Abstract
Introduction
Recent studies have demonstrated that e-prescribing takes longer than handwriting. Additional studies documenting the perceived efficiencies realized from e-prescribing from those who have implemented electronic prescribing are warranted.
Methods
We used a mixed method study design. We report on qualitative date from 64 focus groups with clinicians and office staff from six US states. Participants used one of six e-prescribing software packages. Qualitative data from the focus groups (276 participants) were coded and analyzed using NVivo software. Quantitative data regarding perceived efficiencies were extracted from a survey of 157 clinicians using e-prescribing.
Results
Perceptions of e-prescribing included 64% reporting e-prescribing as very efficient. The next closest method was computer generated fax and prescriptions in which ~25% rated the method as very efficient. Improvements in workflow and record keeping were noted. Perceived efficiencies were realized by decreased errors, availability of formularies at the point of prescribing and refill processing. Perceived inefficiencies noted included the need for dual systems owing to regulations preventing e-prescribing of scheduled medications as well as those introduced with incorrect information on formularies, pharmacy used, and warnings.
Discussion
Overwhelmingly, clinicians and their staff confirmed the perceived efficiencies realized with the adoption of e-prescribing. Perceived efficiencies were realized in knowing formularies, processing refills, and decreasing errors. Opportunities to improve efficiencies could be realized by assuring correct information in the system.
1. INTRODUCTION
According to the largest e-prescribing network in the United States (SureScripts, a privately owned, for-profit commercial entity), ~156,000 prescribers used some variant of electronic prescribing in 2009 (http://www.surescripts.com; accessed on June 1, 2010). Electronic prescribing involves direct communication via computers in physician offices to pharmacies (e.g. community or mail order). Federal initiatives have stimulated increases in electronic prescribing and it is anticipated to take on a greater role in patient management.1 Electronic prescribing has been touted to increase efficiencies and improve patient safety.2
While some argue for the potential for electronic prescribing to increase efficiencies3, research regarding the business justification with respect to efficiency that could be gained with electronic prescribing is sparse. Obstacles to the successful implementation of e-prescribing software in physician office practices are real and include cost of implementation (financial, personnel, and time costs), lack of financial incentives, lack of standardized software, and lack of systematic evidence of effectiveness.4 Indeed, in Sweden, the major potential success factor to implementation was the potential for saving physician time.5 Yet, a recent study6 demonstrated that e-prescribing takes longer than handwriting and e-prescribing at the point of care takes longer than e-prescribing in offices/workstations. This study suggested that e-prescriptions took on average 20 seconds longer than hand written prescriptions, while the other suggested no improvements.7 Studies documenting the efficiencies in the prescription process beyond the act of writing (e.g. dealing with prior authorizations, communicating with the pharmacy regarding formulary changes, pulling charts) are warranted. Understanding the perceptions of efficiencies of e-prescribing from those who have implemented the systems may be of value. The present study was designed to investigate perceived efficiencies of e-prescribing (which may or may not correlate with actual efficiencies).
In the context of a large mixed-method study to evaluate proposed standards for specific functions of electronic prescribing (e.g. medication history, refills requests, cancel/change transactions, and prior authorization), we collected qualitative and quantitative information from physician practices in six states, in various settings (e.g. solo practices to HMO), each setting using one of six different electronic prescribing software solutions. This report focuses on healthcare providers’ opinions about the role of e-prescribing applications in improving efficiency.
2. METHODS
2.1 Funder and ethics
In fall of 2005, the Agency for Healthcare Research and Quality put out a call for proposals for one-year studies on e-prescribing standards required under the Medicare Modernization Act.1 The initial request for proposals required information related to the proposed requirements under the Medicare Modernization Act and as such requested studies focusing on Medicare eligible patients. The Brown University Institutional Review Board and the New England Institutional Review Board approved the study protocol. The mixed-methods study consisted of surveys with providers, patients and staff, as well as both interviews and focus groups in these practices. Physicians participating in the study received a $500 incentive. The incentive was consistent with the extensive nature of the study protocol. The protocol included completion of a baseline survey regarding the practice, completion of surveys for clinician and non-clinician staff, collection of patient surveys, collection of a log of calls between the clinician and the pharmacy, a ½ day to full day onsite observation period in which the study team conducted focus groups, performed informant interviews, audio recorded clinical encounters, observed the office work flow, agreement to be a beta test site for implementation of changes to e-prescribing software, and participation in follow-up survey of clinical staff.
2.2 Participating E-Prescribing systems
In 2005, we partnered with SureScripts, LLC to conduct this study. First, SureScripts identified states with the highest electronic prescribing activity in their network (though at the time this activity was still less than 2% of all prescriptions in each state), and we then subselected the following states to provide geographic diversity: Florida, Massachusetts, New Jersey, Nevada, Rhode Island, and Tennessee. The e-prescribing vendors active in these states and willing to partner with the research team were: OnCallData, InstantDX, LLC, Gaithersburg, MD; in Rhode Island, PocketScript, Zix Corporation, Dallas, TX; in Massachusetts and New Jersey; Rcopia, DrFirst, Inc., Rockville, MD in Massachusetts; Care360, Medplus, Inc., Mason, OH in New Jersey and Florida; eMPOWERx, GoldStandard Multimedia, Inc., Tampa, FL in Florida; and Touchworks, AllScripts, LLC, Chicago, IL in Nevada and Tennessee. SureScripts developed subcontracts with each vendor which varied in the scope of e-prescribing standards needed to be tested; all physician software system vendors were required to assist in recruitment of ambulatory care practices with a patient-mix of at least 25% Medicare eligible patients. The Brown University Institutional Review Board approved the participation agreements (designed by the research team). We provided recruitment packets and training of information in the recruitment packets for each company. The resulting practices represented a convenience sample. Our first contact with practices was when we received signed participation agreements. Thus, we are unable to estimate participation rates among potentially eligible practices. In order to bring together major competitors to collaborate on this important study of e-prescribing standards, we vowed never to disclose the findings in relation to their identity. Thus, we are unable to reveal the particular identities of the vendors in analyses stratified by vendor.
2.3 Subjects
As the study was meant to generate information relevant for the Medicare Modernization Act, we required that physician practices have a patient-mix of at least 25% Medicare eligible patients. Physicians participated in two surveys, conducted a survey of their patients, participated with partners and office staff in the focus group, tested the software changes, and allowed on-site observation lasting ½ day. Focus groups and interviews were conducted in 64 practices with at least some experience using electronic prescribing. Exact length of experience with e-prescribing was not obtained on the surveys. All data collection occurred before changes to the electronic prescribing software were made and testing of new electronic prescribing standards was conducted.
2.4 Clinician surveys
The clinician survey was available in paper form and on the web, with most of the 157 respondents using the latter. The survey included questions relating to the use and perceptions of the impact of e-prescribing on efficiency and improved workflow. One question evaluated efficiencies of e-prescribing to other methods: “From your perspective, how does using the e-prescribing software compare to previous methods with respect to efficiency of care (e.g. increased productivity)?” Valid responses were much worse, somewhat worse, no change, somewhat better, and much better. We also asked respondents to rate different methods of prescribing from their perspective (from very inefficient to very efficient). We included separate questions for e-prescribing, hand-written prescriptions, faxing, computer generated fax, phone, and computer-generated printed prescriptions.
2.5 Development of the focus group guide
Our research team developed a semi-structured facilitator’s guide with input from pharmacists, physicians, software vendors, and researchers. The major subject areas explored were: 1) e-prescribing usability, implementation barriers, and impact on patient safety; 2) functionality- ways it makes job easier, mechanisms to improve safety and efficiency; 3) medication history access; and 4) formulary and benefit information. Probes were developed for each domain. The protocol was piloted at Brown University. We modified the protocol based on the pilot findings before launching the study in the six states. Previously, we have reported on refill functionality8, drug alerts9, patient communication10, and patient safety.11
2.6 Conduct of the sessions
Our research team went on site to each of 64 practices between April and August 2006. We conducted on-site focus groups or individual interviews (if appropriate in solo practices) with 276 clinicians and staff. The trained research assistants held the focus groups and interviews at a time convenient to the practice (e.g. before the medical practice opened in the morning, at lunch, or after hours). To set a relaxed atmosphere and provide an incentive for participation, we provided a meal. Participants provided written informed consent forms and completed demographic surveys. An open-ended approach was used for eliciting information about the experience of using e-prescribing, including both benefits and barriers. Focus group participants described their experiences with e-prescribing software. Suggestions and improvements were solicited as probes when they were not spontaneously provided. Additional probes included queries about particularly helpful or difficult aspect of the software, along with other resources that would be helpful. Additionally, general probing was conducted using facilitative questions such as “Can you tell me more about that? Do you have any other opinions? Is there anything else you’d like to say?” Clarification strategies were also employed by facilitators to summarize participant statements, and check for accuracy, such as “when you say _____, what do you mean by that?”
Focus groups and interviews lasted on average about one hour, were digitally recorded, and professionally transcribed. Research assistants then reviewed each transcript for potential errors and corrected them as needed.
2.7 Data analysis
For qualitative data analysis, an extensive hierarchical coding structure and codebook were initially developed to handle the large volume of qualitative data. This initial structure was developed based on the focus group protocol and review of initial transcripts, and revised and/or expanded during active coding using NVivo qualitative data management software.12 A codebook was created to define all categorical “nodes” and their relationships. Coders were rigorously trained in node definitions, overall coding structure, and coding protocols. Consistency in coding across team members was maintained by: 1) intensive training sessions (to learn about the coding process and node definitions); 2) coding transcripts as a group; 3) regular coding meetings; 4) spot-checking of coded transcripts; 5) node review by the investigator and regular feedback to coders; and 6) 19% of the transcripts were coded independently by more than one research assistant for comparative analysis of coding results.
For quantitative data analysis, we created cross-tabulations of perceptions of efficiency by clinician status (clinician vs. non-clinician) as well as e-prescribing software vendor. When appropriate, chi square analyses were conducted. If cell sizes were less than 5, we collapsed categories into conceptually meaningful groups to enable chi square analyses.
3 RESULTS
3.1 Participant characteristics
Sixty four focus group sessions were held in spring of 2006 over a period of several months. A total of 276 persons participated in the focus groups. In the 64 focus groups, 36% was office staff involved in the e-prescribing process and the remainder was clinicians. Internal medicine (45%) and family medicine (39%) dominated the sample. Nearly one quarter were solo practices.
3.2 Survey results
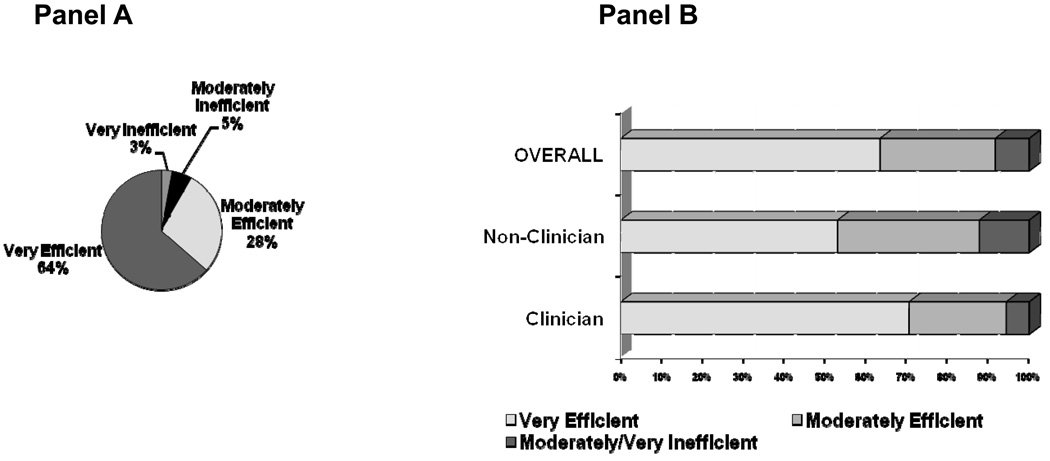
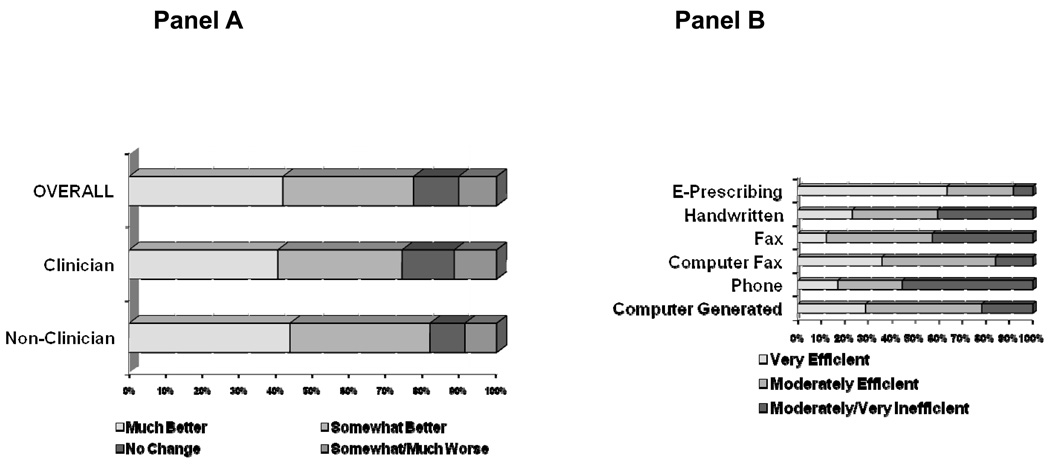
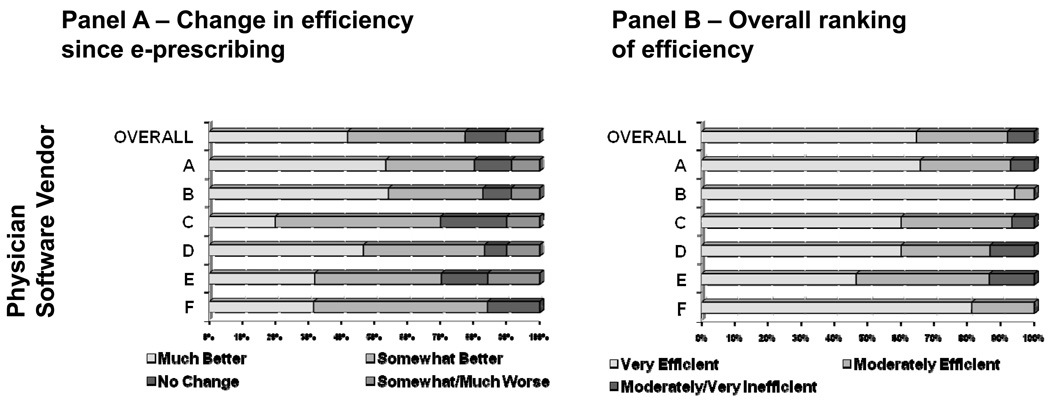
Figure 1 shows the perceptions of efficiency of the physicians and their staff. Panel A shows that 64% rated e-prescribing as very efficient and 3% thought it was very inefficient. Panel B shows that physicians were more likely to rank e-prescribing as very efficient (71%) relative to non-clinicians (53%) (P-value=0.007). Figure 2 shows in Panel A that both clinicians and non-clinicians agreed that e-prescribing made the prescribing process much better. Forty-one percent of clinicians ranked the prescribing process much better compared to 44% of non-clinicians (P-value=0.50). Less than 10% reported that e-prescribing made things somewhat or much worse. Panel B shows the efficiency ranking of each prescribing method. The rank order of prescribing methods scored as very efficient was: e-prescribing (64%), computer fax (26%), computer (24%), hand-written (21%), phone (17%) and fax (11%). Prescribing over the phone was the method most often reported as moderately or very inefficient (54%) and e-prescribing was the least likely reported (8%). Figure 3 shows the variations in perceptions of e-prescribing efficiency by e-prescribing software vendor. In Panel A, regardless of specific vendor used, the majority of respondents indicated that e-prescribing made the prescribing process at least somewhat better. Variation in the proportion of users reporting that e-prescribing made things much better existed, but was not statistically significant. Twenty percent of users of Vendor C ranked that e-prescribing made things much better and among users of Vendors A and B ~54% said much better. Panel B shows that ~60% viewed e-prescribing as very efficient. Estimates of efficiency ranged from 94.1% for Vendor B to 60% Vendors C and D (P-value=0.001).
Figure 1.
Perspective on efficiency of e-prescribing overall (Panel A) and by clinician status (Panel B)
Figure 2.
Change in efficiency of care (e.g., increased workflow & productivity) since e-prescribing adoption by clinician status (Panel A) and efficiency of e-prescribing versus other prescribing methods (Panel B)
Figure 3.
Change in efficiency of care since e-prescribing by software vendor (Panel A) an overall ranking of efficiency of e-prescribing by software vendor (Panel B)
3.3 Focus group findings
Table 1 summarizes the findings from the focus groups. Participants reported that e-prescribing is “efficient” and “timesaving”. The efficiency gains realized were identified as related to 1) “decreased errors and decreased calls to clarify prescriptions” which cut down time spent on the phone with the pharmacy; 2) refill processing; and 3) knowledge of formularies and prior authorizations. Being able to track when prescriptions were written allowed refills to be processed in a timely and efficient basis. Knowing which medications were on formulary and which required prior authorization improved efficiencies in workflow.
Table 1.
Summary points relating to efficiency from the focus groups
| Efficiency gains |
| Saves time related to resolving errors |
| Phone calls with pharmacy reduced and communication improved |
| Refill processing is streamlined |
| Workflow is more efficient; reduced redundancy |
| Knowing formularies and prior authorizations at the point of prescribing saves time |
| Increased time with patients |
| Improved record keeping |
| Inefficiencies realized (computer and human errors) |
| Prescriptions not being received or having delayed receipt by the pharmacy resulting in frustrated patient calls |
| Slow functionality of the software during busy times |
| Patients changing pharmacies, not informing practice and prescriptions ending up in the wrong place |
| Repeated warnings produced by the software being incorrect or distracting |
| Insurance formularies not being kept up to date or being incorrect |
| Hidden cost |
| Needing staff skilled in computer issues related to e-prescribing |
Participants noted that e-prescribing improved organization within the practice, including that it helped organize prescription and refill management, improved record keeping, and made the practice more efficient. Consider this exchange among providers during a focus group:
I think we were a little nervous with something computer generated (how's it going to work?), but it's been really a big cost savings and timesaving.
We thought it was going to take more time, but it didn't.
If anything it saves us time.
Another participant commented: “I think it's been a big help for the office. I think it's made prescription refills go a lot easier, and we keep track of them better, and we can go back and look at them easier. It's made things a lot faster.”
Clinicians also appreciated the efficiency of the technology itself, including that it allowed them to write and send prescriptions directly to the pharmacy while they were meeting with patients and also that it allowed them to approve prescriptions from remote locations, for instance from home, or when working from a different office. These factors were perceived as having a positive impact on workflow. Other benefits to workflow included cutting down on phone calls and paper work. For example, when asked “how would you say the practice changed once the e-prescribing was implemented…both with the patients and the internal workflow?” Clinicians answered that they felt it significantly reduced paperwork and phone calls and significantly improved workflow. In this example, a clinician describes how the workflow is changed by e-prescribing:
“if you look at the total system, it's much less time for the pharmacist and for us and definitely a shifting off the front desk to the medical assistant and the doctor, but even for me I think it's less time because there's less redundancy.”
Participants also commonly commented on the ability of e-prescribing software to provide updated information about medication formularies. Knowing what drugs are covered under which formularies, and when a generic equivalent is a better choice, allowed clinicians to prescribe drugs that they will actually receive. Additionally, having current formulary information saves clinician and office staff time – “[prior to e-prescribing] half of my day is taken up calling back different prescriptions because it's not covered under somebody's insurance” – and allows clinicians to consider the financial needs of patients for whom a generic or lower tier drug is a more economical, but still effective choice. Another software feature that improved the efficiency of the workflow was information about prior authorization. This feature was noted to improve the efficiency of the prescribing process because the physician would know before suggesting a medication that it would require this additional work.
This clinician describes the often frustrating process of finding formulary approved drugs before and after implementing e-prescribing:
One of the biggest benefits I've noticed is the ability to prescribe a medication that you know is on formulary. I think one of the most difficult, time consuming events we have, especially when you're dealing with HMO's, is there are specific formularies… They change it every month, every three months, six months. You don't have a hardcopy of changes. If you do, it's always a year old or expired. I think most time consuming for both the physicians and staff is getting those calls or faxes from the pharmacy stating this drug is not covered or needs prior authorization. Then you have to be in communication with the patient to find out they're not trying to defraud, to find out what's available. Sometimes it's trial and error. You just prescribe one after another after another until you found one that was covered, and then the patient could not tolerate [it]. So that's really been the biggest thing that I've noticed, getting a drug right from the get-go that is going to be available … and avoid all troubleshooting down the road.
Participants also felt that their use of electronic prescribing made them look “high tech,” “efficient” and “well informed” and that it was particularly helpful to patients who did not have to worry about losing their prescriptions. Another benefit for the patients is that the oft-cited efficiency of e-prescribing increasing the available time physicians have to spend with them. This is particularly true when a patient has multiple prescriptions, say a dozen or more. Filling out that many paper prescriptions is time consuming, but e-prescribing them is handled very quickly.
The participants recognized that often the problems stemming from glitches in the e-prescribing required extra and unnecessary time to resolve them. Such instances could have been from delays on the network, technical bugs in the software, or patients not informing physician’s offices of a change in pharmacy.
I guess the biggest problem has been that we feel like we’re doing the thing twice because we’re getting phone calls from pharmacies saying that they’re not receiving it, or we’re getting another fax saying that they haven’t received it knowing that we have done it. And we don’t like to do things twice. …And patients‥ [don’t] like it because they’ll go to pick it up at a pharmacy, it won’t be there because the pharmacist claims that we didn’t send it even though we know we did. So that’s a problem. And that’s happened numerous times. And you know, after four or five times it gets to be a little upsetting.
Some physicians found it was easier, less time consuming, and caused fewer problems to simply hand write a prescription: It’s easier to sit down frankly to write the amoxicillin on a piece of paper and hand it to the patient. There were several aspects of the e-prescribing process that participants considered to be time consuming. Here, an office staff member explains how the refill system works:
The way that our office works [e-prescribing has]caused a little bit more work for the doctor because in the old days I’d get a message, and the patient said they had a sore throat and wanted something called in. I would just write the name of the med, the number and hand it to the nurse, and she would call it in and take care of the rest. Now I have to take that message, bring the patient up, write the script in the system and go to the next one. So it’s more time consuming for the doc.
Participants also reported being slowed down by the process of e-prescribing itself, saying that it took, for example, 45 seconds more per prescription, or two minutes more time per patient to implement. Over the course of a busy day, these relatively small amounts of time add up. This participant describes the process of using the computer system for a prescription.
…you have to bring up the patient [electronic record]. If the medication is already there you click ‘prescribe’, or you could just hit ‘refill’. But say it’s a new medication. Bring up the screen. Put in the name of the medication. Pick the right medication, the right strength- so another screen from there. You can put in the directions. Then you say okay.
The process is even more time consuming when the patient is new to the practice and first has to be entered into the system. One clinician, who had a practice with a high turnover of patients, found this particularly frustrating because the time and effort it took to input the patient record was lost if that patient is not seen again. Further, one inefficiency that was repeatedly mentioned was the need for multiple systems to address the inability to e-prescribe scheduled medications owing to federal regulations.
A hidden cost was identified as a result of the changing composition of the office staff. Although there were no indications that practices would have to increase the size of their staff, some practices did indicate that replacement personnel were hired specifically to serve as the point person for computer issues around electronic prescribing. These personnel became experts on the nuances of the computer hardware and electronic prescribing software and interfaced directly with the software vendor and other computer support services to address any problems. Although there were no explicit remarks about the salary costs for such a skilled person, such personnel may indeed be more expensive than traditional administrative staff.
DISCUSSION
Our study demonstrated that the perceived efficiencies of e-prescribing have little to do with the actual amount of time required to physically write a prescription. Rather, physicians and their staff suggested that efficiencies were gained by reducing redundancy, minimizing calls from pharmacy relating to prescription choices not being on formulary, reduced time spent on prior authorizations, reduced time spent processing refills, and overall better workflow. Providers in our study reported decreased time resolving prescription issues with pharmacy, as well as reduced time dealing with prior authorizations. Further, we have previously reported on decreased time spent performing refill requests.8 These findings are not consistent with two recent studies which used time and motion methods.6,7 One explanation may be that our findings were from 2006 and represented the “early days” of e-prescribing. Although unlikely, it may be that efficiencies of e-prescribing have deteriorated as more users are on the network. Indeed, it is more likely that familiarity breeds efficiency. Inconsistencies with the previous literature may be due to the fact that most of the users in our study were experienced e-prescriber users who were the early adopters of the technology. Our data were based on self-report but considered not just time to write prescriptions, but also the time related to processing prescriptions including pulling of charts and answering phones.
Our findings support the notion that not all products are created equally. Currently, over 200 vendors provide e-prescribing options (e.g. stand alone software and bundled in the electronic medical record) (http://www.surescripts.com; accessed on June 1, 2010). Clinician reports on the efficiency of their products were high, but did vary somewhat across the six vendors. The extent to which these findings would extend to the 200 or more different products available are unknown owing to the differences in software standards and different data management systems.13 Further, the varied reports in efficiency by software vendor may also be a function of how e-prescribing was implemented within these practices. This alternative explanation cannot be ruled out. Nevertheless, physician practices would greatly benefit from guidance regarding the quality of e-prescribing software and expected efficiency gains in a market with no real dominating manufacturer’s presence.
An additional area of functionality that we found influenced efficiency of e-prescribing was the availability of patients’ prescription formulary and eligibility information in real time during an office visit. Clinicians in our study found this feature to be integral to increasing the efficiency and workflow related to the prescribing process. They reported reduced time on the phone with pharmacy, as well as reduced time relating to prior authorizations. Indeed, electronic requests for prescription benefit information have increased 284% from 2008 to 2009. (http://www.surescripts.com; accessed on June 1, 2010). Clinicians in our study appreciated knowing more about costs of medications and felt that this knowledge could ultimately improve adherence because they would be better able to prescribe cost-effective treatments. Inefficiencies in e-prescribing stemmed from inaccurate information. Methods to improve the integration of accurate and up to date formulary information in e-prescribing software would improve efficiencies.
An area of significant inefficiency that was noted related to the prescribing of controlled substances. Physicians may be confused about the regulations regarding what types of prescriptions may be e-prescribed.14 In previous work by our group, physicians noted their frustration with the need for multiple prescribing methods owing to the inability to e-prescribe controlled substances.15 Many preferred to forgo true computer-to-computer e-prescribing in favor of one method (faxing by computer) which covered all prescribing needs. Others who e-prescribed noted frustration with having to maintain dual systems to e-prescribe controlled substances. Calls for changes in US legislation16 and rigorous testing of systems have resulted in changes to regulations that should minimize this concern. Further inefficiencies stemmed from patients not updating physician offices when changing pharmacy and apparently “lost” prescriptions on the network. Physician offices may need to change intake procedures to also ask if there are updates to pharmacy used to prevent some of these issues.
We interpret these data with caution. Owing to the nature and timing of the study, we used a convenience sample. The software vendors participating were open to helping us test the functionality of new e-prescribing standards. By the nature of our agreement with the vendors, we promised not to disclose the vendors’ identities in vendor-specific analyses. Regardless, in 2010, the functionalities of each particular product are likely to have changed in the four years since our study. From this group, we purposefully selected states with high volume e-prescribing (relative to the rest of the country, but still very low) and because we could only include six states, we selected states to also provide geographic diversity. In doing so, we were able to represent a variety of e-prescribing vendors (6 vendors), practice settings (HMO, solo practitioners, etc), and experience with e-prescribing (e.g. the earliest adopters and some new users). Thus, in selecting a convenience sample, we may be presenting an overly optimistic view of the efficiencies of e-prescribing as familiarity breeds efficiency. That said, we must emphasize that e-prescribing was still in a nascent stage in 2006 in the US. We realize that this sample may have over-represented clinician “early adopters” who are highly experienced with e-prescribing. However, we did not specifically ask individual physicians the length of experience they had with each product and as such we do not know how the experience of these clinicians compares to others. Further, some may be concerned that the incentive ($500) stimulated more favorable responses regarding e-prescribing. The multistage protocol involved a myriad of activities including several baseline and follow-up surveys, patient logs, onsite observation, focus groups, and maintaining logs of interaction between the office and the pharmacy. Thus, we believed the incentive was appropriate for the work involved. Lastly, the convenience sample may have included practices highly engaged in e-prescribing, as it may well be that software vendors approached their best clients first. One vendor (C) tried to engage new users into the study; the remainder likely engaged experienced users. Nevertheless, the findings consistently revealed that the participants were highly engaged to provide critical feedback so that improvements in the processes could be made. Although the participants are likely representative of the most experienced e-prescribing users in primary care settings, we believe the sample was appropriate for the mixed-method approach used to address the study question. Lastly, this particular study was intended to provide information regarding e-prescribing for the Medicare population (mostly over 65 years of age). As such, the practices included in the study were mostly family medicine and internal medicine. It may well be that our findings overestimate the efficiencies of e-prescribing owing to the high proportion of elderly patients likely taking more medications than younger populations. We are not able to generalize these findings to specialty practices such as pediatrics, surgery, and other specialties.
E-prescribing adoption appears to have reached a turning point, with accelerated adoption expected in the US with economic stimulus initiatives. This study documents the perceptions of efficiencies from a diverse group of practitioners using varied software products. As the use of e-prescribing spreads, consumers, non-clinical staff and physicians are likely to expect full integration of e-prescribing within the prescribing processes in ambulatory care. For most users of e-prescribing, the efficiencies gained clearly outweigh the concerns.
Supplementary Material
ACKNOWLEDGMENTS
We gratefully acknowledge the assistance of Ken Whittemore, RPh, MBA, and Ajit Dhavle, PharmD, MBA, of SureScripts. This study was funded by the Agency for Healthcare Research and Quality, Department of Health and Human Services (Grant # 1 U18 HS016394-01 entitled Maximizing the effectiveness of e-prescribing between physicians and community pharmacies). The funder had no role in the study design, collection, analysis and interpretation of data, writing of the manuscript and decision to submit for publication. We also acknowledge the support of the VCU Clinical and Translational Science Award (1UL1 RR031990-01).
REFERENCES
- 1.Bell DS, Friedman MA. E-Prescribing and the Medicare Modernization Act: Paving the On-Ramp to Fully Integrated Health Information Technology. Health Affairs. 2005 Sept/Oct;24(5) doi: 10.1377/hlthaff.24.5.1159. [DOI] [PubMed] [Google Scholar]
- 2.Lawrence D. Steps forward on e-prescribing. As e-prescribing becomes more widespread, even hospital organizations without full EMR implementation are seeing gains in clinician workflow and patient safety. Healthc Inform. 2010 May;27(5):24–26. [PubMed] [Google Scholar]
- 3.Weingart SN, Simchowitz B, Shiman L, Brouillard D, Cyrulik A, Davis RB, Isaac T, Massagli M, Morway L, Sands DZ, Spencer J, Weissman JS. Clinicians' assessments of electronic medication safety alerts in ambulatory care. Arch Intern Med. 2009 Sep 28;169(17):1627–1632. doi: 10.1001/archinternmed.2009.300. [DOI] [PubMed] [Google Scholar]
- 4.Hor CP, O'Donnell JM, Murphy AW, O'Brien T, Kropmans TJ. General practitioners' attitudes and preparedness towards Clinical Decision Support in e-Prescribing (CDS-eP) adoption in the West of Ireland: a cross sectional study. BMC Med Inform Decis Mak. 2010 Jan 12;10:2. doi: 10.1186/1472-6947-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steinschaden T, Petersson G, Astrand B. Physicians' attitudes towards eprescribing: a comparative web survey in Austria and Sweden. Inform Prim Care. 2009;17(4):241–248. doi: 10.14236/jhi.v17i4.743. [DOI] [PubMed] [Google Scholar]
- 6.Devine EB, Hollingworth W, Hansen RN, Lawless NM, Wilson-Norton JL, Martin DP, Blough DK, Sullivan SD. Electronic prescribing at the point of care: a time-motion study in the primary care setting. Health Serv Res. 2010 Feb;45(1):152–171. doi: 10.1111/j.1475-6773.2009.01063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hollingworth W, Devine EB, Hansen RN, Lawless NM, Comstock BA, Wilson-Norton JL, Tharp KL, Sullivan SD. The impact of e-prescribing on prescriber and staff time in ambulatory care clinics: a time motion study. J Am Med Inform Assoc. 2007 Nov–Dec;14(6):722–730. doi: 10.1197/jamia.M2377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldman RE, Dube C, Lapane KL. Beyond the basics: Refills by electronic prescribing. Int J Biomedical Informatics 2010. 2010 Jul;79(7):507–514. doi: 10.1016/j.ijmedinf.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 9.Lapane KL, Waring ME, Schneider KL, Dubé C, Quilliam BJ. A mixed method study of the merits of e-prescribing drug alerts in primary care. J Gen Intern Med. 2008 Apr;23(4):442–446. doi: 10.1007/s11606-008-0505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lapane KL, Dubé CE, Schneider KL, Quilliam BJ. Misperceptions of patients vs. providers regarding medication-related communication issues. Am J Manag Care. 2007 Nov;13(11):613–618. [PubMed] [Google Scholar]
- 11.Lapane KL, Waring ME, Schneider KL, Dube C. E-prescribing and patient safety: Results from a mixed method study. Am J Ph Ben. 2010 Nov/Dec; [PMC free article] [PubMed] [Google Scholar]
- 12.NVivo qualitative data analysis software; QSR International Pty Ltd. Version 8. 2008. [Google Scholar]
- 13.Bell DS, Marken RS, Meili RC, Wang JC, Rosen M, Brook RH the RAND Electronic Prescribing Expert Advisory Panel. Recommendations For Comparing Electronic Prescribing Systems: Results Of An Expert Consensus Process. Health Affairs. 2004 Jan–Jun; doi: 10.1377/hlthaff.w4.305. Suppl Web Exclusives:W4-305-17. [DOI] [PubMed] [Google Scholar]
- 14.Grossman JM, Gerland A, Reed MC, Fahlman C. Physicians’ Experiences Using Commercial E-Prescribing Systems. Health Affairs. 2007;26(3):w393–w404. doi: 10.1377/hlthaff.26.3.w393. [DOI] [PubMed] [Google Scholar]
- 15.Lapane KL, Whittemore K, Rupp MT, Dube C, Jackson T, Dhavle A. Final Progress Report submitted to AHRQ on January 28, 2007. Maximizing the effectiveness of e-prescribing between physicians and community pharmacies. [Google Scholar]
- 16.Lapane KL, Quilliam BJ, Dore DD. Roadblock on the health IT superhighway: e-prescribing and the Controlled Substances Act. J Opioid Manag. 2007 Jul–Aug;3(4):181–184. doi: 10.5055/jom.2007.0002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.