Abstract
Background
Racial disparities in survival after out-of-hospital cardiac arrest have been reported but their causes remain uncertain. We sought to determine if hospital racial composition accounted for survival differences for patients hospitalized after cardiac arrest.
Methods
We evaluated hospitalizations of white and black Medicare beneficiaries (2000–2007) admitted from the ED to ICU with a diagnosis of cardiac arrest or ventricular fibrillation. We examined unadjusted survival rates and developed a multivariable logistic regression model which included patient and hospital factors.
Results
We analyzed 68,115 cardiac arrest admissions. Unadjusted survival to hospital discharge was worse for blacks (n=7,942) compared with whites (n=60,173) (30% vs. 33%, p<0.001). In multivariate analyses accounting for patient and hospital factors, adjusted probability of survival was worse for black patients at hospitals with higher proportions of black patients (31%, 95% CI: 29%–32%) compared with predominately white hospitals (46%, 95% CI: 36%–57%; p=.003). Similarly, whites had worse risk adjusted survival at hospitals with higher proportions of black patients (28%, 95% CI: 27%–30%) compared to predominately white hospitals (32%, 95% CI: 31%–33%, p=.006). Blacks were more likely to be admitted to hospitals with low survival rates (23% vs. 15%, p<.001).
Conclusion
Hospitals with large black patient populations had worse cardiac arrest outcomes than predominantly white hospitals, and blacks were more likely to be admitted to these high mortality hospitals. Understanding these differences in survival outcomes may uncover the causes for these disparities and lead to improved survival for all cardiac arrest victims.
Differences in survival from out-of-hospital cardiac arrest between blacks and whites have been previously described but the mechanisms generating these disparities remain uncertain.1–4 Previous studies have identified that pre-hospital factors such as bystander cardiopulmonary resuscitation (CPR), initial rhythm, whether the event was witnessed, and incident location may contribute to racial differences in survival from cardiac arrest.2–6 However, these studies have not accounted for the role of hospital factors after initial resuscitation and intensive care unit (ICU) admission.
These hospital factors may be important. Blacks with cardiovascular disease are more likely to receive care at hospitals with worse risk-adjusted surgical outcomes, longer times to reperfusion therapy, and fewer evidenced-based technologies.7–11 These differences are associated with worse outcomes. Skinner and colleagues demonstrated that hospital racial composition is itself an important predictor of AMI outcome: blacks were more likely to be treated at hospitals with higher proportions of black patients and, those hospitals had higher mortality.12
The same circumstances may be relevant in cardiac arrest as an estimated 80% of cardiac arrests occur at home and current practice is for patients in cardiac arrest to go to the closest hospital.13 Since blacks in the US are more likely to live in racially homogenous neighborhoods and therefore receive care at hospitals which serve these neighborhoods, 14–18 racial differences in post arrest survival may be related to the racial composition of hospitals where blacks are most likely to be admitted. Racial composition is likely a marker of other hospital processes of care which could represent important areas for intervention and improvement.
Our study’s goal was to determine whether the racial composition of US hospitals accounts for racial differences in survival rates for patients hospitalized after out-of-hospital cardiac arrest. We also evaluated if blacks and whites were admitted to hospitals with different survival rates from cardiac arrest to further characterize racial differences in admission patterns.
Methods
Data sources and study population
We examined all fee-for-service Medicare beneficiaries hospitalized for cardiac arrest or ventricular fibrillation (VF) from January 2000 to September 2007. This time frame represents 118,613,902 total admissions for all causes across 4,293 hospitals. To establish a cohort of patients with presumed out-of-hospital cardiac arrest who were resuscitated and admitted to the hospital, we used Medicare Provider Analysis and Review (MedPAR) data to identify individuals with an admission diagnosis of cardiac arrest or VF, (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 427.4, 427.41, and 427.5) admitted from the emergency department to the ICU. Patients were included if identified in the Medicare enrollment database as black or white (considered a valid measure of race as it is self reported at the time of Medicare enrollment).19
To increase the likelihood that the admission diagnosis of VF represented an actual admission for cardiac arrest rather than a non-urgent admission for arrhythmia evaluation, we excluded patients with a procedure, secondary diagnosis or diagnosis related group (DRG) code related to implantable cardioverter defibrillator (ICD) replacement or device check. We also excluded patients discharged alive to home within one day of admission, as this would be highly unlikely in the event of an actual cardiac arrest.
To further support the admission diagnosis of cardiac arrest with consistent inpatient documentation, we included in the cohort only those patients who had a procedure, hospital diagnosis, or DRG code of cardiac arrest, VF, CPR, mechanical ventilation, or heart countershock.
Patient Characteristics
We used the Medicare denominator file to ascertain race, age, and gender (from birth records used for Social Security files). Race and gender were tested as an interaction term in the model and found to not be significant so these variables were entered separately.
We included only patients aged 66 and over to insure that at least one year of data was available before the index hospitalization for cardiac arrest to assess pre-arrest comorbidities. We identified comorbidities, by linking the index MedPAR file with all Medicare records for outpatient visits and inpatient hospitalizations in the 365 days preceding the index hospitalization for cardiac arrest. Comorbid conditions in our model included myocardial infarction, congestive heart failure (CHF), prior arrhythmia, valvular disease, hypertension (HTN), diabetes, and renal disease identified by the coding scheme described by Elixhauser et al. to group diagnosis codes.20 Coronary artery disease was classified by ICD-9-CM codes 410–414, 429.2, and V45.81. We generated a variable “no prior diagnoses” to identify patients with no outpatient or inpatient claims in the year preceding their cardiac arrest.
Diagnoses during the index hospitalization which could be related to the etiology of the cardiac arrest were entered in the model and included concurrent: AMI (410.00–410.92), acute coronary syndrome (412, 411.81, 411.89), pulmonary embolism (415.11, 415.19), sepsis/shock (771.81, 785.50–785.59, hyperkalemia (276.7), and cerebrovascular accident (430–436, 432.0–435.9, 433.00–434.91).
Hospital Variables
We used American Hospital Association annual survey data (2000–2007) and Medicare claims data to identify hospital variables that could account for differences in survival outcomes across racial groups or be correlated with hospital racial composition. These included: academic status, urban location, US Census region, hospital ownership and hospital bed count-divided into tertiles based on the sample distribution. Hospitals (n=526) with incomplete data for variables included in the model were excluded. As a proxy for hospital economic status, we used the median household income reported for Medicare fee-for service beneficiaries admitted to the index hospital per year, and categorized hospitals in tertiles.
We used MedPAR data claims from all hospital discharges for each year to determine hospital racial composition, reflecting the proportion of claims from black patients treated annually for cardiovascular conditions (i.e. DRG in major diagnosis category 5). We then divided the hospitals in our cardiac arrest cohort into quintiles along this dimension. The first quintile represented hospitals whose overall admissions included the fewest black patients and the highest quintile represented hospitals with the highest percentage of admissions for black patients. To further identify the types of hospitals that black and white patients with cardiac arrest were admitted to, we used our cardiac arrest cohort to divided facilities into quintiles reflecting the survival rate per hospital.
Statistical Analyses
Summary statistics are reported by racial group for patient factors and by quintile for hospital level factors. Statistical significance across groups was determined using chi-squared tests for nominal data, t tests for interval data, and Kruskal-Wallis tests for non parametric median data.
We compared unadjusted probability estimates for survival outcomes by race using the chi-square test. To evaluate if blacks and whites were more or less likely to be admitted to hospitals with differing cardiac arrest survival rates we used a non-parametric test of trend for the ranks of across ordered groups.
We created a multivariable logistic regression to adjust for variables hypothesized to explain the relationship between race and survival to hospital discharge and we used a clustered variance estimator to control for clustering of data by hospital. Covariates (for post-arrest patients admitted to the ICU) in the regression model included patient level factors (age, comorbidities, inpatient concurrent conditions) and hospital level factors (each facility’s racial composition, volume, ownership (i.e., for-profit, non-for-profit, government), teaching status, location, income, urban status, and cardiovascular procedure capability [e.g. presences of onsite interventional cardiology]). We included interactions between race and the percentage of black patients per hospital as categorized in quintiles. The primary outcome variable was survival to hospital discharge.
We examined risk-adjusted mortality across quintiles (to determine if blacks and whites had different survival outcomes at different hospitals) and within quintiles to determine if blacks and whites had different survival outcomes at the same hospital). To improve the interpretation of logistic regression results, rather than presenting odds ratios we presented probabilities reflecting unit changes in covariates of interest (e.g. black, hospital race quintile) with all other covariates fixed at their mean.
To further characterize the types of hospitals that black and white patients with cardiac arrest were admitted to, we also used the cardiac arrest cohort to divide hospitals into quintiles by the survival rate per facility. To determine the adjusted probability of survival at these high and low survival facilities, interactions between race and the percentage of survivors per hospital were also categorized in quintiles and included in a multivariate model to assess racial differences within hospitals.
All statistical analyses were performed with Stata version 10, College Station, Texas. The institutional review board of the University of Pennsylvania approved this study. This research was supported by funding from the Robert Wood Johnson Foundation Clinical Scholars program at the University of Pennsylvania (Merchant). This research was also supported by an unrestricted grant from the Institute for Health Technology Studies (Washington, DC), as well as grant 1-R01-HL086919 from the National Heart, Lung, and Blood Institute (Groeneveld). The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
Results
We identified 68,115 admissions for cardiac arrest (from the emergency department to the ICU) to 3,767 hospitals over an approximately 7 year period. Of our sample, 88% (n=60,173) of patients were white and 12% (n=7,942) were black. White patients were older, more likely to be male, and more likely to have a presenting rhythm of VF. Black patients had more comorbidities. (Table 1).
Table I.
Characteristics of patients with cardiac arrest by race (n=68,115)
| White (n=60,173) |
Black (n=7,942) |
p value | |
|---|---|---|---|
| Patient Characteristics | |||
| Age (mean) ± standard deviation | 78.1± 7.3 | 77.4± 7.8 | p=.01 |
| 66–70 | 18% | 23% | p<.001 |
| 71–75 | 22% | 22% | p=.01 |
| 76–80 | 23% | 22% | p<.001 |
| 81–85 | 17% | 13% | p<.001 |
| >85 | 20% | 19% | p<.001 |
| Gender, male | 56% | 39% | p<.001 |
| Admission diagnosis: | |||
| Ventricular fibrillation (42741) | 12% | 8% | p<.001 |
| Cardiac arrest (4275) | 88% | 92% | p<.001 |
| Length of stay: (days) | |||
| Hospital | 5.3±7 | 4.7±7 | p<.01 |
| Intensive care unit | 2.7±75 | 2.4±74 | p<.01 |
| Pre-arrest comorbidities: | |||
| Hypertension | 30% | 42% | p<.001 |
| Congestive heart failure | 25% | 31% | p<.001 |
| Diabetes | 16% | 25% | p<.001 |
| Arrhythmia | 21% | 7% | p<.001 |
| Coronary artery disease | 12% | 18% | p<.001 |
| Renal disease | 7% | 13% | p<.001 |
| Valvular disease | 10% | 9% | p<.001 |
| Myocardial infarction | 6% | 6% | p=.70 |
| No prior diagnoses | 33% | 27% | p<.001 |
| In-hospital concurrent conditions: | |||
| Acute myocardial infarction | 33% | 27% | p<.001 |
| Sepsis/shock | 12% | 14% | p<.001 |
| Acute coronary syndrome | 12% | 6% | p<.001 |
| Hyperkalemia | 7% | 10% | p<.001 |
| Cerebral vascular accident | 5% | 6% | p<.001 |
| Pulmonary embolism | 1% | 2% | p<.001 |
In the analysis of hospital racial composition, overall hospital admissions by race varied from <1% black patients in the lowest quintile to 13%–93% black patients in the highest quintile. Blacks were more likely (63% vs. 15%, p<.001) to be admitted to hospitals with higher proportions of black patients (5th quintile) which represented 24% of US hospitals.
Hospitals with the largest numbers of black patients were more likely to be urban, located in the south, higher volume, academic, and to provide care for patients of lower income (Table 2).
Table II.
Hospital characteristics by racial composition-black patients/hospital (quintile)
| Lowest quintile (0-<1%) |
2nd (1–3%) |
3rd (4–6%) |
4th (7–12%) |
5th (13–93%) |
p | |
|---|---|---|---|---|---|---|
| white patients (n) | 13,281 | 13,350 | 12,817 | 11,969 | 8,756 | |
| black patients (n) | 98 | 305 | 731 | 1,771 | 5,037 | |
| Hospital size * | ||||||
| Large volume | 10% | 21% | 31% | 35% | 31% | P<.001 |
| Hospital type: | ||||||
| Proprietary | 11% | 19% | 18% | 17% | 15% | p<.001 |
| Non-profit | 78% | 73% | 74% | 70% | 64% | p<.001 |
| Government | 11% | 7% | 8% | 13% | 21% | p<.001 |
| Academic | 5% | 9% | 17% | 27% | 25% | p<.001 |
| Urban | 25% | 51% | 51% | 59% | 60% | p<.001 |
| High income† | 29% | 46% | 38% | 36% | 20% | p<.001 |
| Hospital geographic location: | ||||||
| Midwest | 37% | 27% | 26% | 21% | 20% | P<.001 |
| Northeast | 19% | 25% | 21% | 21% | 12% | P<.001 |
| South | 11% | 26% | 40% | 49% | 64% | P<.001 |
| West | 34% | 22% | 13% | 10% | 3% | P<.001 |
| Hospital procedure capabilities: | ||||||
| PCI | 72% | 86% | 91% | 91% | 88% | P<.001 |
| CABG | 41% | 54% | 61% | 63% | 57% | P<.001 |
| ICD | 49% | 64% | 69% | 71% | 65% | P<.001 |
Hospital volume divided into tertiles (large=>275 beds)
Income: median household income of Medicare fee-for service beneficiaries admitted to the index hospital per year in tertiles (high income ≥$45,000)
PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; ICD, Implantable cardioverter defibrillator
The unadjusted probability of survival to discharge was lower among blacks compared with whites (30% vs. 33%, p<0.001). Whites were also more likely to be discharged home (Table 3).
Table III.
Disposition of survivors at hospital discharge (n=21,600)
| White (n=19,297) |
Black (n=2,303) |
p value | |
|---|---|---|---|
| Home | 8% | 6% | p<.001 |
| Another hospital | 10% | 9% | p<.001 |
| Skilled nursing facility | 7% | 8% | p<.001 |
| Hospice | 2% | 2% | p=0.67 |
| Inpatient rehabilitation | 1% | 1% | p=0.81 |
| Discharged against medical advise | <1% | <1% | p=0.72 |
Hospital characterization by racial compositon
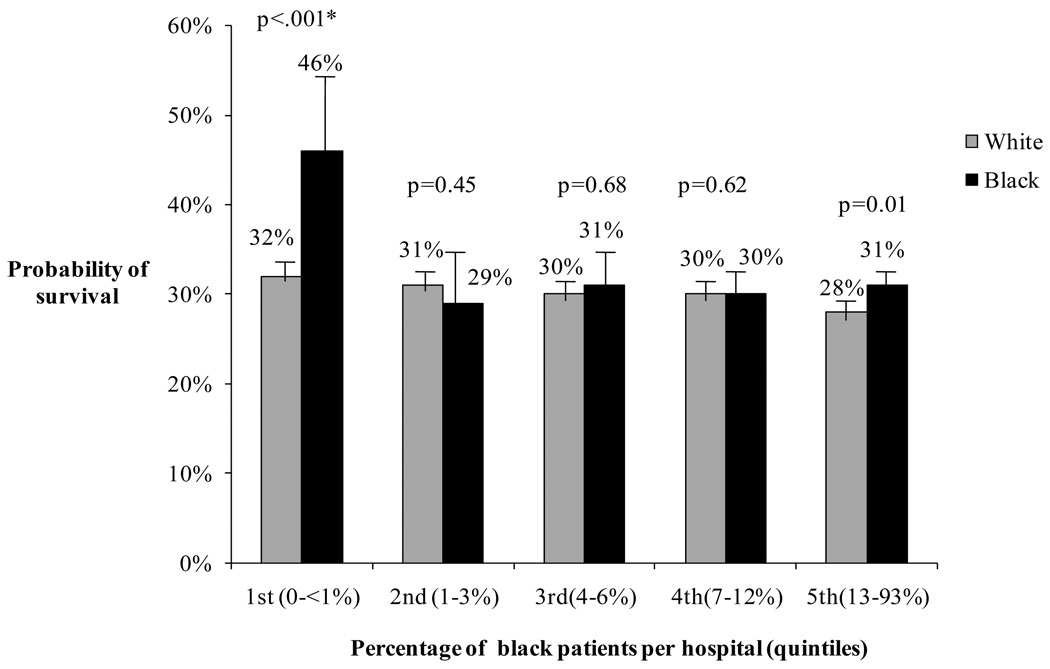
In multivariate analyses accounting for patient and hospital level factors, the racial composition of the hospital was significantly associated with survival outcomes in the quintiles with the lowest and highest percentages of black patients (Figure 1). Black patients had lower survival at hospitals with a higher proportion of black patients (5th quintile) compared with blacks receiving care at hospitals with a predominately white patient population (1st quintile,) (adjusted mean probability of survival 31%, [95% CI 29%–32%] vs. 46% [95% CI 36%–57%], p=.003).
Figure 1. Adjusted survival from cardiac arrest by race and hospital racial composition.
Controlling for patient (age, sex, comorbidites, inpatient concurrent diagnoses) and hospital factors (volume, ownership, teaching status, location, income, urban status, and cardiovascular procedure capability), survival by race is represented in each % black quintile. P values reflect within hospital comparisons by race. Across hospital (quintile 1 versus 5) adjusted survival was significant for blacks (p=.003) and whites (p=.006).
Similarly, white patients at hospitals with the largest numbers of black patients had a lower adjusted mean probability of survival compared with survival for white patients admitted to hospitals with primarily white patients (28% [95% CI 27%–30%] vs. 32% [95% CI 31%–35%], p=0.006).
The regression model had good discrimination (c-statistic=0.73) and calibration (p value for goodness of fit=0.37)
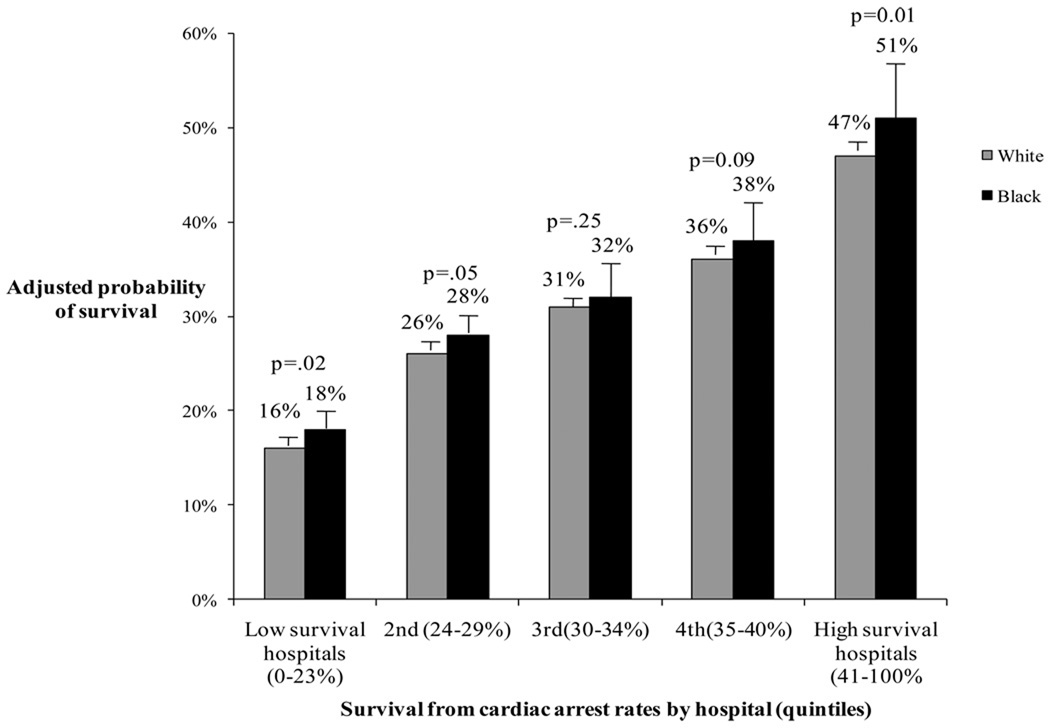
Hospital characterization by arrest survival rates
The adjusted rate of survival was better for blacks compared to whites within hospitals with the lowest survival and the highest survival (Figure 2). Black patients however, were more likely to be admitted to hospitals with worse survival, (23% vs. 15%, p <.001) and white patients were more likely to be admitted to hospitals with better survival (5th quintile vs. 1st quintile (21% vs. 19%, p<.001).
Figure 2. Adjusted survival for blacks and whites at hospitals with high and low survival rates from cardiac arrest.
Controlling for patient and hospital factors the adjusted probability of survival by race is represented in each quintile of hospital survival rate. P values reflect within hospital comparisons by race.
Discussion
This study has three main findings. First, we observed significantly better unadjusted survival from out-of-hospital cardiac arrest for whites compared to blacks. Second, these effects were almost entirely explained by the hospitals where patients were admitted. Blacks were much more likely to go to hospitals that had worse outcomes (for blacks and whites). Third, within groups of hospitals categorized by race percentage and the survival rate/hospital, the few “within-group” racial differences in outcomes favored survival for blacks. These three findings are consistent with a single story: hospitals vary in their ability to deliver care. Because of racial residential segregation, blacks are much more likely to be admitted to hospitals caring for largely black populations, and these hospitals generally have poorer cardiac arrest outcomes for both black and white patients. These results explain a troubling health disparity and suggest that hospital-level influences are a leading reason why there are racial differences in cardiac arrest outcomes. These data are unique in that they are derived from a large population-based cohort of nearly all patients over the age of 66 admitted to nearly all acute care hospitals in the United States with an out-of-hospital cardiac arrest over a seven year period.
The racial composition of the hospital (as a marker of ways in which hospitals may be deficient in some areas of quality and have worse outcomes) is a neglected factor in previous studies of cardiac arrest outcomes. Prior work has primarily focused on the role of pre-hospital factors as predictors of differences in outcomes.1–3, 5, 6 Controlling for these and other factors related to the circumstances of out-of-hospital arrest has not entirely explained racial differences in survival-suggesting a role for hospital factors.3 Data regarding racial differences in in-hospital arrest outcomes also suggest a role for hospital-level influences and processes of care.21, 22 Hospital racial composition represents a potentially important factor to consider as blacks and whites tend to live in racially homogenous areas and receive care at different types of hospitals. Emergent conditions such as cardiac arrest are even more likely than non-urgent conditions to reflect the segregation of the population, since most arrests occur at home and patients tend to be treated at the nearest hospital.
For both white and black patients in our cohort, survival to discharge was lower in hospitals with higher proportions of black patients. It is increasingly apparent that hospitals vary non-randomly in their cardiac arrest outcomes23, 24 and the mechanisms explaining these differences are likely influenced by both measurable and unmeasurable factors.
Variability in treatment intensity of all patients with cardiovascular conditions may be an important contributing factor for observed differences in survival by hospital racial composition.25–30 Surprisingly, we found that hospitals which provided care for higher proportions of black patients were more likely to have the capability to provide treatments like PCI. Capability may not equate to actual utilization in the post-arrest setting however, and prior studies have demonstrated lower rates of revascularization, surgical treatment of cardiac disease, and ICD placement in blacks compared with whites.28, 29, 31–35 These differences have also been elucidated even when controlling for the hospital where patients were admitted.36 A better understanding of how hospital level access and utilization of post-resuscitation therapies influence survival outcomes may help to direct next steps for improving health outcomes and help to determine if there is a case for regionalization of post-arrest care.37, 38
Differences in physician and nursing quality, ancillary support, patient/family preferences regarding end of life care, and other unmeasured domains could account for some of the observed differences.37, 39–41 Improved tools for measuring these factors are needed to better understand differences in hospital level processes of care. The emphasis of our work was not to simply account for all of the factors that influence disparities (unadjusted survival rates prove they exist) but rather to better understand some of the mechanisms driving these differences to help focus possible intervention strategies.
Another area of focus for improving overall arrest rates is in the pre-hospital arena. Notably, we identified a higher adjusted survival rates for black patients in our cohort in the lowest and highest quintiles. One possible explanation for this finding is that consistent with prior reports documenting fewer resuscitation resources in black neighborhoods-black patients with OHCA are less likely to survive arrest pre-hospital, be transferred to an emergency room and then resuscitated and admitted to an ICU.1, 2 The cohort of black patients in our study (resuscitated and admitted to the ICU) may have a favorable survival bias which could explain the higher adjusted survival rates for blacks after accounting for hospital effects.
Limitations
There are several limitations of our findings. We reported racial differences in cardiac arrest survival in a patient population aged 66 and older. Due to significant racial and gender differences in life expectancy, our reported differences in survival outcomes may not be generalizable to a younger patient population. In addition, we developed inclusion and exclusion criteria for claims data to support the likelihood of identifying actual out-of-hospital cardiac arrest, but due to the limitations of claims data we were unable to validate these criteria with actual emergency medical system or emergency department documentation. It is unlikely however that we excluded or included cases in a manner that would have created racial bias.
Our cohort was limited to patients resuscitated from cardiac arrest and subsequently hospitalized, so our findings do not account for differences in initial incidence, attempted resuscitation, initial rhythm etc. which could exist between black and white patients.1, 2, 4, 5 Our intent however was to study a hospitalized population that would be likely to be impacted by differences in hospital factors.
We may have omitted confounding factors related to hospitals that serve large numbers of blacks such as hospital financial status, accessibility of specialist physicians, or general quality of carer.39 Hospital differences in discharge policies may have also impacted our findings. Similarly there may have been unmeasured confounding patient level factors (comorbidities, inpatient diagnoses) that were not included in our model which could account for unexplained variability in outcomes and bias our findings. Despite our limitations, we were however able to include a wide variety of patient and hospital level factors in our analysis.
Conclusion
Racial disparities in hospital survival from cardiac arrest exist but were reduced when accounting for hospital racial composition. Improving care at high mortality hospitals, which disproportionately provide care for black patients, has the potential to improve cardiac arrest survival outcomes for both black and white patients.
Acknowledgements
We thank Joshua P. Metlay, MD, PhD, Katrina Armstrong MD, MSCE, and David A. Asch MD, MBA (Division of General Internal Medicine, University of Pennsylvania, Philadelphia) for critical review of the manuscript. No compensation was provided to these consultants.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
Merchant and Yang: no conflicts of interest to disclose
Becker: Speaker honoraria/ consultant fees: Philips Healthcare, Seattle, WA.
Institutional grant/research support: Philips Healthcare, Seattle, WA; Laerdal Medical, Stavanger, Norway; NIH, Bethesda, MD; Cardiac Science, Bothell, Washington
Groeneveld: Federal employee, No conflicts of interest to disclose
References
- 1.Becker LB, Han BH, Meyer PM, et al. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project. N Engl J Med. 1993;329:600–606. doi: 10.1056/NEJM199308263290902. [DOI] [PubMed] [Google Scholar]
- 2.Iwashyna TJ, Christakis NA, Becker LB. Neighborhoods matter: a population-based study of provision of cardiopulmonary resuscitation. Ann Emerg Med. 1999;34:459–468. doi: 10.1016/s0196-0644(99)80047-x. [DOI] [PubMed] [Google Scholar]
- 3.Galea S, Blaney S, Nandi A, et al. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007;166:534–543. doi: 10.1093/aje/kwm102. [DOI] [PubMed] [Google Scholar]
- 4.Cowie MR, Fahrenbruch CE, Cobb LA, Hallstrom AP. Out-of-hospital cardiac arrest: racial differences in outcome in Seattle. Am J Public Health. 1993;83:955–959. doi: 10.2105/ajph.83.7.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brookoff D, Kellermann AL, Hackman BB, Somes G, Dobyns P. Do blacks get bystander cardiopulmonary resuscitation as often as whites? Ann Emerg Med. 1994;24:1147–1150. doi: 10.1016/s0196-0644(94)70246-2. [DOI] [PubMed] [Google Scholar]
- 6.Chu K, Swor R, Jackson R, et al. Race and survival after out-of-hospital cardiac arrest in a suburban community. Ann Emerg Med. 1998;31:478–482. doi: 10.1016/s0196-0644(98)70257-4. [DOI] [PubMed] [Google Scholar]
- 7.Groeneveld PW, Heidenreich PA, Garber AM. Racial disparity in cardiac procedures and mortality among long-term survivors of cardiac arrest. Circulation. 2003;108:286–291. doi: 10.1161/01.CIR.0000079164.95019.5A. [DOI] [PubMed] [Google Scholar]
- 8.Groeneveld PW, Laufer SB, Garber AM. Technology diffusion, hospital variation, and racial disparities among elderly Medicare beneficiaries: 1989–2000. Med Care. 2005;43:320–329. doi: 10.1097/01.mlr.0000156849.15166.ec. [DOI] [PubMed] [Google Scholar]
- 9.Bradley EH, Herrin J, Wang Y, et al. Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. JAMA. 2004;292:1563–1572. doi: 10.1001/jama.292.13.1563. [DOI] [PubMed] [Google Scholar]
- 10.Konety SH, Vaughan Sarrazin MS, Rosenthal GE. Patient and hospital differences underlying racial variation in outcomes after coronary artery bypass graft surgery. Circulation. 2005;111:1210–1216. doi: 10.1161/01.CIR.0000157728.49918.9F. [DOI] [PubMed] [Google Scholar]
- 11.Rothenberg BM, Pearson T, Zwanziger J, Mukamel D. Explaining disparities in access to high-quality cardiac surgeons. Ann Thorac Surg. 2004;78:18–24. doi: 10.1016/j.athoracsur.2004.01.021. discussion -5. [DOI] [PubMed] [Google Scholar]
- 12.Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112:2634–2641. doi: 10.1161/CIRCULATIONAHA.105.543231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jackson RE, Swor RA. Who gets bystander cardiopulmonary resuscitation in a witnessed arrest? Acad Emerg Med. 1997;4:540–544. doi: 10.1111/j.1553-2712.1997.tb03574.x. [DOI] [PubMed] [Google Scholar]
- 14.Landrine H, Corral I. Separate and unequal: residential segregation and black health disparities. Ethn Dis. 2009;19:179–184. [PubMed] [Google Scholar]
- 15.Hayanga AJ, Kaiser HE, Sinha R, Berenholtz SM, Makary M, Chang D. Residential segregation and access to surgical care by minority populations in US counties. J Am Coll Surg. 2009;208:1017–1022. doi: 10.1016/j.jamcollsurg.2009.01.047. [DOI] [PubMed] [Google Scholar]
- 16.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haas JS, Phillips KA, Sonneborn D, et al. Variation in access to health care for different racial/ethnic groups by the racial/ethnic composition of an individual's county of residence. Med Care. 2004;42:707–714. doi: 10.1097/01.mlr.0000129906.95881.83. [DOI] [PubMed] [Google Scholar]
- 18.Blustein J, Weitzman BC. Access to hospitals with high-technology cardiac services: how is race important? Am J Public Health. 1995;85:345–351. doi: 10.2105/ajph.85.3.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arday SL, Arday DR, Monroe S, Zhang J. HCFA's racial and ethnic data: current accuracy and recent improvements. Health Care Financ Rev. 2000;21:107–116. [PMC free article] [PubMed] [Google Scholar]
- 20.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Chan PS, Nichol G, Krumholz HM, et al. Racial differences in survival after in-hospital cardiac arrest. JAMA. 2009;302:1195–1201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009;361:22–31. doi: 10.1056/NEJMoa0810245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carr BG, Kahn JM, Merchant RM, Kramer AA, Neumar RW. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009;80:30–34. doi: 10.1016/j.resuscitation.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Carr BG, Goyal M, Band RA, et al. A national analysis of the relationship between hospital factors and post-cardiac arrest mortality. Intensive Care Med. 2009;35:505–511. doi: 10.1007/s00134-008-1335-x. [DOI] [PubMed] [Google Scholar]
- 25.Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA. 1993;269:2642–2646. [PubMed] [Google Scholar]
- 26.Kaul P, Lytle BL, Spertus JA, DeLong ER, Peterson ED. Influence of racial disparities in procedure use on functional status outcomes among patients with coronary artery disease. Circulation. 2005;111:1284–1290. doi: 10.1161/01.CIR.0000157731.66268.E1. [DOI] [PubMed] [Google Scholar]
- 27.Schwartz LM, Woloshin S, Welch HG. Misunderstandings about the effects of race and sex on physicians' referrals for cardiac catheterization. N Engl J Med. 1999;341:279–283. doi: 10.1056/NEJM199907223410411. discussion 86-7. [DOI] [PubMed] [Google Scholar]
- 28.Castellanos LR, Normand SL, Ayanian JZ. Racial and ethnic disparities in access to higher and lower quality cardiac surgeons for coronary artery bypass grafting. Am J Cardiol. 2009;103:1682–1686. doi: 10.1016/j.amjcard.2009.02.019. [DOI] [PubMed] [Google Scholar]
- 29.Bao Y, Kamble S. Geographical distribution of surgical capabilities and disparities in the use of high-volume providers: the case of coronary artery bypass graft. Med Care. 2009;47:794–802. doi: 10.1097/MLR.0b013e31819a594d. [DOI] [PubMed] [Google Scholar]
- 30.Basu J, Mobley LR. Trends in racial disparities among the elderly for selected procedures. Med Care Res Rev. 2008;65:617–637. doi: 10.1177/1077558708318284. [DOI] [PubMed] [Google Scholar]
- 31.Groeneveld PW, Heidenreich PA, Garber AM. Trends in implantable cardioverter-defibrillator racial disparity: the importance of geography. J Am Coll Cardiol. 2005;45:72–78. doi: 10.1016/j.jacc.2004.07.061. [DOI] [PubMed] [Google Scholar]
- 32.Brown CP, Ross L, Lopez I, Thornton A, Kiros GE. Disparities in the receipt of cardiac revascularization procedures between blacks and whites: an analysis of secular trends. Ethn Dis. 2008;18 S2-112-7. [PMC free article] [PubMed] [Google Scholar]
- 33.Gaglia MA, Jr, Steinberg DH, Pinto Slottow TL, et al. Racial disparities in outcomes following percutaneous coronary intervention with drug-eluting stents. Am J Cardiol. 2009;103:653–658. doi: 10.1016/j.amjcard.2008.10.043. [DOI] [PubMed] [Google Scholar]
- 34.Epstein AM, Weissman JS, Schneider EC, Gatsonis C, Leape LL, Piana RN. Race and gender disparities in rates of cardiac revascularization: do they reflect appropriate use of procedures or problems in quality of care? Med Care. 2003;41:1240–1255. doi: 10.1097/01.MLR.0000093423.38746.8C. [DOI] [PubMed] [Google Scholar]
- 35.Chan PS, Birkmeyer JD, Krumholz HM, Spertus JA, Nallamothu BK. Racial and gender trends in the use of implantable cardioverter-defibrillators among Medicare beneficiaries between 1997 and 2003. Congest Heart Fail. 2009;15:51–57. doi: 10.1111/j.1751-7133.2009.00060.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barnato AE, Lucas FL, Staiger D, Wennberg DE, Chandra A. Hospital-level racial disparities in acute myocardial infarction treatment and outcomes. Med Care. 2005;43:308–319. doi: 10.1097/01.mlr.0000156848.62086.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Spaite DW, Bobrow BJ, Vadeboncoeur TF, et al. The impact of prehospital transport interval on survival in out-of-hospital cardiac arrest: implications for regionalization of post-resuscitation care. Resuscitation. 2008;79:61–66. doi: 10.1016/j.resuscitation.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 38.Spaite DW, Stiell IG, Bobrow BJ, et al. Effect of transport interval on out-of-hospital cardiac arrest survival in the OPALS study: implications for triaging patients to specialized cardiac arrest centers. Ann Emerg Med. 2009;54:248–255. doi: 10.1016/j.annemergmed.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 39.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 40.Gemson DH, Elinson J, Messeri P. Differences in physician prevention practice patterns for white and minority patients. J Community Health. 1988;13:53–64. doi: 10.1007/BF01321480. [DOI] [PubMed] [Google Scholar]
- 41.Reynolds KS, Hanson LC, Henderson M, Steinhauser KE. End-of-life care in nursing home settings: do race or age matter? Palliat Support Care. 2008;6:21–27. doi: 10.1017/S1478951508000047. [DOI] [PubMed] [Google Scholar]