Abstract
Purpose
To investigate the association between birth month/photoperiod and refraction in infancy.
Methods
722 children with refractions measured between 1 and 3 months were included in this analysis. Non-cycloplegic near retinoscopy was performed by three experienced optometrists over a 32 year period. Photoperiod hours were calculated as the mean daylight hours 30 days after each infant's birth and then grouped into quartiles between 9.12 and 15.25 hrs. Two classifications for birth season were considered: regular season (Spring: March-May, Summer: June-August, Fall: September-November, and Winter: December-February) and alternate season (Spring: February-April, Summer: May-July, Fall: August-October, and Winter: November-January).
Results
The mean infant age was 2.11 +/− 0.55 months. The mean spherical equivalent refraction (SER) was 0.61 +/−1.56D. Children born in the photoperiod group with the most daylight hours had slightly lower refractions than those in the shortest photoperiod group (0.43D±1.60D vs. 0.87D±1.43D, p<0.05). In the longest photoperiod group the percentage of infants with SER<= −0.25D was significantly higher (51/179=28.49%) than in the shortest photoperiod group (31/177=17.51%) (p=0.02). Similar patterns were observed using the alternate season classification, with 1) lower mean SER in infants born in the summer vs. the winter and 2) a higher percentage of SER<= −0.25D in infants born in the summer vs. the winter. However, by regular seasons, the mean SERs were similar between summer and winter.
Conclusions
A small, statistically significant lower refraction was found in infants with the most vs. the least daylight soon after birth, suggesting that light might play a small role in the refractive error of newborns.
Keywords: refractive error, infants, birth season, photoperiod, myopia
The effect of light on refractive error has attracted new interest recently with the finding that myopic children spend fewer hours engaged in sports/outdoor activity than non-myopes.1–4 It has been suggested that this protective effect of outdoor activity on myopia development originates from more hours of light exposure rather than engagement in sports activities.2–3 In contrast, a detrimental effect of light in the form of an association between the use of nursery lighting before the age of 2 years and a greater prevalence of myopia was reported by Quinn et al.5 This finding was not replicated in several similar studies,6–8 but was supported in adults (but not children) in a U.S. study9 and also in children in a large study in Poland.10 Recently, two large studies in Israel and the UK showed that subjects born in the summer compared to the winter had a slightly higher prevalence of severe myopia as adults.11,12 Taking all the evidence from human studies together, it seems that there is no agreement on the effect of light exposure during infancy on later refractive development, while there is consensus that more light exposure at school age reduces the risk of myopia.
Other evidence on the relationship between light and refractive error comes from animal studies. Previous publications indicated that disruption of the light-dark circadian rhythm induced abnormal eye growth and disturbed emmetropization13–15. Chicks reared under constant light were found to develop hyperopia, shallower anterior chamber depths, and flattened corneas.13 However, these results were not mirrored in monkeys. Smith and colleagues did not find any significant differences in vitreous chamber depth, corneal radius, corneal thickness, anterior chamber depth, or lens thickness between monkeys reared in constant light and a control group reared with a 12/12 or 8.5/15.5 light-dark cycle over a 5-month treatment period. However unusual emmetropization was found in three monkeys, with an abnormally steep cornea in one monkey and axial anisometropia in the other two.16 Recently, Ashby el al reported that chicks exposed to high vs. low luminance lighting conditions while wearing diffusing lenses had reduced myopia, and the reduction in deprivation myopia was partially regulated by dopamine.17,18
These contradictory findings suggest that the exact mechanisms of how light affects refractive error in the short- as well as long-term are complex and may also be species-dependent. In this paper we focus on the impact of early light exposure on refractive error in human infants. Specifically, we investigate the association between birth season/photoperiod and infants' refraction shortly after birth.
METHODS
Subjects
Seven hundred and twenty two children with refractions soon after birth (1–3 months) were included in the data analysis. All subjects in this study were participants of a previous longitudinal study of refractive error and visual function that started in the Infant Vision Laboratory at the Massachusetts Institute of Technology (MIT) in 1974 and continued at the New England College of Optometry (NECO) until the middle of 2006. Nearly all subjects (95%) were white and half were female. Subject recruitment and refraction procedures have been described elsewhere.19 Informed written consent forms were signed by a parent or guardian. The project was approved by the Institutional Review Boards at both MIT and NECO, and it adhered to the tenets of the Declaration of Helsinki.
Procedure
Non-cycloplegic near retinoscopy20 was used to measure refractive error. Only three experienced optometrists made the measurements over a 32-year period: Dr. Indra Mohindra from 1974 to the middle of 1980, Dr. Mitch Scheiman from late 1980 to the middle of 1982, and Dr. Frank Thorn from late 1982 to 2006. The non-cycloplegic technique was chosen in order to maintain high retention rates for longitudinal studies of visual development and refractive error.
The non-cycloplegic retinoscopy was performed in a dark room with the infant fixating on the light of the retinoscope at a fixed distance of 50 cm. An adjustment factor of −1.25D was added to account for the 50 cm working distance and tonic accommodation. A detailed description of near retinoscopy and calculation of the adjustment factor has been provided previously.19–21 In this study 28% of the subjects were refracted by Drs. Mohindra and Scheiman, and 72% were refracted by Dr. Thorn.
In performing near retinoscopy on an infant Drs. Mohindra and Scheiman recorded the retinoscopic reading shown by the infant most of the time during a session, while Dr. Thorn used the most hyperopic reading shown by the infant in a session. This difference in technique produced more positive readings from Dr. Thorn by approximately 0.50 D.21 The data used for the current analysis were adjusted to account for this difference.
Refraction data were grouped in three ways
(1) by photoperiod, taking into account the hours of daylight in the month after birth; (2) by regular seasons; and (3) by an alternate classification of season described below.
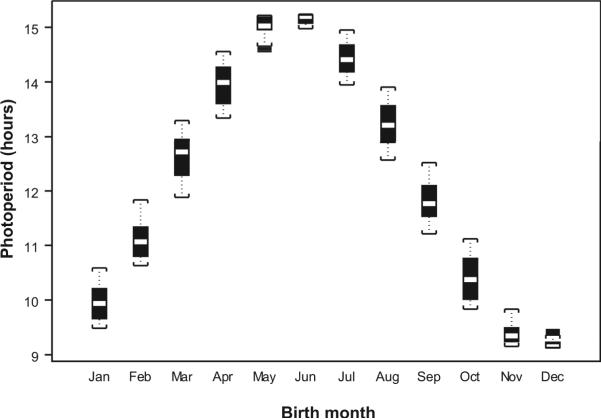
The photoperiod level was computed as the mean daylight hours for the first 30 days after birth in the Boston area. The daylight hours in 2010 were downloaded at the following link (http://www.timeanddate.com/worldclock/city.html?n=43; accessed May 14, 2010). The maximum variation of daylight time for the same day across the last four decades was about 2 minutes; thus data downloaded for 2010 provide a good representation of the daylight time from 1970 to 2010. As shown in Figure 1, the photoperiod levels ranged from 9.125 hours to 15.24 hours, with the fewest hours in December and the most in June. Four photoperiod levels were assigned based on the quartile range of our sample: 1(9.125–9.935); 2(9.935–12.44); 3 (12.44–14.153); and 4 (14.153–15.24). The 6-hour range of hours of daylight in our study was smaller than that reported in the U.K. study (9.31– 18.01 hours) but larger than that in the Israel study (10.1–14.23 hours).11,12
Figure 1.
Photoperiod level (mean hours of daylight) by birth month, where 1 is January and 12 is December.
Birth months were grouped into four regular seasons
Spring (March, April, and May); Summer (June, July, and August); Fall (September, October, and November); and Winter (December, January, and February), the same as those used in the U.K. study.12 An alternative classification of birth season also was considered in order to group together months with more similar light patterns: Spring (February, March, and April); Summer (May, June, and July); Fall (August, September, and October); and Winter (November, December, and January).
Statistical analysis
The refractive error of each subject was taken as the spherical equivalent refraction (SER) by adding the spherical and half of the cylinder power (in negative notation). Due to a high correlation (r=0.98) in refraction between the infants' two eyes, only refraction data of the right eyes were used. A one-way ANOVA was used to test for refractive differences between groups defined by birth seasons or photoperiod categories. Comparisons in refractive error between summer and winter and between the longest and shortest photoperiod groups were conducted via the two-sample t test. The Chi-square test was used to test the association between photoperiod categories/birth season and refractive groups. The two cutoffs used to define refractive groups were: SER<= 0.625D vs. SER> 0.625D and SER<= −0.25D vs. SER> −0.25D. When photoperiod hours were treated as a continuous variable, simple linear regression was conducted to assess the correlation between refractive error and photoperiod hours and ordered logistic regression was applied to evaluate the association between refractive groups and photoperiod hours. Statistical significance was taken as p<0.05.
RESULTS
The numbers of subjects by birth month ranged from 27 to 94, with the fewest subjects born in February and the most subjects in August. The average age of the subjects was 2.11 +/− 0.55 months. The mean spherical equivalent refraction was 0.61 +/−1.56D and the median refraction was 0.625D. The gender distribution in this sample was balanced (367 females vs. 355 males).
The refractions differed significantly across the four photoperiod categories (ANOVA p=0.028), with infants born in the longest photoperiod group having a significantly less plus mean SER (0.43D±1.60D) than those (0.87D±1.43D) born in the shortest photoperiod group (p=0.008), as shown in the top of Table 1 and the first panel in Figure 2. Using the regular classification of birth seasons, the early infancy refractions did not vary significantly across the four groups (p=0.458) and did not differ significantly between summer and winter, the seasons with the most and the least light (p=0.355), as shown in the middle of Table 1 and the second panel of Figure 2. In contrast, significant seasonal variations in the mean early infancy refractions were found using the alternate classification of seasons (ANOVA p<0.05), with more positive mean refractions for infants born in the winter than the summer (p=0.014), as shown in the bottom of Table 1 and the last panel in Figure 2. In addition, using either seasonal classification, the mean refractions were more similar and higher in fall and winter than in spring and summer, which also had similar refractions. When treating photoperiod hours as a continuous variable, the spherical equivalent refraction in diopters in early infancy was negatively correlated with the number of daylight hours (r=-0.08). The effect was small but statistically significant (slope=−0.058, p=0.03). Longer daylight hours were also significantly associated with more negative or less positive refractive groups (either SER<= −0.25D or SER<=0.625D) by ordered logistic regression (common OR=1.08 (1.01, 1.15) per one-hour daylight increase).
Table 1.
Refractive error during early infancy by photoperiod level or season.
| Category | n | mean (sd) | median | SER>0.625D |
|---|---|---|---|---|
| 722 | 0.61[1.56] | 0.625 | ||
|
| ||||
| Photoperiod level | ||||
| 1: [9.125, 9.935) | 177 | 0.87[1.43] | 0.875 | 103 (58.19%) |
| 2: [9.935, 12.440) | 184 | 0.47[1.86] | 0.625 | 87 (47.28%) |
| 3: [12.440, 14.153) | 182 | 0.68[1.24] | 0.625 | 86 (47.25%) |
| 4: [14.153, 15.25) | 179 | 0.43[1.60] | 0.5 | 83 (46.37%) |
| p-value for comparison across 4 groups | 0.028 | 0.080 | ||
| p-value for comparison between longest and shortest photoperiod | 0.008 | 0.034 | ||
|
| ||||
| Regular Seasons | ||||
| Spring: Mar–May | 138 | 0.47[1.67] | 0.5 | 68 (49.28%) |
| Summer: June–Aug | 234 | 0.56[1.39] | 0.625 | 122 (52.14%) |
| Fall: Sep–Nov | 184 | 0.71[1.68] | 0.75 | 107 (58.15%) |
| Winter: Dec–Feb | 166 | 0.70[1.54] | 0.75 | 89 (53.61%) |
| p-value for comparison across 4 groups | 0.458 | 0.430 | ||
| p-value for comparison between summer and winter | 0.355 | 0.850 | ||
|
| ||||
| Alternate Seasons | ||||
| Spring: Feb–April | 124 | 0.44[1.73] | 0.50 | 57 (45.97%) |
| Summer: May–July | 181 | 0.40[1.50] | 0.50 | 83 (45.86%) |
| Fall: Aug–Oct | 210 | 0.74[1.53] | 0.75 | 124 (59.05%) |
| Winter: Nov–Jan | 207 | 0.77[1.50] | 0.75 | 122 (58.94%) |
| p-value for comparison across 4 groups | 0.036 | 0.007 | ||
| p-value for comparison between summer and winter | 0.014 | 0.013 | ||
Figure 2.
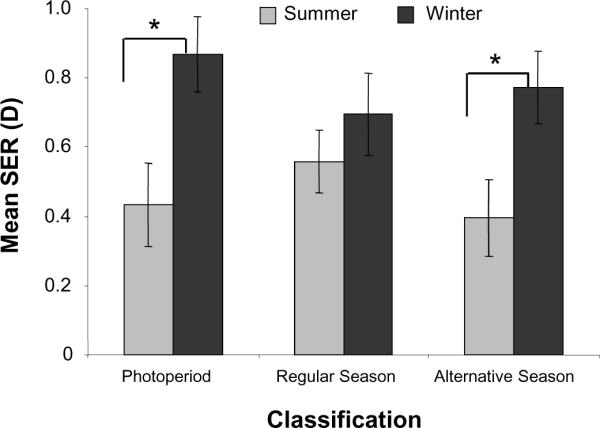
Mean refractive error between the two extreme groups, either the longest vs. the shortest photoperiod groups or summer vs. winter. Error bars are standard errors. The asterisk indicates p-value<0.05.
As shown in Table 1, the percentage of infants with refractions above the median (0.625D) was significantly lower in the longest photoperiod group (83/179=46.37%) than in the shortest photoperiod group (103/177=58.19%; p=0.034). By regular birth seasons, no significant differences in the percentages of subjects with SER>0.625D were found across the four seasons (p=0.430). In comparison, by the alternate season grouping, the percentage of subjects with more positive refractions (SER>0.625D) in the summer (83/181=45.86%) was significantly lower than that in the winter (122/207=58.94%; p=0.013), similar to the photoperiod result.
Previously we showed that children with more negative refractive errors during early infancy were more likely to develop myopia at school age.22 In the current study we defined a more myopic refractive group as SER<= −0.25D. The percentage of infants in this group in the longest photoperiod category was significantly higher (51/179=28.49%) than in the shortest photoperiod category (31/177=17.51%;p=0.020), as shown in the first panel of Figure 3. By regular birth seasons, the proportions of infants with SER <= −0.25D were similar between summer and winter (53/234=22.65% vs. 37/166=22.29%, p=0.971), as shown in the second panel of Figure 3. However, the proportion of infants in this group using the alternate season classification was slightly higher in the summer (52/181=28.73%) than in the winter (41/207=19.81%), as shown in the last panel in Figure 3. The difference approached statistical significance (p=0.053).
Figure 3.
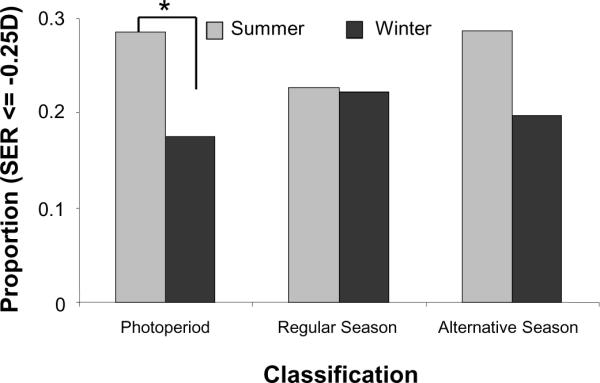
The proportion of subjects with SER<= −0.25D between the two extreme groups. For the photoperiod panel summer and winter refer to the longest (photoperiod category 4) and the shortest (photoperiod category 1) groups, respectively. The asterisk indicates p-value<0.05.
DISCUSSION
In this study we found a small, statistically significant difference in refractive errors shortly after birth across photoperiod categories and when using a classification of seasons similar in light levels to photoperiod. Infants born in the summer had less positive refractions than those born in the winter. However, when using the typical classification of seasons, no significant differences were found.
A higher percentage of infants born in the longest vs. shortest photoperiod group had low refractive error (SER<=−0.25D). A similar trend, with a higher percentage of infants born in the summer vs. winter having SER<=−0.25D, was found by the alternate season classification but not by the regular season classification. The photoperiod difference is in accord with the results of a large study conducted in Israel on young adults,11 but not with results of a U.K. study over a wide age range which reported no significant association between photoperiod and high myopia after adjusting for other covariates.12 Both studies found significant birth season differences in the prevalence of high myopia, with subjects born in the summer having a slightly higher prevalence than those born in the winter. Their seasonal differences, based on the typical classification, agree with our findings for the alternate seasons but not for the regular seasons.
The results of the two studies in the U.K. and Israel have been cited as evidence for a positive association between light exposure in early childhood and myopia in humans. Although the two large studies had statistically significant results, the observed differences are unlikely to have significant biological implications as the maximum differences in the prevalence between two photoperiod groups for any type of myopia (low, moderate or high) were no more than 0.7%. Other frequently cited evidence for the association between light and myopia was based on studies linking nursery lighting and more myopia in childhood,5,10 but conflicting results were found in similar studies.6–8 Our study found significant associations between photoperiod level shortly after birth and refractive error in early infancy, suggesting that light might influence the refractive error of newborns. Previously we reported an association between refractions in infants and older children,22 but it is unclear what role, if any, early light exposure plays.
Other factors in addition to light exposure might be related to season of birth. In our sample birth month might be associated with the education level of the parents, since better educated (and more myopic) parents, especially if on an academic calendar, might plan to have their children born in the summer months. To some extent this might be true in our sample, with the lowest and highest birth rates in February (n = 27) and August (n = 94), respectively. However, we did not collect information on parental education and we do not have sufficient parental refractions from this cohort to rule out these possible confounders. Another factor that might be related to season of birth is the differential outdoor light exposure of infants, with more limited time outside during the winter compared to the other months in Boston.
Despite the conflicting findings in the literature over the role that early light exposure plays in later myopia development, recent results agree that longer hours of sports/outdoor activity after preschool age are protective against myopia development. Two studies have suggested that being outdoors rather than being physically active is the key beneficial factor.2,3 One hypothesis relating light and myopia focuses on the light intensity and suggests that the release of dopamine stimulated by sunlight prohibits abnormal eye growth.2 Findings from animal studies support the involvement of dopamine. Using a form deprivation paradigm Ashby and colleagues showed that chicks reared with high luminance levels (15,000 lux and/or 30,000 lux) had reduced myopia compared to those reared with low luminance levels (500 lux), with the compromised myopization at least partially regulated by dopamine.17,18
There are some limitations in the present study. First, the reported difference in infancy refraction by photoperiod might be attributed in part to differences in parental refractions. Although the Israel and the U.K. studies did not have parental refractions and thus could not adjust for this potential confounder either, Mandel et al. used sibling data as a substitute to account for the familial association.11,12 Their results suggested that family planning is unlikely to account for the significant association between daylight hours and refraction in young adults. It is not clear how much we can extrapolate their findings to ours given the differences in age and in the distribution of daylight hours. Another limitation of our study is that we did not formally collect detailed education or socioeconomic status information from our parents and thus could not adjust our data for these factors.
In conclusion, we found a small but significant difference in early refractive error between infants born in months with the most vs. the least light, suggesting that light might play a small role in the refractive error of newborns.
ACKNOWLEDGMENTS
This work was supported by NEI/NIH grants EY01191, EY014817 and EY018694. We would like to thank all participants in our longitudinal study and their families.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48:3524–32. doi: 10.1167/iovs.06-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, Mitchell P. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–85. doi: 10.1016/j.ophtha.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 3.Dirani M, Tong L, Gazzard G, Zhang X, Chia A, Young TL, Rose KA, Mitchell P, Saw SM. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol. 2009;93:997–1000. doi: 10.1136/bjo.2008.150979. [DOI] [PubMed] [Google Scholar]
- 4.Deng L, Gwiazda J, Thorn F. Children's refractions and visual activities in the school year and summer. Optom Vis Sci. 2010;87:406–13. doi: 10.1097/OPX.0b013e3181da8a85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quinn GE, Shin CH, Maguire MG, Stone RA. Myopia and ambient lighting at night. Nature. 1999;399:113–4. doi: 10.1038/20094. [DOI] [PubMed] [Google Scholar]
- 6.Gwiazda J, Ong E, Held R, Thorn F. Myopia and ambient night-time lighting. Nature. 2000;404:144. doi: 10.1038/35004663. [DOI] [PubMed] [Google Scholar]
- 7.Zadnik K, Jones LA, Irvin BC, Kleinstein RN, Manny RE, Shin JA, Mutti DO, CLEERE Study Group Myopia and ambient night-time lighting. Nature. 2000;404:143–4. doi: 10.1038/35004661. [DOI] [PubMed] [Google Scholar]
- 8.Guggenheim JA, Hill C, Yam TF. Myopia, genetics, and ambient lighting at night in a UK sample. Br J Ophthalmol. 2003;87:580–2. doi: 10.1136/bjo.87.5.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chapell M, Sullivan B, Saridakis S, Costello L, Mazgajiewski N, McGinley J, McGlone J, Andris C, Pasquarella A. Myopia and night-time lighting during sleep in children and adults. Percept Mot Skills. 2001;92:640–2. doi: 10.2466/pms.2001.92.3.640. [DOI] [PubMed] [Google Scholar]
- 10.Czepita D, Goslawski W, Mojsa A, Muszynska-Lachota I. Role of light emitted by incandescent or fluorescent lamps in the development of myopia and astigmatism. Med Sci Monit. 2004;10:CR168–71. [PubMed] [Google Scholar]
- 11.Mandel Y, Grotto I, El-Yaniv R, Belkin M, Israeli E, Polat U, Bartov E. Season of birth, natural light, and myopia. Ophthalmology. 2008;115:686–92. doi: 10.1016/j.ophtha.2007.05.040. [DOI] [PubMed] [Google Scholar]
- 12.McMahon G, Zayats T, Chen YP, Prashar A, Williams C, Guggenheim JA. Season of birth, daylight hours at birth, and high myopia. Ophthalmology. 2009;116:468–73. doi: 10.1016/j.ophtha.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Li T, Troilo D, Glasser A, Howland HC. Constant light produces severe corneal flattening and hyperopia in chickens. Vision Res. 1995;35:1203–9. doi: 10.1016/0042-6989(94)00231-a. [DOI] [PubMed] [Google Scholar]
- 14.Li T, Howland HC, Troilo D. Diurnal illumination patterns affect the development of the chick eye. Vision Res. 2000;40:2387–93. doi: 10.1016/s0042-6989(00)00098-5. [DOI] [PubMed] [Google Scholar]
- 15.Cohen Y, Belkin M, Yehezkel O, Avni I, Polat U. Light intensity modulates corneal power and refraction in the chick eye exposed to continuous light. Vision Res. 2008;48:2329–35. doi: 10.1016/j.visres.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Smith EL, 3rd, Bradley DV, Fernandes A, Hung LF, Boothe RG. Continuous ambient lighting and eye growth in primates. Invest Ophthalmol Vis Sci. 2001;42:1146–52. [PubMed] [Google Scholar]
- 17.Ashby R, Ohlendorf A, Schaeffel F. The effect of ambient illuminance on the development of deprivation myopia in chicks. Invest Ophthalmol Vis Sci. 2009;50:5348–54. doi: 10.1167/iovs.09-3419. [DOI] [PubMed] [Google Scholar]
- 18.Ashby RS, Schaeffel F. The effect of bright light on lens compensation in chicks. Invest Ophthalmol Vis Sci. 2010;51:5247–53. doi: 10.1167/iovs.09-4689. [DOI] [PubMed] [Google Scholar]
- 19.Gwiazda J, Scheiman M, Mohindra I, Held R. Astigmatism in children: changes in axis and amount from birth to six years. Invest Ophthalmol Vis Sci. 1984;25:88–92. [PubMed] [Google Scholar]
- 20.Mohindra I. A non-cycloplegic refraction technique for infants and young children. J Am Optom Assoc. 1977;48:518–23. [PubMed] [Google Scholar]
- 21.Thorn F, Gwiazda J, Held R. Using near retinoscopy to refract infants. In: Vital-Durand F, Atkinson J, Braddick OJ, editors. Infant Vision. Oxford University Press; Oxford: 1996. pp. 113–24. [Google Scholar]
- 22.Gwiazda J, Thorn F, Bauer J, Held R. Emmetropization and the progression of manifest refraction in children followed from infancy to puberty. Clin Vis Sci. 2003;8:337–44. [Google Scholar]