Abstract
Background
It is unknown if comorbid depression in patients with diabetes mellitus increases the risk of intensive care unit (ICU) admission.
Objective
This study examined whether comorbid depression in patients with diabetes increased risk of ICU admission, coronary care unit (CCU) admission, and general medical-surgical unit hospitalization, as well as total days hospitalized, after controlling for demographics, clinical characteristics, and health risk behaviors.
Method
This prospective cohort study included 3,596 patients with diabetes enrolled in the Pathways Epidemiologic Follow-Up Study. We assessed baseline depression with the Patient Health Questionnaire-9. We controlled for baseline demographics, smoking, BMI, exercise, hemoglobin A1c, medical comorbidities, diabetes complications, type 1 diabetes, diabetes duration, and insulin treatment. We assessed time to any ICU, CCU and/or general medical-surgical unit admission using Cox proportional-hazards regression. We used Poisson regression with robust standard errors to examine associations between depression and total days hospitalized.
Results
Unadjusted analyses revealed that baseline probable major depression was associated with increased risk of ICU admission (Hazard Ratio (HR) 1.94, 95% Confidence Interval (95% CI)(1.34–2.81)), but was not associated with CCU or general medical-surgical unit admission. Fully adjusted analyses revealed probable major depression remained associated with increased risk of ICU admission (HR 2.23, 95% CI(1.45–3.45)). Probable major depression was also associated with more total days hospitalized (Incremental Relative Risk 1.64, 95% CI(1.26–2.12)).
Conclusions
Patients with diabetes and comorbid depression have a greater risk of ICU admission. Improving depression treatment in patients with diabetes could potentially prevent hospitalizations for critical illnesses and lower healthcare costs.
INTRODUCTION
Diabetes mellitus is a serious public health burden, accounting for substantial morbidity,1,2 disability,3 mortality,4 and healthcare costs. For a single patient, diabetes and its complications account for up to $3,225 of excess medical costs per hospital day.5 Moreover, poorly controlled diabetes is a known risk factor for critical medical illnesses such as acute myocardial infarction,6 heart failure,7 and sepsis,8 often requiring admission to an intensive care unit (ICU) for treatment, where medical care costs per day can average up to $3,518 per patient.9
In addition to impaired physical health, patients with diabetes frequently have comorbid affective illness. Approximately 11–15% of patients with diabetes mellitus are afflicted with coexisting major depression.10 As with other chronic medical illnesses, diabetes and comorbid mental disorders such as major depression are bidirectionally related.11 Major depression can contribute to bio-behavioral risk factors for diabetes such as obesity and sedentary lifestyle, in turn leading to the development of diabetes and its complications, which can ultimately lead to exacerbations of depressive symptoms.11 In support of this model, comorbid major depression has been found to be associated with poor glycemic control in patients with diabetes,12 increased risk of macrovascular and microvascular complications,13 as well as increased healthcare costs relative to patients with diabetes alone.14 Depression has also been shown to be an independent predictor of increased mortality in patients with type 2 diabetes.15
Since patients with diabetes are at increased risk for major depression, and depression has been shown to increase the risk of poor glycemic control and greater numbers of complications, depression could represent a potentially modifiable risk factor for costly outcomes such as ICU and non-critical hospitalizations. Hospitalization costs in patients with diabetes account for up to 50% of total medical costs each year.5 Depression screening programs coupled with quality improvement treatment programs such as collaborative care could lead to reduced healthcare costs and improved outcomes. To our knowledge, no studies have ascertained whether depression independently increases the risk of initial ICU admission. One study found that a history of depression was a risk factor for readmission to an ICU during the same hospital stay.16 Moreover, prior studies examining the role of major depression in increasing the risk of hospitalization or rehospitalization for a medical illness have had small sample sizes,17,18 have not been prospective in design,19,20 or were limited to patients over the age of 60.19–22
The Pathways Study was a prospective population-based cohort investigation examining the potential adverse impact of major depression in primary care patients with diabetes. The aim of the current investigation was to utilize the Pathways Epidemiologic Follow-Up Study to extend beyond prior investigations by examining whether comorbid depressive symptoms in patients with diabetes mellitus would increase the risk of any hospitalization for medical illness, and particularly ICU admission. We hypothesized that patients with comorbid depression and diabetes would be at greater risk of any hospitalization, including ICU, cardiac care unit (CCU), and general medical-surgical unit admissions than patients with diabetes alone, after adjusting for baseline demographic, health risk behaviors and clinical characteristics. In addition, we hypothesized that comorbid depression in patients with diabetes would be associated with a greater total number of hospital days for medical illness than patients with diabetes alone.
METHODS
The Pathways Epidemiologic Follow-Up Study was developed by a multidisciplinary team from the University of Washington and Group Health Cooperative (GHC) Research Institute. GHC is an integrated health care system with 30 primary care clinics caring for approximately 523,000 patients in western Washington State. The study protocol was reviewed and approved by institutional review boards at the University of Washington and GHC.
Setting
Nine GHC clinics were selected for this study based on the following three criteria: 1) clinics with the largest populations of patients with diabetes, 2) clinics located within a 40-mile geographic radius of Seattle, and 3) clinics with the greatest amount of ethnic and racial diversity.
Patient Population
The cohort for the Pathways Epidemiologic Follow-Up Study was initially sampled between 2000 and 2002. Patients enrolled in the Group Health Diabetes registry were recruited for the study based on previously described eligibility criteria.23,24 Permission to review medical records was obtained for 4,128 patients enrolled in the original Pathways study. Nonconsenting patients were more often younger, female, non-white, less educated, had a shorter duration of diabetes, a lower mean body mass index (BMI), a lower mean hemoglobin A1C (HbA1C), and had less medical comorbidity.25
Predictor of Interest
The predictor of interest was baseline probable major depression as ascertained by the Patient Health Questionnaire-9 (PHQ-9), 26 which was obtained from a mailed baseline survey. This questionnaire can be utilized as a continuous measure of depressive symptom severity. In addition, patients with a PHQ-9 score ≥ 10 with ≥ 5 symptoms scored as being present for half of the days or more for at least 2 weeks (with one of the symptoms being either depressed mood or anhedonia) have symptoms suggestive of the diagnosis of major depression. Patients with two to four depressive symptoms for more than half the days for at least 2 weeks (with one of the symptoms being either depressed mood or anhedonia) have symptoms suggestive of minor depression. The PHQ-9 threshold for a probable case of major depression has been found to have high sensitivity (73%) and specificity (98%) for the diagnosis of major depression based on structured psychiatric interview.26
Potential Confounders
Potential confounders were obtained from the mailed baseline survey, which included questions regarding sociodemographic characteristics (e.g., age, sex, race, educational level, and marital status), diabetes characteristics (age at onset, diabetes type, duration of diabetes, initial treatment prescribed, and type of current treatment), as well as questions regarding height and weight (used to compute BMI), smoking status, and physical activity from the Summary of Diabetes Self-Care Questionnaire.27 Baseline non-diabetic medical comorbidity was measured with the RxRisk, an automated pharmacy-based data model.28 Severity of diabetic complications was measured using the Diabetes Complications Severity Index (DCSI), an automated-data derived measure of diabetic complications based on International Classification of Disease-9th Revision diagnostic codes for diabetic complications and laboratory tests.29 Both RxRisk and DCSI predict subsequent medical costs and mortality.28, 29 HbA1c was also obtained from medical records.
Outcomes of Interest
We report on all ICU, CCU, and general medical-surgical unit hospitalizations that occurred over a 3 year period beginning in March 2003, other than admissions due to mental health conditions (with the exception of delirium or dementia). All eligible hospitalizations were for a minimum of 24 hours. Although enrollment into the Pathways Study began in March 2001, we could not differentiate the type of hospital admission (i.e., ICU, CCU, or general medical-surgical unit) due to lack of location codes for the first two years. Additionally, depression can be a prodromal symptom of failing health or secondary to downward trajectory of medical illness. For these reasons, we do not report on any hospitalizations that occurred in the first two years of the study. Information regarding hospital admission was obtained via automated data abstraction. We also obtained information regarding total inpatient healthcare costs from automated data abstraction. GHC’s cost accounting system assigns budget-based costs instead of charges (i.e., the costs of providing the services) for healthcare services provided at GHC facilities. Healthcare services provided at non-GHC facilities are assigned the cost paid by GHC. Time to any hospitalization was censored at the end of the study, death, or the time of disenrollment.
Statistical Analysis
We used one-way analysis of variance (ANOVA) to examine univariate associations between continuous baseline demographic and clinical characteristics and no depression or probable major or minor depression. We used χ2 tests to ascertain univariate associations between categorical baseline variables and no depression or probable major or minor depression. We also computed the mean total inpatient healthcare costs (with 95% Confidence Intervals (95% CIs)) for each depression group over the 3 year follow-up period.
In order to examine potential associations between probable major or minor depression and hospitalizations, we used Cox-proportional hazards regression models. First, we tested the effect of baseline probable major or minor depression on time to first hospitalization without adjustment, using the group without baseline depression as the reference group. We then added three groups of potential confounding variables to the regression model, including demographic variables (i.e., age, sex, race, marital status, and education), clinical variables including RxRisk scores (categorized into quartiles), DCSI scores, baseline HbA1c, duration of diabetes, type 1 diabetes diagnosis, and whether or not the patient was taking insulin, and self-care characteristics such as BMI, smoking status, and sedentary lifestyle, as well as enrollment status in the Pathways randomized controlled trial30 (which attempted to improve depression outcomes of patients with depression and diabetes), in order to adjust for potential intervention effects on reducing the risk of hospitalization in the regression model. We used these proportional hazards models to examine potential associations between baseline probable major or minor depression and time to first ICU, CCU, and/or general medical-surgical unit admission. We tested the proportionality assumption for each of the proportional hazards models and found that none of the models were in violation.
To examine the effects of probable major or minor depression on the total number of hospital days for medical illnesses, we first calculated the proportion of hospitalized patients among depression groups and tested these proportions using χ2 tests. We then used one-way ANOVA models with Bonferroni corrections for multiple comparisons to examine associations between baseline depression status and the total number of days hospitalized among the entire cohort as well as only among those hospitalized; because the total number of hospitalized days was non-normally distributed across the depression groups, we log-transformed hospitalized days for this analysis. Next, we used Poisson regression models with robust standard errors to adjust for potential confounders. The regression models were developed in a similar fashion to the proportional hazards models, beginning with an unadjusted model followed by the addition of demographics, then baseline clinical characteristics, and finally baseline self-care characteristics as well as enrollment status in the randomized controlled trial. As a sensitivity analysis, we also used zero-inflated negative binomial regression models to adjust for potential confounding variables.31 Since we found no differences in the results between the two methods, we will report the results of the Poisson models. Analyses were performed with appropriate components of the IBM SPSS Statistics 18 (SPSS Inc., Chicago, IL, USA) and STATA 11 (Stata Corporation, College Station, TX, USA) statistical software programs.
RESULTS
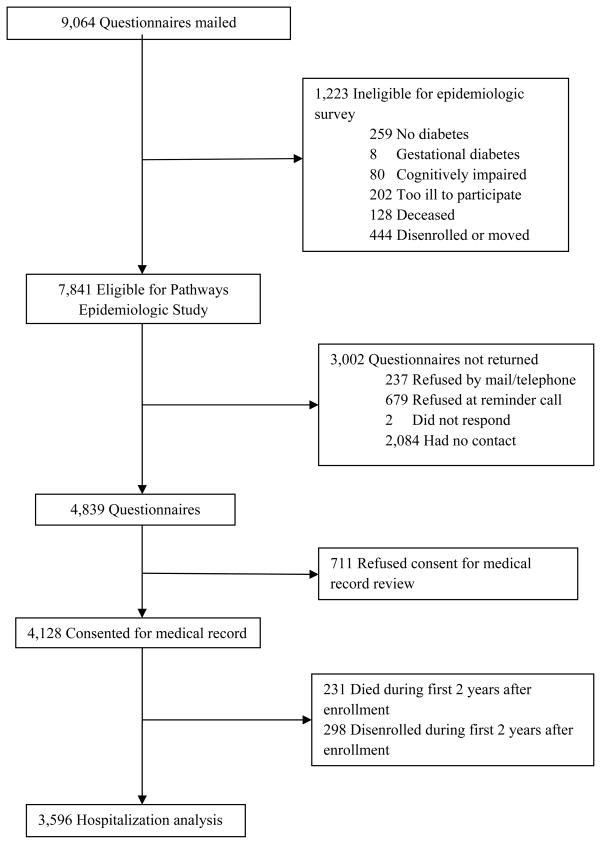
Of the 4,128 patients who consented for medical record review, 231 died and 298 disenrolled from GHC during the first 2 years of the Pathways Epidemiologic Study, 3 patients died on their first day of eligibility for analysis (Figure 1), and 5 patients did not have measures for baseline depression status, leaving 3,591 participants for the current investigation.
Figure 1.
Recruitment of epidemiologic cohort study to assess hospitalizations
Approximately 19% of patients had baseline probable major (11.2%) or minor (7.9%) depression. Compared to patients with minor depressive symptoms or no depression, patients with probable major depression at baseline were younger and more likely to be female, unmarried, smokers, and physically inactive. They also had higher mean RxRisk scores, greater severity of diabetic complications, higher mean HbA1C levels, higher mean BMI, and were more likely to be treated with insulin (Table 1). Furthermore, patients with probable major depression at baseline had higher mean total inpatient healthcare costs over the 3 year follow-up period ($12,447, 95% CI($9,416–$15,477)) compared to patients without depression ($6,700, 95% CI($6,050–$7,350)) or patients with probable minor depression ($6,845, 95% CI($4,854–$8,837)).
Table 1.
Baseline characteristics by depression grouping
| Variables | Total (n = 3,591)a | No Depression (n = 2,904) | Minor Depression (n = 284) | Major Depression (n = 403) | Test Statisticsb |
|---|---|---|---|---|---|
| Age | 63.5 (13.1) | 64.1 (13.0) | 63.9 (13.3) | 58.9 (13.4) | F = 28.38‡ |
| Female | 1,740 (48.5%) | 1,355 (46.7%) | 144 (50.7%) | 241 (59.8%) | χ2 = 25.10‡ |
| Married | 2,328 (64.8%) | 1,920 (66.1%) | 184 (64.8%) | 224 (55.6%) | χ2 = 17.22‡ |
| Non-white | 675 (18.8%) | 522 (18.0%) | 74 (26.1%) | 79 (19.6%) | χ2 = 11.26† |
| Education beyond high school | 2,741 (76.3%) | 2,252 (77.5%) | 191 (67.3%) | 298 (73.9%) | χ2 = 16.60‡ |
| RxRisk score | 3,063.1 (2,355.0) | 3,028.2 (2,313.2) | 3,227.7 (2,357.8) | 3,198.8 (2,631.7) | F = 1.68* |
| DCSI | 1.7 (1.8) | 1.6 (1.8) | 1.9 (2.0) | 2.0 (2.1) | F = 11.05‡ |
| Years since diabetes diagnosis | 9.5 (9.4) | 9.4 (9.5) | 10.6 (10.0) | 9.4 (8.2) | F = 2.04* |
| HbA1C | 7.8 (1.5) | 7.7 (1.5) | 7.9 (1.6) | 8.1 (1.6) | F = 13.03‡ |
| Currently requiring insulin | 1,051 (29.3%) | 800 (27.5%) | 89 (31.3%) | 162 (40.2%) | χ2 = 27.99‡ |
| Type 1 Diabetes | 152 (4.2%) | 132 (4.5%) | 6 (2.1%) | 14 (3.5%) | χ2 = 4.43* |
| BMI | 31.6 (7.1) | 31.0 (6.7) | 32.2 (7.2) | 35.1 (9.1) | F = 62.96‡ |
| Current smoking | 294 (8.2%) | 202 (7.0%) | 29 (10.2%) | 63 (15.6%) | χ2 = 37.13‡ |
| Exercise | |||||
| ≤1 day per week | 1,138 (31.7%) | 832 (28.7%) | 123 (43.3%) | 183 (45.4%) | χ2 = 65.15‡ |
| 2–7 days per week | 2,453 (68.3%) | 2,072 (71.3%) | 161 (56.7%) | 220 (54.6%) | |
| PHQ-9 Score | 5.6 (5.5) | 3.6 (3.3) | 9.7 (2.2) | 16.7 (3.8) | F = 3,151.24‡ |
All values are mean ± SD or n (%) unless otherwise indicated.
Abbreviations (in alphabetic order): BMI = body mass index; DCSI = Diabetes Complications Severity Index; HbA1C = glycosylated hemoglobin; PHQ-9 = Patient Health Questionnaire-9; RxRisk = Non-diabetic medical comorbidity measure.
Five subjects did not have measures for depression status.
F-statistic with 2,3588 degrees of freedom or Pearson χ2 with 2 degrees of freedom.
P < 0.05
P < 0.01
P < 0.001
During the 3 year follow-up period, a total of 1,182 patients with diabetes were hospitalized at least once, including 193 patients with at least one ICU admission, 187 patients with at least one CCU admission, 742 patients with at least one general medical-surgical unit admission, and 60 patients with both ICU and CCU admissions. Among the entire cohort and the 1,182 patients who were hospitalized, patients with baseline probable major depression had a greater number of days hospitalized for medical illnesses compared to those without depressive symptoms or those with probable minor depression (Table 2).
Table 2.
Total hospital days for medical illness over the 3 year period by depression grouping
| Variables | Total (n = 3,591)a | No Depression (n = 2,904) | Minor Depression (n = 284) | Major Depression (n = 403) | Test Statistics |
|---|---|---|---|---|---|
| n (%) with any hospitalization | 1,182 (33) | 926 (32) | 94 (33) | 162 (40) | χ2 = 11.2b† |
| Total hospital days over 3 year period (n=3,591)a | 2.8 (7.6) | 2.5 (6.7) | 2.9 (7.0) | 4.9 (12.2) | F = 17.9c‡ |
| Total hospital days over 3 year period among hospitalized (n=1,182) | 8.6 (11.2) | 7.9 (9.9) | 8.9 (9.7) | 12.2 (16.8) | F = 10.4d‡ |
All values are mean ± SD unless otherwise indicated.
Five subjects did not have measures for depression status.
Pearson χ2 with 2 degrees of freedom.
F-statistic with 2, 3588 degrees of freedom
F-statistic with 2, 1178 degrees of freedom
P < 0.05
P < 0.01
P < 0.001
Unadjusted analyses found that baseline probable major depression was associated with a 1.94-fold increased risk of ICU admission (95% CI(1.34–2.81)) and a 1.95-fold greater risk for more inpatient days over the 3 year follow-up period (95% CI(1.50–2.54)). Additionally, there were non-significant trends for an association between baseline probable major depression and both CCU admission (Hazard Ratio (HR) 1.36, 95% CI(0.89–2.08)) and general medical-surgical unit admission (HR 1.18, 95% CI(0.94–1.47)). After adjusting for demographics, baseline probable major depression in patients with diabetes was associated with a 2.41-fold greater risk of ICU admission (95% CI(1.65–3.52)), a 1.66-fold greater risk of CCU admission (95% CI(1.08–2.55)), a 1.35-fold greater risk of general medical-surgical unit admission (95% CI(1.08–1.70)), and a 2.28-fold greater likelihood of having more total hospital days (95% CI(1.76–2.96)). When baseline illness severity and other clinical measures were included in the analysis, patients with diabetes and baseline probable major depression had a 1.89-fold greater risk of ICU admission (95% CI(1.28–2.79)), and a 1.71-fold greater likelihood of spending more days hospitalized (95% CI(1.35–2.16)). However, the associations with CCU admission (HR 1.31, 95% CI(0.85–2.04)) and general medical-surgical unit admission (HR 1.21, 95% CI(0.96–1.52)) were no longer statistically significant. After adjusting for demographics, baseline clinical characteristics, health-risk behaviors, and enrollment status in the Pathways Randomized controlled trial, baseline probable major depression in patients with diabetes was the single strongest factor associated with ICU admission (Figure 2). Non-significant trends for an association between baseline probable major depression and both CCU and general medical-surgical unit admission remained in the final adjusted model (Table 3).
Figure 2.
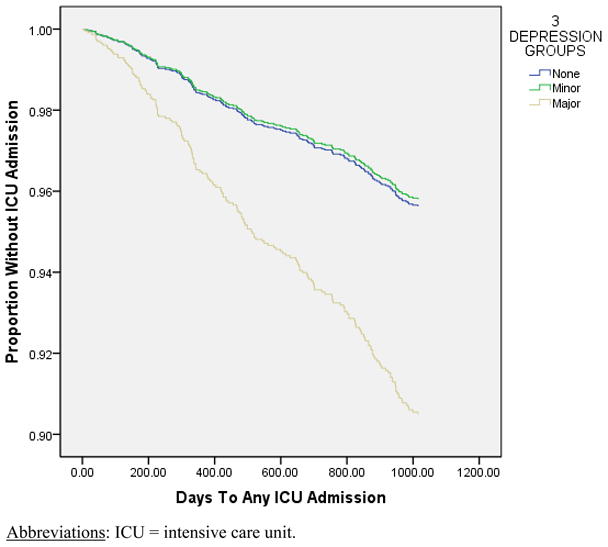
Time to first intensive care unit admission for Pathways epidemiologic cohort by depression group
Abbreviations: ICU = intensive care unit.
Table 3.
Fully adjusted associations of baseline depression and hospital admission groups
| Baseline Variables | ICU Admission, Hazard Ratio (95% CI) | CCU Admission, Hazard Ratio (95% CI) | General Medical-Surgical Unit Admission, Hazard Ratio (95% CI) | Total Hospital Days, Incremental Relative Risk (95% CI) |
|---|---|---|---|---|
| Major depression | 2.23 (1.45 – 3.45) ‡ | 1.21 (0.73 – 2.01) | 1.19 (0.91 – 1.55) | 1.64 (1.26 – 2.12) ‡ |
| Minor depression | 0.96 (0.55 – 1.67) | 0.82 (0.47 – 1.44) | 1.05 (0.80 – 1.36) | 1.01 (0.76 – 1.33) |
| Age | 1.01 (1.00 – 1.03) | 1.03 (1.02 – 1.05) ‡ | 1.02 (1.01 – 1.03) ‡ | 1.02 (1.02 – 1.03) ‡ |
| Male | 1.22 (0.89 – 1.66) | 1.22 (0.89 – 1.68) | 0.80 (0.68 – 0.93) † | 0.96 (0.81 – 1.15) |
| Non-white | 0.65 (0.41 – 1.02) | 1.32 (0.90 – 1.92) | 0.74 (0.59 – 0.92) † | 0.99 (0.77 – 1.27) |
| Single | 0.96 (0.70 – 1.32) | 1.27 (0.93 – 1.75) | 1.06 (0.91 – 1.25) | 1.08 (0.90 – 1.28) |
| < HS education | 1.09 (0.78 – 1.50) | 1.25 (0.90 – 1.72) | 1.02 (0.86 – 1.21) | 1.08 (0.91 – 1.29) |
| RxRisk score | 1.36 (1.14 – 1.62) † | 1.22 (1.01 – 1.46)* | 1.22 (1.12 – 1.33) ‡ | 1.31 (1.18 – 1.45) ‡ |
| DCSI | 1.15 (1.06 – 1.24) ‡ | 1.16 (1.07 – 1.25) ‡ | 1.11 (1.07 – 1.16) ‡ | 1.16 (1.11 – 1.21) ‡ |
| Years since diabetes diagnosis | 1.00 (0.99 – 1.02) | 1.02 (1.00 – 1.03) | 1.00 (1.00 – 1.01) | 1.00 (0.99 – 1.01) |
| HbA1c | 1.02 (0.92 – 1.13) | 1.04 (0.94 – 1.16) | 1.02 (0.97 – 1.08) | 1.07 (0.99 – 1.15) |
| Currently requiring insulin | 1.26 (0.89 – 1.79) | 1.09 (0.76 – 1.57) | 0.95 (0.79 – 1.15) | 1.01 (0.84 – 1.22) |
| Type 1 diabetes | 0.78 (0.30 – 2.07) | 1.40 (0.58 – 3.37) | 0.78 (0.46 – 1.32) | 1.16 (0.60 – 2.27) |
| BMI | 1.00 (0.98 – 1.03) | 1.02 (1.00 – 1.04) | 0.99 (0.98 – 1.00) | 1.01 (0.99 – 1.02) |
| Current smoking | 0.94 (0.50 – 1.75) | 0.95 (0.49 – 1.83) | 1.41 (1.07 – 1.85)* | 1.33 (0.97 – 1.81) |
| Sedentary lifestyle | 0.99 (0.72 – 1.36) | 1.39 (1.02 – 1.88)* | 1.11 (0.95 – 1.30) | 1.19 (1.00 – 1.42) |
| Enrolled in RCT | 0.63 (0.34 – 1.18) | 0.94 (0.49 – 1.79) | 1.02 (0.74 – 1.41) | 0.97 (0.69 – 1.35) |
P < 0.05
P < 0.01
P < 0.001
Abbreviations (in alphabetic order): CI = confidence interval; BMI = body mass index; CCU = coronary care unit; DCSI = Diabetes Complications Severity Index; HbA1c = glycosylated hemoglobin; HS = high school; ICU = intensive care unit; RCT = randomized controlled trial; RxRisk = Non-diabetic medical comorbidity measure.
Baseline probable minor depression was not associated with ICU, CCU, or general medical-surgical unit hospitalizations or total number of days hospitalized in any of the models.
DISCUSSION
In this prospective investigation of patients with diabetes, probable major depression at baseline was the single strongest factor associated with ICU hospitalization, as well as more days spent hospitalized, even after adjusting for baseline medical comorbidity and diabetic complication severity. The present study is the first to identify depression as a prospective risk factor for ICU admission. The association between depression and ICU admission in patients with diabetes found in this study builds upon the findings of prior studies15 that comorbid depression in patients with chronic medical illnesses increases the risk of dire outcomes. While the associations between depression and CCU or general medical-surgical unit admission did not reach statistical significance in the fully adjusted models, there were trends towards greater risk amongst patients with baseline probable major depression, suggesting that the present study may have lacked statistical power to detect these associations. Prior investigations in elderly populations have identified depression as a predictor of hospitalization for medical illnesses.19–22 However, to our knowledge, the present study is the first to find that depressive symptoms were associated with hospitalizations in a cohort that includes only patients with diabetes and patients of mixed ages.
Increased medical comorbidity and diabetes complication severity were also associated with hospitalizations and days hospitalized in the fully adjusted model. Evidence suggests that depression and diabetes complications may be bidirectionally related. Depression has been shown to be a risk factor for development of macro- and microvascular complications,12 and incident diabetes macrovascular complications have been shown to be a risk factor for depression.32 In our model that controlled for diabetes complications, the effect of depressive symptoms may be diminished by “over-controlling” for diabetes complication severity due to depression. Randomized controlled trials of enhanced depression treatment in patients with diabetes have demonstrated improvements in depressive symptoms,30,33 including among patients with increased burden of diabetic complications,34 and new interventions are being designed to translate improved depression treatment in patients with diabetes into improvements in medical outcomes.35
In patients with diabetes, depressive symptoms may be associated with increased risk of ICU admissions because of both behavioral and biological factors. Depression in patients with diabetes is known to be associated with poor adherence to self-care behaviors (i.e., exercise, diet, smoking cessation),11, 12, 36 decreased adherence to disease controlling medications (i.e., oral hypoglycemic, lipid-lowering, and anti-hypertensive agents),36 and an increased risk of having multiple cardiac risk factors,24 all factors also associated with increased risk for critical illnesses.37,38 Depression is also associated with increased inflammation,39 as well as abnormalities in the hypothalamic-pituitary-adrenal axis which lead to chronic glucocorticoid elevations,39 increasing the risk of severe infectious processes due to immunosuppression.40,41 Moreover, chronic glucocorticoid elevation may directly damage brain areas such as the hypothalamus,42,43 increasing the risk of dementia, a risk factor for medical hospitalization in elderly patients when comorbid with depression.21
Improved recognition and treatment of depression in patients with diabetes may produce substantial reductions in healthcare costs through reductions in hospitalizations for medical illnesses. Approximately one in every five healthcare dollars in the U.S. is spent on patients with diabetes, and inpatient medical treatment accounts for 50% of all healthcare costs attributable to diabetes.5 Furthermore, depression prior to a critical illness may be associated with an increased risk of major depression in the months post-ICU,44 potentially increasing the risk of ICU recidivism in depressed patients with diabetes. A previous study of an intervention targeted at reducing depressive symptom burden in elderly patients found that improvements in depression status were associated with reduced inpatient medical admissions and overall decreases in healthcare costs,45 and studies of enhanced depression treatment in patients with diabetes have found reductions in outpatient medical costs,46 as well as a trend towards decreased healthcare costs overall.47 Since inpatient medical treatment accounts for as high as 50% of the healthcare costs in patients with diabetes, investigations that examine the impact of effective depression treatment in patients with diabetes on ICU admissions are needed.
Several important limitations of the present study are noted. First, because a substantial number of patients eligible for the Pathways Epidemiologic Study were either lost to follow-up or did not grant permission for medical record review, there is the potential that non-response bias may affect our results. Second, although our models controlled for clinical severity of diabetes and medical comorbidity, we cannot exclude the possibility that depression in our sample was secondary to impending failing health, and was therefore a proxy for severe medical illness. Third, since baseline depressive symptoms were assessed using a questionnaire (i.e., PHQ-9), and not a structured or semistructured diagnostic interview, a diagnosis of major depression could not be made, hence the use of the phrases “probable major depression” or “symptoms suggestive of major depression” throughout. An additional limitation is that self-report of baseline factors such as physical inactivity, smoking, and BMI may not accurately reflect subsequent health behaviors over the follow-up period. Also, we only measured depression at baseline and depression status may have changed over the follow-up period. However, the Pathways randomized controlled trial found that over 70% of patients with a PHQ-9 score ≥ 10 reported that they had been depressed for more than 2 years.30 In addition, our investigation may have lacked statistical power to detect significant associations between baseline probable major or minor depression and CCU or general medical-surgical unit admissions. Moreover, this study was completed in only one geographic region of the U.S., potentially limiting generalizability. Also, because over 20% of our sample did not fill out the question on income, we did not include this variable in our analyses; however, educational level is an acceptable proxy for socioeconomic status. Finally, due to the observational nature of the present investigation, the possibility of residual confounding does exist.
In conclusion, comorbid depression in patients with diabetes is associated with increased risk of ICU admissions. Furthermore, patients with diabetes and comorbid depression are at increased risk of spending more days hospitalized. In the absence of additional studies, clinicians should include assessment and treatment of depression to other preventive measures such as treating comorbid medical conditions and reducing diabetic complications to reduce critical illness-related admissions among patients with diabetes.
Acknowledgments
This work was supported by grants NRSA-T32/MH20021-12 (Katon), K24MH069741-07 (Katon), and RO1MH073686-04 (Von Korff) from the National Institute of Mental Health.
Footnotes
Potential Conflicts of Interest: Dr. Katon has received honorariums for lectures from Wyeth, Eli Lilly, Forest, and Pfizer pharmaceutical companies and serves on the Advisory Board for Eli Lilly and Wyeth. Dr. Von Korff has received grant funding from Johnson & Johnson. Dr. Ciechanowski is CEO and founder of Same Page, Inc., a consulting company providing services for improving patient-provider relationships. Dr. Lin has received honorariums from Health Star Communications and Prescott Medical. Drs. Davydow, Russo, and Ludman, and Ms. Oliver, have no potential conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Karter AJ, Ferrara A, Liu YJ, Moffet HH, Ackerson LM, Selby JV. Ethnic disparities in diabetic complications in an insured population. JAMA. 2002;287:2519–2527. doi: 10.1001/jama.287.19.2519. [DOI] [PubMed] [Google Scholar]
- 2.Young B, Maynard C, Reiber G, Boyko EJ. Effects of ethnicity and nephropathy on lower extremity amputation risk among diabetic veterans. Diabetes Care. 2003;26:495–501. doi: 10.2337/diacare.26.2.495. [DOI] [PubMed] [Google Scholar]
- 3.Von Korff M, Katon W, Lin EH, Simon G, Ciechanowski P, Ludman E, Oliver M, Rutter C, Young B. Work disability among individuals with diabetes. Diabetes Care. 2005;28:1326–1332. doi: 10.2337/diacare.28.6.1326. [DOI] [PubMed] [Google Scholar]
- 4.Hogan P, Dall T, Nikolov P American Diabetes Association. Economic costs of diabetes in the U.S. in 2002. Diabetes Care. 2003;26:917–932. doi: 10.2337/diacare.26.3.917. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31:596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 6.Kelly TN, Bazzano LA, Fonseca VA, Thethi TK, Reynolds K, He J. Systematic review: glucose control and cardiovascular disease in type 2 diabetes. Ann Intern Med. 2009;151:394–403. doi: 10.7326/0003-4819-151-6-200909150-00137. [DOI] [PubMed] [Google Scholar]
- 7.Bell DSH. Heart failure: the frequent, forgotten, and often fatal complication of diabetes. Diabetes Care. 2003;26:2433–2441. doi: 10.2337/diacare.26.8.2433. [DOI] [PubMed] [Google Scholar]
- 8.Cheadle WG, Mercer-Jones M, Heinzelmann M, Polk HC., Jr Sepsis and septic complications in the surgical patient: who is at risk? Shock. 1996;6:S6–S9. [PubMed] [Google Scholar]
- 9.Halpern NA, Pastores SM. Critical care medicine in the United States 2000–2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38:65–71. doi: 10.1097/CCM.0b013e3181b090d0. [DOI] [PubMed] [Google Scholar]
- 10.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 11.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54:216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 12.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 13.Lin EH, Rutter CM, Katon W, Heckbert SR, Ciechanowski P, Oliver MM, Ludman EJ, Young BA, Williams LH, McCulloch DK, Von Korff M. Depression and advanced complications of diabetes: a prospective cohort study. Diabetes Care. 2010;33:264–269. doi: 10.2337/dc09-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simon GE, Katon WJ, Lin EH, Ludman E, Von Korff M, Ciechanowski P, Young BA. Diabetes complications and depression as predictors of healthcare costs. Gen Hosp Psychiatry. 2005;27:344–351. doi: 10.1016/j.genhosppsych.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, Kinder L, Young B, Von Korff M. The association of comorbid depression and mortality in patients with type 2 diabetes. Diabetes Care. 2005;28:2668–2672. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 16.Paratz J, Thomas P, Adsett J. Re-admission to intensive care: identification of risk factors. Physiother Res Int. 2005;10:154–163. doi: 10.1002/pri.5. [DOI] [PubMed] [Google Scholar]
- 17.Saravay SM, Pollack S, Steinberg MD, Weinschel B, Habert M. Four-year follow-up of the influence of psychological comorbidity on medical rehospitalization. Am J Psychiatry. 1996;153:397–403. doi: 10.1176/ajp.153.3.397. [DOI] [PubMed] [Google Scholar]
- 18.Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS, Blazing MA, Davenport C, Califf RM, Krishnan RR, O’Connor CM. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 19.Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care. 2004;42:512–521. doi: 10.1097/01.mlr.0000127998.89246.ef. [DOI] [PubMed] [Google Scholar]
- 20.Sayers SL, Hanrahan N, Kutney A, Clarke SP, Reis BF, Riegel B. Psychiatric comorbidity and greater hospitalization risk, longer length of stay, and higher hospitalization costs in older adults with heart failure. J Am Geriatr Soc. 2007;55:1585–1591. doi: 10.1111/j.1532-5415.2007.01368.x. [DOI] [PubMed] [Google Scholar]
- 21.Feng L, Yap KB, Kua EH, Ng TP. Depressive symptoms, physician visits and hospitalization among community-dwelling older adults. Int Psychogeriatr. 2009;21:568–575. doi: 10.1017/S1041610209008965. [DOI] [PubMed] [Google Scholar]
- 22.Ng TP, Feng L, Chiam PC, Kua EH. Psychiatric morbidity and acute hospitalization in elderly people. Int Psychogeriatr. 2006;18:701–711. doi: 10.1017/S1041610206003346. [DOI] [PubMed] [Google Scholar]
- 23.Katon W, Von Korff M, Lin E, Simon G, Ludman E, Bush T, Walker E, Ciechanowski P, Rutter C. Improving primary care treatment of depression among patients with diabetes: the design of the Pathways study. Gen Hosp Psychiatry. 2003;25:158–168. doi: 10.1016/s0163-8343(03)00013-6. [DOI] [PubMed] [Google Scholar]
- 24.Katon WJ, Lin EH, Russo J, Von Korff M, Ciechanowski P, Simon G, Ludman E, Bush T, Young B. Cardiac risk factors in patients with diabetes mellitus and major depression. J Gen Intern Med. 2004;19:1192–1199. doi: 10.1111/j.1525-1497.2004.30405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Katon WJ, Lin EHB, Williams LH, Ciechanowski P, Heckbert SR, Ludman E, Rutter C, Crane PK, Oliver M, Von Korff M. Comorbid depression is associated with an increased risk of dementia diagnosis in patients with diabetes: a prospective cohort study. J Gen Intern Med. 2010;25:423–429. doi: 10.1007/s11606-009-1248-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study: Primary Care Evaluation of Mental Disorders; patient health questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 27.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from seven studies and a revised scale. Diabetes Care. 2000;23:943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 28.Fishman PA, Goodman MJ, Hornbrook MC, Meenan RT, Bachman DJ, O’Keeffe Rosetti MC. Risk adjustment using automated ambulatory pharmacy data: the RxRisk model. Med Care. 2003;41:84–99. doi: 10.1097/00005650-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Young BA, Lin E, Von Korff M, Simon G, Ciechanowski P, Ludman EJ, Everson-Stewart S, Kinder L, Oliver M, Boyko EJ, Katon WJ. Diabetes Complications Severity Index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care. 2008;14:15–24. [PMC free article] [PubMed] [Google Scholar]
- 30.Katon WJ, Von Korff M, Lin EH, Simon G, Ludman E, Russo J, Ciechanowski P, Walker E, Bush T. The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry. 2004;61:1042–1049. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]
- 31.Simons JS, Neal DJ, Gaher RM. Risk for marijuana-related problems among college students: an application of zero-inflated negative binomial regression. Am J Drug Alcohol Abuse. 2006;32:41–53. doi: 10.1080/00952990500328539. [DOI] [PubMed] [Google Scholar]
- 32.Katon W, Russo J, Lin EHB, Heckbert SR, Ciechanowski P, Ludman EJ, Von Korff M. Depression and diabetes: factors associated with major depression at five-year follow-up. Psychosomatics. 2009;50:570–579. doi: 10.1176/appi.psy.50.6.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Williams JW, Jr, Katon W, Lin EH, Nöel PH, Worchel J, Cornell J, Harpole L, Fultz BA, Hunkeler E, Mika VS, Unützer J IMPACT Investigators. The effectiveness of depression care management on diabetes-related outcomes in older patients. Ann Int Med. 2004;140:1015–1024. doi: 10.7326/0003-4819-140-12-200406150-00012. [DOI] [PubMed] [Google Scholar]
- 34.Kinder LS, Katon WJ, Ludman E, Russo J, Simon G, Lin EH, Ciechanowski P, Von Korff M, Young B. Improving depression care in patients with diabetes and multiple complications. J Gen Intern Med. 2006;21:1036–1041. doi: 10.1111/j.1525-1497.2006.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Katon W, Lin EH, Von Korff M, Ciechanowski P, Ludman E, Young B, Rutter C, Oliver M, McGregor M. Integrating depression and chronic disease care among patients with diabetes and/or coronary heart disease: the design of the TEAMcare study. Contemp Clin Trials. 2010;31:312–322. doi: 10.1016/j.cct.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, Ciechanowski P, Ludman EJ, Bush T, Young B. Relationship of diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27:2154–2160. doi: 10.2337/diacare.27.9.2154. [DOI] [PubMed] [Google Scholar]
- 37.Shah BR, Hux JE. Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care. 2003;26:510–513. doi: 10.2337/diacare.26.2.510. [DOI] [PubMed] [Google Scholar]
- 38.Wolinsky FD, Overhage JM, Stump TE, Lubitz RM, Smith DM. The risk of hospitalization for congestive heart failure among older adults. Med Care. 1997;35:1031–1043. doi: 10.1097/00005650-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 39.Musselman DL, Betan E, Larsen H, Phillips LS. Relationship of depression to diabetes types 1 and 2: epidemiology, biology, and treatment. Biol Psychiatry. 2003;54:317–329. doi: 10.1016/s0006-3223(03)00569-9. [DOI] [PubMed] [Google Scholar]
- 40.McDonough AK, Curtis JR, Saag KG. The epidemiology of glucocorticoid-associated adverse events. Curr Opin Rheumatol. 2008;20:320–326. doi: 10.1097/BOR.0b013e3282f51031. [DOI] [PubMed] [Google Scholar]
- 41.Lionakis MS, Kontoyiannis DP. Glucocorticoids and invasive fungal infections. Lancet. 2003;362:1828–1838. doi: 10.1016/S0140-6736(03)14904-5. [DOI] [PubMed] [Google Scholar]
- 42.Peavy GM, Lange KL, Salmon DP, Patterson TL, Goldman S, Gamst AC, Mills PJ, Khandrika S, Galasko D. The effects of prolonged stress and APOE genotype on memory and cortisol in older adults. Biol Psychiatry. 2007;62:472–478. doi: 10.1016/j.biopsych.2007.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee BK, Glass TA, McAtee MJ, Wand GS, Bandeen-Roche K, Bolla KI, Schwartz BS. Associations of salivary cortisol with cognitive function in the Baltimore Memory Study. Arch Gen Psychiatry. 2007;64:810–818. doi: 10.1001/archpsyc.64.7.810. [DOI] [PubMed] [Google Scholar]
- 44.Davydow DS, Gifford JM, Desai SV, Bienvenu OJ, Needham DM. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med. 2009;35:796–809. doi: 10.1007/s00134-009-1396-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Unützer J, Katon WJ, Fan MY, Schoenbaum MC, Lin EH, Della Penna RD, Powers D. Long-term cost effects of collaborative care for late-life depression. Am J Manag Care. 2008;14:95–100. [PMC free article] [PubMed] [Google Scholar]
- 46.Simon GE, Katon WJ, Lin EH, Rutter C, Manning WG, Von Korff M, Ciechanowski P, Ludman EJ, Young BA. Cost-effectiveness of systematic depression treatment among people with diabetes mellitus. Arch Gen Psychiatry. 2007;64:65–72. doi: 10.1001/archpsyc.64.1.65. [DOI] [PubMed] [Google Scholar]
- 47.Katon WJ, Russo JE, Von Korff M, Lin EH, Ludman E, Ciechanowski P. Long-term effects on medical costs of improving depression outcomes in patients with depression and diabetes. Diabetes Care. 2008;31:1155–1159. doi: 10.2337/dc08-0032. [DOI] [PMC free article] [PubMed] [Google Scholar]