Abstract
Introduction
Gastroesophageal reflux disease (GERD) is a common condition that impacts patients’ health-related quality of life (HRQoL). The HRQoL of Barrett’s esophagus (BE) has been less well studied. Furthermore, it is unknown to what extent BE patients suffer from psychological distress as a result of carrying a diagnosis of a premalignant condition. We sought to compare BE and GERD (stratified by erosive (ERD) and non-erosive reflux disease (NERD)) with regards to HRQoL and psychological impact.
Methods
In this single-center study of subjects presenting for elective upper endoscopy, consecutive patients with BE and GERD were enrolled. Participants completed questionnaires assessing generic HRQoL (Medical Outcomes Study Short Form-36: SF-36), disease-specific HRQoL (Gastrointestinal Quality of Life Index: GIQLI), a measure of psychological distress (the Revised Hopkins Symptom Checklist: SCL-90R) and a patient-centered assessment of impact of disease severity (the GERD health-related quality of life measure: GERD HRQL).
Results
Patients with BE had the lowest symptom severity compared to those with NERD or ERD (GERD HRQL: 13.7 vs. 18 and 15.9 respectively, p<0.01). Those with BE also had better disease-specific quality of life compared to NERD or ERD patients (GIQLI: 137.2 vs. 124.3 and 131.0 respectively, p<0.001). After adjusting for potential confounding variables including symptom severity and gender, BE patients continued to demonstrate better disease-specific HRQoL, scoring 12.2 points higher on the GIQLI than NERD patients (95% CI 5.1 – 19.3) and 16.3 points higher than ERD patients (95% CI 5.4 – 27.3), as well as better generic HRQoL, scoring 4.8 points higher on the SF-36 physical component summary than NERD patients (95% CI 0.8 – 8.8) and 7.1 points higher than ERD patients (95% CI 1.2–13.1). There were no significant differences between groups in psychological distress, as demonstrated by the SCL-90R global severity index, though BE patients scored lower on the somatization domain compared to NERD and ERD patients. When stratified by gender, females with NERD and BE had worse disease-specific HRQoL than males.
Conclusions
Patients with BE have better generic and disease-specific HRQoL when compared to patients with NERD and ERD. This difference is only partially attributable to lower symptom severity amongst BE patients. Psychological distress did not differ significantly amongst groups. Female gender was associated with worsened HRQoL regardless of GERD disease manifestation. Though more precise instruments may aid in detecting any HRQoL decrements in BE patients due to perceived cancer risk or fear of developing or dying from cancer, we were unable to demonstrate an additional decrement in HRQoL due to cancer risk in subjects with BE.
Keywords: Barrett esophagus, Gastroesophageal reflux, Erosive esophagitis, Non-erosive esophagitis, Quality of Life, Gender
INTRODUCTION
Gastroesophageal reflux disease (GERD) is a common chronic disease, affecting 10–20% of the American population on a regular basis (1). Symptoms associated with GERD include heartburn, acid regurgitation, and chest pain as well as “extra-esophageal” manifestations such as chest pain, nausea, chronic cough, asthma and hoarseness. All of these symptoms may compromise health-related quality of life (HRQoL). In addition, sleep disturbance and associated daytime sleepiness, decrease in mealtime enjoyment, and increased medication costs may contribute to the burden of disease.
Barrett’s esophagus (BE) is a metaplastic change associated with GERD in which the normal squamous esophageal epithelium transforms into intestinal cells after chronic acidic insult from reflux. Population studies demonstrate a prevalence of BE between 1–2% (2, 3), but in patients with GERD symptoms, the prevalence of BE ranges from 10 – 18% (2, 4). Barrett’s esophagus is associated with a 30–125-fold increased risk of adenocarcinoma compared to the general population (5, 6). While the relative risk of adenocarcinoma in patients with BE is quite high, their absolute risk remains low, approximately 0.5% per patient per year (5). Furthermore, cohort studies have generally not shown a decreased life-expectancy in BE (7, 8). Nonetheless, patients with BE may overestimate their individual cancer risk (9), which could affect HRQoL and lead to deleterious psychological effects.
The negative impact of GERD alone on HRQoL and daily function has been examined in numerous studies (10–12). A smaller number of studies have investigated HRQoL in BE patients, documenting a similar decrement to that seen in GERD patients (13, 14). Theoretically, persons with GERD and BE are at risk for both the HRQoL decrease attributable to reflux symptoms (i.e. that seen in GERD), as well the psychological burden of carrying the diagnosis of a pre-cancerous lesion. However, it is unknown to what extent GERD symptoms are responsible for the decreased HRQoL observed in BE, as opposed to the contribution of the threat of cancer. Moreover, there are two different manifestations of GERD: erosive reflux disease (ERD) and non-erosive reflux disease (NERD) (15). Although their histological manifestation is less severe, NERD patients have been demonstrated to have severe impairment in HRQoL (16). Non-erosive patients may have a psychological profile similar to patients with functional bowel disease, who often have increased psychological distress (17).
We performed a cross-sectional analysis of data from a case-control study of BE and GERD patients to examine whether patients with BE have different HRQoL than patients with ERD and NERD, after controlling for patient perception of GERD symptom severity. The aims of this study were to isolate any decrease in HRQoL associated with Barrett’s esophagus by comparing BE patients to GERD patients with similar GERD symptom severity, and to measure any additional psychological distress that may be associated with BE, which could potentially be attributed to cancer risk. Additionally, we sought do determine whether any differences were present in quality of life based on gender and presence of erosive disease.
METHODS
Study Subjects
The original study population was recruited over a 4-year period (2002–2006) from consecutive patients aged 18–80 presenting for elective upper endoscopy at the Gastroenterology Endoscopy Clinic at the University of North Carolina with a primary or secondary indication of reflux symptoms. Cases had both endoscopically and histologically confirmed prevalent BE. All potential cases were solicited for enrollment. Controls were patients without BE but with classic GERD symptoms, consisting of substernal chest burning, regurgitation and/or waterbrash syndrome, with a physician diagnosis of GERD. The control group was stratified based on the presence or absence of erosive disease as verified by esophagitis or erosions visualized on same-day endoscopy. Because GERD patients outnumber BE patients by an estimated 9:1 ratio (4), one fourth of eligible controls were randomly selected using a computer algorithm. An approximately 1:2 case to control ratio was used to improve study power.
Patients were excluded if they could not read or comprehend the informed consent or questionnaires or did not speak English, had undergone prior partial or complete esophageal resection, had undergone endoscopic ablation of their BE, or were found to have esophageal carcinoma on the index endoscopy. The research protocol was reviewed and approved by the Institutional Review Board of the University of North Carolina.
Study Measures
Medical Outcomes Study Short Form-36 (SF-36)
The SF-36 measures generic HRQoL, which allows comparisons between different disease states. The SF-36 measures health status in eight domains: physical functioning (PF), role limitations-physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role limitations-emotional (RE), and mental health (MH). Summary physical component (PCS) and mental component scores (MCS) are also calculated from patient responses (18).
Scores on the SF-36 range from 0–100 on each dimension and on the summary scales, with higher scores indicating better quality of life. The score is standardized in the general population with a mean of 50 and a standard deviation of 10. The scale reliability ranges from 0.78 to 0.93(18). The SF-36 takes relatively little time to complete and has been validated across many populations. Data are available on patients with a wide range of conditions such as angina, clinical depression, congestive heart failure, diabetes and hypertension (19). A 3-point difference on the summary scores is considered clinically meaningful in GERD (12).
Gastrointestinal Quality of Life Index (GIQLI)
The GIQLI is a system-specific measure that has been used in multiple gastrointestinal disease states including GERD (20). It assesses HRQoL in 4 domains: physical well-being, gastrointestinal symptoms, social well-being, and emotional well-being. The GIQLI is composed of 36 multiple-choice questions graded on a 0–4 scale; the final score is the sum of the question responses. Higher scores indicate less severe symptoms and improved HRQoL, and the maximum score is 144.
The Revised Hopkins Symptom Checklist 90 (SCL-90-R)
The SCL-90-R is a widely used measure of psychological distress. This instrument contains 90 questions addressing 9 dimensions of symptoms: somatization (SOM), obsessive-compulsive (OC), interpersonal sensitivity (IS), depression (DEP), anxiety (ANX), hostility (HOS), phobic anxiety (PHOB), paranoid ideation (PAR) and psychosis (PSY) (21). There are also 3 summary measures including a global severity index (GSI), a positive symptom distress index (PSDI) and a positive symptom total (PST). The questions are multiple-choice and graded on a 0–4 scale, with higher scores indicating more distress.
On each scale of the SCL-90-R, results are expressed as t scores with a population mean of 50 and a standard deviation of 10. General population norms are available for comparison with study population scores. A t score at or above the 90th percentile indicates a high level of general psychological distress (22). The SCL-90-R has previously been used to examine psychological distress in GERD patients but not in BE patients.
The Gastroesophageal Reflux Disease-Health Related Quality of Life Questionnaire (GERD-HRQL)
The GERD-HRQL was designed to measure patient perception of severity of symptoms of GERD. It is a 10-question instrument that examines the intensity and frequency of heartburn, difficulty swallowing, bloating, and the burden of GERD medication. Answers are graded from 1–5, with a maximum total score of 50 (23). Higher scores correspond to more severe symptoms and worsened HRQoL. The GERD-HRQL has been found to be reliable and valid in a wide range of patient groups. We used this measure to control for patient-centered assessment of GERD symptom severity in our analysis.
Study Outcomes
The primary outcomes of this study were quality of life and psychological distress, as measured with a generic quality of life instrument (SF-36), a disease-specific instrument (GIQLI), and a measure of psychological symptoms (SCL-90-R). We used the 10-item measure of GERD symptom severity, the GERD-HRQL, to control for the effect of GERD symptomatology on HRQoL. Results were stratified by disease manifestation (BE vs. NERD vs. ERD).
Statistical Analysis
This study was designed with >90% power to calculate a 10% difference in SF-36 summary scores with an alpha of 0.01.
Univariate statistics were used to examine means, standard deviations and shapes of distributions for continuous variables and frequencies for categorical variables. Missing or extreme values were identified and corrected as necessary; no data were imputed. Study participant test scores were eliminated if all questions on a test were answered with the same answer choice. For bivariate analysis, outcome measures were examined using t-tests for variables with two categories and one-way ANOVA for variables with more than two categories.
Multiple linear regression was used to determine the relationship between GERD manifestation and HRQoL outcomes while controlling for potential confounding factors (age, gender, race, BMI, current alcohol use, current smoking, current use of an antireflux medication, comorbidity, and prior mental health diagnosis) and patient perception of GERD severity. Subjects with missing data on relevant variables were excluded from the multivariable analyses. Because gender has previously been associated with differences in quality of life (24), our analysis was repeated after stratification by gender.
RESULTS
Participant characteristics
A total of 529 patients met entry criteria and were enrolled in the study. The characteristics of the study population are shown in Table 1. Patients with BE were older, more commonly male and Caucasian, and more likely to have had anti-reflux surgery as compared to the GERD patients. The non-erosive patients were more likely to be female as compared to the ERD and BE patients (64% female vs. 42% female and 33% female, respectively). Alcohol and tobacco use were most common in the ERD group. There was little difference between groups with respect to body mass index, current pharmacologic treatment of GERD (e.g. with proton pump inhibitor or H2 blocker medication), comorbidities, or prior mental health diagnosis.
Table 1.
Characteristics of the study population (n = 529)*
| GERD |
Barrett’s Esophagus (n = 168) | p** | ||
|---|---|---|---|---|
| Non-erosive (n = 289) | Erosive (n = 72) | |||
| Age (mean years ± SD) | 49.6 ± 13.5 | 50.3 ± 14.7 | 57.6 ± 11.5 | < 0.001 |
| Unknown (n) | 0 | 0 | 1 | |
| Gender | ||||
| Male (n, %) | 105 (36) | 42 (58) | 112 (67) | < 0.001 |
| Female (n, %) | 184 (64) | 30 (42) | 56 (33) | |
| Unknown (n) | 0 | 0 | 0 | |
| Race | ||||
| White (n, %) | 242 (84) | 63 (87) | 159 (95) | <0.01 |
| Non-white (n, %) | 47 (16) | 9 (13) | 9 (5) | |
| Unknown (n) | 0 | 0 | 0 | |
| BMI (mean kg/m2 ± SD) | 28.8 ± 6.9 | 27.8 ± 5.2 | 28.6 ± 5.5 | 0.5 |
| Unknown (n) | 24 | 15 | 8 | |
| Current alcohol use | ||||
| Yes (n, %) | 122 (51) | 33 (70) | 56 (48) | 0.03 |
| No (n, %) | 119 (49) | 14 (30) | 60 (52) | |
| Unknown (n) | 48 | 25 | 52 | |
| Current smoking | ||||
| Yes (n, %) | 39 (16) | 12 (27) | 25 (20) | 0.2 |
| No (n, %) | 199 (84) | 33 (74) | 100 (80) | |
| Unknown (n) | 51 | 27 | 43 | |
| Current medical GERD treatment | ||||
| Yes (n, %) | 251 (94) | 59 (95) | 152 (94) | 0.9 |
| No (n, %) | 16 (6) | 3 (5) | 10 (6) | |
| Unknown (n) | 22 | 10 | 6 | |
| Previous GERD surgery | ||||
| Yes (n, %) | 18 (10) | 4 (10) | 21 (21) | 0.02 |
| No (n, %) | 166 (90) | 38 (90) | 79 (79) | |
| Unknown (n) | 105 | 30 | 68 | |
| Comorbid conditions present | ||||
| Yes (n, %) | 227 (85) | 47 (76) | 132 (81) | 0.20 |
| No (n, %) | 40 (15) | 15 (24) | 30 (19) | |
| Unknown (n) | 22 | 10 | 6 | |
| Prior mental health diagnosis | ||||
| Yes (n, %) | 121 (45) | 22 (35) | 72 (44) | 0.4 |
| No (n, %) | 146 (55) | 40 (65) | 90 (56) | |
| Unknown (n) | 22 | 10 | 6 | |
Current alcohol defined as any current alcohol use. Current smoking defined as any current cigarette use. Erosive esophagitis defined as erosive disease seen on endoscopy. Medical GERD treatment defined as pharmaceutical treatment for GERD symptoms. GERD surgery defined as previous surgery for GERD symptoms. Comorbidity defined as any additional non-psychiatric chronic medical condition. Mental health diagnosis defined as any current or past psychiatric diagnosis.
p<0.05 by ANOVA for continuous variables and chi-square for categorical variables; missing data was not included in the statistical analysis.
Outcome measures
Response rates
The GERD HRQL questionnaire was completed by 395/529 participants (74.7%), the SF-36 was completed by 374/529 (70.7%), the GIQLI was completed by 365/529 (69.0%), and the SCL-90R was completed by 391/529 (73.9%). Response rates did not differ between cases and controls.
Generic quality of life
Unadjusted results of the SF-36 summary scores stratified by disease manifestation are shown in Table 2. There was a significant difference between groups with respect to the mental component score (MCS), with BE patients scoring on average 3 points higher than NERD or ERD patients (51.7 vs. 48.3 and 48.5 respectively, p= 0.02 for comparison). While there was a slight improvement in the physical component score (PCS) in BE patients compared to controls, this was not statistically significant (p=0.46).
Table 2.
Overall relationship between quality of life and psychological distress by disease manifestation
| Measure (mean ± SD) | GERD |
Barrett’s Esophagus (n = 168) | p* | |
|---|---|---|---|---|
| Non-erosive (n = 289) | Erosive (n = 72) | |||
| GERD-HRQL † | 18.0 ± 11.2 | 15.9 ± 10.8 | 13.7 ± 10.5 | < 0.01 |
| Unknown (n) | 72 | 17 | 45 | |
| SF-36 PCS# | 40.0 ± 12.7 | 40.1 ± 12.5 | 41.8 ± 12.7 | 0.5 |
| Unknown (n) | 94 | 12 | 49 | |
| SF-36 MCS** | 48.3 ± 11.0 | 48.5 ± 11.7 | 51.7 ± 10.9 | 0.02 |
| Unknown (n) | 94 | 12 | 49 | |
| GIQLI‡ | 124.3 ± 24.1 | 131.0 ± 20.8 | 137.2 ± 21.1 | < 0.001 |
| Unknown (n) | 97 | 15 | 52 | |
| SCL-90-R GSI†† | 58.0 ± 11.4 | 58.0 ± 12.2 | 56.4 ± 11.7 | 0.5 |
| Unknown (n) | 84 | 12 | 42 | |
p value calculated with ANOVA
GERD severity based upon 10-question GERD-HRQL. Higher scores indicate more severe symptomatology
SF-36 PCS = Physical component summary score from the Medical Outcomes Study Short-Form 36. Lower scores indicate lower quality of life.
SF-36 MCS = Mental component summary score from the Medical Outcomes Study Short-Form 36. Lower scores indicate lower quality of life.
GIQLI = Gastrointestinal Quality of Life Index. Lower scores indicate more severe symptoms.
SCL-90-R GSI = Global severity index (standardized T-score) of the Revised Hopkins Symptoms Checklist 90. A T score at or above the 90th percentile indicates a high level of psychological distress.
Multivariate analysis adjusting for potential confounding variables (including symptom severity) demonstrated a similar difference between BE patients and GERD patients with respect to the MCS, but it was no longer statistically significant (Table 3). There was a significant difference on the PCS in the adjusted model, however, with BE patients demonstrating a better physical component score than both NERD patients (difference of 4.8, 95% CI 0.8 – 8.8) and ERD patients (difference of 7.1, 95% CI 1.2–13.1).
Table 3.
Multivariable analysis of the relationship between quality of life and psychological distress and manifestation of reflux disease, controlling for severity of GERD symptoms*
| Adjusted measure (mean) | Non- erosive (n = 105) | Erosive (n = 42) | Barrett’s (n = 112) | Barrett’s vs Erosive |
Barrett’s vs Non-erosive |
||
|---|---|---|---|---|---|---|---|
| Difference | 95% CI | Difference | 95% CI | ||||
| SF-36 PCS‡ (n = 184) | 39.8 | 37.5 | 44.6 | 7.1 | 1.2, 13.1 | 4.8 | 0.8, 8.8 |
| SF-36 MCS# (n = 184) | 48.6 | 48.9 | 51.7 | 2.8 | −2.9, 8.4 | 3.1 | −0.7, 6.9 |
| GIQLI† (n = 183) | 125.5 | 121.4 | 137.7 | 16.3 | 5.4, 27.3 | 12.2 | 5.1, 19.3 |
| SCL-90-R GSI** (n = 190) | 57.5 | 57.2 | 55.3 | −1.9 | −7.3, 3.4 | −2.2 | −5.7, 1.2 |
Multiple linear regression used to calculate scores adjusted for age, gender, race, BMI, current alcohol use, current smoking, current use of an antireflux medication, comorbidity, and prior mental health diagnosis.
SF-36 PCS = Physical component summary score from the Medical Outcomes Study Short-Form 36. Lower scores indicate lower quality of life.
SF-36 MCS = Mental component summary score from the Medical Outcomes Study Short-Form 36. Lower scores indicate lower quality of life.
GIQLI = Gastrointestinal Quality of Life Index. Lower scores indicate more severe symptoms.
SCL-90-R GSI = Global severity index (standardized T-score) of the Revised Hopkins Symptoms Checklist 90. A T score at or above the 90th percentile indicates a high level of psychological distress.
Comparison of subdomain results of the SF-36 demonstrated significant differences between groups with respect to the bodily pain, vitality and role limitations-emotional subscales, with BE patients scoring higher than both NERD and ERD patients indicating better HRQoL in these categories. Patients with BE had better HRQoL in all other subscales of the SF-36 apart from physical functioning (role limitations-physical, general health, social functioning, and mental health) but these differences were not statistically significant (Figure 1).
Figure 1.
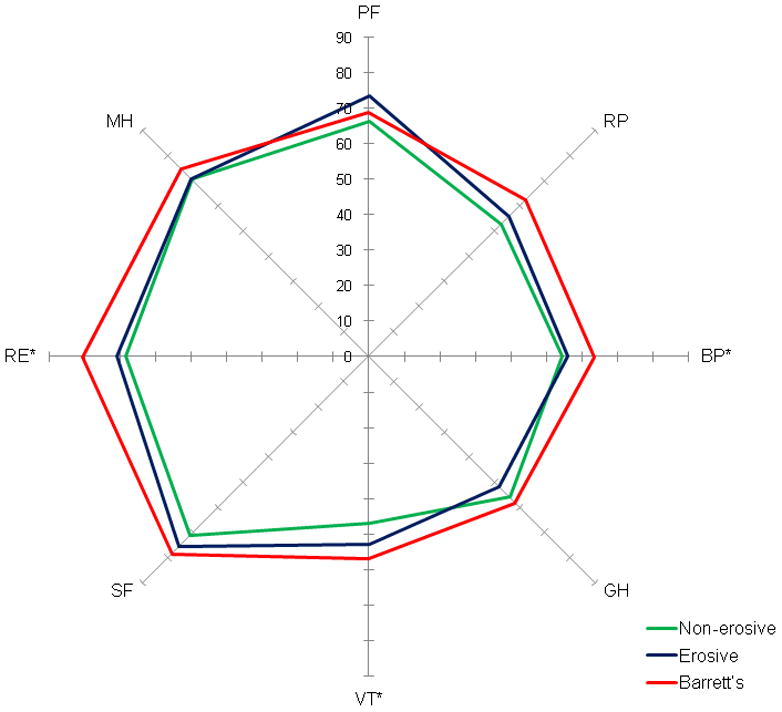
Radar graph of relationship between patients with Barrett’s esophagus, erosive esophagitis, and non-erosive reflux disease with respect to scores on the Medical Outcomes Study Short-Form-36 (SF-36) subscale scores. Lower scores (towards center of graph) indicate lower quality of life. Figure shows that Barrett’s esophagus patients scored better than GERD patients most subscales of the SF-36. Differences were statistically-significant for the bodily pain, vitality, and role-emotional subscales.
* p <0.05, calculated with ANOVA
PF = physical functioning, RP = role physical, BP = bodily pain, GH = general health, VT = vitality, SF = social functioning, RE = role emotional, MH = mental health.
Disease-specific quality of life
Unadjusted results from the GIQLI questionnaire in the 3 groups are shown in Table 2. There was a significant difference between groups with BE patients scoring higher on the GIQLI than ERD or NERD patients, indicating better disease-specific HRQoL (137.2 vs. 131.0 and 124.3 respectively, p <0.001). When adjusted for potential confounding variables, there remained a difference between the BE and GERD groups, with BE patients scoring 12.2 points higher on the GIQLI than NERD patients (95% CI 5.1 – 19.3) and 16.3 points higher than ERD patients (95% CI 5.4 – 27.3)(Table 3).
Psychological distress
We found no difference between groups with respect to the global severity index (GSI) of the SCL-90R in either the unadjusted comparison (Table 2) or the adjusted model (Table 3). Scores on the 9 dimensions and 3 summary measures of the scale are shown in Table 4. Among the psychological dimensions of the SCL-90R, there was a small, but significant difference between groups with respect to the somatization dimension, with BE patients scoring lower than ERD and NERD patients (58.3 vs. 59.7 and 57.4 respectively, p = 0.02). This indicates that BE patients may have less psychological distress related to somatization compared to GERD patients. However, given the lack of an overall difference in the GSI, multiple testing issues, and the relative instability of the dimension scores on the SCL-90R, these data must be viewed cautiously.
Table 4.
Relationship between psychologic distress (SCL-90-R) and manifestation of reflux disease
| Score* (mean ± SD) | GERD |
Barrett’s (n = 168) | |
|---|---|---|---|
| Non-erosive (n = 289) | Erosive (n = 72) | ||
| Global severity index | 58.0 ± 11.4 | 58.0 ± 12.2 | 56.4 ± 11.7 |
| Somatization† | 61.9 ± 11.3 | 59.7 ± 12.3 | 58.3 ± 11.6 |
| Obsessive-compulsive | 57.4 ± 11.9 | 57.9 ± 10.7 | 56.4 ± 11.7 |
| Interpersonal sensitivity | 54.5 ± 11.4 | 54.8 ± 12.0 | 53.0 ± 10.9 |
| Depression | 57.5 ± 11.1 | 57.2 ± 12.0 | 57.1 ± 12.2 |
| Anxiety | 55.2 ± 11.6 | 53.3 ± 11.6 | 53.2 ± 12.8 |
| Hostility | 53.2 ± 10.3 | 53.8 ± 10.8 | 52.7 ± 10.2 |
| Phobic anxiety | 51.9 ± 10.7 | 51.6 ± 9.3 | 51.7 ± 9.9 |
| Paranoid ideation | 50.8 ± 11.2 | 52.5 ± 11.2 | 50.6 ± 11.3 |
| Psychoticism | 55.9 ± 11.0 | 56.4 ± 10.2 | 54.7 ± 10.7 |
| Positive symptom distress index | 57.2 ± 9.9 | 56.9 ± 9.7 | 55.1 ± 10.4 |
| Positive symptom total | 56.8 ± 11.2 | 56.6 ± 12.0 | 55.2 ± 10.5 |
| Missing (n) | 84 | 12 | 42 |
Standardized T scores of the SCL-90-R (Revised Hopkins Symptoms Checklist 90). A T score at or above the 90th percentile indicates a high level of psychological distress.
p = 0.02 for the comparison of the overall score between non-erosive, erosive, and BE subjects. All other comparisons are not significant.
Role of symptom severity
Subjects with non-erosive disease were found to report worse patient assessment of GERD symptom severity than those with ERD or BE as measured by the GERD HRQL (18.0 vs. 15.9 and 13.7 respectively, p <0.01)(Table 2). When we controlled for patient perception of symptom severity by adding GERD-HRQL into the regression model, patients with BE continued to display significantly better disease-specific quality of life than NERD patients, as measured by the GIQLI (137.7 vs. 125.5, difference = 12.2, 95% CI = 5.1 – 19.3). In addition, BE patients demonstrated improved generic HRQoL as measured by the physical component summary measure of the SF-36, when compared with NERD patients (44.6 vs. 39.8, difference = 4.8, 95% CI = 0.8 – 8.8). The improved SF-36 summary score for BE patients represents a clinically meaningful difference, given that it is greater than 3.0. There were no significant differences between ERD and NERD patients on any of the HRQoL or psychological distress summary measures, nor were there differences between the BE and NERD patients in terms of psychological distress (as measured by the SCL-90R GSI) (Table 3).
Role of gender
After stratifying by gender, males with BE reported lower symptom severity than males with GERD. This trend was similar in females, but it did not reach statistical significance (Figure 2). Women reported significantly worse GI-specific quality of life in both the NERD and BE groups as compared to men in these groups (Supplementary Table, Figure 3). Both men and women with NERD still had worsened GIQLI scores compared to those of ERD and BE men and women. Men with ERD had higher SF-36 PCS scores than women with ERD, but otherwise, there were no significant differences between genders with respect to SF-36 summary scores, or SCL-90R GSI.
Figure 2.
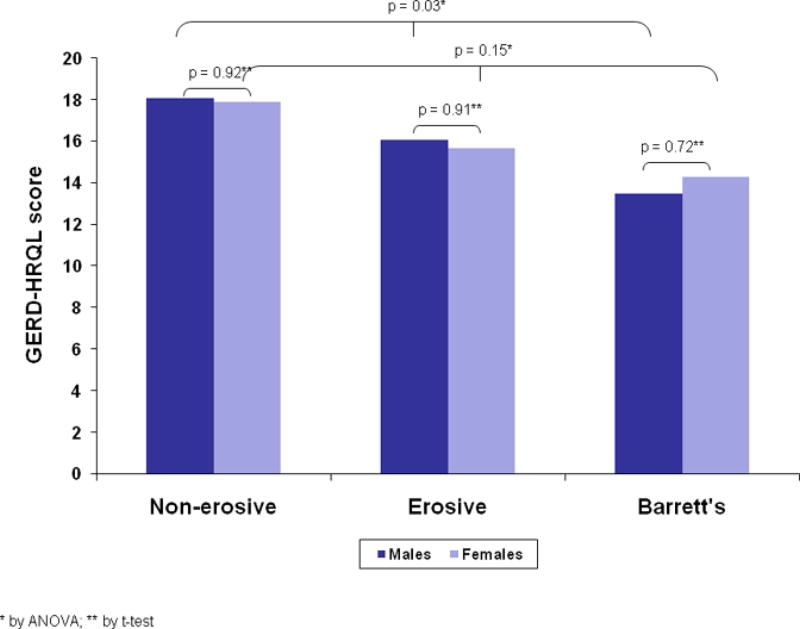
Symptom severity, as measured by the GERD-HRQL score by disease manifestation and gender.
Figure 3.
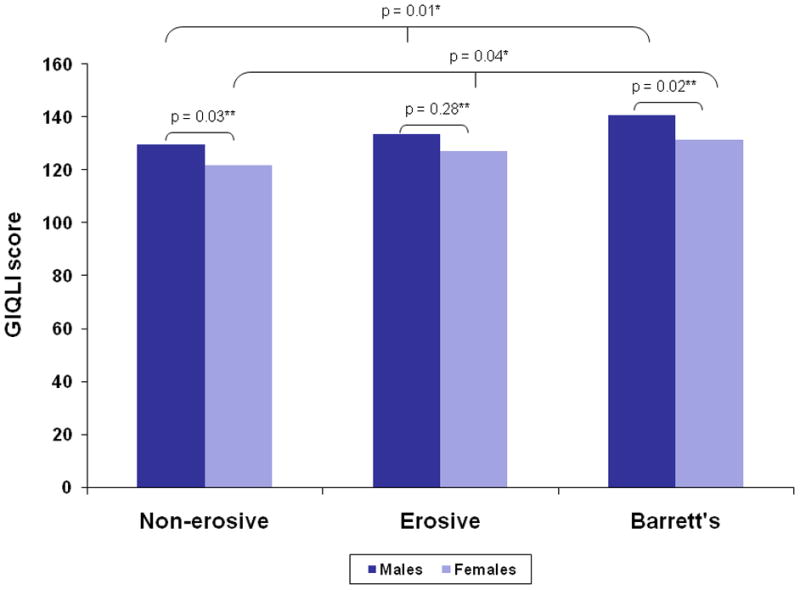
Gastrointestinal disease-specific quality of life (as measured by GIQLI), stratified by disease manifestation and gender.
*by oneway ANOVA, **by t-test
DISCUSSION
Our study showed there are differences in HRQoL based upon GERD manifestation. Patients with BE generally had better HRQoL than those with NERD or ERD. After adjusting for symptom severity, this difference was statistically-significant as measured by the GIQLI, and the SF-36 mental component summary. There were few differences between groups with respect to the SCL-90-R, apart from the finding that BE patients had somewhat less somatization than other groups.
When stratified by gender, both male and female NERD patients reported worse generic (SF-36) and disease-specific HRQoL (GIQLI) than ERD and BE patients of the same sex. Women had worse GI-specific quality of life than men in both the NERD and BE groups, and worse generic HRQoL in the ERD group. Because there were more women in the NERD group, it appears that the worsened HRQoL in the NERD group is partially confounded by gender. However, when we controlled for other variables including gender, the difference in HRQoL between NERD and ERD or BE patients remained statistically significant.
Overall, these findings suggest that the HRQoL decrement in BE is related to loss of function secondary to physical symptoms but not psychological distress. It is possible that patients with NERD may actually have functional esophageal disease with a prominent psychological component. The patients with NERD reported significantly worse HRQoL on almost all measures examined in this study. These findings can be attributed to perceiving symptoms as more severe and being more refractory to treatment. Because BE patients presumably had true acidic insults to their esophagus in the past in order to have undergone metaplasia, the NERD patients might be expected to have the best HRQoL as their disease manifestation would be the least severe; on the contrary, these subjects demonstrated the worst quality of life. Additionally, women in each of the groups were observed to have worse quality of life than men on most study measures. Improved HRQoL in BE patients may be due to fewer symptoms, as some authors have described (25). A recent population study estimated that up to 46% of BE patients may be asymptomatic (26). However, this observation persisted after we controlled for symptom severity. Therefore, we hypothesize that the trends reported here are due to a heightened sensitivity and symptom perception of patients with NERD.
As compared to the general population, patients with GERD and BE in this study report worse quality of life on every dimension of the SF-36, with scores that are comparable to patients with diabetes and clinical depression (18). Health related quality of life in BE patients has been assessed by other investigators. Kulig et. al reported SF-36 summary score results on 702 German patients with BE, 2660 ERD patients, and 2853 NERD patients (14). The reported PCS and MCS scores for BE patients were 42.6 and 46.2 respectively, similar to our findings of 41.8 and 51.7. Interestingly, results for NERD patients were higher for the PCS (43.5 vs. 40.0) and lower for the MCS (43.9 vs. 48.3) compared to our findings. Eloubedi et. al conducted a study of 107 patients with BE and 104 with GERD but without BE using the SF-36 and the Quality of Life in Reflux and Dyspepsia (QOLRAD) questionnaire (13). A measure of symptom severity was also used, but was not controlled for in a multivariate regression model comparing groups. The authors reported no significant differences between groups with respect to either HRQoL measure. Two studies have reported GIQLI scores on BE patients in the 94–96 range, but both were in the pre-operative setting prior to Nissen fundoplication. Therefore, patients would be expected to be suffering more severe symptoms than the average BE patient, which may explain the difference compared to our GIQLI mean of 137.2. One study that utilized the SCL-90 in GERD patients reported higher scores on dimensions of somatization, obsessiveness, interpersonal sensitivity, phobia, psychosis, and the global severity index compared to healthy controls (27, 28). While no studies have been done previously using the SCL-90R in BE patients, several studies have used the Hospital Anxiety and Depression scale (HADS) to evaluate psychological symptoms. A study of BE patients in an endoscopic surveillance program reported that BE patients had higher anxiety scores than the general population, but a second study demonstrated only minimal depression and anxiety for BE patients on the HADS (29, 30).
Our study has several strengths. We assessed a large number of patients with various manifestations of GERD. Previously validated tools were used to assess HRQoL and psychological stress. Importantly, we were able to control for several possible confounders including a patient assessment of GERD symptom severity, which has not been done in past investigations. GERD manifestation was assessed with same-day endoscopy, minimizing misclassification.
Several limitations can also be described. All patients in the study were presenting to a single tertiary care center and may not reflect the population of GERD patients treated in the community. Additionally, our study population was primarily white, which reflects the overall BE population but may limit the generalizability to patients of different races. Importantly, though the parent study was a case-control design, our study measured HRQoL and psychological distress at one point in time, so that temporality of HRQoL decrements in relationship to the time of diagnosis cannot be firmly established. Also, because we did not demand cessation of acid-suppressive medication prior to endoscopy, our NERD group was likely “contaminated” with treated erosive disease. It is important to note however, that if differential misclassification of ERD subjects into the NERD group occurred, the effect would tend to minimize, not accentuate, the differences in HRQoL we report between the NERD and ERD groups. Since pH testing was not a part of this study, the NERD group could also contain patients with typical GERD symptoms but without actual reflux (e.g. patients with functional heartburn). Nevertheless, such testing is uncommon for GERD patients in practice, and this group was representative of the typical NERD patients seen at our institution, contributing to the external validity of our results.
In addition, there are limitations due to the use of multiple HRQoL measurement tools. Because each participant was asked to fill out 4 different multi-item questionnaires, we did have missing data for each measure. Though response rates were similar between cases and controls, patients who completed the HRQoL assessments may still differ from those who did not do so. Also, because of the nature of the HRQoL measurements used and the preponderance of subscales for each measure (17 for the SF-36 and SCL-90R combined), some statistically significant differences between subscales may be a consequence of multiple testing. However, consistent trends amongst subscales favoring improved HRQoL on the SF-36 and less psychological distress SCL-90R for BE patients adds validity to the individual subscale differences. Furthermore, the finding that NERD patients have the most somatization is supported by prior studies, assuming that functional heartburn patients are included in this category (17). Nevertheless, because of multiple testing concerns, our a priori hypothesis testing focused on the summary measure comparisons, and we performed pairwise comparisons only if oneway ANOVA testing was significant. Therefore, our main findings in BE patients of reduced symptom severity, improved disease-specific HRQoL, and improved generic HRQoL as measured by SF-36 summary measures are minimally affected by multiple testing.
In summary, our study showed that patients with GERD have worse quality of life than patients with BE, even after controlling for GERD symptoms. When stratified, females have worse quality of life than males. In addition, patients with GERD symptoms and NERD have higher levels of psychological distress. Future studies are indicated to further examine the psychological component of NERD, and efforts should be directed at improving HRQoL in this disorder. Additionally, more precise instruments may aid in detecting any HRQoL decrements in BE patients due to perceived cancer risk or fear of developing or dying from cancer.
Supplementary Material
Acknowledgments
Financial support: This research was supported, in part, by grants from the National Institutes of Health K23 DK59311-01 (Dr. Shaheen), and T32 DK 07634 (Dr. Crockett).
Footnotes
Guarantor of the article: N. Shaheen
Specific author contributions: Dr. Crockett and Q. Lippmann drafted the manuscript. Dr. Dellon and Q. Lippmann performed the statistical analysis, data interpretation, and edited the manuscript. Dr. Shaheen designed and initiated the study, oversaw the data collection, performed data interpretation, and edited the manuscript. All authors approved the final manuscript.
Potential competing interests: None
References
- 1.Locke GR, 3rd, Talley NJ, Fett SL, et al. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–56. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 2.Csendes A, Smok G, Burdiles P, et al. Prevalence of Barrett’s esophagus by endoscopy and histologic studies: a prospective evaluation of 306 control subjects and 376 patients with symptoms of gastroesophageal reflux. Dis Esophagus. 2000;13:5–11. doi: 10.1046/j.1442-2050.2000.00065.x. [DOI] [PubMed] [Google Scholar]
- 3.Ronkainen J, Aro P, Storskrubb T, et al. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129:1825–31. doi: 10.1053/j.gastro.2005.08.053. [DOI] [PubMed] [Google Scholar]
- 4.Winters C, Jr, Spurling TJ, Chobanian SJ, et al. Barrett’s esophagus. A prevalent, occult complication of gastroesophageal reflux disease. Gastroenterology. 1987;92:118–24. [PubMed] [Google Scholar]
- 5.Drewitz DJ, Sampliner RE, Garewal HS. The incidence of adenocarcinoma in Barrett’s esophagus: a prospective study of 170 patients followed 4.8 years. Am J Gastroenterol. 1997;92:212–5. [PubMed] [Google Scholar]
- 6.O’Connor JB, Falk GW, Richter JE. The incidence of adenocarcinoma and dysplasia in Barrett’s esophagus: report on the Cleveland Clinic Barrett’s Esophagus Registry. Am J Gastroenterol. 1999;94:2037–42. doi: 10.1111/j.1572-0241.1999.01275.x. [DOI] [PubMed] [Google Scholar]
- 7.Anderson LA, Murray LJ, Murphy SJ, et al. Mortality in Barrett’s oesophagus: results from a population based study. Gut. 2003;52:1081–4. doi: 10.1136/gut.52.8.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eckardt VF, Kanzler G, Bernhard G. Life expectancy and cancer risk in patients with Barrett’s esophagus: a prospective controlled investigation. Am J Med. 2001;111:33–7. doi: 10.1016/s0002-9343(01)00745-8. [DOI] [PubMed] [Google Scholar]
- 9.Shaheen NJ, Green B, Medapalli RK, et al. The perception of cancer risk in patients with prevalent Barrett’s esophagus enrolled in an endoscopic surveillance program. Gastroenterology. 2005;129:429–36. doi: 10.1016/j.gastro.2005.05.055. [DOI] [PubMed] [Google Scholar]
- 10.El-Dika S, Guyatt GH, Armstrong D, et al. The impact of illness in patients with moderate to severe gastro-esophageal reflux disease. BMC Gastroenterol. 2005;5:23. doi: 10.1186/1471-230X-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaplan-Machlis B, Spiegler GE, Revicki DA. Health-related quality of life in primary care patients with gastroesophageal reflux disease. Ann Pharmacother. 1999;33:1032–6. doi: 10.1345/aph.18424. [DOI] [PubMed] [Google Scholar]
- 12.Revicki DA, Wood M, Maton PN, et al. The impact of gastroesophageal reflux disease on health-related quality of life. Am J Med. 1998;104:252–8. doi: 10.1016/s0002-9343(97)00354-9. [DOI] [PubMed] [Google Scholar]
- 13.Eloubeidi MA, Provenzale D. Health-related quality of life and severity of symptoms in patients with Barrett’s esophagus and gastroesophageal reflux disease patients without Barrett’s esophagus. Am J Gastroenterol. 2000;95:1881–7. doi: 10.1111/j.1572-0241.2000.02235.x. [DOI] [PubMed] [Google Scholar]
- 14.Kulig M, Leodolter A, Vieth M, et al. Quality of life in relation to symptoms in patients with gastro-oesophageal reflux disease-- an analysis based on the ProGERD initiative. Aliment Pharmacol Ther. 2003;18:767–76. doi: 10.1046/j.1365-2036.2003.01770.x. [DOI] [PubMed] [Google Scholar]
- 15.Orlando RC. Current understanding of the mechanisms of gastro-oesophageal reflux disease. Drugs. 2006;66(Suppl 1):1–5. doi: 10.2165/00003495-200666001-00002. discussion 29–33. [DOI] [PubMed] [Google Scholar]
- 16.Kovacs Z, Kerekgyarto O. Psychological factors, quality of life, and gastrointestinal symptoms in patients with erosive and non-erosive reflux disorder. Int J Psychiatry Med. 2007;37:139–50. doi: 10.2190/1147-44K4-MMQQ-122X. [DOI] [PubMed] [Google Scholar]
- 17.Shapiro M, Green C, Bautista JM, et al. Functional heartburn patients demonstrate traits of functional bowel disorder but lack a uniform increase of chemoreceptor sensitivity to acid. Am J Gastroenterol. 2006;101:1084–91. doi: 10.1111/j.1572-0241.2006.00525.x. [DOI] [PubMed] [Google Scholar]
- 18.Ware J, Kosinski M, Dewey J. How to Score Version 2 of the SF-36 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2000. [Google Scholar]
- 19.Tarlov AR, Ware JE, Jr, Greenfield S, et al. The Medical Outcomes Study. An application of methods for monitoring the results of medical care. JAMA. 1989;262:925–30. doi: 10.1001/jama.262.7.925. [DOI] [PubMed] [Google Scholar]
- 20.Eypasch E, Williams JI, Wood-Dauphinee S, et al. Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. Br J Surg. 1995;82:216–22. doi: 10.1002/bjs.1800820229. [DOI] [PubMed] [Google Scholar]
- 21.Derogatis LR, Rickels K, Rock AF. The SCL-90 and the MMPI: a step in the validation of a new self-report scale. Br J Psychiatry. 1976;128:280–9. doi: 10.1192/bjp.128.3.280. [DOI] [PubMed] [Google Scholar]
- 22.Derogatis LR. SCL-90-R: Administration, Scoring and Procedure Manual. Baltimore: Clinical Psychometrics Research; 1983. [Google Scholar]
- 23.Velanovich V. The development of the GERD-HRQL symptom severity instrument. Dis Esophagus. 2007;20:130–4. doi: 10.1111/j.1442-2050.2007.00658.x. [DOI] [PubMed] [Google Scholar]
- 24.Enck P, Dubois D, Marquis P. Quality of life in patients with upper gastrointestinal symptoms: results from the Domestic/International Gastroenterology Surveillance Study (DIGEST) Scand J Gastroenterol Suppl. 1999;231:48–54. doi: 10.1080/003655299750025264. [DOI] [PubMed] [Google Scholar]
- 25.Madisch A, Miehlke S, Sell S, et al. Patients with Barretts esophagus experience less reflux complaints. Gastroenterology. 2006;130:A263–A263. [Google Scholar]
- 26.Zagari RM, Fuccio L, Wallander MA, et al. Gastro-oesophageal reflux symptoms, oesophagitis and Barrett’s oesophagus in the general population: the Loiano-Monghidoro study. Gut. 2008;57:1354–9. doi: 10.1136/gut.2007.145177. [DOI] [PubMed] [Google Scholar]
- 27.Nunez-Rodriguez MH, Miranda Sivelo A. Psychological Factors in Gastroesophageal Reflux Disease Measured by SCL-90-R Questionnaire. Dig Dis Sci. 2008 doi: 10.1007/s10620-008-0276-0. [DOI] [PubMed] [Google Scholar]
- 28.van der Velden AW, de Wit NJ, Quartero AO, et al. Maintenance treatment for GERD: residual symptoms are associated with psychological distress. Digestion. 2008;77:207–13. doi: 10.1159/000143796. [DOI] [PubMed] [Google Scholar]
- 29.Essink-Bot ML, Kruijshaar ME, Bac DJ, et al. Different perceptions of the burden of upper GI endoscopy: an empirical study in three patient groups. Qual Life Res. 2007;16:1309–18. doi: 10.1007/s11136-007-9239-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosmolen W, Boer K, Van Ianschot J, et al. Fear of cancer recurrence after endoscopic and surgical treatment for early neoplasia in Barrett’s esophagus. Gastroenterology. 2007;132:A474–A475. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


