | .10* | −.14** | −.11* | −.07 | .04 | --- | ||||||||||||
| 8. PCL Re-experience T1 | .06 | .22*** | −.05 | −.04 | −.01 | .06 | .17*** | --- | |||||||||||
| 9. PCL Avoidance T1 | −.01 | .14** | −.03 | −.09 | −.03 | .06 | .16*** | .65*** | --- | ||||||||||
| 10. PCL Arousal T1 | .03 | .21*** | −.07 | −.07 | −.09* | .04 | .20*** | .65*** | .67*** | --- | |||||||||
| 11. PCL Re-experience T2 | .07 | .27*** | −.06 | −.12** | −.03 | .00 | .32*** | .54*** | .45*** | .48*** | --- | ||||||||
| 12. PCL Avoidance T2 | .03 | .28*** | −.08 | −.16*** | −.07 | .06 | .35*** | .44*** | .50*** | .45*** | .79*** | --- | |||||||
| 13. PCL Arousal T2 | .02 | .31*** | −.07 | −.12** | −.05 | .05 | .32*** | .45*** | .42*** | .53*** | .80** | .81*** | --- | ||||||
| 14. DAS | .07 | −.08 | −.02 | .08 | .07 | −.15** | −.20*** | −.08 | −.06 | −.02 | −.27*** | −.35*** | −.30*** | --- | |||||
| 15. Closeness | −.05 | −.07 | −.00 | .15** | .05 | −.02 | −.06 | −.11* | −.10* | −.05 | −.15** | −.31*** | −.20*** | .47*** | --- | ||||
| 16. APQ Positive | −.01 | −.04 | −.08 | .18*** | .11* | .05 | −.12* | −.06 | −.10 | −.07 | −.10 | −.17** | −.09 | .17** | .10 | --- | |||
| 17. APQ Discipline | −.02 | .05 | .12* | .01 | −.07 | .03 | .09 | .11* | .15** | .06 | .19*** | .17** | .18*** | −.24*** | −.02 | −.04 | --- | ||
| 18. APQ Supervision | .09 | .09 | −.03 | −.11* | −.02 | −.03 | .12* | .17** | .14** | .12* | .19*** | .16** | .16** | −.17** | −.05 | −.17** | .34*** | --- | |
| 19. SAS-SR Involvement | −.06 | −.15*** | −.13** | .15*** | .12** | .01 | −.14** | −.20*** | −.21*** | −.21*** | −.34*** | −.39*** | −.40*** | .29*** | .22*** | .45*** | −.25*** | −.24*** | --- |
p < .001;
p < .001;
p < .05
Further, participants reported relatively high levels of social support while deployed (M = 4.01 on a scale of 1 to 5). On average the sample was characterized by subclinical levels of drinking on the AUDIT screening measure at Time 2 with scores ranging from 0 to 40. In the present sample of fathers returning from combat, 31% were above the standard cut score of eight for identifying problematic drinking.
Marital Adjustment and Perceived Parenting Behaviors
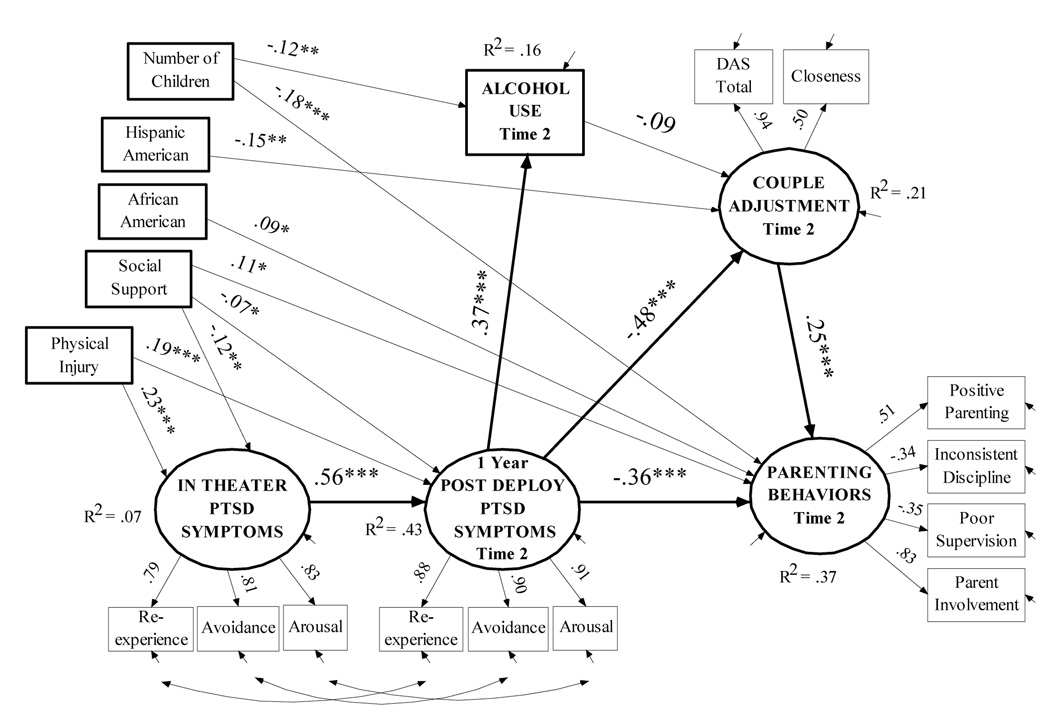
Effects of change in PTSD were specified as a latent variable SEM model regressing the perceived parenting behaviors domain and couple adjustment domain on the control variables, alcohol use, and change in PTSD defined as a latent variable autoregressive factor using the three subscales of the PCL as indicators. Results of the SEM path model are shown in Figure 2 in the form of standardized factor loadings and beta paths for the regression path model. The model provided adequate fit to the data with a high comparative fit index (CFI = .97), a χ2 minimization ratio less than 2.00 (χ2/df =1.66), and a low root mean square error of approximation (RMSEA = .038, 90% C.I. = .027 to .048).
Figure 2.
Structural Equation Model for effects of Change in PTSD Symptoms on Couple Adjustment and Perceived Parenting Behaviors. Paths are standardized coefficients. [χ2(101) = 168.05, p = .00, comparative fit index (CFI) = .97, χ2 ratio (χ2/df) =1.66, root mean square error of approximation (RMSEA) = .038, 90% C.I. = .027 to .048]. *p < .05; **p < .01, ***p < .001, †p < .10.
Focusing on couple adjustment and perceived parenting behaviors, the primary hypothesis was supported: increases in PTSD symptoms from Time 1 to Time 2 were associated with lower levels of couple adjustment (β = −.48, p < .001) and lower levels of effective parenting (β = −.36, p < .001). Change in PTSD predicted couple adjustment, and couple adjustment, in turn, was associated with better parenting (β = .25, p < .001), however, the direct effect of change in PTSD on parenting was not mediated (i.e., the direct effect remained significant when couple adjustment was entered as a potential mediator). Results showed that change in PTSD exhibited both a direct and indirect effect on perceived parenting behaviors.
The hypothesis regarding alcohol use as a risk factor for parenting and couple adjustment was not supported. PTSD was associated with higher levels of alcohol use (β = .37, p < .001), but alcohol use was not significantly associated with couple adjustment or parenting. Other secondary hypotheses were supported, however, regarding effects of social support and deployment injury. Higher levels of Time 1 social support were associated with lower levels of Time 1 in-theater PTSD and decreases in PTSD symptoms from Time 1 to Time 2. Conversely, deployment injury was independently associated with higher levels of in-theater and increases in PTSD symptoms. In addition, Time 1 social support predicted higher levels of perceived parenting behaviors at Time 2 but not couple adjustment.
Among the control variables, African American fathers reported higher levels of effective parenting behaviors relative to European Americans, and Hispanic Americans exhibited lower levels of couple adjustment. Number of children was associated with lower levels of drinking but also with lower levels of perceived effective parenting behaviors. Prior deployment was not associated with outcomes and therefore not shown for clarity in the model. Overall, the control variables and the hypothesized predictors explained 37% of the variance in perceived parenting behaviors and 21% of the variance in couple adjustment.
Given the significant effects of social support and deployment injury on Time 1 and Time 2 PTSD, we wanted to further examine tests of indirect effects on parenting and couple adjustment through intervening variables in the path diagram. Indirect effects represent the meaningful influence of an exogenous predictor on the endogenous outcomes specified in the model. MPlus5.2 provides estimates of total effects, indirect effects, and specific indirect effects. Computationally, MPlus conducts bootstrap sampling to compute estimates of the indirect effect standard errors. Total effects are the combined direct and indirect influence on a variable, indirect effects are the total influence through intervening variables, and specific indirect paths are tests of specific influence.
In this case we were interested in specific effects through PTSD. Results are shown in Table 3. Starting with deployment injury effects on parenting, the total effect (combined direct and indirect paths) on parenting was significant (β = −.17, p <.001). The total effect is also a special case of the bivariate relationship controlling for other variables. Rows 2 and 3 showed that injury status had significant indirect influence and specifically through its effects on PTSD. In fact, the data indicated that both deployment injury and social support had significant indirect effects through PTSD on the outcomes. This suggested that PTSD was an important mechanism linking injury and social support to marital adjustment and perceived parenting behaviors.
Table 3.
Total, Indirect, and Specific Indirect Path Effects of T1 Social Support and Physical Injury on T2 Couple and Perceived Parenting Behaviors
| Perceived Parenting Behaviors | Beta | SE | t | |
|---|---|---|---|---|
| Total Effect: Injured→T2 Perceived Parenting Behaviors | −.17 | .05 | −3.33*** | |
| Total Indirect Effect: Injured→ T2 Perceived Parenting Behaviors | −.15 | .03 | −4.90*** | |
| Specific Indirect: Injured→T1 PTSD→ T2 PTSD→ T2 Perceived Parenting Behaviors | −.05 | .01 | −3.09*** | |
| Total Effect: T1 Social Support→ T2 Perceived Parenting Behaviors | .19 | .05 | 3.51*** | |
| Total Indirect Effect: T1 Social Support→T2 Perceived Parenting Behaviors | .07 | .03 | 2.81** | |
| Specific Indirect: T1 Social Support →T1 PTSD→T2 PTSD→T2 Perceived Parenting Behaviors | .04 | .01 | 2.21* | |
| Couple Adjustment | ||||
| Total Effect: Injured→T2 Couple Adjustment | −.07 | .05 | −1.42 | |
| Total Indirect Effect: Injured→T2 Couple Adjustment | −.11 | .02 | −3.88*** | |
| Specific Indirect: Injured→T1 PTSD→ T2 PTSD→T2 Couple Adjustment | −.06 | .02 | −3.49*** | |
| Total Effect: T1 Social Support→T2 Couple Adjustment | .08 | .05 | 1.47 | |
| Total Indirect Effect: T1 Social Support→T2 Couple Adjustment | .06 | .02 | 2.69* | |
| Specific Indirect: T1 Social Support→T1 PTSD→ T2 PTSD→T2 Couple Adjustment | .05 | .02 | 2.35* | |
Note: T1 = Time 1in-theater data, surveyed one month prior to return home; T2 = Time 2 one year post deployment; PTSD = PTSD Symptoms;
p < .001;
p < .001;
p < .05
Discussion
To our knowledge, the study findings are the first to show a direct link between increases in PTSD and post-deployment self-reports of couple and parenting difficulties. Reintegration into a family following combat deployment requires renegotiating roles as partner and parent (Faber, Willerton, Clymer, MacDermid, & Weiss, 2008). Our findings suggest that symptoms of PTSD may exert their influence at multiple levels within the family, making these difficult transitions even more complicated. A growing body of research has produced data showing the association of individual PTSD symptoms with social/family context variables, but research has been slow to examine putative mechanisms through which this influence is exerted (Monson, Taft, & Fredman, 2009). The use of a developmental-ecological framework enabled us to go beyond the purely descriptive, by providing an opportunity to study linkages over time between PTSD symptoms and their mechanisms of influence within the family (i.e. parenting behavior and couple adjustment). In this study we have provided preliminary evidence of the importance of PTSD symptoms for self-reported parenting behaviors and couple adjustment, paving the way for more extensive studies examining reciprocal and transactional linkages.
Contrary to our hypothesis, we did not find that couple adjustment mediated the relationship between PTSD symptoms and parenting. Thus, although PTSD had significant direct effects on both self-reported couple adjustment and parenting, as well as an indirect effect on parenting through couple adjustment, the data did not indicate that the influence of PTSD symptoms on perceived parenting was due solely to their effect on the couple relationship.
How and why might PTSD impair parenting behaviors? PTSD symptoms of emotional numbing/avoidance may manifest in detachment from family activities and reduced monitoring of, and involvement with children, and hyper-arousal symptoms may spark volatile or emotionally dysregulated parent-child interactions, particularly in stressful situations, (such as those around discipline or conflict). No research has examined associations with parenting behaviors, but Samper, Taft, King, and King (2004) found associations between emotional numbing symptoms of PTSD and parenting satisfaction in a nationally representative sample of 250 male Vietnam veterans. Similarly, studies with couples have found that symptoms of numbing/avoidance and anger/arousal are particularly related to impaired relationship satisfaction and interpersonal violence (see Galovski and Lyons, 2004, for a review).
It is important to point out that because couple adjustment and parenting were only measured cross-sectionally (i.e., at Time 2), directionality of effects cannot be parsed out. It is possible that stressors within the family (i.e., parenting and couple adjustment difficulties) increase PTSD symptoms following return from deployment, and/or even likely that the relationships are reciprocal and transactional in nature, such that PTSD symptoms worsen parenting and couple adjustment, which in turn exacerbates PTSD symptoms (Monson et al., 2009). More complex empirical (developmental-ecological) models are needed to account for the reciprocal and transactional linkages among combat PTSD, parenting, and couple adjustment.
Among secondary hypotheses, deployment injury was not significantly associated with perceived parenting behavior (once other variables were accounted for), but was significantly associated with PTSD symptoms at both time points; PTSD symptoms thus fully mediated the relationship between injury and parenting. This finding confirms the importance of PTSD as a central construct through which injury may be linked to parenting and couple adjustment in returning veterans, and suggests that the emotional impact of an injury (i.e., resultant PTSD symptoms) may be more influential to parenting than the physical impact. In conjunction with our finding of relatively high reports of deployment injury in our National Guard sample, this finding has important implications for the provision of psychological services (and particularly PTSD treatment) to injured National Guardsmen. No published research has investigated the impact of combat deployment injury on parenting behavior, but the importance of understanding this relationship has been noted (Cozza et al., 2005), particularly in light of medical advances resulting in increased survival rates after injuries in OEF/OIF compared to prior conflicts (Tanielian & Jaycox, 2008). The absence of information regarding the severity of injuries sustained precludes conclusions about the effects of more severe injuries (such as loss of limb or moderate to severe head injuries) on couple adjustment and parenting; these may have distinct effects obscured by less severe injuries that were also included in our injury variable.
The high rates of alcohol use and PTSD symptoms found among veterans in this study, as well as increases in both over the course of the first year post-deployment, are consistent with those reported in prior studies of the current conflicts (Hoge et al., 2006; Milliken et al, 2007). As predicted, PTSD symptoms were associated with higher levels of alcohol use. This finding is particularly important given that most National Guard personnel do not receive treatment in VA settings but in community mental health settings with professionals less familiar with combat PTSD, making it arguably more likely for PTSD to go untreated in favor of other interventions (e.g., alcohol treatment or addressing the psychological effects of an injury).
Consistent with hypotheses, higher perceived social support assessed in-theater predicted more effective perceived parenting behaviors one year later; extent of social support also was negatively associated with subsequent increase in PTSD symptoms. Social support thus appears to be an important protective buffer for National Guard soldiers and their families. Strong perceived social support may be particularly critical for National Guard populations, who are not typically afforded the formal support structures of Active Duty personnel (the military base community, military healthcare, etc). The finding that social support directly influences parenting is not surprising, given prior developmental literature indicating that support systems protect caregiver functioning and parenting (e.g., Campbell & Lee, 1992). Our data also are somewhat consistent with Kaniasty and Norris’ (2008) finding that immediately post-trauma, social support buffered the negative effects of traumatic stress but, as time went on, persisting symptoms of PTSD did lead to a longer term erosion in support. Further longitudinal follow-up is needed to ascertain the impact of increase in PTSD on subsequent social support following return from deployment (social support was assessed in this sample only in-theater).
Among the socio-demographic control variables, ethnic/racial differences were noted in relation to outcome variables, with African American fathers reporting higher levels of effective parenting, and Hispanic Americans reporting lower levels of couple adjustment, both relative to European Americans. More research is needed to confirm these findings, particularly because the sample proportions of both minority populations were very small (5 and 6% respectively). Few studies have examined family functioning among minority groups in the US military; none have examined parenting (Drummet, Coleman, & Cable, 2003; McCubbin & McCubbin, 1988).
We acknowledge several limitations to this study. By recruiting from a specific Army National Guard combat brigade team we were able to assess participants who returned home at around the same time, preserving the temporal homogeneity and the internal validity of the study. However, these factors, coupled with the 49% response rate, also constitute threats to the external validity of the study. Thus, this mid-western sample may not necessarily be representative of all Army National Guard brigades, and results may not generalize to other military components (e.g., Active Duty service members, who are more likely to be younger, unpartnered and without children). Although baseline scores indicated no significant differences between respondents and non-respondents, it is possible that they differed in other aspects of functioning not measured here. Given the survey nature of the study and sample size, we relied on self-report measures of parenting and PTSD, but in doing so we were unable to gather multi-informant data (i.e. from spouses and children) or multi-method data (e.g., observational measures of parenting). This mono-method bias means that the observed relationships may be due in part to the effect of PTSD on perceptions of parenting rather than actual parenting behaviors. Study resource limitations prevented us from asking respondents to report on child behavior, which is an important associated factor of parenting. Finally, while aspects of this study were longitudinal (i.e., measurement of PTSD), the assessments of parenting and couple adjustment were only conducted at Time 2, post deployment. Thus, relations between couple adjustment and parenting are cross-sectional.
Data from this study indicating the influence of increases in PTSD symptoms on perceived parenting behaviors highlight the need for further research, given the importance of parenting for child adjustment, particularly in risk contexts (Collins, Maccoby, Steinberg, Hetherington, & Bornstein, 2000). No studies to date have examined relationships between combat related PTSD, parenting behaviors, and child adjustment in military families (Palmer, 2008), although prior studies have shown associations of parental PTSD symptoms with children’s externalizing problems, hostility and aggression (e.g. Caselli & Motta, 1995; Glenn et al, 2002). However, associations between parenting behaviors and children’s adjustment have been examined in other contexts. Parenting behaviors have been shown to mediate the impact of external stressors on children’s externalizing problems across a range of circumstances, including parental mental illness, substance abuse, family transitions, poverty, and family violence (Belsky, 1984; Conger et al., 1992; Conger et al., 2002; Elder et al., 1986; Patterson, 1982; Patterson, 2005). Future research will need to use multiple informant ratings and methods to assess parenting behaviors and child adjustment in order to better elucidate the relationship between those constructs and PTSD.
Given the overwhelming number of fathers (compared with mothers) in the US Military, far more research is needed to answer questions about the impact of PTSD on fathers’ parenting, the influence of fathers’ parenting on mothers’ parenting, and their combined influence on child adjustment. The higher incidence of combat PTSD, and associated risks among the large military sub-populations who are more likely to be parenting (i.e. NG/R populations) provides a strong impetus for advancing this research agenda.
Although an emerging focus of clinical research and practice examines the impact of PTSD on couples and couple interventions (e.g., Erbes, Polusny, MacDermid, & Compton, 2008; Monson, Price, Rodriguez, Ripley, & Warner, 2004), there is a serious dearth of literature on interventions to support parenting among veterans and no published studies of parenting interventions for NG/R families. We speculate that effective parenting preventive interventions for families affected by combat stress – and particularly National Guard families - might enhance parenting practices and improve parent-child relationships as well as increase social support, protecting parenting in the face of family stress, role overload, and conflict for fathers (DeGarmo, Patras, & Eap, 2008). Indeed, prior data from randomized prevention trials of effective parenting programs have indicated benefits to parents’ mental health (reductions in depression) as well as improvements in parenting and child adjustment (Forgatch & DeGarmo, 1999; Forgatch, Patterson, DeGarmo & Beldavs, 2009). The field is in its early stages and much research remains to be done, but with significant numbers of OEF/OIF veterans suffering from PTSD and other mental health problems who are caring for dependent children, there is a clear need for further research in this area (Palmer, 2008). The need is particularly relevant for populations at higher risk for PTSD such as National Guard and Reservists, who are less likely to seek out VA services, who may be more socially isolated, and who often lack the supports available to active duty families.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
Contributor Information
Abigail H. Gewirtz, Department of Family Social Science & Institute of Child Development, University of Minnesota
Melissa A. Polusny, Minneapolis VA Medical Center, Center for Chronic Disease Outcomes Research, & University of Minnesota Medical School
David S. DeGarmo, Oregon Social Learning Center
Anna Khaylis, Minneapolis VA Medical Center & University of Minnesota Medical School
Christopher R. Erbes, Minneapolis VA Medical Center & University of Minnesota Medical School
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The alcohol use disorders identification test. Guidelines for use in primary care. World Health Organization. 2001 from http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6a.pdf.
- Belsky J. Determinants of parenting: A process model. Child Development. 1984;55:83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick SM, Darnell A, Charney DS. Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. American Journal of Psychiatry. 1996;153(3):369–375. doi: 10.1176/ajp.153.3.369. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Browne T, Hull L, Horn O, Jones M, Murphy D, Fear NT, et al. Explanations for the increase in mental health problems in UK reserve forces who have served in Iraq. The British Journal of Psychiatry. 2007;190:484. doi: 10.1192/bjp.bp.106.030544. [DOI] [PubMed] [Google Scholar]
- Campbell KE, Lee BA. Sources of personal neighbor networks: Social integration, need, or time? Social Forces. 1992;70(4):1077–1100. [Google Scholar]
- Carroll EM, Rueger DB, Foy DW, Donahoe C. Vietnam combat veterans with posttraumatic stress disorder: Analysis of marital and cohabitating adjustment. Journal of abnormal psychology (1965) 1985;94(3):329–337. doi: 10.1037//0021-843x.94.3.329. [DOI] [PubMed] [Google Scholar]
- Caselli LT, Motta RW. The effect of PTSD and combat level on Vietnam veterans' perceptions of child behavior and marital adjustment. Journal of Clinical Psychology. 1995;51(1):4–12. doi: 10.1002/1097-4679(199501)51:1<4::aid-jclp2270510102>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Caspi A, Bolger N, Eckenrode J. Linking person and context in the daily stress process. Journal of Personality and Social Psychology. 1987;52(1):184–195. doi: 10.1037//0022-3514.52.1.184. [DOI] [PubMed] [Google Scholar]
- Clapp JD, Beck J. Understanding the relationship between PTSD and social support: The role of negative network orientation. Behaviour Research and Therapy. 2009;47(3):237–244. doi: 10.1016/j.brat.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the social sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Collins WA, Maccoby EE, Steinberg L, Hetherington EM, Bornstein MH. Contemporary research on parenting: The case for nature and nurture. Annual progress in child psychiatry and child development. 2000;55(2):218–232. [PubMed] [Google Scholar]
- Conger RD, Conger KJ, Elder GH, Jr, Lorenz FO, Simons RL, Whitbeck LB. A family process model of economic hardship and adjustment of early adolescent boys. Child Development. 1992;63(3):526–541. doi: 10.1111/j.1467-8624.1992.tb01644.x. [DOI] [PubMed] [Google Scholar]
- Conger RD, Ge X, Elder GH, Jr, Lorenz FO, Simons RL. Economic stress, coercive family process, and developmental problems of adolescents. Child Development. 1994;65:541–561. [PubMed] [Google Scholar]
- Conger RD, Wallace LE, Sun Y, Simons RL, McLoyd VC, Brody GH. Economic pressure in African American families: a replication and extension of the family stress model. Developmental Psychology. 2002;38(2):179–193. [PubMed] [Google Scholar]
- Conigrave KM, Hall WD, Saunders JB. The AUDIT questionnaire: Choosing a cutoff score. Addiction. 1995;90:1349–1356. doi: 10.1046/j.1360-0443.1995.901013496.x. [DOI] [PubMed] [Google Scholar]
- Cozza SJ, Chun RS, Polo JA. Military families and children during operation Iraqi freedom. Psychiatric Quarterly. 2005;76(4):371–378. doi: 10.1007/s11126-005-4973-y. [DOI] [PubMed] [Google Scholar]
- Davidson AC, Mellor DJ. The adjustment of children of Australian Vietnam veterans: Is there evidence for the transgenerational transmission of the effects of war-related trauma? Australian and New Zealand Journal of Psychiatry. 2001;35(3):345–351. doi: 10.1046/j.1440-1614.2001.00897.x. [DOI] [PubMed] [Google Scholar]
- DeGarmo DS, Patras J, Eap S. Social support for divorced fathers' parenting: Testing a stress-buffering model. Family Relations. 2008;57(1):35–48. doi: 10.1111/j.1741-3729.2007.00481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillman DA. Mail and internet surveys: The tailored design method 2007 update. Hoboken. Hoboken, NJ: John Wiley & Sons Inc; 2007. [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychol Bull. 1990;108(1):50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Drummet AR, Coleman M, Cable S. Military families under stress: Implications for family life education. Family Relations. 2003;52:279–287. [Google Scholar]
- Elder GHJ, Caspi A, Downey G. Problem behavior and family relationships: Life course and intergenerational themes. In: Sorensen AB, Weinert F, Sherrod LR, editors. Human development and the life course: Multidisciplinary perspectives. New York: Lawrence Earlbaum; 1986. pp. 293–340. [Google Scholar]
- Elgar FJ, Waschbusch DA, Dadds MR, Sigvaldason N. Development and validation of a short form of the Alabama Parenting Questionnaire. Journal of Child and Family Studies. 2007;16(2):243–259. [Google Scholar]
- Erbes CR, Polusny MA, MacDermid S, Compton JS. Couple therapy with combat veterans and their partners. Journal of Clinical Psychology. 2008;64(8):972–983. doi: 10.1002/jclp.20521. [DOI] [PubMed] [Google Scholar]
- Faber A, Willerton E, Clymer SR, MacDermid SM, Weiss HM. Ambiguous absence, ambiguous presence: A longitudinal study of military families in war time. Journal of Family Psychology. 2008;22:222–230. doi: 10.1037/0893-3200.22.2.222. [DOI] [PubMed] [Google Scholar]
- Ferrier-Auerbach AG, Erbes CR, Polusny MA, Rath M, Sponheim S. Predictors of emotional distress reported by soldiers in the combat zone. Journal of Psychiatric Research. 2010;44:470–476. doi: 10.1016/j.jpsychires.2009.10.010. [DOI] [PubMed] [Google Scholar]
- Forgatch MS, DeGarmo DS. Parenting Through Change: An effective prevention program for single mothers. Journal of Consulting and Clinical Psychology. 1999;67:711–724. doi: 10.1037//0022-006x.67.5.711. [DOI] [PubMed] [Google Scholar]
- Forgatch MS, Patterson GR, DeGarmo DS, Beldavs ZG. Testing the Oregon delinquency model with 9-year follow-up of the Oregon Divorce Study. Development and Psychopathology. 2009;21(02):637–660. doi: 10.1017/S0954579409000340. [DOI] [PubMed] [Google Scholar]
- Frick PJ. The Alabama parenting questionnaire. Unpublished instrument, University of Alabama; 1991. [Google Scholar]
- Fuls SJ. Dissertation Abstracts International Section A: Humanities and Social Sciences. 1995. Parenting attitudes and behaviors in Vietnam veterans. [Google Scholar]
- Galovski T, Lyons JA. Psychological sequelae of combat violence: A review of the impact of PTSD on the veteran's family and possible interventions. Aggression and Violent Behavior. 2004;9(5):477–501. [Google Scholar]
- Gartstein MA, Fagot BI. Parental depression, parenting and family adjustment, and child effortful control: Explaining externalizing behaviors for preschool children. Journal of Applied Developmental Psychology. 2003;24(2):143–177. [Google Scholar]
- Glenn DM, Beckham JC, Feldman ME, Kirby AC, Hertzberg MA, Moore SD. Violence and hostility among families of Vietnam veterans with combat-related posttraumatic stress disorder. Violence and Victims. 2002;17:473–489. doi: 10.1891/vivi.17.4.473.33685. [DOI] [PubMed] [Google Scholar]
- Goff BSN, Crow JR, Reisbig AMJ, Hamilton S. The impact of individual trauma symptoms of deployed soldiers on relationship satisfaction. Journal of Family Psychology. 2007;21(3):344. doi: 10.1037/0893-3200.21.3.344. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA: Journal of the American Medical Association. 2006;295(9):1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hunsley J, Best M, Lefebvre M, Vito D. The seven-item short form of the Dyadic Adjustment Scale: Further evidence for construct validity. American Journal of Family Therapy. 2001;29:325–335. [Google Scholar]
- Hunsley J, Pinsent C, Lefebvre M, James-Tanner S, Vito D. Construct validity of the short forms of the Dyadic Adjustment Scale. Family Relations. 1995;44(3):231–237. [Google Scholar]
- Jacobson IG, Ryan MAK, Hooper TL, Smith TC, Amoroso PJ, Boyko EJ, et al. Alcohol use and alcohol-related problems before and after military combat deployment. Journal of American Medical Association. 2008;300:663–675. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan B, Marmar CR, Fairbank JA, Schlenger WE, Kulka RA, Hough RL, et al. Problems in families of male Vietnam veterans with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1992;60(6):916–926. doi: 10.1037//0022-006x.60.6.916. [DOI] [PubMed] [Google Scholar]
- Kaniasty K, Norris FH. Longitudinal linkages between perceived social support and posttraumatic stress symptoms: Sequential roles of social causation and social selection. Journal of Traumatic Stress. 2008;21(3) doi: 10.1002/jts.20334. [DOI] [PubMed] [Google Scholar]
- King DW, Taft C, King LA, Hammond C, Stone ER. Directionality of the association between social support and Posttraumatic Stress Disorder: A longitudinal investigation 1. Journal of Applied Social Psychology. 2006;36(12):2980–2992. [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation. NY, NY: Psychology Press; 2008. [Google Scholar]
- McCarroll JE, Thayer LE, Liu X, Newby JH, Norwood AE, Fullerton CS, et al. Spouse abuse recidivism in the U.S. Army by gender and military status. Journal of Consulting and Clinical Psychology. 2000;68(3):521–525. [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA: Journal of the American Medical Association. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Monson CM, Price JL, Rodriguez BF, Ripley MP, Warner RA. Emotional deficits in military-related PTSD: An investigation of content and process disturbances. Journal of Traumatic Stress. 2004;17:275–279. doi: 10.1023/B:JOTS.0000029271.58494.05. [DOI] [PubMed] [Google Scholar]
- Monson CM, Taft CT, Fredman SJ. Military-related PTSD and intimate relationships: From description to theory-driven research and intervention development. Clinical Psychology Review. 2009;29:707–714. doi: 10.1016/j.cpr.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. MPlus: Statistical Analysis with Latent Variables Users Guide. 5th ed. Los Angeles, CA: StatModel; 2007. [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Palmer C. A theory of risk and resilience factors in military families. Military Psychology. 2008;20(3):205–217. [Google Scholar]
- Patterson G. Coercive family process. Eugene, OR: Castalia Publishing Co; 1982. [Google Scholar]
- Patterson G, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. American Psychologist. 1989;44(2):329–335. doi: 10.1037//0003-066x.44.2.329. [DOI] [PubMed] [Google Scholar]
- Patterson GR. Next Generation of PMTO Models. The Behavior Therapist. 2005;28:27–33. [Google Scholar]
- Polusny MA, Erbes C, Arbisi P, Thuras P, Reddy MK, Erickson D, et al. Prospective predictors of resilience in OIF deployed National Guard soldiers. Paper presented at the APA 2008 Convention; Boston, MA.2008. [Google Scholar]
- Prigerson HG, Maciejewski PK, Rosenheck RA. Combat trauma: Trauma with highest risk of delayed onset and unresolved PTSD symptoms, unemployment, and abuse among men. Journal of Nervous and Mental Disease. 2001;189:99–108. doi: 10.1097/00005053-200102000-00005. [DOI] [PubMed] [Google Scholar]
- Renshaw KD, Rodrigues CS, Jones DH. Psychological symptoms and marital satisfaction in spouses of Operation Iraqi Freedom veterans. Journal of family psychology. 2008;22:586–594. doi: 10.1037/0893-3200.22.3.586. [DOI] [PubMed] [Google Scholar]
- Riggs DS, Byrne CA, Weathers FW, Litz BT. The quality of the intimate relationships of male Vietnam veterans: Problems associated with posttraumatic stress disorder. Journal of Traumatic Stress. 1998;11:87–101. doi: 10.1023/A:1024409200155. [DOI] [PubMed] [Google Scholar]
- Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric Properties of the PTSD Checklist--Civilian Version. Journal of Traumatic Stress. 2003;16(5):495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- Ruggiero KJ, Rheingold AA, Resnick HS, Kilpatrick DG, Galea S. Comparison of two widely used PTSD-screening instruments: Implications for public mental health planning. Journal of Traumatic Stress. 2006;19(5):699–707. doi: 10.1002/jts.20141. [DOI] [PubMed] [Google Scholar]
- Samper RE, Taft CT, King DW, King LA. Posttraumatic stress disorder symptoms and parenting satisfaction among a national sample of male Vietnam veterans. Journal of Traumatic Stress. 2004;17(4):311–315. doi: 10.1023/B:JOTS.0000038479.30903.ed. [DOI] [PubMed] [Google Scholar]
- Sharpley CF, Rogers HJ. Preliminary validation of the Abbreviated Spanier Dyadic Adjustment Scale: Some psychometric data regarding a screening test of marital adjustment. Educational and Psychological Measurement. 1984;44(4):1045. [Google Scholar]
- Solomon Z, Waysman M, Levy G, Fried B, Mikulincer M, Benbenishty R, et al. From front line to home front. Family Process. 1992;31:289–302. doi: 10.1111/j.1545-5300.1992.00289.x. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38(1):15–28. [Google Scholar]
- Tanielian T, Jaycox LH. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Santa Monica, CA: Rand; 2008. [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD checklist: Reliability, validity, and diagnostic utility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies.1993. [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33(9):1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Wothke W. Longitudinal and multi-group modeling with missing data. In: Little TD, Schnabel KU, Baumert J, editors. Modeling longitudinal and multiple group data: Practical issues, applied approaches, and specific examples. Mahwah, NJ: Erlbaum; 2000. pp. 269–281. [Google Scholar]