Abstract
Background and Purpose
Stroke incidence and prevalence estimates in developing countries should include stroke cases not presenting to hospital. We performed door-to-door stroke case ascertainment in Durango Municipality, Mexico to estimate stroke incidence and prevalence, and to determine the error made by only ascertaining hospital cases.
Methods
Between September 2008 and March 2009, 1996 housing units were randomly sampled to screen for stroke in Durango Municipality residents ≥35 years of age. Field workers utilized a validated screening tool. Those screening positive were referred to a neurologist for history and examination and if confirmed, a head CT scan. Prevalence and cumulative incidence from the door-to-door surveillance were calculated and compared with previously reported hospitalization rates during the same defined time.
Results
Respondents included 2437 subjects from 1419 homes. The refusal rate was 3.8%. Twenty subjects had verified or probable stroke. The prevalence of probable or verified stroke was 7.7/1000 (95% CI: 4.3/1000, 11.2/1000). Five patients had a stroke during the time of the hospital surveillance, yielding a cumulative incidence of 232.3/100,000 (95% CI: 27.8, 436.9). Two of the 5 cases were captured by door-to-door surveillance but not by hospital surveillance.
Conclusions
This study provides the first community-based stroke prevalence and incidence estimates in Mexico. The wide confidence intervals, despite the large number of surveyed housing units, suggest the need for more advanced sampling strategies for stroke surveillance in the developing world.
Keywords: Stroke, Epidemiology, World Health, Mexico, Surveillance, Methods
Introduction
As stroke has become a major health problem for many Latin American countries, the widely-recognized paucity of good quality stroke epidemiology data from these countries is a major impediment to stroke reduction.1 Development and maintenance of a stroke surveillance system is essential to estimate the burden of stroke in communities and monitor the success of interventions. The Brain Attack Surveillance in Durango (BASID) project was established to build the vital infrastructure necessary for a surveillance system for stroke in a representative Mexican community. BASID emerged from an international collaboration to study stroke epidemiology in a similar fashion to the Brain Attack Surveillance in Corpus Christi (BASIC) study in Texas, USA2.
Recently, BASID reported the crude annual stroke hospitalization rate for those 25 and older as 143/100,000 (95% CI: 128–158).3 However, hospital surveillance alone is usually inadequate to identify all stroke cases since not all patients present to a hospital,4 perhaps due to mild stroke severity and expense of hospitalization. Instead, multiple sources of case ascertainment are often used in population-based studies to identify stroke patients outside hospitals, as outlined by WHO in its STEPS project.5 Indeed, door-to-door surveillance may be the only way to determine the proportion of subjects missed by limiting surveillance in Durango Municipality to hospitals and their emergency departments. We therefore performed a study of randomly selected households to estimate stroke incidence and prevalence, and to determine the proportion of cases missed by hospital surveillance only.
Methods
BASID took place in Durango Municipality, located in northern Mexico and encompassing one large city, Durango City, and 112 small towns and villages. The total population was 527,157 in 2005 (target population ≥35 years old: 168,859), with approximately 90% of the population residing within Durango city, the capital of Durango State. The door-to-door surveillance ran from September, 2008, to March 2009.
In stage 1, Durango Municipality households were randomly sampled to find household members who screened positive for stroke or stroke symptoms. During stage 2, participants who screened positive in stage 1 were invited to have an evaluation by a neurologist (AR) to verify a clinical diagnosis of stroke and were offered a head CT, if not previously performed.
Inclusion criteria were that subjects were ≥35 years old and had resided in Durango Municipality during the preceding 6 months. If a person normally residing in the house in Durango City and surrounding suburban towns was absent during the survey, five more attempts to contact him/her were made, either the same day or on a subsequent day. Due to the difficulty in traveling to rural towns, only one in-person contact attempt was made to find the subjects residing in those areas. If a family member stated the subject was available by phone, phone contact was attempted on a subsequent day. If two phone contact attempts were unfruitful, a proxy interview was allowed. The relationship of the person providing the proxy for the subject was noted. If no proxy was available, absent subjects were coded as non responders.
Field workers approach to residents
Five field workers received training in the use of the survey questionnaires. Address, age, and gender were noted for residents who declined participation. In residents who agreed to participate, a brief cognitive screen was done to ensure they had the cognitive ability to answer for themselves; three survey questionnaires were then administered. The first gathered demographic and baseline community stroke risk factors. The second ascertained history of possible fatal stroke in others in the household during the time of hospital surveillance (August 2007-July 2008) and requested permission to review relevant medical records. The third questionnaire was designed to determine stroke-free status in the respondent. We used a validated, Spanish translation of a modified version of the World Health Organization instrument for assessment of stroke prevalence in developing countries.6, 7 This instrument consists of eight questions aimed at identifying if the individual has ever experienced a sudden focal neurological deficit that lasted more than 24 hours.
Anyone who answered “yes” to one or more of the eight questions was considered positive for suspected stroke and invited to participate in the second part of the study. These subjects were invited to attend an outpatient clinic at the General Hospital of Durango City, where a neurologist performed a medical history and neurological examination. The diagnosis of stroke was established using the definition of the World Health Organization8 as patients with a rapid onset of a focal or global deficit lasting more than 24 hours without a competing, plausible, non-vascular cause. Definite stroke was defined as meeting the WHO definition and having confirmation by imaging. Probable stroke was defined as meeting the WHO definition but with no imaging performed or imaging was performed, but unavailable for review. Medical history was focused on presence of vascular risk factors, symptoms, and medical record review from the time of the event. A structured neurologic exam focused on eliciting focal neurologic deficits, utilizing a validated Spanish version of the National Institute of Health Stroke Scale.9 A non-enhanced head CT scan was performed in order to confirm stroke and to classify stroke type.
Sampling Framework
Selection of housing units was conducted in a stratified, multistage design. Durango Municipality was divided into two strata: Durango City, and all other localities in the Municipality. From each stratum, Basic Geostatistical Areas (AGEB, Spanish acronym, similar to census tracts) were sampled at random proportional to size (size was the number of housing units in the AGEB).10 Street blocks within AGEB’s were randomly selected, and finally, housing units within street blocks were chosen using systematic sampling. The total number of housing units selected from each stratum was approximately proportional to the number of housing units in each stratum. Table 1 shows the strata, the number of housing units per strata, and the final number of housing units selected from each.
Table 1.
Survey Strata for Durango Municipality
| Strata | Description | No. AGEBs by Strata | Total No. of Housing Units by Strata (% in Municipality) | No. Housing Units Selected for Survey by Strata |
|---|---|---|---|---|
| Urban | Durango City | 300 | 112,809 (88.8) | 1657 |
| Other | Rest of Durango Municipality | 72 | 14,243 (11.2) | 339 |
| Total | 372 | 127,052 | 1996 |
Statistical Analysis
Descriptive statistics for all variables collected were calculated. Stroke prevalence was defined as any history of stroke. Cumulative stroke incidence was defined as new stroke occurring between August 2007 – July 2008. Cumulative Stroke incidence was calculated as the number of cases divided by the number of people at risk based on 2005 Census data. However, given the multistage sampling design and non response rate, the cumulative stroke incidence, prevalence rate and their 95% confidence intervals were calculated by constructing a weighted average of the cumulative stroke incidence and prevalence rates in strata (defined below) using survey weights. Survey weights were constructed using standard formulas11 and were based on location (urban vs. rural), age, and gender and adjusted for non-response. For the purpose of constructing survey weights, age was categorized into six levels of ten year intervals: 35–44, 45–54, 55–64, 65–74, 75–84, and ≥85. In order to adjust the survey weights for the non-response rate, we used the number of eligible people in responding households to estimate the average number of eligible people in non-responding households. Cumulative incidence was reported as cases per 100,000, and prevalence as cases per 1,000. All calculations were done using SAS version 9.2.
Ethics
The BASID project was approved by the Institutional Review Board of the University of Michigan and the National Institute of Medical Sciences and Nutrition Salvador Zubiran in Mexico as well as the three public hospitals in Durango Municipality. All study personnel completed U.S. NIH Human Subjects Protection Training, translated to Spanish. Two separate consent processes were used for the door to door survey. In stage 1, the stroke questionnaire survey, oral consent was obtained and an informational study handout was given to eligible participants that summarized information about the study. For participants who screened positive in stage 1, written consent was obtained to participate in stage 2.
Results
A total of 1996 housing units were screened by study personnel (Table 1). We excluded 577 homes (28.9%) for one or more of the following reasons: 380 homes (65.9%) because residents were < 35 years old; 136 (23.6%) were uninhabited; 30 (5.2%) because residents lived in Durango Municipality <6 months; 25 (4.3%) because residents were out of home during screening in remote areas and we were unable to contact them later; and 22 (3.8%) homes with people that refused to participate. Of the remaining 1419 homes (71.1%) one or more eligible residents participated in the survey interview; 1189 (83.8%) were from urban areas and 230 (16.2%) from non-urban localities.
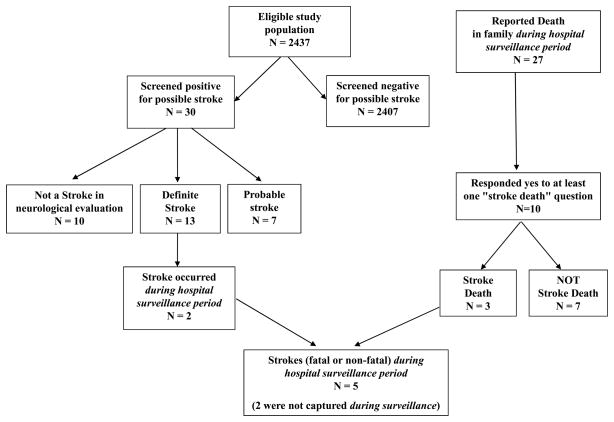
A total of 2437 surveys were obtained (2049 from urban areas and 388 from non-urban localities). The majority of the sample were women (56.7%) and the sample had a mean age of 51.5 years. Figure 1 shows the flow chart of the eligible population and stroke status. Thirty residents screened positive for possible stroke; ten subjects were found not to have had a stroke after neurological evaluation and head CT scan. The other 20 met clinical criteria for stroke. In 13 of the 20, neurologic exam and head CT verified stroke. Of the seven remaining subjects, in 3 the stroke was suspected based on neurologic history and examination but final validation was not possible as the patients did not attend the head CT appointment; and in 4 subjects, we were unable to verify stroke because they refused to participate in the second part of the study (2 lived too far away and 2 found travel too difficult due to advanced age or severe disability). These final seven subjects were classified as probable stroke.
Figure 1.
Flow of Patient Enrollment and Outcomes
The prevalence of probable or verified stroke was 7.7/1000 (95% CI: 4.3/1000, 11.2/1000); for only verified stroke, it was 5.1/1000 (95% CI: 2.3/1000, 7.9/1000). The small number of stroke cases precludes a further classification into stroke types. Demographics and stroke risk factors of participants are shown in Table 2 by stroke status and gender. Table 3 compares the cumulative stroke incidence and in-hospital case-fatality rates obtained during the hospital surveillance period with that of the door-to-door survey. As five patients with a stroke were identified in the door-to-door survey (two who survived and three who died) during the hospital surveillance period (August 2007 - July 2008), the cumulative incidence obtained from door-to-door surveillance was 232.3/100,000 (95% CI: 27.8, 436.9). When standardized to the WHO population the cumulative incidence was 270.7/100,000 (95% CI: 33.6, 507.9). This compares with the rate obtained in the same population from hospital only surveillance where the stroke rate was 178.3/100,000 (95% CI: 159.2, 199.6) and when standardized to the WHO population the stroke rate was 208.5/100,000 (95% CI: 184.9, 232.2).
Table 2.
Demographics and stroke risk factors of all respondents to door-to-door survey
| Eligible Population | Screened negative for possible stroke | Screened positive for possible stroke | Verified Stroke | Probable Stroke | Not a Stroke | |
|---|---|---|---|---|---|---|
| N | 2437 | 2407 | 30 | 13 | 7 | 10 |
| Age, mean (SD) | 51.5 (12.6) | 51.4 (12.6) | 59.0 (12.9) | 64.0 (14.2) | 58.7 (6.9) | 52.8 (12.5) |
| Female | 56.7% (1381) | 56.5% (1361) | 66.7% (20) | 53.9% (7) | 57.1% (4) | 90.0% (9) |
| Needed proxy | 1.1% (26) | 0.9% (21) | 16.7% (5) | 30.8% (4) | 14.3% (1) | 0.0% (0) |
| Have phone | 89.9% (2190) | 89.8% (2162) | 93.3% (28) | 100% (13) | 71.4% (5) | 100% (10) |
| Heart Disease | 5.3% (125) | 5.0% (121) | 23.3% (7) | 23.1% (3) | 0.0% (0) | 40.0% (4) |
| Hypertension | 29.1% (708) | 28.6% (688) | 66.7% (20) | 46.2% (6) | 85.7% (6) | 80.0% (8) |
| Diabetes | 14.5% (353) | 14.2% (341) | 40.0% (12) | 46.2% (6) | 57.1% (4) | 20.0% (2) |
| Current smoker | 20.5% (500) | 20.5% (494) | 20.0% (6) | 15.4% (2) | 42.8% (3) | 10.0% (1) |
| Seen Physician in past year | 76.1% (1854) | 75.8% (1825) | 96.7% (29) | 92.3% (12) | 100% (7) | 100% (10) |
| Lived/Worked in USA | 14.8% (361) | 14.8% (356) | 16.7% (5) | 23.1% (3) | 28.6% (2) | 0.0% (0) |
Table 3.
Comparison of cumulative stroke incidence (95% CI) from 8/2007 – 7/2008 between hospital surveillance3 and door-to-door survey. At-risk population ≥ 35 years: 168,859.
|
Hospital Surveillance Study | ||
| Strokes (n, incidence) | 301 | 178.3 (159.2, 199.6)/100,000 |
| In-hospital stroke case-fatality rate (n, %) | 113 | 37.5% |
|
Door-to-door Survey | ||
| Surveyed population ≥ 35 years (n) | 2,437 | |
| Strokes during hospital surveillance (n, incidence) | 5 | 232.3 (27.8, 436.9)/100,000 |
| Strokes captured by hospital surveillance phase (n) | 3 | |
| Strokes missed by hospital surveillance phase (n) | 2 | |
| Strokes occurring outside of Durango (n) | 1 | |
| In-hospital stroke case-fatality rate (n, %) | 2 | 40.0% |
Of the two stroke cases missed during hospital surveillance, one was an 89 year old female who received medical care in an outpatient clinic only. The other patient was a 70 year old female who had a stroke outside Durango Municipality and was discharged to her Durango Municipality home, where she died three months later from medical complications associated with severe stroke disability.
Finally, by restricting the analysis to those ≥45 years old, we were able to compare the annual cumulative stroke incidence in Non-Hispanic Whites (NHW’s) and Mexican Americans (MA’s) in Corpus Christi, Texas (BASIC study)2 with Mexicans in Durango Municipality. Of the 1558 people ≥45 years old surveyed in Durango Municipality, 5 had verified stroke during the survey period, giving a cumulative incidence of 386/100,000, compared with the cumulative stroke incidence for U.S. MA’s (560/100,000) and NHW’s (453/100,000).
Discussion
This extension of the BASID project utilizing the epidemiology “gold standard” of door-to-door surveillance suggests that cases are truly missed using ascertainment strategies that focus only on hospitals in Mexico. However, despite the labor intensiveness of a door-to-door approach to 2437 subjects, stroke is rare enough to leave wide confidence intervals on estimates of incidence and prevalence. For more precise estimates, a much larger sample size with prohibitive expense and time would be needed. For example, using random sampling, in the case of Durango Municipality, which has a target population of 168,859 and a point estimate of stroke incidence of 232/100,000, a sample size of 20,000 would be needed to obtain a margin of error of ± 24/100,000, or 10%. However, there are additional, more sophisticated sampling techniques that could have been used to achieve smaller margins of errors without necessarily increasing costs.
One sampling technique that could increase the precision is to initially perform a screening phase to identify the location of residents at high-risk for stroke, for example by focusing on the elderly. Once high risk areas are identified, they would be over-sampled in comparison to low-risk areas (e.g. neighborhoods with younger residents), a framework known as disproportionate sampling.12 A higher precision is gained by focusing efforts on the subpopulations where more cases are likely to be found. In the BASID door-to-door surveillance, only 6% of our sample was ≥75 years and only 16% were ≥65.
Other screening methods can be employed to capture more strokes. The most cost-effective is telephone interviews. However, they may bias towards patients with higher socio-economic status (who are likely already captured in hospital based-surveillance) and towards urban residents (in Durango Municipality, ~70% of the rural population have phones compared to 94% of those in urban homes). Mailing surveys is another approach, but could lead to a lower response rate and underestimation of cases particularly in populations with limited mail services (e.g. rural areas in developing countries). Another possibility would be to simply include neighboring houses if the target house was unoccupied at the time of the visit.
Another sampling technique is network sampling, which works under the assumption that members of the stroke population know each other. In this framework, surveyors ask an identified member of the affected population (i.e. a stroke survivor) to identify other affected members. For example, stroke sufferers may know other stroke victims through stroke support groups or by knowledge of relatives and friends. This reduces the number of contacts necessary by obtaining information on multiple subjects from one case. Alternatively, the cases identified by the first case may be contacted, and again asked to identify more cases. When this process is iterated, that is, each case found is asked to identify more cases until no more cases are identified, the technique is called snowballing. Though it is more difficult to identify isolated cases using network sampling and snowballing,13 statistical approaches can be used to obtain an estimate of the missed cases by evaluating the overlap cases (those cases identified multiple times).12 Multiple sampling techniques can be used in combination to compensate for their individual limitations, though combining methods may require complex computational analysis to obtain correct standard errors.
The proportion of stroke patients admitted to hospitals reported in recent population-based studies in developing countries is variable, ranging from 66% in Georgia14 to as high as 95% in Brazil.15 The cumulative stroke incidence of 232.3/100,000 found in the current study is similar to that reported in recent population-based studies in developing countries, with the notable exception of Iran16 and Georgia14 which report the highest incidences of stroke in developing countries.
Although the BASID cumulative stroke incidence in Mexico is consistent with most developing countries, MA’s living in the US have a higher cumulative stroke incidence compared with Mexicans living in Durango Municipality. One possibility to explain the discrepancy between stroke incidence rates in Durango Municipality and in Corpus Christi, is due to environmental or lifestyle changes that alters stroke susceptibility, as occurred in Japanese immigrants to the United States.17 An important focus of future work in both Durango Municipality and Corpus Christi will be to explore the social, environmental, biological, and genetic reasons for the discrepant stroke incidence in Mexicans on both sides of the border.
The stroke prevalence rate of 5.1–7.7/1000 in the community of Durango Municipality is within the range found in other Latin America door-to-door surveys (Table 4).18–23 Other studies have used different definitions and age groups making comparisons difficult. Prevalence rates are also comparable to those in European population-based studies, where the range of crude stroke prevalence was 5–10/1000.24
Table 4.
Door-to-door prevalence studies of stroke in Latin America
| Study | Population Screened | Number of strokes | Stroke Prevalence × 1,000 | Stroke Prevalence in the elderly* × 1,000 |
|---|---|---|---|---|
| Peru, 1995 (Cuzco)18 | 3,246 older than 15 years, from a urban population of 210,000 | 21 | 6.2 | NR† |
| Colombia, 1997 (Sabaneta)19 | 13,588 persons (all ages) from a urban population of 17,670 | 76 | 5.6 | 46.7 |
| Bolivia, 2000 (Cordillera)20 | 9,995 persons (all ages) from a rural population of 55,675 | 16 | 1.7 | 19.3 |
| Honduras, 2003 (Tegucigalpa)21 | 1,553 persons (all ages) from a urban population of 1,180,676 | 9 | 5.7 | NR† |
| Ecuador, 2004 (Atahualpa)22 | 1,568 older than 15 years, from a rural population of 1,671 | 10 | 6.4 | 36.1 |
| Honduras, 2007 (Salama)23 | 5,608 persons (all ages) from a rural population of 6,289 | 20 | 3.6 | 32.7 |
| Mexico, 2010 (Durango) | 2,437 older than 35 years, from a urban and rural population of 168,859 | 20 | 7.7 | 18.2 |
Some studies define elderly as ≥60, some as ≥65 years old.
NR: not reported
In summary, this work provides the first population-based study of stroke incidence and prevalence in Mexico comparing both hospital and door-to-door surveillance. Stroke cases that do not present to hospital are important in developing countries. More advanced sampling techniques are needed to maximize efficiency of community surveillance methods.
Acknowledgments
ACKKNOWLEDGEMENTS AND FUNDING PAGE
This project was funded by NIH R03 NS059056 and R01 NS38916.
Footnotes
Conflicts of Interest/Disclosures:
Carlos Cantu-Brito, MD, MSc: none
Jennifer J Majersik, MD, MS: none
Brisa N Sánchez, PhD: none
Angel Ruano, MD: none
Daniela Becerra-Mendoza: none
Jeffrey J Wing MPH: none
Lewis B Morgenstern, MD: none
References
- 1.Lavados PM, Hennis AJ, Fernandes JG, et al. Stroke epidemiology, prevention, and management strategies at a regional level: Latin America and the Caribbean. Lancet Neurol. 2007;6:362–72. doi: 10.1016/S1474-4422(07)70003-0. [DOI] [PubMed] [Google Scholar]
- 2.Morgenstern LB, Smith MA, Lisabeth LD, et al. Excess stroke in Mexican Americans compared with non-Hispanic Whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2004;160:376–83. doi: 10.1093/aje/kwh225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cantu-Brito C, Majersik JJ, Sánchez BN, et al. Hospitalized Stroke Surveillance in the Community of Durango, Mexico – the Brain Attack Surveillance in Durango (BASID) Study. Stroke. 2010;41:878–84. doi: 10.1161/STROKEAHA.109.577726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sudlow CL, Warlow CP. Comparable studies of the incidence of stroke and its pathological types: results from an international collaboration. International Stroke Incidence Collaboration. Stroke. 1997;28:491–9. doi: 10.1161/01.str.28.3.491. [DOI] [PubMed] [Google Scholar]
- 5.STEPwise approach to surveillance (STEPS) World Health Organization; [Accessed May 31, 2010]. http://www.who.int/chp/steps/en/ [Google Scholar]
- 6.Research protocol for measuring the prevalence of neurological disorders in developing countries. Geneva: Neurosciences Programme, World Health Organization; 1981. [Google Scholar]
- 7.Del Brutto OH, Idrovo L, Mosquera A, et al. Validation of a screening questionnaire for stroke detection in Spanish-speaking communities. Rev Neurol. 2004;39:301–4. [PubMed] [Google Scholar]
- 8.Hatano S. Experience of a multicenter stroke register: a preliminary report. Bull Word Healthy Organ. 1976;54:541–53. [PMC free article] [PubMed] [Google Scholar]
- 9.Dominguez R, Vila JF, Augustovski F, et al. Spanish cross-cultural adaptation and validation of the National Institutes of Health Stroke Scale. Mayo Clin Proc. 2006;81:476–80. doi: 10.4065/81.4.476. [DOI] [PubMed] [Google Scholar]
- 10.(INEGI) Instituto Nacional de Estadística. [Accessed May 31, 2010];Geografía e informática. www.inegi.gob.mx.
- 11.Lohr SL. Sampling: Design and Analysis. Pacific Grove: Brooks/Cole Publishing Company; 1999. [Google Scholar]
- 12.Kalton G, Anderson DW. Sampling Rare Populations. Journal of the Royal Statistical Society Series A (General) 1986;149:65–82. [Google Scholar]
- 13.Sudman S, Kalton G. New Developments in the Sampling of Special Populations. Annual Review of Sociology. 1986;12:401–29. [Google Scholar]
- 14.Tsiskaridze A, Djibuti M, van Melle G, et al. Stroke incidence and 30-day case-fatality in a suburb of Tbilisi: results of the first prospective population-based study in Georgia. Stroke. 2004;35:2523–8. doi: 10.1161/01.STR.0000144683.96048.98. [DOI] [PubMed] [Google Scholar]
- 15.Minelli C, Fen LF, Minelli DP. Stroke incidence, prognosis, 30-day, and 1-year case fatality rates in Matao, Brazil: a population-based prospective study. Stroke. 2007;38:2906–11. doi: 10.1161/STROKEAHA.107.484139. [DOI] [PubMed] [Google Scholar]
- 16.Azarpazhooh MR, Etemadi MM, Donnan GA, et al. Excessive incidence of stroke in Iran: evidence from the Mashhad Stroke Incidence Study (MSIS), a population-based study of stroke in the Middle East. Stroke. 2010;41:e3–e10. doi: 10.1161/STROKEAHA.109.559708. [DOI] [PubMed] [Google Scholar]
- 17.Robertson TL, Kato H, Rhoads GG, et al. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California. Incidence of myocardial infarction and death from coronary heart disease. Am J Cardiol. 1977;39:239–43. doi: 10.1016/s0002-9149(77)80197-5. [DOI] [PubMed] [Google Scholar]
- 18.Jaillard AS, Hommel M, Mazetti P. Prevalence of stroke at high altitude (3380 m) in Cuzco, a town of Peru. A population-based study. Stroke. 1995;26:562–8. doi: 10.1161/01.str.26.4.562. [DOI] [PubMed] [Google Scholar]
- 19.Uribe CS, Jimenez I, Mora MO, et al. Epidemiology of cerebrovascular diseases in Sabaneta, Colombia (1992–1993) Rev Neurol. 1997;25:1008–12. [PubMed] [Google Scholar]
- 20.Nicoletti A, Sofia V, Giuffrida S, et al. Prevalence of stroke: a door-to-door survey in rural Bolivia. Stroke. 2000;31:882–5. doi: 10.1161/01.str.31.4.882. [DOI] [PubMed] [Google Scholar]
- 21.Medina MT, Duron RM, Ramirez F, et al. Prevalencia de enfermedades neurológicas en Tegucigalpa: El estudio Kennedy. Rev Med Hondur. 2003;71:8–17. [Google Scholar]
- 22.Del Brutto OH, Idrovo L, Mosquera A, et al. Stroke in rural Ecuador: a three-phase, door-to-door survey. Neurology. 2004;63:1974–5. doi: 10.1212/01.wnl.0000145293.04832.78. [DOI] [PubMed] [Google Scholar]
- 23.Thompson-Cerna AR, Medina MT. The prevalence of cerebrovascular disease in the rural community of Salama, Honduras, using the capture-recapture epidemiological method. Rev Neurol. 2007;44:460–4. [PubMed] [Google Scholar]
- 24.Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2:43–53. doi: 10.1016/s1474-4422(03)00266-7. [DOI] [PubMed] [Google Scholar]