Abstract
Background
The use of antithrombotic medications after ischemic stroke is recommended for deep vein thrombosis (DVT) prophylaxis and secondary stroke prevention. We assessed the rate of receipt of these therapies among eligible ischemic stroke patients aged ≥65 years and determined the effects of age and other patient characteristics on treatment.
Methods and Results
The analysis included Medicare fee-for-service beneficiaries discharged with ischemic stroke (ICD-9 433, 434, 436) randomly selected for inclusion in the Medicare Health Care Quality Improvement Program’s National Stroke Project 1998–1999, 2000–2001. Patients discharged from non-acute facilities, transferred, or terminally ill were excluded. Receipt of in-hospital pharmacological DVT prophylaxis, antiplatelet medication, anticoagulants for atrial fibrillation, and antithrombotic medications at discharge were assessed in eligible patients, stratified by age (65–74, 75–84, 85+ yrs). Descriptive models identified characteristics associated with treatment. Among 31,554 patients, 14.9% of those eligible received pharmacologic DVT prophylaxis, 83.9% antiplatelet drugs, 82.8% anticoagulants for atrial fibrillation, and 74.2% were discharged on an antithrombotic medication. Rates of treatment decreased with age, and were lowest for patients aged 85 years or older. Admission from a skilled nursing facility and functional dependence were associated with lower treatment rates.
Conclusions
There was substantial underuse of antithrombotic therapies among elderly ischemic stroke patients, particularly among the very elderly, those admitted from skilled nursing facilities, and patients with functional dependence. The reasons for low use of antithrombotic therapies, including the apparent underuse of DVT prophylaxis in otherwise eligible patients, require further investigation.
Keywords: stroke, prevention, medical care, deep vein thrombosis, elderly
Introduction
Stroke is an important public health problem in the elderly, with 75% of all strokes occurring in persons age 65 years and older.1 Stroke is the third most common cause of death and a leading cause of disability among Americans in this age group.2,3 The absolute number of elderly individuals with stroke will increase in the coming decades because of the stable or increasing incidence of stroke4–7 coupled with a growing elderly population.8,9 Patients who survive an acute ischemic stroke are at increased risk for recurrence, with the highest rates occurring within the first few weeks and reaching 10% after the first year.10,11
Treatment guidelines recommend the use of aspirin for patients with acute ischemic stroke, pharmacological and non-pharmacological prophylaxis for deep vein thrombosis (DVT), anticoagulation for atrial fibrillation, and a variety of antithrombotic drugs for secondary prevention.12 Despite their effectiveness,11,13–19 there is widespread underutilization of antithrombotic drugs among elderly stroke patients,20–27 suggesting that older patients may be receiving suboptimal care. There are relatively little age specific data regarding the utilization of antithrombotics among the very elderly, particularly for stroke patients 85 years of age or older in the United States. This represents an important gap because the proportion of the population over 85 years of age will increase fivefold by 2050.8 Given the increasing longevity of the U.S. population and the greater survivorship of stroke patients, it is important to determine whether proven secondary preventive therapies are appropriately utilized among the very elderly. Older age is associated with an increased risk of poststroke in-hospital mortality in Medicare beneficiaries, independent of sex, cognitive status, concomitant cardiac disease or stroke severity.28 The results of studies conducted in other countries assessing age-related differences in the receipt of secondary preventive interventions are inconsistent.29,30 Variation in the use of these therapies may exist within the elderly population due to factors such as the prevalence of comorbid illness, impaired functional status, and perceived feasibility of treating patients of advanced age with medications such as warfarin.22,31,32 We sought to determine whether there were age-specific differences in the receipt of pharmacologic DVT prophylaxis and antithrombotic drugs using a large, random sample of elderly patients hospitalized for acute ischemic stroke in the United States. A secondary aim was to determine whether there were patient characteristics that were associated with a greater likelihood of treatment within age groups.
Methods
Study participants were part of the Medicare Health Care Quality Improvement Program’s National Stroke Project.23,33 In brief, the National Stroke Project was authorized by the Health Care Financing Administration (now the Centers for Medicare & Medicaid Services) to improve the quality of care for patients with stroke or transient ischemic attack (TIA). A systematic random sample of up to 750 hospitalized, fee-for-service Medicare beneficiaries with a primary discharge diagnosis of stroke was identified from each of the 50 states, the District of Columbia, and Puerto Rico during two periods of data collection (1998–1999 and 2000–2001). These patients were drawn from 3,876 hospitals. Patients were included in the present study if they had a primary diagnosis of ischemic stroke (ICD-9-CM codes 433.x1, 434.x1, and 436) and had confirmatory physician documentation of a new event. Patients were excluded if they were younger than 65 years of age (n=4211), missing data on age or sex (n=15), transferred to or from another acute care facility (n=3868), discharged within one day (n=605), had left the hospital against medical advice (n=131), or had terminal cancer or an illness with a life expectancy of less than 6 months (n=1519); these exclusions are not mutually exclusive. Patients discharged alive within 1 day were excluded because they likely had conditions that were miscoded or misdiagnosed as ischemic stroke (e.g., syncope, migraine, or hypoglycemia). Transfers were excluded because care at the other acute care facility was not captured in the medical record.
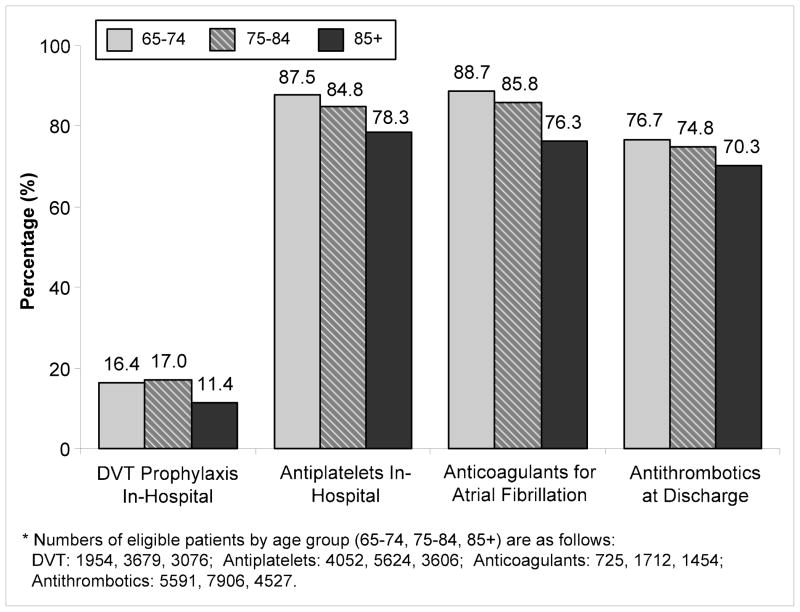
Data were obtained from medical record review by two clinical data abstraction centers using computerized abstraction tools. Patient sex, age, race-ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other), skilled nursing facility residence prior to admission, comorbid conditions, medical history, and discharge disposition (home, skilled nursing facility, or other) were recorded. The patients’ pre-stroke and discharge functional statuses were assessed using categories that reflect the modified Rankin scale (Figure 1), and were categorized as either independent, needing assistance, or dependant. We also assessed the change in scores from admission to discharge among patients discharged alive (patients who died in-hospital were not assigned a modified Rankin score).
Figure 1.
The Comparison between the Modified Rankin Scale and the National Stroke Project Mobility Variables
Outcome measures included the rates of pharmacological DVT prophylaxis by the end of day 2 among non-ambulatory patients not receiving mechanical DVT prophylaxis, antiplatelet medication during the hospitalization, anticoagulants (either warfarin, intravenous, subcutaneous, or low-molecular weight heparin) during the hospitalization among those with atrial fibrillation, and the prescription of or plan for an antithrombotic drug at discharge among patients eligible for these therapies. Table 1 gives the inclusion and exclusion criteria for each of the quality indicators. These conservative criteria were used to determine the frequency of treatment in a group of patients who generally should be given antithrombotic therapy.
Table 1.
Stroke Treatment and Eligibility Criteria*
| Treatment Definition | Number Treated | Eligibility Exclusion Criteria† | Number Eligible | Percent Treated | |
|---|---|---|---|---|---|
| DVT Prophylaxis |
|
1,295 |
|
8,709 | 14.9% |
| Antiplatelet Drugs |
|
11,137 |
|
13,282 | 83.9% |
| Anticoagulants for Atrial Fibrillation |
|
3,221 |
|
3,891 | 82.8% |
| Antithrombotics at Discharge |
|
13,380 |
|
18,024 | 74.2% |
Additional clinical contraindications for acute anticoagulation may not be reflected in these analyses; Information on size of stroke was not available.
Subcategories of eligibility exclusion criteria are not mutually exclusive
DVT: deep vein thrombosis; NSAIDs: nonsteroidal antiinflammatory drugs; ASA: aspirin
Treatment rates were stratified by patient age (65–74, 75–84, and ≥85 years), as well as by admission from a skilled nursing facility and functional status at discharge. Hierarchical regression models were used to both identify patient characteristics associated with the receipt of therapies among eligible candidates and to account for patient clustering within hospitals. Model covariates included age, sex, race-ethnicity, comorbid conditions (diabetes, hypertension, prior stroke/TIA, history of atrial fibrillation, congestive heart failure, and myocardial infarction), admission from a skilled nursing facility, functional status at discharge, and change in functional score from admission to discharge. Discharge to a skilled nursing facility was included only in the model for antithrombotic treatment at discharge.
Based on bivariate results, we tested for an age interaction with admission location and modified Rankin score at discharge in each of the models. We used standard rounding procedures to the hundredth place for the odds ratios and 95% confidence intervals presented. Due to missing modified Rankin scores (ranging from 1.6% to 21.1% across treatment categories), we created a variable for the missing data that was included in secondary analyses. Analyses were conducted using SAS version 9.1.3 (SAS Institute Inc., Cary, North Carolina). Hierarchical models were estimated using the GLIMMIX procedure in SAS. The authors had full access to the data and take responsibility for its integrity. All authors have read and agreed to the manuscript as written.
Results
Characteristics of the 31,554 patients who met initial study criteria are presented in Table 2. Patients aged 75 years and older were more likely to have had a prior stroke, a history of atrial fibrillation, congestive heart failure, and angina but were less likely to have hypertension or diabetes than patients aged 65–74. Older patients were more likely to have been admitted from a skilled nursing facility, more likely to be functionally dependent at admission and discharge, and less likely to be discharged home as compared with younger patients (p<0.001 for each comparison).
Table 2.
Demographic and Clinical Characteristics
| Total | Age (yrs) |
P-value | ||||
|---|---|---|---|---|---|---|
| 65–74 (N=9054) |
75–84 (N=13929) |
85+ (N=8571) |
||||
| N | % | % | % | % | ||
| Gender | <0. 001 | |||||
| Male | 12,462 | 39.5 | 49.7 | 39.9 | 28.2 | |
| Female | 19,092 | 60.5 | 50.3 | 60.1 | 71.8 | |
| Age, mean ± SD | 79.4 ± 7.7 | 70.1 ± 2.8 | 79.6 ± 2.8 | 89.0 ± 3.5 | ||
| Race | ||||||
| Non-Hispanic White | 24,816 | 78.7 | 73.7 | 80.3 | 81.1 | <0. 001 |
| Non-Hispanic Black | 2,993 | 9.5 | 13.5 | 8.3 | 7.2 | |
| Hispanic | 633 | 2.0 | 2.9 | 1.8 | 1.4 | |
| Other | 3,112 | 9.9 | 9.9 | 9.6 | 10.3 | |
| Comorbidity and Medical History | ||||||
| Prior Stroke | 17,090 | 54.2 | 53.0 | 55.3 | 53.6 | 0.002 |
| Prior TIA | 885 | 2.8 | 2.8 | 3.0 | 2.5 | 0.071 |
| Atrial Fibrillation | 6,667 | 21.1 | 13.3 | 21.6 | 28.7 | <0. 001 |
| Congestive Heart Failure | 6,151 | 19.5 | 13.1 | 18.8 | 27.4 | <0. 001 |
| Hypertension | 25,128 | 79.6 | 81.5 | 80.3 | 76.5 | <0. 001 |
| Diabetes Mellitus | 9,742 | 30.9 | 40.3 | 30.8 | 21.0 | <0. 001 |
| IHD/Angina | 16,445 | 52.1 | 49.7 | 53.4 | 52.6 | <0. 001 |
| Prior Myocardial Infarction | 10,229 | 32.6 | 31.7 | 33.1 | 32.9 | 0.083 |
| Admitted from Skilled Nursing Facility | 3,118 | 10.1 | 4.2 | 8.8 | 18.4 | <0. 001 |
| Functional Status at Admission | <0. 001 | |||||
| Independent | 18,900 | 60.3 | 72.3 | 61.3 | 45.8 | |
| Needs Assistance | 9,955 | 31.7 | 22.5 | 31.3 | 42.3 | |
| Dependent | 2,505 | 8.0 | 5.2 | 7.4 | 12.0 | |
| Functional Status at Discharge | <0. 001 | |||||
| Independent | 5,518 | 19.0 | 30.0 | 18.0 | 8.2 | |
| Needs Assistance | 12,182 | 41.9 | 40.2 | 43.3 | 41.3 | |
| Dependent | 11,402 | 39.2 | 29.8 | 38.7 | 50.5 | |
| Discharge Disposition | <0. 001 | |||||
| Home | 11,143 | 35.3 | 49.1 | 34.8 | 21.6 | |
| Skilled Nursing Facility | 9,667 | 30.6 | 17.4 | 29.9 | 45.8 | |
| Rehabilitation Hospitals | 6,216 | 19.7 | 23.2 | 21.2 | 13.6 | |
| Other | 2,443 | 7.7 | 5.9 | 7.7 | 9.7 | |
TIA = transient ischemic attack; IHD = ischemic heart disease
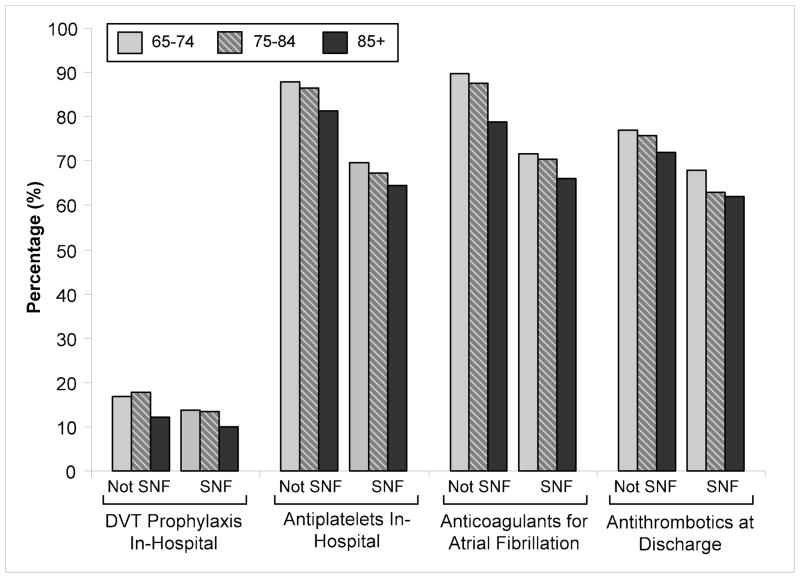
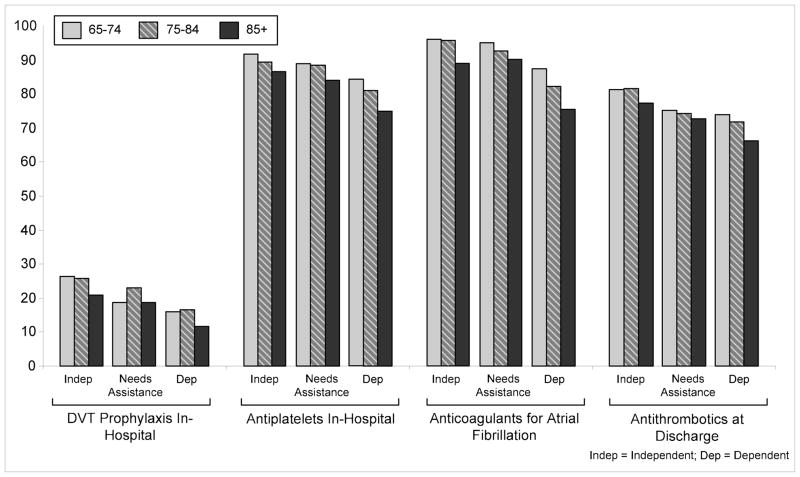
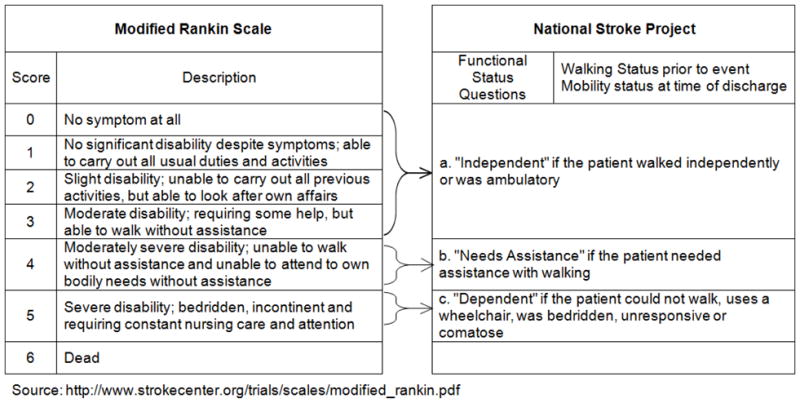
The proportion of eligible patients who received antithrombotic therapies decreased with advancing age except in the case of pharmacological DVT prophylaxis, which was slightly higher among patients aged 75–84 years as compared with those 65–74 years old (Figure 2). Overall rates of pharmacological DVT prophylaxis were particularly low, ranging from 11.4%–17.0% of eligible patients across age groups. In secondary analyses, we included patients who received non-pharmacologic DVT prophylaxis, but results were essentially unchanged. Treatment rates ranged from 78.3%–87.5% across age groups for antiplatelet drugs, 76.3%–88.7% for anticoagulants among those with atrial fibrillation, and 70.3%–76.7% for antithrombotic drugs at discharge. Treatment rates were lower for patients who were admitted from a skilled nursing facility (Figure 3) and those who were functionally dependent (Figure 4) within each age group.
Figure 2.
Receipt of Therapies by Age Group
Figure 3.
Receipt of Therapies by Admission Source (SNF vs. Not SNF) Stratified by Age
Figure 4.
Receipt of Therapies by Discharge Modified Rankin Score (Independent, Needs Assistance or Dependent) Stratified by Age
In risk-adjusted analyses (Table 3), the receipt of DVT prophylaxis as well as the use of antiplatelet drugs during the hospitalization did not differ between patients aged 65–74 years and 75–84 years, although the receipt of DVT prophylaxis was lower for those over age 85 years. Receipt of in hospital anticoagulants for atrial fibrillation decreased with advancing age and was lowest for patients 85 years or older. The likelihood of receiving antithrombotic drugs at discharge did not differ between patients aged 65–74 and 75–84 years; however, those 85 years of age or older were less likely to receive these drugs.
Table 3.
Risk-Adjusted Analysis of Quality Indicators*
| Characteristics | DVT Prophylaxis in Hospital | Antiplatelet Drugs in Hospital | Anticoagulants for AF in Hospital | Antithrombotics at Discharge | ||||
|---|---|---|---|---|---|---|---|---|
| N=6864 | N=28942 | N=3372 | N=17742 | |||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Demographics | ||||||||
| Age 75–84 (vs. 65–74) | 0.95 | (0.81–1.11) | 1.01 | (0.95–1.08) | 0.72 | (0.53–0.97) | 0.96 | (0.88–1.04) |
| Age 85+ (vs. 65–74) | 0.58 | (0.48–0.70) | 0.98 | (0.91–1.06) | 0.48 | (0.35–0.65) | 0.84 | (0.76–0.93) |
| Male (vs. Female) | 1.12 | (0.98–1.28) | 1.02 | (0.97–1.08) | 1.13 | (0.91–1.39) | 1.08 | (1.01–1.16) |
| Black Race (vs. White) | 0.75 | (0.61–0.93) | 1.06 | (0.96–1.17) | 0.95 | (0.61–1.46) | 0.88 | (0.78–0.99) |
| Other/Hispanic Race (vs. White) | 0.81 | (0.65–1.01) | 0.97 | (0.89–1.06) | 0.52 | (0.38–0.71) | 1.10 | (0.98–1.23) |
| Medical History | ||||||||
| Diabetes | 1.19 | (1.04–1.36) | 1.09 | (1.02–1.15) | 1.12 | (0.89–1.41) | 0.89 | (0.83–0.96) |
| Hypertension | 0.97 | (0.83–1.14) | 1.31 | (1.23–1.40) | 1.26 | (1.01–1.57) | 1.18 | (1.09–1.29) |
| Prior Stroke | 1.37 | (1.20–1.57) | 1.02 | (0.97–1.08) | 1.01 | (0.83–1.23) | 1.13 | (1.05–1.21) |
| Atrial Fibrillation | 4.23 | (3.69–4.85) | 0.36 | (0.34–0.39) | 1.82 | (1.48–2.23) | 1.80 | (1.63–1.99) |
| Prior MI | 1.10 | (0.97–1.26) | 1.09 | (1.02–1.15) | 1.08 | (0.88–1.32) | 1.14 | (1.05–1.23) |
| CHF | 1.34 | (1.16–1.55) | 0.80 | (0.75–0.86) | 0.88 | (0.72–1.09) | 0.91 | (0.83–1.00) |
| Admitted from SNF (vs. not SNF) | 0.83 | (0.70–0.99) | 0.58 | (0.53–0.63) | 0.38 | (0.30–0.50) | 0.80 | (0.71–0.91) |
| Functional Score at Discharge | ||||||||
| Needs Assistance (vs. Independent) | 0.72 | (0.55–0.93) | 0.93 | (0.86–1.00) | 0.75 | (0.52–1.07) | 0.75 | (0.68–0.82) |
| Dependent (vs. Independent) | 0.43 | (0.34–0.55) | 0.66 | (0.61–0.72) | 0.19 | (0.14–0.27) | 0.68 | (0.61–0.76) |
| Discharged to SNF (vs. not SNF) | - | - | - | - | - | - | 0.68 | (0.62–0.74) |
Adjusted for all the variables listed in the table, as well as change in functional status. SNF = Skilled Nursing Facility
Patients who were admitted from a skilled nursing facility were less likely to receive DVT prophylaxis (p=0.0003 for ineraction between age and SNF admission) antiplatelet drugs in the hospital, anticoagulants for atrial fibrillation (p <0.0001 for interaction between age and SNF admission), and antithrombotics at discharge. Increasing levels of functional dependence were associated with progressively lower rates of utilization of each of these therapies (needs assistance and dependent vs. functional independence), with a significant interaction between age and functional status at discharge for the receipt of DVT (p<0.0001) and anticoagulants for atrial fibrillation (p<0.0001). In secondary analysis, the inclusion of patients with missing Rankin scores did not appreciably alter the results. Elderly black patients were less likely to receive DVT prophylaxis in hospital and antithrombotics at discharge than white patients, but there were no differences for antiplatelet drugs or anticoagulants during the hospitalization. Hispanic patients and those belonging to other race-ethnic groups were less likely to receive inhospital anticoagulants as compared to non-Hispanic Whites. The relationship of these covariates with receipt of antithrombotic drugs remained unchanged when age was treated as a continuous variable in the analysis.
Discussion
Although national guidelines recommending the use of antithrombotic drugs for DVT prophylaxis and secondary stroke prevention have been in place for many years,16,34,35 we found an overall underutilization of these therapies in eligible elderly patients hospitalized with ischemic stroke, particularly among the oldest patients. Among eligible ischemic stroke patients 85+ years of age, only 11% received pharmacological DVT prophylaxis, 78% received antiplatelet medications, 76% received anticoagulants for atrial fibrillation, and 70% received antithrombotics at discharge. Because we assessed treatment rates among eligible patients, these relatively low utilization rates cannot be attributed to differences in contraindications by age. Decreased mobility and admission from a skilled nursing facility were also associated with lower receipt of each therapy. Race-ethnicity was associated with the rates of DVT prophylaxis, anticoagulant use for atrial fibrillation, and antithrombotic use at discharge, but these associations were inconsistent across race-ethnic groups and treatments. The overall low use of DVT prophylaxis and the reasons for these differences in otherwise eligible patients requires further investigation.
Prior analyses using the National Stroke Project data show that antithrombotics prescribed at discharge for patients with acute stroke or transient ischemic attack and warfarin for patients with atrial fibrillation are underutilized in patients age 65 years or older.23,33 Our analyses extend this prior work, stratifying the receipt of treatment by age groups for the subset of patients with a new ischemic stroke. We found that the underutilization of therapies is even more pronounced for the very elderly, and differs by other patient characteristics including admission location and level of functional dependence. The receipt rate of therapy for atrial fibrillation in our study was higher than that reported by Jencks et al. This is likely due to their consideration of all Medicare patients with a principal discharge diagnosis of atrial fibrillation whether or not they had an ischemic stroke. In contrast, we determined the receipt of therapy among ischemic stroke patients with documented evidence of atrial fibrillation during the hospitalization. Our lower rate of antithrombotic use at discharge as compared with Jencks et al likely reflects differences in inclusion and exclusion criteria.
DVT prophylaxis in immobilized stroke patients can reduce the risk of death due to pulmonary embolism by 56% to 82%.36 Although we found the level of utilization to be consistent with the reported rate of 13.8% among eligible Medicare patients in Michigan,37 they were lower than those reported from the California Acute Stroke Pilot Registry (CASPR, 64% in 2003 and 43% in 2004) and Get-With-The-Guidelines (GWTG)-Stroke (74% in 2003) databases.38–40 Rates may be higher in GWTG-Stroke and CASPR hospitals as they have a particular interest in stroke and both are designed as quality improvement programs. Variation in rates between studies may also reflect differences in the age distributions of included patients, differing criteria for appropriate prophylaxis, as well as the accuracy of assessment and documentation for the level of patient activity by day 2 of the hospitalization. There may also be increased DVT prophylactic use over time, as evidenced by the increase from 13.8–17.9% found in Medicare beneficiaries from 1998–2002,41 and a 15.8% increase in GWTG-Stroke hospitals from 2003 through 2007.38
More than three-quarters of patients who were eligible to receive antiplatelet drugs during the hospitalization received them, with the proportion declining in successively older age groups. These observations are consistent with another study that found unadjusted utilization rates of 73.7% among stroke patients age 65–75 years of age, and 71.9% among those >75 years old; however, risk adjusted analyses combined the older groups and compared them with patients younger than 65 years of age.42 Hierarchical models revealed no difference in the receipt of antiplatelet drugs across age groups during the acute hospitalization.
Direct comparisons with prior research reporting utilization rates of warfarin for in-hospital atrial fibrillation with our study are limited because these other studies either included patients <65 years of age43,44 or those without a diagnosis of acute ischemic stroke.21,23,32,33 A recent study of ischemic stroke patients treated at designated stroke centers in Ontario reported similar rates of treatment as our study, with a non-significant decrease in the receipt of warfarin at discharge (87.2% for <59 years, 81.5% for 60–69 years, 82.7% for 70–79 years, and 76.8% for 80+ years of age).29 Older patients with atrial fibrillation are known to benefit from anticoagulant treatment;45–48 however, we found lower receipt rates in the older age groups. This suggests that patient age may influence physicians’ decisions to prescribe warfarin independent of other demographic and clinical factors, a finding consistent with other reports in older populations.21,43 One explanation for this age difference may be physicians’ desire to avoid hemorrhagic stroke, the risk for which increases with age.22 Although the risk of major anticoagulant-associated bleeding is higher in the very elderly,48 the risks do not offset the benefits for most high risk patients with atrial fibrillation if anticoagulants are carefully administered.45–48
We found that one-fourth of eligible patients did not receive antithrombotic medications at discharge, a rate that is somewhat higher than the 16%-17% reported in two studies of Medicare patients in Michigan during the same time period.24,41 It is possible that our observed rate differs because of local variations in stroke care that are not evident within a single geographic location. Furthermore, the Michigan studies included cases with transient arterial occlusion (ICD-9 code 362.34), restricted stroke cases to white or black race, and excluded cases in which there was physician documentation that at least one antithrombotic therapy was considered but not prescribed.
Volpato et al found no difference in the prescription of antithrombotic therapy at discharge among elderly stroke patients in Italian clinical centers, but did find lower utilization rates with decreased functional independence.27 A Canadian study reported similar rates of antithrombotics at discharge across all elderly age groups (<59, 60–69, 70–79, and 80+), but only included patients admitted to designated stroke centers in Ontario which may represent a higher level of care than in non-stroke center facilities.29 Our findings differ from data reported from CASPR, which found no age difference (80+ vs. <80) in optimal utilization of antithrombotic therapy.49 Optimal therapy was defined as receipt at discharge of at least one medication from the class (i.e., an antiplatelet drug or an anticoagulant) or a valid contraindication to treatment. There was wide variation in the rates of actual and optimal treatment across the 11 CASPR hospitals. The differences in reported results between this study and ours may reflect greater variation in our sample, which was drawn from hospitals across the United States, and/or may represent selection bias (and as noted above CASPR hospitals were selected based on their interest in stroke care and experience in using registries). Higher compliance rates would also be expected among committed hospitals that were aware they were being monitored for these therapies, including those participating in quality improvement programs such as the GWTG-Stroke program.40
Our study has several limitations. First, we may have underestimated the proportion of patients prescribed antithrombotics prior to admission or at discharge due to lack of documentation, particularly for non-prescription medications such as aspirin. We used a conservative approach, excluding patients with a range of potential contraindications for the use of antiplatelet drugs, yet still found a large proportion of untreated patients. Additional clinical contraindications for acute anticoagulation may not have been documented and information on stroke size, which might affect the use of these drugs, was not available. Determining patient immobility from chart review had moderate reliability, and may have influenced the observed rates. The data reflect treatment patterns at the time of the study. Although care may have improved over time, practice recommendations for the use of antithrombotic therapies have not appreciably changed.16,34,35 We did not have information on reasons that physicians may not have prescribed these medications; however, a review of published articles assessing practice patterns and barriers to warfarin use in the setting of atrial fibrillation indicates that advanced patient age is consistently identified as a factor influencing decision making.22 Finally, our findings may not be generalizable to patients who are transferred to or from other facilities as they were excluded from the analysis.
Our findings suggest that antithrombotic medication use is not optimal, and that treatment rates may be affected by patient age as well as other patient characteristics, including admission from a skilled nursing facility and functional status. These differences were present regardless of patient demographics and comorbidities. Further research is needed to replicate these results in other data resources and understand the reasons for these differences. The underutilization of antithrombotic drugs among elderly stroke patients, particularly the very elderly, suggests that there may be an opportunity to improve their post-stroke DVT prophylaxis and secondary preventive care. Future work will need to determine the effectiveness of performance improvement activities such as primary stroke center certification,50 the Get-With-The-Guidelines-Stroke program,40 and other similar efforts in the elderly population.
Acknowledgments
We appreciate the contributions of our dear friend, mentor, and colleague, the late Dr. Lawrence M. Brass, for his support and enthusiasm of this research.
Funding sources: The analyses upon which this publication is based were performed under Contract Number 500-99-IA03, funded by the Centers for Medicare & Medicaid Services, an agency of the U.S. Department of Health and Human Services. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. The authors assume full responsibility for the accuracy and completeness of the ideas presented. This project was supported by grant number 5 R03 HS013940 from the Agency for Healthcare Research and Quality and grant number 5 R03 AG022075 from the National Institute of Aging. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of CDC.
Footnotes
Conflict of Interest Disclosures: None
References
- 1.Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2:43–53. doi: 10.1016/s1474-4422(03)00266-7. [DOI] [PubMed] [Google Scholar]
- 2.Bonita R. Epidemiology of stroke. Lancet. 1992;339:342–4. doi: 10.1016/0140-6736(92)91658-u. [DOI] [PubMed] [Google Scholar]
- 3.Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, Hailpern SM, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O’Donnell C, Roger V, Sorlie P, Steinberger J, Thom T, Wilson M, Hong Y. Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 4.Broderick JP, Phillips SJ, Whisnant JP, O’Fallon WM, Bergstralh EJ. Incidence rates of stroke in the eighties: the end of the decline in stroke? Stroke. 1989;20:577–82. doi: 10.1161/01.str.20.5.577. [DOI] [PubMed] [Google Scholar]
- 5.Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Stroke incidence, prevalence, and survival: secular trends in Rochester, Minnesota, through 1989. Stroke. 1996;27:373–80. [PubMed] [Google Scholar]
- 6.Fang J, Alderman MH. Trend of stroke hospitalization, United States, 1988–1997. Stroke. 2001;32:2221–6. doi: 10.1161/hs1001.096193. [DOI] [PubMed] [Google Scholar]
- 7.Gillum RF, Sempos CT. The end of the long-term decline in stroke mortality in the United States? Stroke. 1997;28:1527–9. doi: 10.1161/01.str.28.8.1527. [DOI] [PubMed] [Google Scholar]
- 8.Day JC. U.S. Bureau of the Census, Current Population Reports, U.S. Government Printing Office; Washington, DC: 1996. Population Projections of the United States by Age, Sex, Race, and Hispanic Origin: 1995 to 2050; pp. 25–1130. [Google Scholar]
- 9.Khaw KT. How many, how old, how soon? BMJ. 1999;319:1350–2. doi: 10.1136/bmj.319.7221.1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gubitz G, Sandercock P. Prevention of ischaemic stroke. BMJ. 2000;321:1455–9. doi: 10.1136/bmj.321.7274.1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–67. doi: 10.7326/0003-4819-146-12-200706190-00007. [DOI] [PubMed] [Google Scholar]
- 12.Adams HP, Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C, Lyden PD, Morgenstern LB, Qureshi AI, Rosenwasser RH, Scott PA, Wijdicks EF. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115:e478–534. doi: 10.1161/CIRCULATIONAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- 13.Adams RJ, Albers G, Alberts MJ, Benavente O, Furie K, Goldstein LB, Gorelick P, Halperin J, Harbaugh R, Johnston SC, Katzan I, Kelly-Hayes M, Kenton EJ, Marks M, Sacco RL, Schwamm LH American Heart A, American Stroke A. Update to the AHA/ASA Recommendations for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack. Stroke. 2008;39:1647–52. doi: 10.1161/STROKEAHA.107.189063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Albers GW, Amarenco P, Easton JD, Sacco RL, Teal P. Antithrombotic and thrombolytic therapy for ischemic stroke. Chest. 2001;119:300S–320S. doi: 10.1378/chest.119.1_suppl.300s. [DOI] [PubMed] [Google Scholar]
- 15.Albers GW, Amarenco P, Easton JD, Sacco RL, Teal P. Antithrombotic and thrombolytic therapy for ischemic stroke: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:483S–512S. doi: 10.1378/chest.126.3_suppl.483S. [DOI] [PubMed] [Google Scholar]
- 16.Albers GW, Easton JD, Sacco RL, Teal P. Antithrombotic and thrombolytic therapy for ischemic stroke. Chest. 1998;114:683S–698S. doi: 10.1378/chest.114.5_supplement.683s. [DOI] [PubMed] [Google Scholar]
- 17.Albers GW, Hart RG, Lutsep HL, Newell DW, Sacco RL. AHA Scientific Statement. Supplement to the guidelines for the management of transient ischemic attacks: A statement from the Ad Hoc Committee on Guidelines for the Management of Transient Ischemic Attacks, Stroke Council, American Heart Association. Stroke. 1999;30:2502–11. doi: 10.1161/01.str.30.11.2502. [DOI] [PubMed] [Google Scholar]
- 18.Sacco RL, Adams R, Albers G, Alberts MJ, Benavente O, Furie K, Goldstein LB, Gorelick P, Halperin J, Harbaugh R, Johnston SC, Katzan I, Kelly-Hayes M, Kenton EJ, Marks M, Schwamm LH, Tomsick T. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37:577–617. doi: 10.1161/01.STR.0000199147.30016.74. [DOI] [PubMed] [Google Scholar]
- 19.Wolf PA, Clagett GP, Easton JD, Goldstein LB, Gorelick PB, Kelly-Hayes M, Sacco RL, Whisnant JP. Preventing ischemic stroke in patients with prior stroke and transient ischemic attack: A statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke. 1999;30:1991–4. doi: 10.1161/01.str.30.9.1991. [DOI] [PubMed] [Google Scholar]
- 20.Albers GW, Yim JM, Belew KM, Bittar N, Hattemer CR, Phillips BG, Kemp S, Hall EA, Morton DJ, Vlasses PH. Status of antithrombotic therapy for patients with atrial fibrillation in university hospitals. Arch Intern Med. 1996;156:2311–6. [PubMed] [Google Scholar]
- 21.Brass LM, Krumholz HM, Scinto JM, Radford M. Warfarin use among patients with atrial fibrillation. Stroke. 1997;28:2382–9. doi: 10.1161/01.str.28.12.2382. [DOI] [PubMed] [Google Scholar]
- 22.Bungard TJ, Ghali WA, Teo KK, McAlister FA, Tsuyuki RT. Why do patients with atrial fibrillation not receive warfarin? Arch Intern Med. 2000;160:41–6. doi: 10.1001/archinte.160.1.41. [DOI] [PubMed] [Google Scholar]
- 23.Jencks SF, Huff ED, Cuerdon T. Change in the quality of care delivered to Medicare beneficiaries, 1998–1999 to 2000–2001. JAMA. 2003;289:305–12. doi: 10.1001/jama.289.3.305. [DOI] [PubMed] [Google Scholar]
- 24.Lisabeth LD, Roychoudhury C, Brown DL, Levine SR. Do gender and race impact the use of antithrombotic therapy in patients with stroke/TIA? Neurology. 2004;62:2313–5. doi: 10.1212/01.wnl.0000130500.44011.75. [DOI] [PubMed] [Google Scholar]
- 25.Munschauer FE, Priore RL, Hens M, Castilone A. Thromboembolism prophylaxis in chronic atrial fibrillation. Practice patterns in community and tertiary-care hospitals. Stroke. 1997;28:72–6. doi: 10.1161/01.str.28.1.72. [DOI] [PubMed] [Google Scholar]
- 26.Perez I, Melbourn A, Kalra L. Use of antithrombotic measures for stroke prevention in atrial fibrillation. Heart. 1999;82:570–4. doi: 10.1136/hrt.82.5.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Volpato S, Maraldi C, Ble A, Ranzini M, Rita Atti A, Dominguez LJ, Barbagallo M, Fellin R, Zuliani G. Prescription of antithrombotic therapy in older patients hospitalized for transient ischemic attack and ischemic stroke: the GIFA study. Stroke. 2004;35:913–7. doi: 10.1161/01.STR.0000121648.74433.b5. [DOI] [PubMed] [Google Scholar]
- 28.Retchin SM, Brown RS, Yeh SC, Chu D, Moreno L. Outcomes of stroke patients in Medicare fee for service and managed care. Jama. 1997;278:119–24. [PubMed] [Google Scholar]
- 29.Saposnik G, Black SE, Hakim A, Fang J, Tu JV, Kapral MK. Age disparities in stroke quality of care and delivery of health services. Stroke. 2009;40:3328–35. doi: 10.1161/STROKEAHA.109.558759. [DOI] [PubMed] [Google Scholar]
- 30.Rudd AG, Hoffman A, Down C, Pearson M, Lowe D. Access to stroke care in England, Wales and Northern Ireland: the effect of age, gender and weekend admission. Age Ageing. 2007;36:247–55. doi: 10.1093/ageing/afm007. [DOI] [PubMed] [Google Scholar]
- 31.Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, Culebras A, DeGraba TJ, Gorelick PB, Guyton JR, Hart RG, Howard G, Kelly-Hayes M, Nixon JV, Sacco RL. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2006;113:e873–923. doi: 10.1161/01.STR.0000223048.70103.F1. [DOI] [PubMed] [Google Scholar]
- 32.Bo S, Ciccone G, Scaglione L, Taliano C, Piobbici M, Merletti F, Pagano G. Warfarin for non-valvar atrial fibrillation: still underused in the 21st century? Heart. 2003;89:553–4. doi: 10.1136/heart.89.5.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jencks SF, Cuerdon T, Burwen DR, Fleming B, Houck PM, Kussmaul AE, Nilasena DS, Ordin DL, Arday DR. Quality of medical care delivered to Medicare beneficiaries: A profile at state and national levels. JAMA. 2000;284:1670–6. doi: 10.1001/jama.284.13.1670. [DOI] [PubMed] [Google Scholar]
- 34.Adams HP, Jr, Brott TG, Crowell RM, Furlan AJ, Gomez CR, Grotta J, Helgason CM, Marler JR, Woolson RF, Zivin JA, Feinberg W, Mayberg M. Guidelines for the management of patients with acute ischemic stroke. A statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 1994;25:1901–14. doi: 10.1161/01.str.25.9.1901. [DOI] [PubMed] [Google Scholar]
- 35.Laupacis A, Albers G, Dalen J, Dunn MI, Jacobson AK, Singer DE. Antithrombotic therapy in atrial fibrillation. Chest. 1998;114:579S–589S. doi: 10.1378/chest.114.5_supplement.579s. [DOI] [PubMed] [Google Scholar]
- 36.Geerts WH, Heit JA, Clagett GP, Pineo GF, Colwell CW, Anderson FA, Jr, Wheeler HB. Prevention of venous thromboembolism. Chest. 2001;119:132S–175S. doi: 10.1378/chest.119.1_suppl.132s. [DOI] [PubMed] [Google Scholar]
- 37.Roychoudhury C, Jacobs BS, Baker PL, Schultz D, Mehta RH, Levine SR. Acute ischemic stroke in hospitalized Medicare patients: evaluation and treatment. Stroke. 2004;35:e22–3. doi: 10.1161/01.STR.0000106138.71007.BF. [DOI] [PubMed] [Google Scholar]
- 38.Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, Ellrodt G, Cannon CP, Liang L, Peterson E, Labresh KA. Get With the Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119:107–15. doi: 10.1161/CIRCULATIONAHA.108.783688. [DOI] [PubMed] [Google Scholar]
- 39.California Acute Stroke Pilot Registry (CASPR) Investigators. The impact of standardized stroke orders on adherence to best practices. Neurology. 2005;65:360–5. doi: 10.1212/01.wnl.0000171706.68756.b7. [DOI] [PubMed] [Google Scholar]
- 40.LaBresh KA, Reeves MJ, Frankel MR, Albright D, Schwamm LH. Hospital treatment of patients with ischemic stroke or transient ischemic attack using the “Get With The Guidelines” program. Arch Intern Med. 2008;168:411–7. doi: 10.1001/archinternmed.2007.101. [DOI] [PubMed] [Google Scholar]
- 41.Jacobs BS, Baker PL, Roychoudhury C, Mehta RH, Levine SR. Improved quality of stroke care for hospitalized Medicare beneficiaries in Michigan. Stroke. 2005;36:1227–31. doi: 10.1161/01.STR.0000166026.14624.29. [DOI] [PubMed] [Google Scholar]
- 42.Simpson CR, Wilson C, Hannaford PC, Williams D. Evidence for age and sex differences in the secondary prevention of stroke in Scottish primary care. Stroke. 2005;36:1771–5. doi: 10.1161/01.STR.0000173398.99163.9e. [DOI] [PubMed] [Google Scholar]
- 43.Albers GW, Bittar N, Young L, Hattemer CR, Gandhi AJ, Kemp SM, Hall EA, Morton DJ, Yim J, Vlasses PH. Clinical characteristics and management of acute stroke in patients with atrial fibrillation admitted to US university hospitals. Neurology. 1997;48:1598–604. doi: 10.1212/wnl.48.6.1598. [DOI] [PubMed] [Google Scholar]
- 44.Kapral MK, Laupacis A, Phillips SJ, Silver FL, Hill MD, Fang J, Richards J, Tu JV. Stroke care delivery in institutions participating in the Registry of the Canadian Stroke Network. Stroke. 2004;35:1756–62. doi: 10.1161/01.STR.0000130423.50191.9f. [DOI] [PubMed] [Google Scholar]
- 45.EAFT (European Atrial Fibrillation Trial) Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. Lancet. 1993;342:1255–62. [PubMed] [Google Scholar]
- 46.Mant J, Hobbs FD, Fletcher K, Roalfe A, Fitzmaurice D, Lip GY, Murray E. Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): a randomised controlled trial. Lancet. 2007;370:493–503. doi: 10.1016/S0140-6736(07)61233-1. [DOI] [PubMed] [Google Scholar]
- 47.Rash A, Downes T, Portner R, Yeo WW, Morgan N, Channer KS. A randomised controlled trial of warfarin versus aspirin for stroke prevention in octogenarians with atrial fibrillation (WASPO) Age Ageing. 2007;36:151–6. doi: 10.1093/ageing/afl129. [DOI] [PubMed] [Google Scholar]
- 48.Stroke Prevention in Atrial Fibrillation Investigators. Adjusted-dose warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk patients with atrial fibrillation: Stroke Prevention in Atrial Fibrillation III randomised clinical trial. Lancet. 1996;348:633–8. [PubMed] [Google Scholar]
- 49.Ovbiagele B, Hills NK, Saver JL, Johnston SC. Secondary-prevention drug prescription in the very elderly after ischemic stroke or TIA. Neurology. 2006;66:313–8. doi: 10.1212/01.wnl.0000196476.10103.52. [DOI] [PubMed] [Google Scholar]
- 50.Douglas VC, Tong DC, Gillum LA, Zhao S, Brass LM, Dostal J, Johnston SC. Do the Brain Attack Coalition’s criteria for stroke centers improve care for ischemic stroke? Neurology. 2005;64:422–7. doi: 10.1212/01.WNL.0000150903.38639.E1. [DOI] [PubMed] [Google Scholar]