Abstract
Objective
To explore the relationship between treatment setting characteristics and diagnostic attributions of depression among community-dwelling African Americans.
Methods
Data come from the National Survey of American Life, a nationally representative sample of African Americans and Caribbean Blacks. Major Depression (MD) was assessed using the Composite International Diagnostic Inventory. Participants were categorized into four diagnostic groups: Never MD, MD never attributed to physical health problems (i.e., affective depression), MD sometimes attributed to physical health problems (i.e., complicated depression), and MD always attributed to physical health problems (i.e., physical depression). Multinomial regression was used for assessment.
Results
Among 441 participants, 66.4% were classified as affective depression, 17.8% as complicated depression, and 15.8% as physical depression. Seeking treatment from a mental health professional was associated with increased likelihood of being in the complicated depression group (Adjusted odds ratio (AOR): 5.52; 95% Confidence Interval (CI): 2.28 – 13.36). Seeking treatment from a family doctor was associated with physical depression (AOR: 2.93; 95% CI: 1.18 – 7.26). Seeking care from three or more different healthcare providers was associated with complicated depression (AOR: 1.99; 95% CI: 1.17 – 3.40).
Conclusion
Results suggest that encounters with healthcare providers influence the diagnostic attribution of depression in a systematic manner.
Keywords: Depression, treatment-seeking, minority health, mental health, primary care
OBJECTIVES
According to the Global Burden of Disease projections, major depression (MD) will be the second leading cause of disability adjusted life years world-wide, and the leading cause among developing regions by 2020 [1]. In the United States, approximately 16% of adults will experience MD at some point in their lifetime [2]. Despite the high prevalence and functional burden associated with depression, the majority of persons with MD do not receive treatment. The Centers for Disease Control and Prevention estimates that only 15.6%, 24.3% and 39.0% of people with mild, moderate, and severe MD, respectively, ever contact a mental health professional [3]. Persons with MD who do seek treatment generally do so from general healthcare providers [4]. The National Mental Health Association estimates that over 40% those with clinically diagnosed MD were first diagnosed by their primary care provider [5]. This has implications for quality of care, as several reports suggest that MD treatment in typical primary care settings is sub-optimal [6–7]. Within this treatment context, MD often co-occurs with physical symptoms or illness [8–9] and can complicate the diagnosis of physical health conditions [10–11]. Conversely, many the symptoms of MD are non-specific and common to other physiological illnesses (e.g., fatigue, appetite disturbances, sleeping difficulties, concentration problems) [12], making MD difficult to diagnosis and treat in the context of other physical health problems.
Depression, treatment, and race
Relative to non-Hispanic whites, MD among African Americans is more likely to be severe and disabling – and more likely to be untreated [13]. In this context it is necessary to understand how African Americans with depressive symptoms seek care, and how MD is diagnosed by healthcare practitioners. African Americans have substantially greater risk of developing type 2 diabetes, heart disease, some forms of cancer, and many other chronic health conditions relative to non-Hispanic whites [14]. Given the propensity for depression to co-occur with chronic physical illness [15], the disproportionate confluence of depressive symptoms and physical health problems among African Americans may be an important source of diagnostic confusion regarding MD in this group [16–17]. There is suggestive evidence that African Americans report experiencing more somatic depressive symptoms (e.g., fatigue, appetite changes, sleeping problems) than their white counterparts [18], which increases the likelihood of attributing the syndrome to a medical cause. It is within this context that the present study examined the treatment setting factors that influence diagnostic attributions of MD. Specifically, we sought to explore if particular healthcare provider settings are related to diagnostic attribution of depression syndrome among African Americans.
METHODS
Sample
Data come from the National Survey of American Life (NSAL), which is one of three surveys within the National Institute of Mental health Collaborative Psychiatric Epidemiology Surveys (CPES). The goal of the CPES initiative was to describe the occurrence of mental illness and related impaired functioning and treatment in a culturally-relevant manner. The CPES was the first dataset of its kind to assess this topic in selected racial/ethnic groups that had a large enough sample for statistically relevant results [19].
The NSAL is a nationally-representative survey of African Americans and Caribbean Blacks, as well as non-Hispanic whites who live in predominantly African American Census tracts. Details of the sampling design and interviewing strategy have been discussed elsewhere [20]. The total NSAL sample included 3,570 African Americans, 1,621 blacks of Caribbean descent, and 891 non-Hispanic whites. Analysis for the present study was limited to African American participants who had complete data on MD (N = 3,432). Those participants excluded due to missing data on MD were younger but otherwise did not differ from those included in the analysis (data not shown).
Measures
Major depression
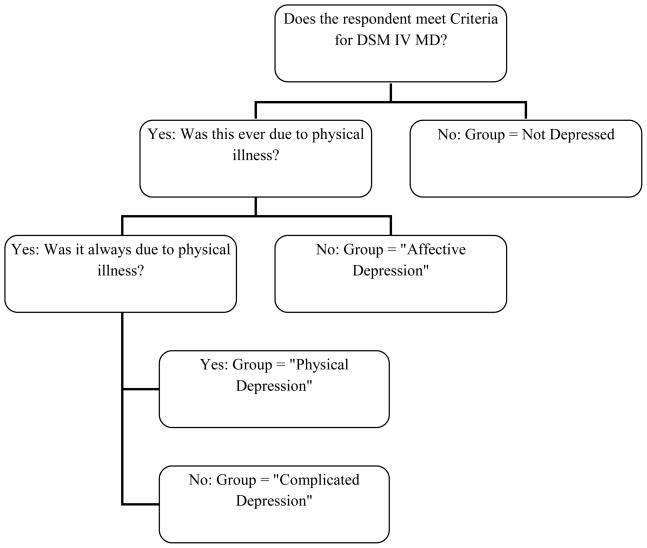
MD was assessed using a modified version of the World Mental Health Composite International Diagnostic Inventory (CIDI) [21]. The reliability and validity of the CIDI have been extensively evaluated, including in the NSAL sample specifically [13]. The CIDI has moderate concordance with clinical psychiatric interviews (κ = 0.43, sensitivity: 44%, specificity: 96%), consistent with other fully-structured diagnostic interviews of depression [22]. The diagnostic attribution of MD (e.g., always due to physical illness or injury, sometimes due to physical illness/injury, and never due to physical illness/injury) was assigned using items from the CIDI questionnaire as illustrated by Figure 1. Using these items, participants were categorized by investigators into one of four mutually-exclusive diagnostic attribution groups: No depression: Never met criteria for MD; Affective depression: met criteria for MD and depressive symptoms were never due to physical illness or injury; Complicated depression: met criteria for MD and depressive symptoms were sometimes, but not always, due to physical illness or injury; and Physical depression: met criteria for MD and depressive symptoms were always due to physical illness or injury.
Figure 1. Flowchart of the diagnostic attributions of major depression.
This flowchart illustrates how the four categories of depressive symptomology (not depression, affective, complicated, and physical depression) were determined from the CIDI questionnaire.
Treatment settings
The main predictors concerned treatment setting characteristics, including having a usual place for care and type of care sought for MD. Usual place of care was assessed by asking participants if they had one place or person that they seek for medical advice. For those who did, usual place of care was categorized as either a clinic, doctor’s office, health center, or hospital.
Healthcare setting for treatment of depressive symptoms was ascertained by asking participants who met CIDI criteria for MD, “Did you (ever) talk to a medical doctor or other professional about your (sadness/or/discouragement/or/lack of interest) (in the past 12 months)?” depending on the recency of the depressive episode. For those who had received treatment for MD at least once, the specific type of provider was identified from a list of four types: mental health professional, family doctor, other type of medical professional (e.g., a specialist other than a mental health professional, such as a cardiologist, rheumatologist, etc.), and religious/spiritual counselor or healer. These options were not mutually-exclusive, and thus we created an additional variable indicating whether participants had seen multiple types of providers for MD, categorized as one or two versus three or more types of providers.
Other covariates
Demographic variables included age, gender, marital status (categorized as married/living with someone, divorced/separated/widowed, and never married), and two indicators of socioeconomic status: income (categorized as <$20,000, $20,000 to <$40,000 and $40,000 or greater) and education (categorized as 0 – 11 years, 12 years, and >12 years). Health insurance status was assessed asking participants what type of insurance, if any, the respondent had, and if that insurance covered mental health expenses. This was then categorized into a three-level variable indicating no insurance, medical insurance with no mental health coverage, and medical insurance with mental health coverage. Health status was assessed by summing the number of common medical conditions reported, including arthritis, ulcer, cancer, high blood pressure, diabetes, liver problems, kidney problems, stroke, asthma, chronic liver disease, blood circulation problems, sickle cell disease, heart problems, glaucoma, fertility problems, osteoporosis, fibroid tumors, and anemia. This count was then collapsed into three categories representing zero, one or two, and three or more health conditions for analysis.
Analysis
Rao-Scott chi-square statistics were used to determine initial associations between the outcome and predictor variables in order to select variables for the multiple regression models. Because the dependent variable, diagnostic attribution of MD, had more than two levels and is purely categorical, multinomial logistic regression using the generalized logit model was performed to estimate the adjusted relative odds (AOR) between the dependent and predictor variables [23]. The reference group for the dependent variable was affective depression for all models, and thus the odds ratio for each predictor is interpreted as the likelihood of being categorized as physical or complicated depression as compared to being classified as affective depression. A series of nested models were fit to determine the association between treatment setting characteristics and diagnostic attribution of depression adjusting for potential confounders. These models were adjusted for demographic and socioeconomic characteristics, insurance status, and health status. Survey weighting procedures were used to adjust estimates for the complex sampling design. All analyses were performed using SAS 9.2 Software.
The NSAL was approved by the Institutional Review Board at the University of Michigan and all participants provided informed consent.
RESULTS
As shown by Table 1, the majority of the sample (87.2%) did not meet DSM-IV criteria for MD. Of those who did meet criteria (N=441), 66.4% were classified as affective depression, 17.8% were categorized as complicated depression, and the remaining 15.8% were categorized as physical depression. Overall, 253 (57.3%) of those who met criteria for MD, regardless of diagnostic attribution, had seen a healthcare professional at least once for this condition. Those in the affective depression group were younger (χ2 = 12.30, p=0.06) and more likely to be women (χ2 = 9.65, p<0.01) relative to the other MD diagnostic attribution groups. Those in the complicated depression group had fewer years of education (χ2 = 8.06, p=0.09), were more likely to have a hospital as their usual place of care (χ2 = 13.71, p<0.03), and had a higher burden of health conditions (χ2 = 23.34, p<0.01) as compared to the other depression groups. Those in the physical depression group were more likely to have seen a healthcare professional for their depressive symptoms (χ2 = 8.11, p<0.02). Marital status, income, insurance status, and having a usual place of care did not significantly differ across categorizes of diagnostic attribution of MD.
Table 1.
Demographic characteristics according to depression status: African American subsample of the NSAL
| Not Depressed | Affective Depression | Complicated Depression | Physical Depression | χ2, p-value* | |
|---|---|---|---|---|---|
| N (weighted%) | N (weighted%) | N (weighted%) | N (weighted%) | ||
| Total | 2991 | 294 | 80 | 67 | |
| Female | 1887 (54.4) | 231 (73.6) | 53 (54.1) | 45 (56.3) | 9.65, <0.01 |
| Marital status | |||||
| Married/cohabitating | 1062 (43.0) | 87 (34.9) | 17 (25.7) | 16 (35.2) | 5.82, 0.21 |
| Divorced/Separated/Widowed | 955 (25.8) | 90 (27.3) | 37 (43.9) | 29 (32.5) | |
| Never married | 974 (31.2) | 117 (37.8) | 26 (30.4) | 22 (32.3) | |
| Income | |||||
| < $20,000 | 1252 (35.5) | 125 (35.4) | 49 (47.0) | 37 (43.0) | 4.50, 0.34 |
| $20,000 to $39,999 | 869 (29.4) | 82 (27.5) | 21 (29.7) | 17 (26.4) | |
| $40,000 and above | 870 (35.1) | 87 (37.0) | 10 (23.3) | 13 (30.5) | |
| Education | |||||
| 0 to 11 years | 759 (23.9) | 78 (23.0) | 30 (37.8) | 18 (22.4) | 8.06, 0.09 |
| 12 years | 1145 (38.3) | 100 (32.9) | 29 (31.1) | 24 (36.1) | |
| 13 or more years | 1087 (37.8) | 116 (44.1) | 21 (31.1) | 25 (41.5) | |
| Age group | |||||
| 18 to 29 years | 681 (24.5) | 87 (32.0) | 15 (23.6) | 9 (11.2) | 12.30, 0.06 |
| 30 to 39 years | 706 (22.4) | 69 (21.9) | 18 (18.5) | 19 (36.1) | |
| 40 to 49 years | 641 (22.5) | 68 (23.3) | 24 (29.5) | 21 (29.7) | |
| 50+ years | 963 (30.5) | 70 (22.8) | 23 (28.5) | 18 (23.0) | |
| Health insurance status | |||||
| No insurance | 583 (19.3) | 61 (20.8) | 24 (25.0) | 10 (14.5) | 1.78, 0.78 |
| Does not include mental health coverage | 651 (22.2) | 51 (15.1) | 13 (15.0) | 11 (16.4) | |
| Includes mental health coverage | 1756 (58.5) | 182 (64.1) | 43 (59.9) | 46 (69.2) | |
| Has a usual place for care | 2593 (86.0) | 252 (86.5) | 64 (81.1) | 62 (92.4) | 3.36, 0.19 |
| Type of usual care facility | |||||
| Clinic | 370 (14.9) | 37 (14.0) | 20 (29.9) | 11 (20.4) | 13.71, 0.03 |
| Doctors office | 1623 (61.6) | 154 (64.4) | 27 (40.8) | 41 (63.3) | |
| Health center | 194 (8.0) | 27 (11.0) | 6 (7.5) | 4 (4.9) | |
| Hospital | 360 (15.5) | 30 (10.5) | 11 (21.7) | 6 (11.4) | |
| Number of health conditions | |||||
| None | 1060 (36.7) | 71 (26.6) | 18 (23.2) | 7 (14.8) | 23.34, <0.01 |
| 1 or 2 | 1275 (42.9) | 141 (46.1) | 21 (19.3) | 30 (42.0) | |
| 3 or more | 656 (20.4) | 82 (27.3) | 41 (57.5) | 30 (43.3) | |
| Saw a healthcare professional for depressive symptoms | |||||
| Yes | 153 (56.9) | 55 (68.5) | 45 (78.4) | 8.11, 0.02 | |
| No | 127 (43.1) | 20 (31.5) | 15 (21.6) | ||
| Type of professional seen for depressive symptoms** | |||||
| Mental health professional | 116 (76.4) | 50 (95.1) | 34 (75.2) | 11.43, <0.01 | |
| Family doctor | 86 (52.1) | 28 (58.8) | 31 (73.0) | 6.85, 0.03 | |
| Other type of medical professional | 53 (33.2) | 26 (54.7) | 24 (55.9) | 13.22, <0.01 | |
| Religious/spiritual healer | 87 (55.4) | 27 (60.7) | 22 (43.1) | 3.21, 0.20 | |
| Saw 1 or 2 types of professionals | 60 (57.1) | 19 (35.1) | 11 (37.2) | 11.4, <0.01 | |
| Saw 3+ types of professionals | 55 (42.9) | 23 (64.9) | 21 (62.8) | ||
P-value refers to comparison of affective, complicated and physical depression diagnostic attribution categories.
Categories are not mutually exclusive
Association between treatment setting and diagnostic attribution of MD
As shown by Table 2, compared to those who saw any other type of provider, those who saw a mental health professional were significantly more likely to be classified as complicated depression. This relationship remained even after adjusting for demographic and health characteristics (AOR: 5.52; 95% CI: 2.28 – 13.36). As shown by Table 3, receiving care from a family doctor was significantly associated with likelihood of being categorized as physical depression (AOR: 2.93; 95% CI: 1.18 – 7.26), but was not significantly associated with complicated depression. Seeing a medical professional other than a mental health provider or family doctor was also associated with diagnostic attribution of depression. Participants who saw other types of healthcare providers were more likely to report complicated depression (AOR: 2.44; 95% CI: 1.26 – 4.72) or physical depression (AOR: 2.52; 95% CI: 1.14 – 5.60) as opposed to affective depression (data not shown). There was no significant association between seeing religious/spiritual healer and diagnostic attribution of MD (AOR: 1.15; 95% CI: 0.57 – 2.36 for complicated depression and AOR: 0.54; 95% CI: 0.23 – 1.30 for physical depression) (data not shown).
Table 2.
Relationship between seeing a mental health professional and diagnostic attribution of MD
| Predictors | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Complicated vs. Affective Depression | Physical vs. Affective Depression | Complicated vs. Affective Depression | Physical vs. Affective Depression | Complicated vs. Affective Depression | Physical vs. Affective Depression | |
| Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | |
| Saw mental health professional (ref. No) | 6.07 (2.73, 13.48) | 0.94 (0.40, 2.22) | 6.13 (2.48, 15.19) | 0.81 (0.28, 2.29) | 5.52 (2.28, 13.36) | 0.80 (0.28, 2.27) |
| Age (ref. 18–29 years) | ||||||
| 30 to 39 years | 0.85 (0.23, 3.10) | 7.62 (1.84, 31.66) | 0.77 (0.20, 2.92) | 7.63 (1.78, 32.75) | ||
| 40 to 49 years | 1.37 (0.47, 3.97) | 6.49 (1.35, 31.23) | 1.17 (0.39, 3.54) | 6.09 (1.20, 30.98) | ||
| 50+ years | 1.58 (0.47, 5.36) | 4.48 (0.78, 25.57) | 0.97 (0.25, 3.69) | 3.88 (0.70, 21.50) | ||
| Sex (ref. Male) | 0.41 (0.22, 0.79) | 0.23 (0.10, 0.49) | 0.32 (0.15, 0.66) | 0.18 (0.08, 0.40) | ||
| Insurance (ref. Has mental health coverage) | ||||||
| Insurance but no mental health coverage | 0.57 (0.21, 1.53) | 1.51 (0.67, 3.37) | 0.52 (0.18, 1.49) | 1.54 (0.67, 3.58) | ||
| No health insurance | 1.53 (0.58, 4.01) | 0.51 (0.13, 1. 88) | 1.60 (0.59, 4.33) | 0.61 (0.16, 2.36) | ||
| Number of health conditions (ref. None) | ||||||
| 1 or 2 conditions | 0.79 (0.28, 2.23) | 1.89 (0.42, 8.53) | ||||
| 3+ conditions | 2.59 (0.83, 8.04) | 2.31 (0.47, 11.26) | ||||
| Total N | 253 | 253 | 253 | |||
Sample is restricted to those who met DSM-IV criteria for MD and had seen at least once healthcare provider for these depressive symptoms.
Table 3.
Relationship between seeing a family doctor and diagnostic attribution of MD
| Predictors | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Complicated vs. Affective Depression | Physical vs. Affective Depression | Complicated vs. Affective Depression | Physical vs. Affective Depression | Complicated vs. Affective Depression | Physical vs. Affective Depression | |
| Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | |
| Saw family doctor (ref. No) | 1.31 (0.64, 2.69) | 2.48 (1.26, 4.88) | 1.62 (0.77, 3.43) | 2.97 (1.26, 7.03) | 1.67 (0.78, 3.60) | 2.93 (1.18, 7.26) |
| Age (ref. 18 to 29) | ||||||
| 30 to 39 years | 0.71 (0.22, 2.36) | 5.16 (1.26, 21.23) | 0.61 (0.17, 2.17) | 5.26 (1.25, 22.09) | ||
| 40 to 49 years | 1.25 (0.43, 3.60) | 4.86 (1.01, 23.40) | 1.04 (0.36, 3.06) | 4.79 (0.94, 24.44) | ||
| 50+ years | 1.11 (0.32, 3.81) | 3.11 (0.56, 17.42) | 0.68 (0.20, 2.37) | 2.77 (0.51, 15.01) | ||
| Sex (ref. Male) | 0.33 (0.17, 0.64) | 0.18 (0.07, 0.42) | 0.26 (0.12, 0.57) | 0.15 (0.06, 0.37) | ||
| Insurance (ref. Has mental health coverage) | ||||||
| Insurance but no mental health coverage | 0.57 (0.21, 1.57) | 1.90 (0.80, 4.53) | 0.56 (0.20, 1.57) | 1.89 (0.75, 4.75) | ||
| No health insurance | 1.48 (0.58, 3.74) | 0.58 (0.16, 2.07) | 1.56 (0.64, 3.82) | 0.65 (0.18, 2.41) | ||
| Number of health conditions (ref. None) | ||||||
| 1 or 2 conditions | 0.60 (0.21, 1.74) | 1.58 (0.38, 6.58) | ||||
| 3+ conditions | 2.24 (0.79, 6.38) | 1.96 (0.40, 9.65) | ||||
| Total N | 253 | 253 | 253 | |||
Sample is restricted to those who met DSM-IV criteria for MD and had seen at least once healthcare provider for these depressive symptoms.
Approximately 40% of those who met criteria for MD and sought care for this syndrome did so from three or more different types of healthcare providers (i.e., family doctor, mental health professional, and religious healer). As shown by Table 4, those who sought care from three or more types of providers were significantly more likely to be categorized as complicated depression relative to those who only saw one or two professionals (AOR: 1.99; 95% CI: 1.17 – 3.40). Seeing multiple professionals was not significantly associated with likelihood of being categorized as physical depression in the fully-adjusted model.
Table 4.
Relationship between seeing multiple professionals and diagnostic attribution of MD
| Predictors | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Complicated vs. Affective Depression | Physical vs. Affective Depression | Complicated vs. Affective Depression | Physical vs. Affective Depression | Complicated vs. Affective Depression | Physical vs. Affective Depression | |
| Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | Odds Ratio (95%CI) | |
| Saw 3+ professionals (ref. Saw 1 or 2) | 2.43 (1.29, 4.59) | 1.80 (0.97, 3.36) | 2.76 (1.53, 4.95) | 1.75 (0.88, 3.47) | 2.43 (1.33, 4.44) | 1.59 (0.75, 3.37) |
| Age (ref. 18 to 29 years) | ||||||
| 30 to 39 years | 0.74 (0.22, 2.51) | 7.14 (1.82, 28.05) | 0.69 (0.19, 2.42) | 7.23 (1.78, 29.43) | ||
| 40 to 49 years | 1.31 (0.47, 3.65) | 6.09 (1.37, 27.02) | 1.14 (0.40, 3.24) | 5.87 (1.27, 27.18) | ||
| 50+ years | 1.05 (0.35, 3.09) | 3.98 (0.75, 21.16) | 0.73 (0.22, 2.38) | 3.58 (0.68, 18.97) | ||
| Sex (ref. Male) | 0.32 (0.17, 0.61) | 0.22 (0.10, 0.48) | 0.28 (0.14, 0.56) | 0.19 (0.08, 0.41) | ||
| Insurance (ref. Has mental health coverage) | ||||||
| Insurance but no mental health coverage | 0.56 (0.21, 1.49) | 1.64 (0.75, 3.56) | 0.57 (0.21, 1.55) | 1.63 (0.72, 3.72) | ||
| No health insurance | 1.55 (0.58, 4.16) | 0.52 (0.14, 1.91) | 1.57 (0.59, 4.16) | 0.61 (0.16, 2.40) | ||
| Number of health conditions (ref. None) | ||||||
| 1 or 2 conditions | 0.59 (0.21, 1.66) | 1.71 (0.37, 7.98) | ||||
| 3+ conditions | 1.88 (0.69, 5.21) | 2.04 (0.40, 10.46) | ||||
| Total N | 253 | 253 | 253 | |||
Sample is restricted to those who met DSM-IV criteria for MD and had seen at least once healthcare provider for these depressive symptoms.
A consistent finding across the models presented in Tables 2 and 3 was that women were less likely to be categorized as complicated or physical depression relative to men (i.e., women were more likely to be classified in the affective depression group, even after adjustment for demographic, socioeconomic, and health-related factors). Also, those aged 30 to 39 and 40 to 49 years old were more likely to be categorized as physical depression, but not complicated depression, relative to the youngest age group (aged 18 to 29) in all models. Insurance status was only significantly predictive of MD diagnostic attribution in the analysis examining seeking care from multiple types of providers (Table 4). In this analysis, those who had insurance that did not include mental health coverage were significantly more likely to be categorized as physical depression (AOR: 3.72; 95% CI: 1.39 – 10.03) relative to those with insurance that included mental health coverage.
Exploring the influence of self-selection
Although the results discussed above are consistent with the hypothesis that different types of healthcare providers vary as to whether they attribute the cause of depressive symptoms to affective or physical sources, it is also possible that individuals experiencing depressive symptoms select particular health providers based on their own particular notions of the source of these symptoms (i.e., persons self-identify that their depressive symptoms are due to a physical cause and therefore seek care from their family physician). In order to explore this self-selection hypothesis, we re-ran the analyses with depression diagnostic category as the main predictor and type of healthcare provider as the outcome. These models were adjusted for the same set of demographic, socioeconomic, and health characteristics as the analyses described above. Those in the complicated depression group were more likely to have sought care from a mental health professional as compared to those with affective depression (AOR: 5.88; 95% CI: 2.52 – 13.76). Those in the physical depression group were more likely to have sought care from a family physician relative to those with affective depression (AOR: 3.13; 95% CI: 1.22 – 8.03). Both those in the complicated (AOR: 2.73; 95% CI: 1.27 – 5.86) and physical depression (AOR: 2.39; 95% CI: 1.26 – 4.54) groups were more likely to have sought care from other types of healthcare providers. Finally, those in the complicated depression group were more likely to have sought care from three or more different types of providers (AOR: 1.96; 95% CI: 1.21 – 3.18) as compared to those in the affective depression group.
DISCUSSION
The major finding of this study is that treatment setting characteristics are related to the diagnostic attribution of MD among community-living African American adults. Persons who received care from a family doctor were more likely to attribute their depressive symptoms to a physical illness or injury rather than psychopathology. Those who sought care from three or more types of professionals were more likely to be categorized as complicated rather than affective depression, consistent with the notion that seeing multiple professionals would produce differing clinical opinions about the nature and source of the depressive symptoms. These findings complement work by Ueblacker and colleagues (2006) which reported that persons who received care for any psychiatric condition in general medical settings, or in multiple settings, were more likely to have comorbid medical problems than those who received care in specialty psychiatric settings only [24]. In sum, the clinical characteristics of MD, particularly concerning the role of physical health problems as a confounding factor, varies in the population and by treatment setting. These findings are consistent with they hypothesis that the diagnostic attribution of depression syndrome (that is, whether it is identified as a purely psychological state, a consequence of a physical health problem, or a bit of both) is substantially related to the type of health professional seen for care, as all the participants examined in this analysis met diagnostic criteria for MD.
Previous studies have demonstrated heterogeneity among African Americans with regards to treatment-seeking for mental health problems [25–27,4]. The findings of the present study emphasize the heterogeneity of MD presentation within the African American population; of the 441 cases that met DSM-IV criteria for MD, approximately one-third were categorized as either complicated or physical depression. These findings are important because the differential diagnosis of depressive symptomology may result in differing treatment strategies or treatment priorities. Such tailoring is likely beneficial when based on characteristics of the clinical presentation, but if provider characteristics are driving these differences such tailoring may be unwarranted [28]. For example, if a provider determines that a patient’s depressive symptoms are simply a consequence of a physical illness or injury rather than an independent clinical condition, the patient’s depression may not be effectively treated with psychotherapy or medication even if these treatments would be warranted [29].
Part of the association between treatment settings and diagnostic attribution of MD may be due to patient self-selection into particular treatment settings (e.g., persons who feel their depressive symptoms are due to a physical health problem such as comorbid diabetes may preferentially seek out their family doctor for care). However, the association between treatment settings and diagnostic attribution of MD persisted even after accounting for physical health comorbidities, suggesting that influences other than self-selection play a role in this observed relationship. This self-selection hypothesis also presupposes that individuals can accurately identify the source of their symptoms, despite these symptoms being non-specific and common to many health conditions.
In addition to patient-level factors, the association between treatment settings and depression diagnosis may also be explained by provider-level factors, including provider comfort or perceived competence in treating psychiatric conditions. Family doctors and other general providers may not feel competent in either identifying or treating depression [30], and this may influence how they interpret depression syndrome when individuals do present in their clinics [31]. However, recent research efforts such as the Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT) have demonstrated that depression care management can be effectively integrated into primary care settings [32]. Even if MD is identified by the healthcare provider, provider-level characteristics can also influence if and how depression treatment guidelines are followed [33], as well as how patients express symptoms and interact with their physician regarding development of a treatment plan [34].
Regardless of treatment setting, women were consistently more likely to be classified as the affective depression group as opposed to either the complicated or physical depression attribution groups. There is limited evidence that healthcare providers may be more likely to label women with depressive symptoms as having psychologically-based depression whereas men’s depressive symptoms may be linked to physical health [35]. Alternatively, women and men may present to treatment with different symptomology of depression [36]. Future research should explore both provider and patient-level characteristics that contribute to this consistent gender difference.
A substantial portion of those who met criteria for MD and sought care for these symptoms reported seeing three or more different types of providers. Seeking care from multiple providers may be an indicator of dissatisfaction with treatment progress or plan at the initial provider. Alternatively, this could simply reflect the current limits of access to specialty care which require referrals from primary care providers [37]. Insurance status was only related to depression diagnostic attribution in this analysis of multiple providers, in that those with health insurance without mental health coverage were more likely to be categorized in the physical rather than affective depression group. This finding was independent of demographic, socioeconomic, and health factors, suggesting that in this sample if an individual only had coverage to see a medical professional and not a mental health professional, their depressive symptoms were more likely to be identified as related to physical illness.
Strengths and Limitations
The primary strengths of this study are the use of a nationally-representative sample of African Americans (one of the few datasets of its kind) and use of a diagnostic measure of MD. The study also explored multiple aspects of treatment seeking, including type of healthcare professional seen for depressive symptoms specifically. However, these results should be interpreted in light of study limitations. This analysis is cross-sectional, and as such cannot exclude the influence of patient self-selection into particular providers as a determinant of the associations reported here. Data were collected using an interview questionnaire and therefore all the variables, including reports of treatment-seeking behaviors and health conditions, were determined by self-report which may be subject to recall or information bias. We also did not have detailed information about the types of providers respondent’s sought for care (e.g., years in practice, advanced degrees, practice size) or mental health treatment preferences of the respondents (e.g., medication, psychotherapy) that may have that influenced self-selection or contributed to the associations between treatment setting and diagnostic attributions.
Significance
These findings suggest the need for increased awareness of the multifactorial presentation of depression among African Americans. Improved diagnostic tools for primary care physicians and other types of medical professionals may help these practitioners to distinguish between symptoms of MD and symptoms related to physical illnesses, as well as increase provider confidence in depression screening and providing referrals to appropriate care [38]. Implementation of regular depression screening in all care settings could raise awareness among both providers and patients about mental health promotion and treatment. Several studies have demonstrated the effectiveness of co-localizing depression care management within primary care settings, [39–40]. Future research should examine whether such efforts influence the diagnosis of MD by healthcare providers, particularly for African Americans.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global burden of disease study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, et al. The epidemiology of major depressive disorder: Results from the national comorbidity survey replication (NCS-R) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 3.CDC/NCHIS. Data briefs - number 7. 2008 september; Retrieved 7/27/2010, from http://www.cdc.gov/nchs/data/databriefs/db07.htm.
- 4.Neighbors HW, Caldwell C, Williams DR, Nesse R, Taylor RJ, Bullard, et al. Race, ethnicity and the use of services for mental disorders. Arch Gen Psychiatry. 2007;64:485–94. doi: 10.1001/archpsyc.64.4.485. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Family Physicians. Mental health care services by family physicians (position paper) -- policy & advocacy -- american academy of family physicians. Retrieved 3/15/2010, from http://www.aafp.org/online/en/home/policy/policies/m/mentalhealthcareservices.html.
- 6.Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. Am J Public Health. 2002;92:92–8. doi: 10.2105/ajph.92.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Arch of Gen Psychiatry. 2001;58:55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- 8.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54:216–26. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 9.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: Results from the world health surveys. Lancet. 2007;370:851–8. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 10.Katon W, Ciechanowski P. Impact of major depression on chronic medical illness. J of Psychosom Res. 2002;53:859–63. doi: 10.1016/s0022-3999(02)00313-6. [DOI] [PubMed] [Google Scholar]
- 11.Lebowitz BD, Pearson JL, Schneider LS, Reynolds CF, 3rd, Alexopoulos GS, et al. Diagnosis and treatment of depression in late life. consensus statement update. JAMA. 1997;278:1186–90. [PubMed] [Google Scholar]
- 12.Nair J, Nair SS, Kashani JH, Reid JC, Mistry SI, Vargas VG. Analysis of the symptoms of depression--a neural network approach. Psychiatry Res. 1999;87:193–201. doi: 10.1016/s0165-1781(99)00054-2. [DOI] [PubMed] [Google Scholar]
- 13.Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, et al. Prevalence and distribution of major depressive disorder in african americans, caribbean blacks, and non-hispanic whites: Results from the national survey of american life. Arch of Gen Psychiatry. 2007;64:305–15. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 14.Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benton T, Staab J, Evans DL. Medical co-morbidity in depressive disorders. Ann Clin Psychiatry. 2007;19:289–303. doi: 10.1080/10401230701653542. [DOI] [PubMed] [Google Scholar]
- 16.Jackson JS. Health and mental health disparities among black Americans. In: Hager M, editor. Modern psychiatry: Challenges in educating health professionals to meet new needs. New York: Josiah Macy Jr. Foundation; 2002. pp. 246–54. [Google Scholar]
- 17.Schwartz S, Meyer IH. Mental health disparities research: The impact of within and between group analyses on tests of social stress hypotheses. Soc Sci Med. 2010;70:1111–8. doi: 10.1016/j.socscimed.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Das AK, Olfson M, McCurtis HL, Weissman MM. Depression in african americans: Breaking barriers to detection and treatment. J Fam Pract. 2006;55:30–9. [PubMed] [Google Scholar]
- 19.Jackson JS, Neighbors HW, Nesse RM, Trierweiler SJ, Torres M. Methodological innovations in the national survey of american life. Int J Methods Psychiatr Res. 2004;13:289–98. doi: 10.1002/mpr.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, et al. The national survey of american life: A study of racial, ethnic and cultural influences on mental disorders and mental health. Int J Methods Psychiatr Res. 2004;13:196–207. doi: 10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC, Ustun TB. The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eaton WW, Hall AL, Macdonald R, McKibben J. Case identification in psychiatric epidemiology: A review. Int Rev of Psychiatry. 2007;19:497–507. doi: 10.1080/09540260701564906. [DOI] [PubMed] [Google Scholar]
- 23.Allison PD. Logistic regression using the SAS system: Theory and application. Cary, NC: SAS Institute Inc; 1999. [Google Scholar]
- 24.Uebelacker LA, Wang PS, Berglund P, Kessler RC. Clinical differences among patients treated for mental health problems in general medical and specialty mental health settings in the National Comorbidity Study Replication. Gen Hosp Psychiatry. 2006;28:387–95. doi: 10.1016/j.genhosppsych.2006.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neighbors HW. Professional help use among black Americans: Implications for unmet need. Am J Community Psychol. 1984;12:551–566. doi: 10.1007/BF00897212. [DOI] [PubMed] [Google Scholar]
- 26.Neighbors HW, Jackson JS, Bowman PJ, Gurin G. Stress, coping, and black mental health: Preliminary findings from a national study. Prev Hum Serv. 1983;2:5–29. doi: 10.1300/J293v02n03_02. [DOI] [PubMed] [Google Scholar]
- 27.Neighbors HW, Howard CS. Sex differences in professional help use among adult blacks. Am J Community Psychol. 1987;15:403–17. doi: 10.1007/BF00915210. [DOI] [PubMed] [Google Scholar]
- 28.Epstein SA, Hooper LM, Weinfurt KP, DePuy V, Cooper LA, et al. Primary care physicians’ evaluation and treatment of depression: Results of an experimental study using video vignettes. MedCare Res Rev. 2008;65:674–95. doi: 10.1177/1077558708320987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van der Feltz-Cornelis CM, Nuyen J, Stoop C, Chan J, Jacobson AM, et al. Effect of interventions for major depressive disorder and significant depressive symptoms in patients with diabetes mellitus: A systematic review and meta-analysis. Gen Hosp Psychiatry. 2010;32:380–95. doi: 10.1016/j.genhosppsych.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 30.Mitchell AJ, Vaze A, Rao S. Clinical diagnosis of depression in primary care: A meta-analysis. Lancet. 2009;374:609–19. doi: 10.1016/S0140-6736(09)60879-5. [DOI] [PubMed] [Google Scholar]
- 31.Menchetti M, Belvederi Murri M, Bertakis K, Bortolotti B, Berardi D. Recognition and treatment of depression in primary care: Effect of patients’ presentation and frequency of consultation. J Psychosom Res. 2009;66:335–41. doi: 10.1016/j.jpsychores.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 32.Bruce ML, Ten Have TR, Reynolds CF, 3rd, Katz II, Schulberg HC, Mulsant BH, Bown GK, MvAvay GJ, Pearson JL, Alexopoulos GS. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 33.Smolders M, Laurant M, Verhaak P, Prins M, van Marwijk H, et al. Which physician and practice characteristics are associated with adherence to evidence-based guidelines for depressive and anxiety disorders? Med Care. 2010;48:240–8. doi: 10.1097/MLR.0b013e3181ca27f6. [DOI] [PubMed] [Google Scholar]
- 34.Wittink MN, Barg FK, Gallo JJ. Unwritten rules of talking to doctors about depression: Integrating qualitative and quantitative methods. Annals of Family Medicine. 2006;4:302–9. doi: 10.1370/afm.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bertakis KD, Helms LJ, Callahan EJ, Azari R, Leigh P, et al. Patient gender differences in the diagnosis of depression in primary care. J Womens Health Gend Based Med. 2001;10:689–98. doi: 10.1089/15246090152563579. [DOI] [PubMed] [Google Scholar]
- 36.Romans SE, Tyas J, Cohen MM, Silverstone T. Gender differences in the symptoms of major depressive disorder. J Nerv Ment Dis. 2007;195:905–11. doi: 10.1097/NMD.0b013e3181594cb7. [DOI] [PubMed] [Google Scholar]
- 37.Grembowski DE, Martin D, Patrick DL, Diehr P, Katon W, et al. Managed care, access to mental health specialists, and outcomes among primary care patients with depressive symptoms. J Gen Intern Med. 2002;17:258–69. doi: 10.1046/j.1525-1497.2002.10321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tavabie JA, Tavabie OD. Improving care in depression: Qualitative study investigating the effects of using a mental health questionnaire. Qual Prim Care. 2009;17:251–61. [PubMed] [Google Scholar]
- 39.Gallo JJ, Zubritsky C, Maxwell J, Nazar M, Bogner HR, et al. Primary care clinicians evaluate integrated and referral models of behavioral health care for older adults: Results from a multisite effectiveness trial (PRISM-e) Ann Fam Med. 2004;2:305–9. doi: 10.1370/afm.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gallo JJ, Bogner HR, Morales KH, Ford DE. Patient ethnicity and the identification and active management of depression in late life. Arch Intern Med. 2005;165:1962–1968. doi: 10.1001/archinte.165.17.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.