Abstract
Objective
We previously reported that a history of abuse was associated with a poorer response to combination treatment in the Treatment of Resistant Depression in Adolescents study (TORDIA). We now report on the nature and correlates of abuse that might explain these findings.
Method
Youth who did not benefit from an adequate selective serotonin re-uptake inhibitor (SSRI) trial (N=334) were randomized to: an alternative SSRI; an alternative SSRI plus cognitive behavior therapy (CBT); venlafaxine; or venlafaxine plus CBT. Analyses examined the effect of history of abuse on response to the pharmacotherapy and combination therapy.
Results
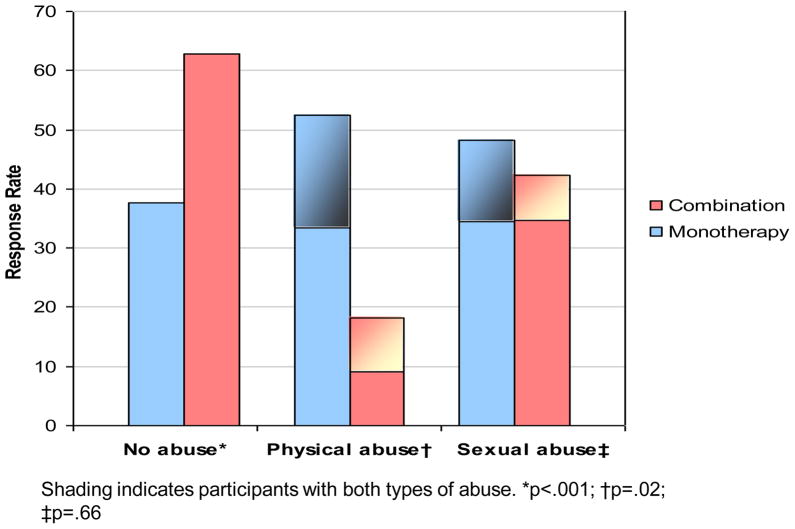
Those without a history of physical abuse (PA) or sexual abuse (SA) had a higher 12-week response rate to combination therapy compared to medication mono-therapy (62.8% vs. 37.6%; OR=2.8, 95% CI: 1.6–4.7, p<0.001). Those with a history of SA had similar response rates to combination vs. medication monotherapy (48.3% vs. 42.3%; OR=1.3, 95% CI: 0.4–3.7; p=0.66), while those with history of PA had a much lower rate of response to combination therapy (18.4% vs. 52.4%, OR=0.1; 95% CI: 0.02–0.43). Even after adjusting for other clinical predictors, a history of PA moderated treatment outcome.
Conclusion
These results should be considered within the limitations of a post-hoc analysis, lack of detailed assessment of abuse and other forms of trauma, and neuropsychological status. Depressed patients with history of abuse, especially PA may require specialized clinical approaches. Further work is needed to understand by what mechanisms a history of abuse affects treatment response.
Keywords: Depression, adolescents, cognitive behavioral therapy, abuse, selective serotonin reuptake inhibitor
Introduction
The relationship between a history of physical or sexual abuse and increased risk of adverse mental health outcomes, including depression is well-established.1, 2 Moreover, childhood history of abuse may be associated with an earlier age of depression onset, more chronic course, and suicidal behavior.3–6 However, there are few studies examining the association between history of abuse and response to treatment among depressed patients, particularly among adolescents.
In a study examining the efficacy of psychotherapy, pharmacotherapy, and combination therapy for chronic depression in adults, Nemeroff et al7 found that participants with a history of child trauma (parental loss, abuse, or neglect) responded better to cognitive behavioral therapy (CBT), with or without the antidepressant nefazodone, compared to antidepressant alone, with a history of physical abuse most strongly accounting for this finding. Both a history of sexual abuse8 and of either experiencing or witnessing actual or threatened serious injury9 have been reported to result in a lower response to CBT in depressed adolescents. In the Treatment for Adolescents with Depression Study (TADS), a history of trauma flattened out expected differences among treatment groups, and in those with history of sexual abuse, there was a non-significant trend for a lower response to CBT only compared to the other treatments.10
In the Treatment of Resistant Depression in Adolescents study (TORDIA) study, we recently found that those with a history of physical or sexual abuse had a superior response to medication mono-therapy compared to the combination of CBT and medication, which is the reverse of the pattern of response found among those without a history of abuse.11, 12 However, in reporting the moderation of treatment response by history of abuse, we did not examine, or control for other possible confounding factors associated with a history of abuse that might influence treatment response, such as age of onset, chronicity, parental psychopathology, family discord, and poverty.13–17
The overarching aim of this secondary analysis of the TORDIA study is to unpack the previously reported relationship between a history of abuse and poorer response to combination treatment12 by examining if: 1) the lower response to combination therapy was among those with history of physical abuse, sexual abuse, or both, and 2) this moderation effect is due to baseline differences in severity and comorbidity, other correlated family variables, treatment variation, or is best be explained by history of abuse itself.
Methods
Participants
All participants had clinically significant depression despite adequate, pre-trial treatment with an SSRI at a dosage equivalent to 20mg. of fluoxetine for at least 4 weeks, with the final 4 weeks at a dosage equivalent to 40mg of fluoxetine, unless this dose could not be tolerated. Significant depression was defined as a total score ≥40 on the Child Depression Rating Scale-Revised (CDRS-R)18 and a score ≥4 on Clinical Global Impression- Severity (CGI-S).19 The CDRS-R is a 17-item scale, which results in total scores ranging from 17 to 113, with a total score ≥40 indicating clinically significant depression.20 The CGI-I is a measure of clinical improvement, as rated on a scale of 1 (very much improved) to 7 (very much worse).19 Both the CDRS and CGI-I were completed by an independent evaluator (IE), blind to treatment assignment.
Exclusion criteria were: completing ≥2 prior adequate SSRI trials; history of non-response to an adequate trial of venlafaxine; prior trial of CBT, with ≥7 sessions; on medications with psychoactive properties, excluding some study-allowed medications at stable doses (≥6 weeks duration); diagnoses of bipolar spectrum disorder, psychosis, autism, eating disorders, substance abuse or dependence; hypertension (diastolic blood pressure ≥90); and females who were pregnant, breast-feeding, or not reliably using contraception.
The study was approved by each site’s local IRB; all participants gave informed assent and consent after they turned age 18, and parents gave informed consent.
Randomization and treatment
Participants were randomly assigned to one of four treatments following the failed SSRI treatment: switching to a second SSRI; switching to venlafaxine; switching to a second SSRI combined with CBT; or switching to venlafaxine combined with CBT. Randomization was balanced both within and across sites on: incoming treatment medication, comorbid anxiety, chronic depression (duration ≥24 months), and suicidal ideation (Beck Depression Inventory [BDI] item 9 ≥2).21
Cognitive Behavioral Therapy
Therapists who provided CBT had at least a master’s degree in a mental health field, and had at least one year prior experience in using this treatment modality. CBT drew upon the manuals that emphasize cognitive restructuring and behavior activation, emotion regulation, social skills, and problem solving for participants, and that also emphasize parent-child sessions to decrease criticism and to improve support, family communication, and problem solving.11 The protocol consisted of 12 weekly sessions (60–90 minutes each) of CBT, 3 to 6 of which were to be family sessions. A median of 9 CBT sessions were delivered across the treatment groups. Therapy audiotapes were reviewed using the Cognitive Therapy Rating Scale22 by on-site supervisors, supervisors in Pittsburgh, and one external consultant, with a high proportion rates as acceptable (>93.9%).
Pharmacotherapy
Participants in the SSRI switch groups who were initially treated with citalopram, sertraline, or fluvoxamine were randomized to receive either fluoxetine or paroxetine. If they were initially treated with fluoxetine, they were switched to receive paroxetine and vice versa. After the FDA warnings on paroxetine, citalopram was used in its stead. The SSRI dosage was 10mg per day for the first week and 20mg per day for weeks 2 to 6, with an option to increase to 40mg per day if there was insufficient clinical improvement (CGI-I ≥3). The venlafaxine dosages for weeks 1 to 4 were 37.5, 75, 112.5, and 150 mg, respectively, with an option to increase to 225mg at week 6. If intolerable adverse effects developed after a medication increase, the participant’s dosage was lowered to either 20 mg of an SSRI or to 150 mg of venlafaxine.
Pharmacotherapists were either psychiatrists or master’s degree–nurses working with the supervision of a psychiatrist. The study psychiatrist examined participants at entry, 6 weeks, and 12 weeks. Medication sessions were 30–60 minutes in duration and included assessment of vital signs, adverse effects, safety, and symptomatic response, and occurred weekly for the first 4 weeks and every other week thereafter.
Blinding Procedure
The intent was for study participants and clinicians to be blinded to medication treatment assignment and for IE to be blinded to both medication and CBT assignment. Blinding for medication was maintained by use of 3 encapsulated pills daily for all prescriptions, some of which might be placebo to mask drug type and dose. The blinding to CBT for IE was maintained by scheduling the IE’s assessments at a time not contiguous with CBT sessions and by asking participants and staff not to discuss CBT treatment assignment when the IE was present. In 64 cases, the blinding of the IE was compromised, most commonly because of participant disclosure of receiving CBT, although results were similar after controlling for the effects of unblinding.11
Outcome and measures
The primary outcome, “adequate clinical response” at week 12, was defined as at 50% reduction in CDRS score and a Clinical Global Impressions- Improvement (CGI-I) score ≤2. The Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL) was used to ascertain DSM-IV diagnoses of major depressive disorder and comorbid conditions.23 History of lifetime physical and sexual abuse was assessed among other traumatic events in the post traumatic stress disorder section the K-SADS-PL. Physical abuse was defined as “bruises sustained on more than one occasion, or more serious injury sustained”. Sexual abuse, on the other hand, was defined as isolated or repeated incidents of genital fondling, oral sex, or vaginal or anal intercourse”. The adolescents were also assessed for hopelessness, suicidal ideation, alcohol and substance use, and family conflict using the Beck Hopelessness Scale (BHS)24, Suicide Ideation Questionnaire-Jr (SIQ-Jr),25 Drug Use Screening Instrument (DUSI)26 and Conflict Behavior Questionnaire- Adolescent version and Parent versions (CBQ-A and CBQ-P),27 respectively. Functional status was assessed by the IE using the Children’s Global Adjustment Scale (CGAS).28
Inter-rater Reliability
Inter-rater reliability was monitored throughout the study and remained high for diagnosis of depression and dysthymia (κ=0.70; 95% CI, 0.49–0.89; N=150), for CDRS-R (intra-class correlation coefficient=0.85; 95%CI, 0.80–0.89; N=324), and for both the CGI-S and CGI-I (for both, intra-class correlation coefficient=0.84; 95% CI, 0.74–0.89; N=176).
Statistical analysis
The Statistical Package for Social Sciences (SPSS 14.0) was used to conduct statistical analysis. Pearson chi-square and independent sample t-test were conducted to examine, in those who received combined treatment, the baseline variables associated with history of abuse, to see if any of these correlates might explain the relationship between abuse and response to combined treatment. Baseline variables significantly associated with abuse were controlled for in a binary logistic regression with response to treatment being the outcome. P-values less than 0.05 were considered to be statistically significant.
Results
Out of the 334 enrolled participants, 43 (13.1%) had a history of physical abuse (PA) and 55 (16.9%) had a history of sexual abuse (SA); of these, 17 patients (5.2%) had a history of both. We conducted analyses both including and excluding the latter 17 participants, and, since findings were similar, we report herein on results including those 17 participants. Those proportions assigned to CBT for those with a history of PA (51.2%) and SA (47.3%) was similar to those without such a history. The response rate was 50.0% among those with a history of SA only, 34.6% in those with history of PA only, and 35.3% among those with history of both physical and sexual abuse.
A history of SA was not related to response in the overall sample (45.5% vs. 48.9%, odds-ratio [OR]=0.9, 95 % confidence interval [CI]:0.5–1.6, p=0.64). There was non-significant trend for PA to be associated with lower response rates compared to no history of PA (34.9% vs. 50.2%, OR=0.5, 95% CI: 0.3–1.0, p=0.06). Figure 1 shows the rates of response in combination vs. medication monotherapy stratified by abuse history. Among participant with no history of either PA or SA, combination therapy had higher rates of response compared to monotherapy (62.8% vs. 37.6%; OR=2.8, 95% CI: 1.6–4.7, p<0.001). Among participants with a history of SA, the rates of response to combination treatment and to medication monotherapy were similar (42.3% vs. 48.3%. OR=0.8, 95% CI: 0.3–2.3; p=0.66). Among adolescents with a history of PA, response rates were significantly lower in the combination condition than in medication monotherapy (18.2% vs. 52.4%, OR= 0.2, 95% CI: 0.1–0.8, p=0.02. The relationship between a history of PA and response to combination therapy persisted even when excluding those 17 participants who had history of both PA and SA (OR=0.09, 95% CI: 0.01–0.6, p=0.01). Excluding those with both PA and SA, PA was found to moderate treatment response to combination treatment relative to those without a history of abuse (p=0.001), whereas for those with a history of SA, the effect of moderation was non-significant (p=0.18).
Figure 1.
Response rate vs. treatment stratified by history and type of abuse.
PA vs. no abuse in those with combination treatment
Because PA but not SA was found to moderate response to combination therapy, we examined the characteristics of those who received combination therapy with PA (with or without history of SA) to those who received combination without a history of PA (Table 1), and also compared those treated with combination treatment with a history of PA vs, SA,
Table 1.
Demographic, clinical, & environmental characteristics of the participants in those who received combined treatment by history of physical abuse
| Physical Abuse | |||
|---|---|---|---|
| No | Yes | p-value | |
| N= 141 | N= 22 | ||
| Demographic Characteristics | |||
| Age (years, MD, SD) | 15.9±1.5 | 16.5±1.2 | 0.09 |
| Sex (N, % Female) | 97 (68.8) | 18 (81.8) | 0.21 |
| Race/Ethnicity (N, %White) | 121 (85.8) | 17 (77.3) | 0.34 |
| Income (median, dollars) | 65,000 | 45,000 | 0.12 |
| Parents’ Education (N, %≥ College Graduate) | 67 (50.4) | 7 (33.3) | 0.15 |
| Clinical Characteristics (M, SD) | |||
| Children’s Depression Rating Scale | 58.7±10.5 | 61.1±12.6 | 0.32 |
| Children’s Global Assessment Scale | 51.2±7.4 | 48.2±7.5 | 0.08 |
| Clinical Global Impressions Severity | 4.5±0.7 | 4.5±0.7 | 0.98 |
| Beck Depression Inventory | 20.4±11.8 | 27.0±15.5 | 0.02 |
| Beck Hopelessness Scale | 10.1±5.3 | 12.3±5.8 | 0.07 |
| Comorbidity | |||
| Anxiety (Including PTSD) | 48 (35.0) | 11 (52.4) | 0.13 |
| Post-Traumatic Stress Disorder | 5 (3.5) | 4 (18.2) | 0.02 |
| Attention Deficient Hyperactivity Disorder | 25 (18) | 4 (18.2) | 0.98 |
| Oppositional/Conduct | 15 (10.8) | 0 (0.0) | 0.22 |
| Dysthymia | 34 (24.5) | 11 (50.0) | 0.01 |
| First Episode | 32 (23.5) | 7 (33.3) | 0.33 |
| Duration Current MDD Episode | 21.7±19.5 | 26.1±20.1 | 0.34 |
| Age Onset Current MDD Episode (yrs) | 14.0±2.1 | 14.1±2.0 | 0.78 |
| DUSI impairment | 11.2±18.3 | 10.0±14.1 | 0.77 |
| History of self-injurious behavior | 49 (35.3) | 14 (63.6) | 0.01 |
| Suicidality | |||
| History of Suicide | 23 (16.3%) | 12 (54.5%) | <0.001 |
| SIQ-Jr | 38.8±22 | 55.5±27.1 | 0.002 |
| Parental Psychopathology | |||
| Beck Depression Inventory | 9.6±9.4 | 6.9±8.3 | 0.24 |
| Beck Anxiety Inventory | 8.5±8.0 | 7.3±6.9 | 0.52 |
| Family Environment | |||
| Conflict Behavior (Adolescent) | 8.4±6.4 | 9.7±6.9 | 0.40 |
| Conflict Behavior (Parent) | 8.9±6.0 | 7.5±5.2 | 0.33 |
Note: DUSI = Drug Use Screening Instrument; MDD = Major Depressive Disorder; PTSD = Post-traumatic Stress Disorder; SIQ-Jr = Suicide Ideation Questionnaire-Jr..
Although those with a history of PA showed no association with any demographic variable, they did have with higher baseline self-reported depression (27.0±15.5 vs. 20.4±11.8, t=−2.3, df=159, p=0.02) and suicidal ideation (55.5±27.1 vs. 38.8±2.0, t=−3.1, df=157, p=0.002), as well as higher lifetime rates of PTSD (OR=6.0; 95% CI: 1.5–24.6), dysthymia, (OR=3.1, 95% CI 1.2–7.8) suicide attempts (OR=6.2, 95% CI, 2.4–15.9), and non-suicidal self injurious behavior (OR=3.2, 95% CI: 1.3–8.2).
There were no differences between those with and without a history of PA with respect to attended CBT sessions (7.0±4.6 vs. 8.5±3.4, t=1.5, df= 24.7, p=0.15) or the frequency of receipt of the different CBT components. There was a non-significant tendency for those with a history of PA to have attended fewer pharmacotherapy sessions as compared to the no-PA group (6.6±2.8 vs. 7.8±2.1, t= −1.9, df=24.9, p=0.06). There were also no differences between the two groups with respect to medication assignment (54.5% vs. 48.9% assigned to an SSRI, χ2=0.24, p=0.62), the type of SSRI they were switched to (50.0% vs. 52.2% switched to fluoxetine, χ2=0.02, p=0.89), the maximum dose of SSRI (34.2±10.8 vs. 31.8±9.9mg, t=0.7, df=79, p=0.47), or maximum dose of venlafaxine (161.2±75.1 vs. 179.2±54.2mg, t=−0.9, df=80, p=0.35). There was also no difference between the two groups with respect to prescription of adjunctive medications for sleep (22.7% vs. 15.6%, Fisher’s exact test [FET]: p=0.37) or anxiety (9.1% vs. 3.5%, FET: p=0.23).
In the full logistic model assessing the impact of PA, adolescents with history of PA were only one-tenth (OR=0.08; 95% CI: 0.02–0.36) as likely to have adequate response to combined treatment as compared to the no-PA group, even after controlling for age, baseline self-reported psychopathology (suicidal ideation, depression, hopelessness), comorbidity (PTSD, dysthymia), history of suicide attempts and NSSI, number of CBT sessions, and number of pharmacotherapy session, CGAS score, and site (Table 2). The most parsimonious model, obtained by backwards-stepping logistic regression, retained PA history (OR= 0.08; 95% CI: 0.02–0.32), age, BDI, number of CBT sessions attended, history of PTSD, and site (Table 2). History of PA had no significant interaction with any of the variables retained in the last step of the backward mode (all p-values>0.05).
Table 2.
Multivariable logistic regression model predicting adequate response to combination treatment at week 12.
| p-value | OR | 95% CI | |
|---|---|---|---|
| Full model | |||
| History of physical abuse | <0.01 | 0.08 | 0.02–0.36 |
| Number of CBT sessions | 0.23 | 1.13 | 0.92–1.38 |
| Number of pharmacotherapy sessions | 0.94 | 0.99 | 0.72–1.36 |
| Beck Depression Inventory | 0.11 | 0.96 | 0.92–1.01 |
| History of Post-Traumatic Stress Disorder | 0.03 | 13.7 | 1.32–141.9 |
| History of suicide attempt | 0.96 | 0.97 | 0.31–3.07 |
| History of self-injurious behavior | 0.21 | 0.58 | 0.24–1.36 |
| History of dysthymia | 0.98 | 1.01 | 0.37–2.74 |
| SIQ-JR | 0.30 | 1.01 | 0.99–1.04 |
| Age | 0.08 | 1.29 | 0.97–1.71 |
| Children’s Global Adjustment Scale | 0.36 | 1.03 | 0.97–1.09 |
| Beck Hopelessness Scale | 0.14 | 0.93 | 0.85–1.02 |
| Site | 0.13 | - | - |
| Backward model | |||
| History of physical abuse | <0.01 | 0.08 | 0.02–0.32 |
| Number of CBT session | 0.03 | 1.13 | 1.01–1.27 |
| Beck Depression Inventory | <0.01 | 0.95 | 0.92–0.99 |
| Age | 0.04 | 1.33 | 1.01–1.75 |
| Post-traumatic Stress Disorder | 0.03 | 12.64 | 1.26–126.54 |
| Site | 0.09 | - | - |
Note: Hosmer and Lemeshow: Full Model, χ28=4.17, p=0.84; Backward Model, χ28=8.01, p=0.43. CBT = Cognitive Behavioral Therapy; CI = Confidence interval; SIQ-Jr = Suicide Ideation Questionnaire-Jr.
Within those participants who received combination treatment, those with a history of PA were more likely than those with a history of SA to be male (26.7% vs. 0.0%, FET, p=0.03), have higher SIQ scores (55.3±31.2 vs. 35.7±17.2, t=2.1, df=21.5, p=0.04), but lower DUSI scores (8.0±9.2 vs. 21.8±24.2, t=−2.2, df=22.5, p=0.04); these differences were not sufficient to explain the better response to combination treatment in those with a history of SA vs. PA.
Discussion
In this paper, we have found that the negative impact of a history of abuse on response to combination treatment relative to medication monotherapy in the TORDIA study is mostly explained by a history of physical abuse.12 In those with a history of SA, the responses to combination treatment and medication monotherapy were similar, whereas in those without a history of abuse, combination treatment is clearly superior. Those participants with a history of PA had many characteristics that might be expected to predict a poorer response to treatment, namely higher self-reported depression, suicidal ideation, hopelessness, and history of PTSD, dysthymic disorder, suicide attempt, and non-suicidal self-injury. However, even after controlling for these variables, adolescents with a history of PA were still 10 times as likely to have an adequate response to medication monotherapy as to combined treatment. Thus, we are not able to identify the mechanism by which physical abuse affects treatment outcome, except to say that it is not attributable to differences in baseline characteristics, or amount or quality of treatment received.
These results should be considered within the context of strengths and limitations of this study. This study is one of the first to examine the impact of different types of abuse on treatment outcome in depressed adolescents, and randomization was preserved with respect to the rates of abuse across treatment cells. Treatment was randomly assigned and was carefully monitored for quality. On the other hand, TORDIA was not designed to examine the best modality of treating depression among youth with a history of abuse. Although the sample size of TORDIA is relatively large, the number of participants with a history of abuse is relatively small. We did not collect details about severity, frequency, duration, and timing of abuse, and the relation between victim and perpetrator. In addition, neglect, verbal abuse, and other traumatic or stressful life events, such as witnessing domestic violence, or loss of a relative or friend were not assessed, all of which have been shown to have an impact on clinical outcome.2, 29–31 The PTSD screen of the KSADS has limitations as an assessment of abuse and may miss more than 1/3 of youth with abuse histories.32 Finally, because this study excluded youth who were not living with their primary caregiver, these results might not be generalizable to children with active protective services involvement, who often receive pharmacological treatment.33
In this report, adolescents with history of PA had higher rates of PTSD than those without history of PA. It has been shown that exposure therapy, such as trauma-focused CBT (TF-CBT), is more effective that supportive treatment for the treatment of abused youth with PTSD,34–36 and in those studies, this treatment was also more efficacious in reducing depressive symptoms.35 Moreover, Cohen et al reported that augmenting TF-CBT with sertraline did not further improve PTSD symptoms as compared to TF-CBT monotherapy.37 In contrast, the depression-focused CBT in TORDIA did not include either exposure therapy or trauma-focused sessions. Nevertheless, the negative impact of a history of PA on response to combination treatment persisted even after controlling for PTSD, suggesting that this comorbid disorder alone did not explain the poorer response of CBT in those with a history of PA. Similarly, the impact of PA on outcome persisted after controlling of other negative prognosticators for outcome, such as greater depressive severity, suicidal ideation, hopelessness, dysthymic disorder, or history of non-suicidal self-injury, suggesting that the impact of PA on outcome was not just explained by higher symptomatology or more complex clinical presentation.12, 38
Fergusson and colleagues13, 39 reported that history of trauma is a marker for chronic environmental stress leading to more adverse psychiatric outcome in the adults. However, in the TORDIA combination therapy group, there was no difference between the physical and non-PA groups with respect to current family conflict. Moreover, active abuse was an exclusion from the TORDIA clinical trial. Therefore, the poorer response of physically abused participants more likely reflects an effect of abuse per se rather than of associated ongoing environmental adversity, at least with respect to family conflict, socioeconomic status, and parental self-reported depression.
Previous studies have documented a difference in response to treatment between those with and without history of abuse.7, 8 In chronically depressed adults, Nemeroff et al 7 found that a significant interaction between history of physical (but not sexual) abuse and treatment outcome. Patients with trauma history, defined as PA, parental loss, or other trauma, preferentially responded to psychotherapy versus medication. This finding is in the opposite direction of our finding in TORDIA. This difference in findings in the Nemeroff et al. study compared to TORDIA could be due to their wider definition of trauma, difference in age group, or use of a different modality of psychotherapy, cognitive behavioral analysis system of psychotherapy, which has a greater interpersonal focus than the CBT employed in this study. On the other hand, in the treatment of adolescent depression, a history of abuse, trauma, or maltreatment is associated with a less vigorous response to CBT, whether compared to other forms of psychotherapy or to medication, although in previous reports, sexual abuse had a more profound effect than physical abuse.8–10
It is unclear why PA showed such a poor response to combination treatment, as compared to participants with a history of SA. This difference was not attributable to baseline differences in the two sub-samples. Nevertheless, even a history of sexual abuse had an impact on outcome, since those with a history of SA were half as likely to respond to combination therapy, and 1.4 times more likely to respond to medication monotherapy compared to those with no history of SA. While these findings were not as pronounced as those findings in those with a history of PA, and we were not able to demonstrate statistically significant evidence of moderation, these findings were certainly consistent with other reports in the literature.8, 10 While there were few baseline differences between those with a history of PA vs. SA, there could have been differences in important domains that were not assessed, such as frequency or severity of abuse, history of neglect, verbal abuse, intercurrent life events, family history of psychiatric disorder, attachment style, or neuropsychological functioning. Another possibility is that PA and SA actually do result in different risks for psychopathology40 and response to treatment. Unfortunately, the literature is inconsistent when comparing the impact of SA vs. PA.2, 7, 8, 10
Abuse is known to have profound developmental neurobiological effects that might in turn influence treatment response. Successful participation in CBT psychotherapy for depression involves the ability to form a relationship, to learn and remember, to participate in rewarding activities, and to face unpleasant emotions. The effects of abuse could undercut all of these domains, since abuse negatively impacts the development of interpersonal relationships, attention, executive function, working memory, and response to reward, and also increases attentional bias away from threat.41–43 These findings are likely reflections of the impact of abuse on brain development in critical regions such as the corpus collusum, hippocampus, and prefrontal cortex.44, 45 Since many sequelae are in proportion to the current severity of PTSD, it may be the psychotherapeutic approaches that target trauma may be required prior to engagement in CBT for depression.
In summary, these results support further investigation of the mechanisms by which maltreatment history confers an apparently greater treatment resistance to depression-focused CBT. In particular, both those with a history of PA and SA showed a lower response to combination treatment than was found in those without an abuse history, and, in the case of PA, response to medication was greatly superior to combination therapy. Furthermore, this effect of PA persisted even after adjusting for other clinical correlates known to convey treatment resistance. These data suggest that this group of patients may require a specialized approach, which could include trauma-focused CBT, and other psychotherapeutic approaches that take into account the neurpsychological profile of the depressed youth with a history of abuse. Future treatment studies should gather better information on history of abuse, other traumas, as well as the neuropsychological profile of such youth, in order to understand the processes that may moderate treatment response and to develop treatments that better target depression in youth with a history of abuse.
Acknowledgments
This work was supported by National Institute of Mental Health (NIMH) grants MH61835 (Pittsburgh); MH61856 (Galveston); MH61864 (UCLA); MH61869 (Portland); MH61958 (Dallas); and MH62014 (Brown), and MH66371 (Pittsburgh). NIMH program staff participated in the design, implementation, analysis, and preparation of reports of the study.
We thank the families and adolescents who participated in this study. We are indebted to the NIMH Data and Safety Monitoring Board for monitoring the progress of the study. We also thank all contributing individuals listed in the original report of this study13 for their important assistance in the conduct of this study.
Footnotes
The opinions and assertions contained in this report are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Health and Human Services, the National Institutes of Health, or the NIMH.
Clinical Trial Registry Information: Treatment of SSRI-Resistant Depression in Adolescents(TORDIA); NCT00018902; http://www.clinicaltrials.gov.
Disclosure: Dr. Asarnow has served as a consultant for Pfizer. She has received funding from Philip Morris. A family member receives funding from Bristol-Myers Squibb, and has served as a consultant for Roche, Novartis, Sanofi-Adventis, and Janssen.
Dr. Wagner has received research support from the National Institute of Mental Health, and has served on the advisory board for Forest.
Dr. Birmaher receives research support from the National Institute of Mental Health. He has served as a consultant for Schering Plough. He has participated in advisory board forums sponsored by Dey Pharma, L.P., and Forest. He has received royalties from Random House and Lippincott Williams and Wilkins.
Dr. Keller has served as a consultant or received honoraria from Abbott, CENEREX, Cephalon, Cypress Bioscience, Cyberonics, Forest, Janssen, JDS, Medtronic, Organon, Novartis, Pfizer, Roche, Solvey, Wyeth, and Sierra Neuropharmaceuticals. He has received research support from Pfizer. He has served on the advisory boards for Abbott, Bristol-Myers Squibb, CENEREX, Cyberonics, Cypress Bioscience, Forest, Janssen, Neuronetics, Novartis, Organon, and Pfizer.
Dr. McCracken has received research support from Seaside Pharmaceuticals, Bristol-Myers Squibb, and Aspect. He has served as a consultant to BioMarin and Shionogi. He has received honoraria from the American Academy of Child and Adolescent Psychiatry, the Tourette Syndrome Association, CME Outfitters, and Veritas.
Dr. Emslie has received research support from Biobehavioral Diagnostics, Eli Lilly and Co., Forest, GlaxoSmithKline, and Somerset. He has served as a consultant for Biobehavioral Diagnostics, Eli Lilly and Co., Forest, GlaxoSmithKline, Pfizer, and Wyeth.
Dr. Brent has received research support from the National Institute of Mental Health. He has received royalties from Guilford Press. He serves as an editor for UpToDate Psychiatry.
Drs. Shamseddeen, Clarke, Vitiello, Iyengar, and Ryan, and Ms. Mayes and Ms. Porta report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fergusson DM, Boden JM, Horwood LJ. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse Negl. 2008 Jun;32(6):607–619. doi: 10.1016/j.chiabu.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 2.Green JG, McLaughlin KA, Berglund PA, et al. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010 Feb;67(2):113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Enns MW, Cox BJ, Afifi TO, De Graaf R, Ten Have M, Sareen J. Childhood adversities and risk for suicidal ideation and attempts: a longitudinal population-based study. Psychol Med. 2006 Dec;36(12):1769–1778. doi: 10.1017/S0033291706008646. [DOI] [PubMed] [Google Scholar]
- 4.Bifulco A, Brown GW, Moran P, Ball C, Campbell C. Predicting depression in women: the role of past and present vulnerability. Psychol Med. 1998 Jan;28(1):39–50. doi: 10.1017/s0033291797005953. [DOI] [PubMed] [Google Scholar]
- 5.Brown GW, Moran P. Clinical and psychosocial origins of chronic depressive episodes. I: A community survey. Br J Psychiatry. 1994 Oct;165(4):447–456. doi: 10.1192/bjp.165.4.447. [DOI] [PubMed] [Google Scholar]
- 6.Brown GW, Harris TO, Hepworth C, Robinson R. Clinical and psychosocial origins of chronic depressive episodes. II. A patient enquiry. Br J Psychiatry. 1994 Oct;165(4):457–465. doi: 10.1192/bjp.165.4.457. [DOI] [PubMed] [Google Scholar]
- 7.Nemeroff CB, Heim CM, Thase ME, et al. Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma. Proc Natl Acad Sci U S A. 2003 Nov 25;100(24):14293–14296. doi: 10.1073/pnas.2336126100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barbe RP, Bridge JA, Birmaher B, Kolko DJ, Brent DA. Lifetime history of sexual abuse, clinical presentation, and outcome in a clinical trial for adolescent depression. J Clin Psychiatry. 2004 Jan;65(1):77–83. doi: 10.4088/jcp.v65n0113. [DOI] [PubMed] [Google Scholar]
- 9.Shirk SR, Kaplinski H, Gudmundsen G. School-Based Cognitive-Behavioral Therapy for Adolescent Depression. Journal of Emotional and Behavioral Disorders. 2009;17(2):106–117. [Google Scholar]
- 10.Lewis CC, Simons AD, Nguyen LJ, et al. Impact of Childhood Trauma on Treatment Outcome in the Treatment for Adolescents with Depression Study (TADS) J Am Acad Child Adolesc Psychiatry. 2010 Feb;49(2):132–140. doi: 10.1097/00004583-201002000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. 2008 Feb 27;299(8):901–913. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asarnow JR, Emslie G, Clarke G, et al. Treatment of selective serotonin reuptake inhibitor-resistant depression in adolescents: predictors and moderators of treatment response. J Am Acad Child Adolesc Psychiatry. 2009 Mar;48(3):330–339. doi: 10.1097/CHI.0b013e3181977476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fergusson DM, Lynskey MT, Horwood LJ. Childhood sexual abuse and psychiatric disorder in young adulthood: I. Prevalence of sexual abuse and factors associated with sexual abuse. J Am Acad Child Adolesc Psychiatry. 1996 Oct;35(10):1355–1364. doi: 10.1097/00004583-199610000-00023. [DOI] [PubMed] [Google Scholar]
- 14.Kaufman J, Birmaher B, Brent D, Dahl R, Bridge J, Ryan ND. Psychopathology in the relatives of depressed-abused children. Child Abuse Negl. 1998 Mar;22(3):171–181. doi: 10.1016/s0145-2134(97)00170-1. [DOI] [PubMed] [Google Scholar]
- 15.Bernet CZ, Stein MB. Relationship of childhood maltreatment to the onset and course of major depression in adulthood. Depress Anxiety. 1999;9(4):169–174. [PubMed] [Google Scholar]
- 16.Arnow BA. Relationships between childhood maltreatment, adult health and psychiatric outcomes, and medical utilization. J Clin Psychiatry. 2004;65 (Suppl 12):10–15. [PubMed] [Google Scholar]
- 17.Zielinski DS. Child maltreatment and adult socioeconomic well-being. Child Abuse Negl. 2009 Oct;33(10):666–678. doi: 10.1016/j.chiabu.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 18.Poznanski EO, Freeman LN, Mokros HB. Children’s Depression Rating Scale—Revised. Psychopharmacol Bull. 1985:21. [Google Scholar]
- 19.Guy E. ECDEU Assessment Manual for Psychopharmacology - Revised. Rockville, MD: National Institutes of Mental Health; 1976. [Google Scholar]
- 20.Poznanski EO, Mokros HB. Children’s Depression Rating Scale - Revised. Los Angeles, CA: Western Psychological Services; 1996. [Google Scholar]
- 21.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961 Jun;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 22.Vallis TM, Shaw BF, Dobson KS. The Cognitive Therapy Scale: psychometric properties. J Consult Clin Psychol. 1986 Jun;54(3):381–385. doi: 10.1037//0022-006x.54.3.381. [DOI] [PubMed] [Google Scholar]
- 23.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997 Jul;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Beck AT, Steer RA. Manual for the Beck Hopelessness Scale. San Antonio, Tx: Psychological Corporation; 1988. [Google Scholar]
- 25.Reynolds WM. Suicidal Ideation Questionnaire: Professional Manual. Odessa, FL: Psychological Assessment Resources; 1988. [Google Scholar]
- 26.Kirisci L, Mezzich A, Tarter R. Norms and sensitivity of the adolescent version of the drug use screening inventory. Addict Behav. 1995 Mar–Apr;20(2):149–157. doi: 10.1016/0306-4603(94)00058-1. [DOI] [PubMed] [Google Scholar]
- 27.Robin AL, Foster SL. Negotiating parent-adolescent conflict. New York: Guilford Press; 1989. [Google Scholar]
- 28.Shaffer D, Gould MS, Brasic J, et al. A children’s global assessment scale (CGAS) Arch Gen Psychiatry. 1983 Nov;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 29.Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. Am J Public Health. 2001 May;91(5):753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teicher MH, Samson JA, Polcari A, McGreenery CE. Sticks, stones, and hurtful words: relative effects of various forms of childhood maltreatment. Am J Psychiatry. 2006 Jun;163(6):993–1000. doi: 10.1176/ajp.2006.163.6.993. [DOI] [PubMed] [Google Scholar]
- 31.Wiersma JE, Hovens JG, van Oppen P, et al. The importance of childhood trauma and childhood life events for chronicity of depression in adults. J Clin Psychiatry. 2009 Jul;70(7):983–989. doi: 10.4088/jcp.08m04521. [DOI] [PubMed] [Google Scholar]
- 32.Grasso D, Boonsiri J, Lipschitz D, et al. Posttraumatic stress disorder: the missed diagnosis. Child Welfare. 2009;88(4):157–176. [PMC free article] [PubMed] [Google Scholar]
- 33.Zito JM, Safer DJ, Sai D, et al. Psychotropic medication patterns among youth in foster care. Pediatrics. 2008 Jan;121(1):e157–163. doi: 10.1542/peds.2007-0212. [DOI] [PubMed] [Google Scholar]
- 34.King NJ, Tonge BJ, Mullen P, et al. Treating sexually abused children with posttraumatic stress symptoms: a randomized clinical trial. J Am Acad Child Adolesc Psychiatry. 2000 Nov;39(11):1347–1355. doi: 10.1097/00004583-200011000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. J Am Acad Child Adolesc Psychiatry. 2004 Apr;43(4):393–402. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deblinger E, Mannarino AP, Cohen JA, Steer RA. A follow-up study of a multisite, randomized, controlled trial for children with sexual abuse-related PTSD symptoms. J Am Acad Child Adolesc Psychiatry. 2006 Dec;45(12):1474–1484. doi: 10.1097/01.chi.0000240839.56114.bb. [DOI] [PubMed] [Google Scholar]
- 37.Cohen JA, Mannarino AP, Perel JM, Staron V. A pilot randomized controlled trial of combined trauma-focused CBT and sertraline for childhood PTSD symptoms. J Am Acad Child Adolesc Psychiatry. 2007 Jul;46(7):811–819. doi: 10.1097/chi.0b013e3180547105. [DOI] [PubMed] [Google Scholar]
- 38.Brent DA, Kolko DJ, Birmaher B, et al. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. J Am Acad Child Adolesc Psychiatry. 1998 Sep;37(9):906–914. doi: 10.1097/00004583-199809000-00010. [DOI] [PubMed] [Google Scholar]
- 39.Fergusson DM, Horwood LJ, Lynskey MT. Childhood sexual abuse and psychiatric disorder in young adulthood: II. Psychiatric outcomes of childhood sexual abuse. J Am Acad Child Adolesc Psychiatry. 1996 Oct;35(10):1365–1374. doi: 10.1097/00004583-199610000-00024. [DOI] [PubMed] [Google Scholar]
- 40.Muehlenkamp JJ, Kerr PL, Bradley AR, Adams Larsen M. Abuse subtypes and nonsuicidal self-injury: preliminary evidence of complex emotion regulation patterns. J Nerv Ment Dis. 2010 Apr;198(4):258–263. doi: 10.1097/NMD.0b013e3181d612ab. [DOI] [PubMed] [Google Scholar]
- 41.Beers SR, De Bellis MD. Neuropsychological function in children with maltreatment-related posttraumatic stress disorder. Am J Psychiatry. 2002 Mar;159(3):483–486. doi: 10.1176/appi.ajp.159.3.483. [DOI] [PubMed] [Google Scholar]
- 42.Pine DS, Mogg K, Bradley BP, et al. Attention bias to threat in maltreated children: implications for vulnerability to stress-related psychopathology. Am J Psychiatry. 2005 Feb;162(2):291–296. doi: 10.1176/appi.ajp.162.2.291. [DOI] [PubMed] [Google Scholar]
- 43.Guyer AE, Kaufman J, Hodgdon HB, et al. Behavioral alterations in reward system function: the role of childhood maltreatment and psychopathology. J Am Acad Child Adolesc Psychiatry. 2006 Sep;45(9):1059–1067. doi: 10.1097/01.chi.0000227882.50404.11. [DOI] [PubMed] [Google Scholar]
- 44.Jackowski AP, Douglas-Palumberi H, Jackowski M, et al. Corpus callosum in maltreated children with posttraumatic stress disorder: a diffusion tensor imaging study. Psychiatry Res. 2008 Apr 15;162(3):256–261. doi: 10.1016/j.pscychresns.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Coplan JD, Abdallah CG, Tang CY, et al. The role of early life stress in development of the anterior limb of the internal capsule in nonhuman primates. Neurosci Lett. 2010 Aug 16;480(2):93–96. doi: 10.1016/j.neulet.2010.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]