Abstract
Non-tuberculous mycobacterial skin infections have an increasing incidence. In immunocompetent patients, they usually follow local trauma. We present a case of cutaneous Mycobacterium abscessus infection following mesotherapy. The lesions were successfully treated with a combination of clarithromycin, ciprofloxacin, and doxycycline. Atypical mycobacterial infection should be suspected in patients who develop late-onset skin and soft tissue infection after cutaneous injury, injection, and surgical intervention, particularly if they do not respond to conventional antibiotic treatment.
Key Words: Non-tuberculous mycobacteria, Mycobacterium abscessus, Mesotherapy
Introduction
Skin and soft tissue infections caused by non-tuberculous mycobacteria have been increasingly described as a complication associated with many procedures, including liposuction, illicit soft tissue augmentation, acupuncture, and contamination from medical instruments during surgery [1, 2, 3, 4, 5]. Mycobacterium abscessus is a rapid-growing atypical mycobacterium that has been reported to cause a variety of cutaneous infections. Herein, we report a case of cutaneous M. abscessus infection associated with mesotherapy injection.
Case Report
A previously healthy 44-year-old woman presented with a 3-week history of tender erythematous nodules on her face. The lesions had developed 2 weeks after mesotherapy injection for facial rejuvenation, using an unknown substance administered by an uncertified aesthetician. She had no fever or other systemic symptoms. Her friends who underwent mesotherapy administered by the same practitioner developed similar lesions. The lesions did not improve after a 2-week course of oral cephalexin. Physical examination revealed multiple, discrete, tender erythematous nodules and plaques with minimal serosanguinous discharge on both cheeks (fig. 1) and on the forehead (fig. 2). There was no lymphadenopathy. The results of the rest of the examination were normal. A skin biopsy specimen obtained from a nodule on the right cheek revealed dense inflammation predominantly consisting of neutrophils, histiocytes and multinucleated giant cells in the superficial and deep dermis (fig. 3). Gram staining, fungal and acid-fast bacilli stains were negative. Tissue culture was positive for M. abscessus, sensitive to clarithromycin, ciprofloxacin, doxycycline, cefoxitin, and amikacin. Bacterial and fungal cultures were negative. The patient was treated with a combination of clarithromycin 500 mg twice daily, doxycycline 100 mg twice daily, and ciprofloxacin 500 mg twice daily according to the bacterial sensitivity testing. The lesions started to improve 2 weeks after initiation of the therapy. The patient completed 6 months of treatment, which resulted in complete resolution of the lesions with minimal atrophic hyperpigmented scars. There was no recurrence at the 3-month follow-up.
Fig. 1.

Erythematous nodules and plaques on the right cheek.
Fig. 2.

Erythematous nodules and plaques on the forehead.
Fig. 3.
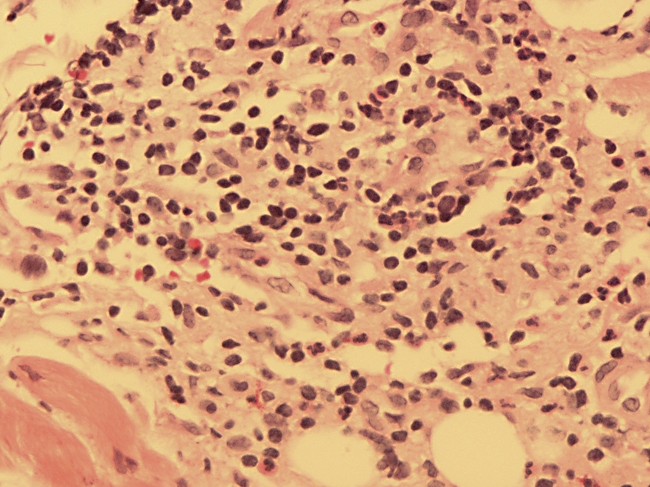
Hematoxylin and eosin-stained slide, ×400. A dense inflammatory infiltrate composed of neutrophils and histiocytes in the dermis.
Discussion
Mesotherapy was first introduced in France in 1952, consisting of an injection of highly diluted drugs and different substances into the dermis and subcutaneous tissue. It causes both the chemical and physical stimulation of cutaneous mesoderm. Direct injection in involved sites allows lower dosages of drugs to be used. All intravenously injectable drugs may be used, except oily and alcoholic solvents. This technique was originally developed to treat localized pain, vascular and lymphatic disorders, but its use in aesthetic medicine has increased in recent years [5].
M. abscessus belongs to the group of rapidly growing non-tuberculous mycobacteria which is characterized by a rapid growth rate (within 7 days) on the culture. The organism is ubiquitously present in soil, decaying vegetation, and water (e.g., natural water, sewage water, drinking water tanks, and tap water). M. abscessus causes a wide range of clinical diseases including skin and soft-tissue infection, keratitis, osteomyelitis, pulmonary infection, and disseminated infection. In skin and soft-tissue infection, it usually follows penetrating trauma and typically occurs in immunocompetent individuals [6]. There are several reports of outbreaks of M. abscessus infections caused by non-sterile techniques or contaminated materials, following surgery, liposuction, foreign body implantation, mesotherapy, acupuncture, and soft tissue augmentation [1, 2, 3, 4, 5].
The clinical presentations of cutaneous M. abscessus infection ranges from asymptomatic to tender erythematous violaceous nodules and plaques, cellulitis, abscesses, ulcer, and draining sinus with serosanguinous discharge [7]. The lesions may be solitary or multiple, and localized lymphadenopathy is occasionally seen. The onset is varied from a few weeks to months after exposure [8].
Approximately 10–20% of localized cutaneous M. abscessus infections in immunocompetent patients resolve spontaneously without treatment in an average of 8 months [9]. Currently, there is no standard guideline for the treatment of cutaneous M. abscessus infection. Multiple modalities including surgery, draining of abscesses, removal of necrotic tissue, foreign body removal, and an extended course of antibiotics are recommended. The in vitro sensitivity helps guiding antimicrobial therapy. However, the in vivo efficacy against the mycobacteria is not completely reflected by in vitro sensitivity alone, but also depends on the function of local and general host defenses against the infection. M. abscessus is usually susceptible to clarithromycin, amikacin, linezolid, tigecycline and variably susceptible to cefoxitin and imipenem (table 1). Clarithromycin is generally the recommended drug of choice. It should be given in a combination with other antibiotics for 4–6 months. Monotherapy is not recommended in treating M. abscessus infection because of the potential for emergence of antibiotic resistance, as has been reported with other mycobacteria, such as Mycobacterium chelonae [10].
Table 1.
Antimycobacterial drugs, typical sensitivity pattern, and recommended dose for M. abscessus infection [6]
| Drugs | Typical sensitivity pattern | Dosage∗ and route |
|---|---|---|
| Clarithromycin | S | 500–1,000 mg/day PO |
| Azithromycin | S | 500–1,000 mg/day PO |
| Amikacin | S | <800-l,000 mg/day IV, IM |
| Linezolid | S | 1,200 mg/day PO |
| Tigecycline | S | 100 mg/day IV |
| Cefoxitin | V | 12,000 mg/day IV |
| Imipenem | V | 25 mg/kg/day IV |
| Ciprofioxacin | R | 1,000 mg/day PO |
| Sulfamethoxazole | R | 3,000 mg/day PO |
| Doxycycline | R | 200 mg/day PO |
Dosage in adult patients with normal renal function. S = sensitive; V = variable; R = resistant; PO = per os; IV = intravenous; IM = intramuscular.
In conclusion, we report a case of cutaneous M. abscessus infection associated with mesotherapy. This case emphasizes the importance of adequate sterile measures in all medical procedures and stresses the need to suspect the possibility of an atypical mycobacterium infection in patients who develop late-onset skin and soft tissue infection after cutaneous injury, injections, and surgical interventions, particularly if they do not respond to conventional antibiotic treatment.
Disclosure Statement
The authors have no conflicts of interest.
Footnotes
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
References
- 1.Fisher EJ, Gloster HM., Jr Infection with Mycobacterium abscessus after Mohs micrographic surgery in an immunocompetent patient. Dermatol Surg. 2005;31:790–794. doi: 10.1097/00042728-200507000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Murillo J, Torres J, Bofill L, Ríos-Fabra A, Irausquin E, Istúriz R, Guzmán M, Castro J, Rubino L, Cordido M. Skin wound infection by rapidly growing mycobacteria: an unexpected complication of liposuction and liposculpture. The Venezuelan Collaborative Infectious and Tropical Diseases Study Group. Arch Dermatol. 2000;136:1347–1352. doi: 10.1001/archderm.136.11.1347. [DOI] [PubMed] [Google Scholar]
- 3.Ryu HJ, Kim WJ, Oh CH, Song HJ. Iatrogenic Mycobacterium abscessus infection associated with acupuncture: clinical manifestations and its treatment. Int J Dermatol. 2005;44:846–850. doi: 10.1111/j.1365-4632.2005.02241.x. [DOI] [PubMed] [Google Scholar]
- 4.Toy BR, Frank PJ. Outbreak of Mycobacterium abscessus infection after soft tissue augmentation. Dermatol Surg. 2003;29:971–973. doi: 10.1046/j.1524-4725.2003.29262.x. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Navarro X, Barnadas MA, Dalmau J, Coll P, Gurguí M, Alomar A. Mycobacterium abscessus infection secondary to mesotherapy. Clin Exp Dermatol. 2008;33:658–659. doi: 10.1111/j.1365-2230.2008.02869.x. [DOI] [PubMed] [Google Scholar]
- 6.Petrini B. Mycobacterium abscessus: an emerging rapid-growing potential pathogen. APMIS. 2006;114:319–328. doi: 10.1111/j.1600-0463.2006.apm_390.x. [DOI] [PubMed] [Google Scholar]
- 7.Uslan DZ, Kowalski TJ, Wengenack NL, Virk A, Wilson JW. Skin and soft tissue infections due to rapidly growing mycobacteria: comparison of clinical features, treatment, and susceptibility. Arch Dermatol. 2006;142:1287–1292. doi: 10.1001/archderm.142.10.1287. [DOI] [PubMed] [Google Scholar]
- 8.Piersimoni C, Scarparo C. Extrapulmonary infections associated with nontuberculous mycobacteria in immunocompetent persons. Emerg Infect Dis. 2009;15:1351–1358. doi: 10.3201/eid1509.081259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weitzul S, Eichhorn PJ, Pandya AG. Nontuberculous mycobacterial infections of the skin. Dermatol Clin. 2000;18:359–377. doi: 10.1016/s0733-8635(05)70182-0. [DOI] [PubMed] [Google Scholar]
- 10.Tebas P, Sultan F, Wallace RJ, Jr, Fraser V. Rapid development of resistance to clarithromycin following monotherapy for disseminated Mycobacterium chelonae infection in a heart transplant patient. Clin Infect Dis. 1995;20:443–444. doi: 10.1093/clinids/20.2.443. [DOI] [PubMed] [Google Scholar]


