Abstract
A range of innovative computer-based interventions for psychiatric disorders have been developed, and are promising for drug use disorders, due to reduced cost and greater availability compared to traditional treatment. Electronic searches were conducted from 1966 to November 19, 2009 using MEDLINE, Psychlit, and EMBASE. 468 non-duplicate records were identified. Two reviewers classified abstracts for study inclusion, resulting in 12 studies of moderate quality. Eleven studies were pilot or full-scale trials compared to a control condition. Interventions showed high acceptability despite substantial variation in type and amount of treatment. Compared to treatment-as-usual, computer-based interventions led to less substance use as well as higher motivation to change, better retention, and greater knowledge of presented information. Computer-based interventions for drug use disorders have the potential to dramatically expand and alter the landscape of treatment. Evaluation of internet and phone-based delivery that allow for treatment-on-demand in patients’ own environment is needed.
Automated computer-based treatment is a promising vehicle for providing behaviorally-based interventions for drug use disorders. These systems offer a number of potential advantages, including low cost, greater accessibility and 24-hour availability, opportunity for more frequent and/or longer therapeutic contact, greater confidentiality, increased flexibility and convenience, and increased opportunities for practicing skills (Budman, 2000; Marks, Shaw, & Parkin, 1998; Nadelson, 1987). Such systems may even be preferred by some clients who dislike therapy or have concerns about confidentiality, and may be particularly useful in rural or remote settings, where access to psychotherapy for substance use disorders may be limited and accompanied by increased stigma (Connors, Tonnigan, & Miller, 2001; Hall & Huber, 2000). Automated computer-based systems also offer more consistent and precise delivery of interventions across patients. This standardization can be of value therapeutically and, from a scientific perspective, may permit a detailed examination of active components. The current systematic review evaluated computer-based interventions for drug use disorders.
Computer-based interventions have been shown to be effective for psychiatric disorders such as depression and anxiety (Cavanagh & Shapiro, 2004; Kaltenthaler, Parry, Beverley, & Ferriter, 2008; Reger & Gahm, 2009; Spek et al., 2007) and health issues such as diabetes, poor nutrition and sexual risk behaviors (Montani, Bellazzi, Quaglini, & d'Annunzio, 2001; Portnoy, Scott-Sheldon, Johnson, & Carey, 2008; Ybarra & Bull, 2007). Computer-based interventions for anxiety have shown moderate to large mean effect sizes compared to wait list controls or placebo (weighted, Hedges’ g = .76 to .88; Cavanagh & Shapiro, 2004; Reger & Gahm, 2009; Spek et al., 2007; and unweighted, Cohen’s d = .96: Cavanagh & Shapiro, 2004; Reger & Gahm, 2009; Spek et al., 2007). In contrast, mean effect sizes for depression (unweighted d =.27, weighted g = .34), sexual risk behavior (unweighted d = .26 to .35), poor nutrition (unweighted d =.15), and health maintenance (unweighted d =.18) have also been significant, though substantially smaller (Carroll et al., 2008; Cavanagh & Shapiro, 2004; Noar, Black, & Pierce, 2009; Portnoy et al., 2008; Spek et al., 2007).
Computer and internet based systems for addressing substance use disorders have also been developed in recent years, with encouraging evidence suggesting positive treatment outcomes (Carroll et al., 2008; Carroll & Rounsaville, 2007; Copeland & Martin, 2004; Marsch, Bickel, & Grabinski, 2007; Myung, McDonnell, Kazinets, Seo, & Moskowitz, 2009). Much of the research has focused on alcohol abuse and tobacco. For tobacco, meta-analyses have shown abstinence rates from computer-based interventions are about 1.5 times higher than control conditions (Myung et al., 2009). Computer-based alcohol-related interventions are generally well received (Bewick et al., 2008) and significantly improve alcohol use outcomes compared to no treatment and assessment only interventions (Carey, Scott-Sheldon, Elliott, Bolles, & Carey, 2009; Elliott, Carey, & Bolles, 2008). However, estimated effect sizes for alcohol-related interventions tend to be lower than those for tobacco (Carey et al., 2009; Portnoy et al., 2008). This may be due to differences in length of respective computer-based interventions since interventions in tobacco studies (e.g., 10–12 weeks) tend to be longer than those in alcohol studies (e.g., short assessment with personalized feedback). Moreover, within computer-based smoking cessation trials, those with longer interventions appear to be associated with higher effect sizes (Myung et al., 2009).
To our knowledge only one systematic review included illicit drug abuse. Portnoy and colleagues (2008) presented a meta-analysis of 11 studies of alcohol and drug use disorders, only 1 of which evaluated drug use. Thus, the aim of the current study was to conduct a systematic review of computer-based interventions for illicit drug use disorders.
Methods and Materials
Search Strategies
Studies were identified in the Ovid MEDLINE and PsychINFO databases from 1966 to November 19, 2009 using the subject headings and text words found in Table 1. The computer-related terms were combined with the intervention terms using the “adj5” operator for Ovid and the “w/5” operator for Scopus and those results were combined with the drug-related terms using the Boolean “and” operator. The abstracts of all results of the search were independently reviewed for possible inclusion by three of five authors (BM, BG, TF). Studies were included if they: 1) reported findings of a research study (not a review, letter, etc.); 2) involved a computer-based intervention; 3) enrolled patients with a substance-related disorder that was not alcohol or tobacco. Computer-based interventions were defined as a those in which the primary treatment was provided by an automated, computer-based system rather than etherapy or etreatment in which a computer is used as the method of providing therapist-based treatment (e.g., video or audio conferencing, email contact, or therapist-based texting). Study inclusion/exclusion agreement between authors was measured using kappa and disagreement was settled by consensus between all authors.
Table 1.
Specific Medical Subject Headings (MeSH) Terms and Text Words in MEDLINE, EMBASE and PsychINFO
| Concept | MeSH terms | Text words |
|---|---|---|
| Computer-related | Therapy, computer-assisted/a or online therapy/b or computer assisted therapy/b | Computer assist* or computer tailor* or computer base* or computer guide* or computer administer* or computerized or computerized or internet assist* or internet tailor* or internet base* or internet guide* or web assist* or web tailor* or web base* or web guide* or interactive voice or automated telephone or automated phone or ivr or tivr or; interapy or software base* or software assist* or interactiv* |
| Intervention | Intervention or therapy or treatment | |
| Drug-related | Exp addiction/ or exp drug users/ or exp methadone maintenance/ | Substance abuse or substance related disorder* or drug abuse or "drug use" or addiction or opioid or opiate or heroin or stimulant* or cocaine or marijuana or cannabis or amphetamine* or methamphetamine* or sedative* or hallucinogen* or ecstasy or mdma or inhalant* or ketamine or polydrug or tobacco or smoking or alcohol or drinking |
MEDLINE term
PsychINFO term.
Full manuscripts of articles chosen for possible inclusions were independently reviewed by two authors (DB, CC), and were evaluated based on the same criteria above. Discrepancies were settled by review and consensus between all authors.
Data Extraction
Data about study methodology and outcomes were extracted by two reviewers independently using a custom-designed data collection form. Briefly, data were collected on: 1) study design; 2) subject selection; 3) inclusion/exclusion criteria; 4) sample description (N, group n’s, age, gender, education, race/ethnicity); 5) Setting; 6) Intervention details (modality, duration, number of sessions, length of sessions, type of therapy); 7) Outcomes.
Due to the heterogeneous nature of the studies (in terms of populations, research designs and outcome measures) it was not deemed appropriate to combine the data using meta-analysis.
Assessment of Study Quality
Two authors independently assigned a quality index score according to a 31-point scale proposed by Downs and colleagues that assesses reporting, external validity, bias (internal validity), confounding (external validity), and power (Downs & Black, 1998). Inter-rater agreement on this scale was assessed by computing Pearson’s product moment correlation coefficient.
Results
Literature Search Results
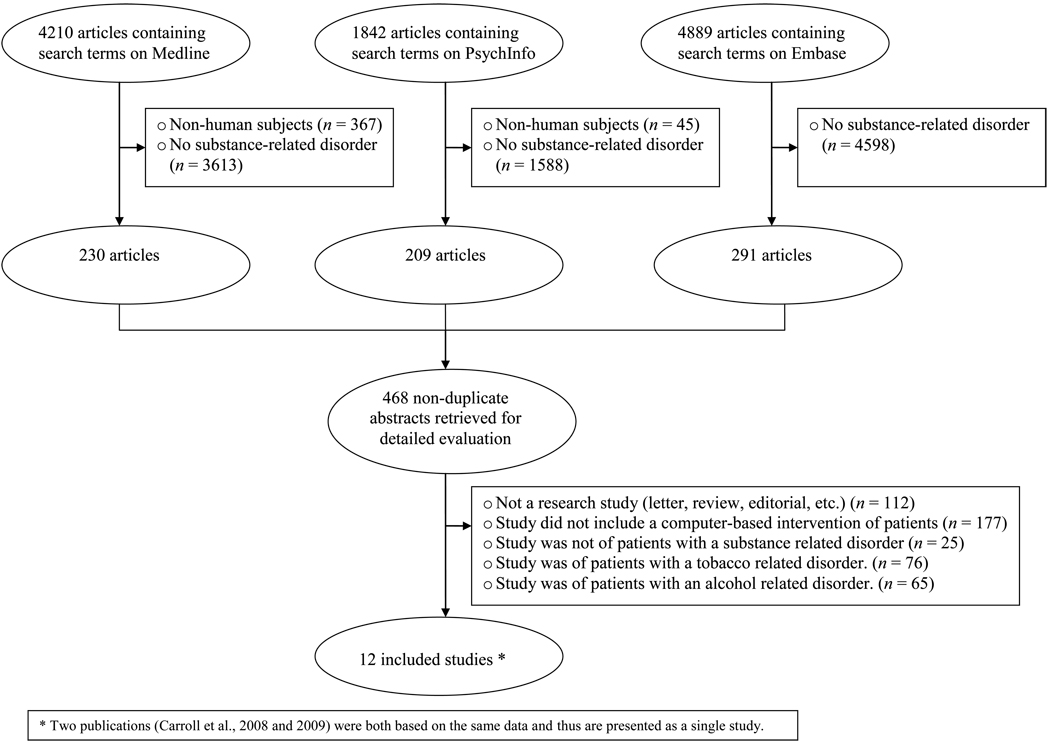
A total of 468 unique abstracts were identified by the literature search described above (230 from MEDLINE, 209 from PsychINFO, and 291 from EMBASE). Of these 18 were initially categorized for possible inclusion, 439 for exclusion and 11 were re-evaluated by all authors due to discrepancies, of which 7 were categorized for possible inclusion, leading to a total of 25 articles being initially considered for possible inclusion. The level of agreement for studies excluded after the initial title and abstract review was substantial, kappa = 0.75.
Of the 25 articles categorized for possible inclusion, 11 were initially categorized for inclusion, 6 for exclusion and 7 were re-evaluated by all authors due to discrepancies, of which 1 was categorized for inclusion. The level of agreement for studies excluded at this stage was moderate, kappa = 0.56. A summary of the search and reasons for exclusion are detailed in Figure 1.
Figure 1.
Flowchart of the process of selecting studies designed to evaluate computer-based interventions for drug abuse.
Study Characteristics
Summary of Findings
Study characteristics (samples, treatment, and outcomes) are provided in Tables 2–4. Sample sizes of the studies ranged from 19 to 909 (mean = 163, median = 102). Consistent with national data about treatment admissions for substance-related disorders, participants in the studies selected for this systematic review were generally in their 20s to early 30s, included men and women, and were comprised of individuals from different racial/ethnic groups, with the majority being white and male (SAMHSA - Office of Applied Studies, 2009). Participants in two studies were postpartum women (Ondersma, Chase, Svikis, & Schuster, 2005; Ondersma, Svikis, & Schuster, 2007), those in 3 studies were predominantly male (Grohman & Fals-Stewart, 2003; Grohman, Fals-Stewart, & Donnelly, 2006), and subjects in the remaining 7 studies were male and female. Drug of abuse also varied across the studies. Four studies evaluated opioid users exclusively (Barber, 1990; Bickel, Marsch, Buchhalter, & Badger, 2008; Chopra et al., 2009; Marsch & Bickel, 2004) while the other studies included more than one type of drug user (5 cocaine, 8 cannabis, 6 alcohol and 5 other). Two included studies were conducted in the Australia (Barber, 1990; Kay-Lambkin, Baker, Lewin, & Carr, 2008) and the rest in the United States.
Table 2.
Subject Characteristics for Studies Designed to Evaluate Computer-Based Interventions for Drug Use
| Author (year) | Population | N | Age (mean± SD, years) |
Sex (% male) |
Race/ethnicity | Drug |
|---|---|---|---|---|---|---|
| Barber (1990) | Inmates in drug treatment units in Melbourne, Australia | 30 | NPa | NPa (male and female) | NPa | Opioids |
| Bickel et al. (2008) | Substance abuse treatment seeking, already in substance abuse treatment | 135 | 28.6±8.3 | 56% | 96% white | Opioids |
| Carroll et al. (2008, 2009) | Outpatient substance abuse treatment seeking | 77 | 41.6±10.2 | 57 | 34% white | 69% cocaine |
| 46% AAb | 16% opioids | |||||
| 12% Hispanic | 18% alcohol | |||||
| 6% Native American | 7% cannabis | |||||
| Chopra et al. (2009) | Outpatient substance abuse treatment seeking | 127 | 32± 11.1 | 58 | 98% white | Opioids |
| Grohman & Fals-Stewart (2003) | Residential substance abuse treatment seeking | 120 | 32± 5.2 | 71 | 52% white | 65% cocaine |
| 32% AAb | 60% alcohol | |||||
| 13% Hispanic | 29% opiate | |||||
| 3% other | 17% cannabis | |||||
| 23% other | ||||||
| Grohman et al. (2006) | Veterans recently enrolled in treatment | 19 | 47 ± 5.2 | 89 | 39% white | 74% cannabis |
| 58% AAb | 68% alcohol | |||||
| 5% Hispanic | 58% cocaine | |||||
| 58% other | ||||||
| Hall & Huber (2000) | Already in substance abuse treatment | 909 | 32 ± 1.4 | 77 | 83% white | 85% alcohol |
| 59% cannabis | ||||||
| Kay-Lambkin et al. (2009) | Outpatient substance abuse treatment seeking | 97 | 35 (range 18–61) | 46 | 93% white | Alcohol or cannabis |
| Marsch & Bickel (2004) | Currently in substance abuse treatment | 30 | 36 ± 1.37 | 63 | 90% white | IVc opioid |
| 3% AAb | ||||||
| 7% Hispanic | ||||||
| Ondersma et al. (2005) | Postpartum women recruited from hospital’s obstetrics department | 30 | 23 ± 5.6 | 0 | 97% AAb | 37% cannabis |
| 27% cocaine, amphetamines, opiates, hallucinogens or inhalants | ||||||
| Ondersma et al. (2007) | Postpartum women recruited from hospital’s obstetrics department | 107 | 25 ± 5.6 | 0 | 97% AAb | Cannabis and other |
| Ruggiero et al. (2006) | Probability sample of adults in New York City following September 11th attacks | 285 | 42 ± 13.6 | 47 | 73% white | Any illicit drug |
| 9% Asian | ||||||
| 6% AAb | ||||||
| 9% Hispanic | ||||||
| 3% other |
Not provided
African American
Intravenous
Table 4.
Hierarchy of Treatment Outcomes for Studies Designed to Evaluate Computer-Based Interventions for Drug Use
| Studies Evaluating Drug Use Outcomes | ||||||
|---|---|---|---|---|---|---|
| Author (year) | Study quality |
Analysis types | Control group | Attrition rate | Primary outcome measures | Results |
| Bickel et al. (2008) | 21 | Intent to treat | TAUb and therapist-delivered CRAc | Computer CRAc - 62% |
|
|
| Therapist CRAc – 58% | ||||||
| Standard – 53% | ||||||
| Carroll et al. (2008, 2009) | 20 | Intent to treat, treatment exposed | TAUb | Experimental -33% |
|
|
| Control – 312% | ||||||
| 82% During post treatment follow up | ||||||
| Chopra et al. (2009)a | 19 | Intent to treat | TAUb | Voucher contingency-85% |
|
|
| Medication contingency- 60% | ||||||
| TAUb – 76% | ||||||
| Kay-Lambkin et al. (2009) | 20 | Intent to treat | Therapist delivered CBTf, Single brief intervention | Computer – 72% |
|
|
| Therapist – 66% | ||||||
| Single BIg – 70% | Self reported cannabis use | Greater reduction for computer and therapist than single BIg | ||||
| Ondersma et al. (2005) | 18 | Intent to treat | Assessment only | Experimental – 33% |
|
|
| Control – 20% | ||||||
| Ondersma et al. (2007) | 24 | Intent to treat, completers only | Assessment only | Experimental – 29% |
|
|
| Control – 29% | ||||||
| Barber (1990) | 6 | Intent to treat | TAUb | NPi |
|
|
| Grohman & Fals-Stewart (2003) | 18 | Intent to treat | TAUb and computer-assisted typing tutorial | Experimental – 62% |
|
|
| TAUb – 82% | ||||||
| Typing group – 82% | ||||||
| Grohman et al. (2006) | 13 | Intent to treat | TAUb | NPi |
|
|
| Hall & Huber (2000) | 11 | Intent to treat | TAUb, offsite case manager | NPi |
|
|
| Marsch & Bickel (2004) | 18 | Completers only | Counselor-facilitated instruction | 0 |
|
|
| Ruggiero et al. (2006) | 15 | Completers only | None | 50% |
|
|
Computer-delivered CRAc was confounded with contingency management (medication or voucher). Both conditions were compared to Standard care.
Treatment as usual
Community reinforcement approach
Medication contingency
Voucher contingency
Cognitive behavioral therapy
Brief intervention
Not provided
Characteristics of the computer-based interventions varied in presentation modality, length, number of sessions, and therapist involvement. All but 2 studies involved presentation of material via an on-site computer. One study evaluated a web-based system accessed via a home computer (Ruggiero et al., 2006), while another evaluated an interactive voice response (IVR) system accessed through a regular telephone (Hall & Huber, 2000). Four studies used single session or brief interventions (Barber, 1990; Ondersma et al., 2005; Ondersma et al., 2007; Ruggiero et al., 2006), and 1 used 3–5, 30 minute sessions over 1 week (Marsch & Bickel, 2004), based on motivational enhancement and/or psycho-education. With the exception of the IVR study, the remaining involved multiple sessions similar in frequency and length to traditional therapy sessions (6 to 69 sessions, 20–50 minutes in length) and were based on behavioral interventions of cognitive behavioral therapy (CBT: Carroll et al., 2008; Carroll et al., 2009; Kay-Lambkin et al., 2008), community reinforcement approach (CRA: Bickel et al., 2008; Chopra et al., 2009), or cognitive rehabilitation (Grohman & Fals-Stewart, 2003; Grohman et al., 2006). Therapists were involved in the computer-based treatment in 3 studies, although therapist time and frequency of contact were limited compared to TAU conditions (Bickel et al., 2008; Chopra et al., 2009; Kay-Lambkin et al., 2008). All but one study (Ruggiero et al., 2006) used a randomized design with a control group.
Hierarchy of Treatment Outcomes
Drug use outcomes were evaluated in 6 studies (see Table 4: Bickel et al., 2008; Carroll et al., 2008; Carroll et al., 2009; Chopra et al., 2009; Kay-Lambkin et al., 2008; Ondersma et al., 2005; Ondersma et al., 2007) with 4 including urinalysis data (Bickel et al., 2008; Carroll et al., 2008; Carroll et al., 2009; Chopra et al., 2009; Ondersma et al., 2007). Except for one brief intervention study (Ondersma et al., 2005), computer based treatment showed better drug use outcomes (both self-report and urinalysis) than treatment-as-usual (TAU). Reported or estimated effect sizes based on reported data for these primary outcomes during treatment were d = 1.11, .45, and .46, for self-reported drug use (Carroll et al., 2008, Kay-Lambkin et al., 2008, and Ondersma et al., 2007, respectively), and d = .36, .59, .36 for urinalysis data (Bickel et al., 2008; Carroll et al., 2008; Ondersma et al., 2007, respectively). Of five studies that evaluated treatment retention, three showed no differences (Bickel et al., 2008; Carroll et al., 2008; Chopra et al., 2009) and two showed improved retention compared to treatment-as-usual (Grohman & Fals-Stewart, 2003; Grohman et al., 2006). Three studies that also directly compared the same therapeutic content delivered either via computer or a therapist/counselor showed similar treatment response (Bickel et al., 2008; Kay-Lambkin et al., 2008; Marsch & Bickel, 2004). Lasting effects of treatment, examined by follow-up assessments after the end of the intervention were evaluated in 5 studies, with all 5 reporting better outcome for the computer-based intervention (Carroll et al., 2009; Grohman & Fals-Stewart, 2003; Kay-Lambkin et al., 2008; Marsch & Bickel, 2004; Ondersma et al., 2007).
Ratings of satisfaction with the computer-based system were evaluated in 5 studies, with two studies (Hall & Huber, 2000; Marsch & Bickel, 2004) reporting that the computer-based treatment was preferable to control conditions, and the other three (Carroll et al., 2008; Ondersma et al., 2005; Ruggiero et al., 2006) reporting high ratings of participant satisfaction.
Study Quality
Individual quality scores for each study are presented in Table 4. The quality of the articles varied from 6 to 24 with a mean of 16.9 (SD=4.9) and the inter-rater reliability was excellent (r =0.88).
Discussion
Computer-based interventions for drug use disorders show initial evidence of efficacy during treatment and some evidence that effects continue after treatment. Despite heterogeneity of samples, methods, and intervention types, studies evaluated showed improved self-reported and urinalysis outcomes for computer-based interventions compared to control conditions. In addition, computer-based interventions were associated with high levels of client satisfaction as measured by direct assessment, and participants exhibited similar levels of engagement and retention as those in therapist provided treatments. Despite the promising findings, research of computer-based treatments for drug use disorders is still clearly in its infancy, when publication bias may be stronger. Most studies were primarily prototype testing. Although a few randomized controlled trials with drug use outcomes and relevant controls have been published (Bickel et al., 2008; Carroll et al., 2008; Carroll et al., 2009; Chopra et al., 2009; Kay-Lambkin et al., 2008; Ondersma et al., 2007), these are still small scale efficacy trials, for which effect sizes are less stable. In particular, studies comparing content delivered via computer vs. therapist are inadequately powered to detect what may be clinically meaningful differences or to clearly establish that treatments are comparable.
Despite these limitations, the positive early findings clearly call for larger efficacy and effectiveness trials. In designing these larger scale efficacy trials, standardization is needed for outcome measures and control conditions. Such standardization would facilitate comparison across efficacy trials. For example, inclusion of biologically verified point prevalence follow-up measures would allow comparison across clinical trials and would provide clinically relevant data. Similarly, given variability in drug use profiles, measures such as days or weeks of abstinence would provide improved comparability across drugs of abuse than measures of reductions in quantity or frequency. Ideally, uniformity is needed in control conditions not only to provide a consistent standard of care across comparable studies, but to evaluate controls for time and attention. Treatment-as-usual controls are less ideal due to low fidelity and high variability both within and across studies. Additional studies that compare computer-based treatments to the same content delivered via therapist are needed to further evaluate comparability. However, these studies need to be sufficiently powered to provide confidence intervals to not only evaluate differences between conditions, but also to establish treatment equivalence within a clinically meaningful range. Finally, given the great potential for computer-based treatments to be cost effective, research evaluating the relative cost benefit and cost efficacy of computer-based and therapist-delivered interventions is needed.
Comparisons with reviews of computer-based treatments for tobacco and alcohol studies suggest that different types of systems have been emphasized for varying drugs of abuse. Most of the computer-based alcohol interventions have focused on brief interventions using assessment with personalized feedback. Many of the these studies have focused on at-risk populations such as college students (Elliott et al., 2008), who are not currently dependent or seeking treatment. For tobacco, there are many smoking cessation programs intended for extended use throughout abstinence (e.g., Stomp Out Smoking, Not on Tobacco, Clearing the Air, and Comprehensive Health Enhancement Support System for Smoking Cessation and Relapse Prevention; Myung et al., 2009). In the current review, most of the trials that included standard drug abuse outcomes involved longer intervention periods consistent with traditional drug abuse treatment. Although these variations in systems address the need for a range of interventions at different points in the drug use disorder trajectory, systematic reviews have generally compared all computer-based intervention equally (Carey et al., 2009; Elliott et al., 2008; Myung et al., 2009). Future reviews should address target population and length of intervention as well as other factors.
Despite variations in drug of abuse, stage of drug use disorder addressed, and outcome measures used, most studies to date have reported delivering the intervention via a computer on-site, rather than via internet, phone, or mobile access. Such alternative delivery options offer a number of advantages that deserve exploration. First, patients can use the systems in their own environment, perhaps even during cravings or other high-risk situations. Mobile phones are often taken everywhere and could be an easy access point for treatment-on-demand. Second, patients can learn the material at their own pace, repeating material as frequently as they wish, or move on quickly to new material, rather than waiting for access to an on-site computer. Finally, “outgoing” systems can contact individuals via email, text, or phone, rather than being limited to patient initiated contact. These type of interventions have been shown to be effective for other disorders requiring behavioral change such as diabetes (Cole-Lewis & Kershaw, 2010). Although they have not been evaluated for drug use disorders, electronic contact from businesses and other organizations is common practice and would likely not be out of the ordinary for users. Outgoing messages, combined with patient initiated contact may improve patient satisfaction, retention, and overall treatment response.
Based on the findings of the current review, computer-based interventions are a promising development for drug use disorders. They have the potential to dramatically expand and alter the landscape of treatment due to their low cost, consistent presentation, and easy accessibility and availability. By expanding treatment options and availability, such systems may make treatment more attractive for the large percentage of abusing and dependent individuals who do not seek treatment. Such systems may also be more easily implemented in a range of contexts including traditional treatment, brief intervention for at-risk populations, stepped-care management, and long-term re-engagement in settings such as primary-care.
In addition, a range of patient and provider level factors likely influence effective implementation of computer-based treatments. Familiarity with computers, provider acceptance and support, age, gender, and learning styles are only a few of the possible variables that may affect client acceptance of, preference for, and overall treatment response to computer-based treatments. Similarly, computers can collect a wealth of process information such as duration, patient choice, as well as response to directed items throughout any specific treatment episode. Additional exploration is needed on such factors to identify potential mechanisms of action and to provide more detailed evaluation of patient change.
Table 3.
Treatment Characteristics for Studies Designed to Evaluate Computer-Based Interventions for Drug Use
| Author (year) | Setting | Treatment delivery modality |
Length of intervention |
Number of sessions (length) |
Therapist involvement |
Experimental treatment description |
|---|---|---|---|---|---|---|
| Barber (1990) | Prison (drug treatment unit) | On-site computer | NPa | 1 (NPa) | No | Motivational, psycho-education |
| Bickel et al. (2008) | Outpatient research clinic | On-site computer | 23 weeks | 69 (20–30 minutes) | Yes | CRAb with contingency management |
| Carroll et al. (2008, 2009) | Outpatient substance abuse clinic | On-site computer | 8 weeks | 6 (45 minutes) | No | CBTc |
| Chopra et al. (2009) | Outpatient substance abuse clinic | On-site computer | 12 weeks | 36 (30 minutes) | Yes | CRAb with contingency management |
| Grohman & Fals-Stewart (2003) | Residential substance abuse treatment program | On-site computer | 2 months | 24 (50 minutes) | No | Cognitive rehabilitation |
| Grohman et al. (2006) | Outpatient substance abuse clinic (VAg) | On-site computer | 3/4 weeks | 10 (30 minutes) | Not specified | Cognitive rehabilitation |
| Hall & Huber (2000) | Outpatient substance abuse clinic | IVRe through telephone | NPa | NPa | Yes | Voice message system with psychoeducation component |
| Kay-Lambkin et al. (2009) | Outpatient substance abuse clinic | On-site computer | 3 months | 9 | Yes | CBTc and MEd |
| Marsch & Bickel (2004) | Research setting | On-site computer | 1 week | 3–5 (30 minutes) | No | Psycho-education |
| Ondersma et al. (2005) | Hospital | On-site computer | Single session | 1 (20 minutes) | No | Brief motivational enhancement |
| Ondersma et al. (2007) | Hospital | On-site tablet PCf | Single session | 1 (20 minutes) | No | Brief motivational enhancement |
| Ruggiero et al. (2006) | Unsupervised at home | Home computer | Unclear | 1 (1–30 minutes) | No | Brief motivational enhancement |
Not provided
Community reinforcement approach
Cognitive behavioral therapy
Motivational enhancement
Interactive voice response
Personal computer
Veterans Administration
Acknowledgements
The research was supported by the National Institute on Drug Abuse Grants K01 DA022398 (BM, TF, & BG) and K23 DA024050 (DB). This study was presented in part at the 70th annual scientific meeting of the College on Problems of Drug Dependence (June, 2009), Reno, NV.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barber JG. Computer-assisted drug prevention. Journal of Substance Abuse Treatment. 1990;7:125–131. doi: 10.1016/0740-5472(90)90008-e. [DOI] [PubMed] [Google Scholar]
- Bewick BM, Trusler K, Barkham M, Hill AJ, Cahill J, Mulhern B. The effectiveness of web-based interventions designed to decrease alcohol consumption--a systematic review. Preventive Medicine. 2008;47:17–26. doi: 10.1016/j.ypmed.2008.01.005. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA, Buchhalter AR, Badger GJ. Computerized behavior therapy for opioid-dependent outpatients: a randomized controlled trial. Experimental & Clinical Psychopharmacology. 2008;16:132–143. doi: 10.1037/1064-1297.16.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budman SH. Behavioral health care dot-com and beyond: Computer-mediated communications in mental health and substance abuse treatment. American Psychologist. 2000;55:1290–1300. [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Elliott JC, Bolles JR, Carey MP. Computer-delivered interventions to reduce college student drinking: A meta-analysis. Addiction. 2009;104:1807–1819. doi: 10.1111/j.1360-0443.2009.02691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Nuro KF, et al. Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT. American Journal of Psychiatry. 2008;165:881–888. doi: 10.1176/appi.ajp.2008.07111835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Rounsaville BJ. Enduring effects of a computer-assisted training program for cognitive behavioral therapy: A 6-month follow-up of CBT4CBT. Drug & Alcohol Dependence. 2009;100:178–181. doi: 10.1016/j.drugalcdep.2008.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ. A vision of the next generation of behavioral therapies research in the addictions. Addiction. 2007;102:850–862. doi: 10.1111/j.1360-0443.2007.01798.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanagh K, Shapiro DA. Computer treatment for common mental health problems. Journal of Clinical Psychology. 2004;60:239–251. doi: 10.1002/jclp.10261. [DOI] [PubMed] [Google Scholar]
- Chopra MP, Landes RD, Gatchalian KM, Jackson LC, Buchhalter AR, Stitzer ML, et al. Buprenorphine medication versus voucher contingencies in promoting abstinence from opioids and cocaine. Experimental and Clinical Psychopharmacology. 2009;17:226–236. doi: 10.1037/a0016597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiologic Reviews. 2010;32:56–69. doi: 10.1093/epirev/mxq004. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connors GJ, Tonnigan JS, Miller WR. A Longitudinal model of intake symptomatology, AA participation and outcome: Retrospective study of the Project MATCH outpatient and aftercare samples. Journal of Studies on Alcohol. 2001;62:817–825. doi: 10.15288/jsa.2001.62.817. [DOI] [PubMed] [Google Scholar]
- Copeland J, Martin G. Web-based interventions for substance use disorders: A qualitative review. Journal of Substance Abuse Treatment. 2004;26:109–116. doi: 10.1016/S0740-5472(03)00165-X. [DOI] [PubMed] [Google Scholar]
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott JC, Carey KB, Bolles JR. Computer-based interventions for college drinking: A qualitative review. Addictive Behaviors. 2008;33:994–1005. doi: 10.1016/j.addbeh.2008.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grohman K, Fals-Stewart W. Computer-assisted cognitive rehabilitation with substance-abusing patients: Effects on treatment response. Journal of Cognitive Rehabilitation. 2003;21:10–17. [Google Scholar]
- Grohman K, Fals-Stewart W, Donnelly K. Improving treatment response of cognitively impaired veterans with neuropsychological rehabilitation. Brain & Cognition. 2006;60:203–204. [PubMed] [Google Scholar]
- Hall JA, Huber DL. Telephone management in substance abuse treatment. Telemedicine Journal and e-Health. 2000;6:401–407. doi: 10.1089/15305620050503870. [DOI] [PubMed] [Google Scholar]
- Kaltenthaler E, Parry G, Beverley C, Ferriter M. Computerised cognitive-behavioural therapy for depression: Systematic review. British Journal of Psychiatry. 2008;193:181–184. doi: 10.1192/bjp.bp.106.025981. [DOI] [PubMed] [Google Scholar]
- Kay-Lambkin FJ, Baker AL, Lewin TJ, Carr VJ. Technology and innovation in the psychosocial treatment of methamphetamine use, risk and dependence. Drug & Alcohol Review. 2008;27:318–325. doi: 10.1080/09595230801914768. [DOI] [PubMed] [Google Scholar]
- Marks I, Shaw S, Parkin R. Computer-aided treatments of mental health problems. Clinical Psychology: Science and Practice. 1998;5:151–170. [Google Scholar]
- Marsch LA, Bickel WK. Efficacy of computer-based HIV/AIDS education for injection drug users. American Journal of Health Behavior. 2004;28:316–327. doi: 10.5993/ajhb.28.4.3. [DOI] [PubMed] [Google Scholar]
- Marsch LA, Bickel WK, Grabinski MJ. Application of interactive, computer technology to adolescent substance abuse prevention and treatment. Adolescent Medicine. 2007;18:342–356. [PubMed] [Google Scholar]
- Montani S, Bellazzi R, Quaglini S, d'Annunzio G. Meta-analysis of the effect of the use of computer-based systems on the metabolic control of patients with diabetes mellitus. Diabetes Technology & Therapeutics. 2001;3:347–356. doi: 10.1089/15209150152607123. [DOI] [PubMed] [Google Scholar]
- Myung S-K, McDonnell DD, Kazinets G, Seo HG, Moskowitz JM. Effects of web- and computer-based smoking cessation programs: Meta-analysis of randomized controlled trials. Archives of Internal Medicine. 2009;169:929–937. doi: 10.1001/archinternmed.2009.109. [DOI] [PubMed] [Google Scholar]
- Nadelson T. The inhuman computer/the too-human psychotherapist. American Journal of Psychotherapy. 1987;41:489–498. doi: 10.1176/appi.psychotherapy.1987.41.4.489. [DOI] [PubMed] [Google Scholar]
- Noar SM, Black HG, Pierce LB. Efficacy of computer technology-based HIV prevention interventions: A meta-analysis. Aids. 2009;23:107–115. doi: 10.1097/QAD.0b013e32831c5500. [DOI] [PubMed] [Google Scholar]
- Ondersma SJ, Chase SK, Svikis DS, Schuster CR. Computer-based brief motivational intervention for perinatal drug use. Journal of Substance Abuse Treatment. 2005;28:305–312. doi: 10.1016/j.jsat.2005.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma SJ, Svikis DS, Schuster CR. Computer-based brief intervention a randomized trial with postpartum women. American Journal of Preventive Medicine. 2007;32:231–238. doi: 10.1016/j.amepre.2006.11.003. [erratum appears in American Journal of Preventive Medicine (2007), 32, 549] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portnoy DB, Scott-Sheldon LAJ, Johnson BT, Carey MP. Computer-delivered interventions for health promotion and behavioral risk reduction: a meta-analysis of 75 randomized controlled trials, 1988–2007. Preventive Medicine. 2008;47:3–16. doi: 10.1016/j.ypmed.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reger MA, Gahm GA. A meta-analysis of the effects of internet- and computer-based cognitive-behavioral treatments for anxiety. Journal of Clinical Psychology. 2009;65:53–75. doi: 10.1002/jclp.20536. [DOI] [PubMed] [Google Scholar]
- Ruggiero KJ, Resnick HS, Acierno R, Coffey SF, Carpenter MJ, Ruscio AM, et al. Internet-based intervention for mental health and substance use problems in disaster-affected populations: A pilot feasibility study. Behavior Therapy. 2006;37:190–205. doi: 10.1016/j.beth.2005.12.001. [DOI] [PubMed] [Google Scholar]
- SAMHSA - Office of Applied Studies. Treatment Episode Data Set (TEDS) Highlights -- 2007 National Admissions to Substance Abuse Treatment Services. Rockville, MD: 2009. (Vol. HHS Publication No. (SMA) 09-4360) [Google Scholar]
- Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: A meta-analysis. Psychological Medicine. 2007;37:319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- Ybarra ML, Bull SS. Current trends in Internet- and cell phone-based HIV prevention and intervention programs. Current HIV/AIDS Reports. 2007;4:201–207. doi: 10.1007/s11904-007-0029-2. [DOI] [PubMed] [Google Scholar]