Abstract
Introduction/ Methods
To assess whether revised electrocardiographic (ECG) criteria improve Emergency Department identification of patients with acute myocardial infarction (MI) or unstable angina (UA) and predict outcome, we studied 120 patients with a nondiagnostic initial ECG by prior criteria. ECGs were read in a blinded fashion months apart with standard and then revised criteria, and analyzed by Chi square and logistic regression analysis.
Results
In 12 subjects (10%), the initial ECG was now interpreted as diagnostic of ischemia. Eleven (92%) had an MI, 1 had UA (8%), and none had a noncardiac diagnosis. Ischemic ECG changes were strongly associated with MI or UA (p=0.003). At 1 year follow-up, ECG changes diagnostic of ischemia were associated with a trend toward higher mortality (25% vs. 7%, p=0.07) but after adjustment for clinical factors, ECG changes were not an independent predictor of 1-year mortality.
Conclusions
Revision of the ECG criteria for ischemia was associated with enhanced diagnostic performance and identified a subset of patients at higher risk.
Introduction
Electrocardiographic (ECG) criteria for acute myocardial ischemia that may lead to myocardial infarction (MI) have recently been revised, in part to address gender differences (1). Specifically, the following features are now considered evidence of ischemia in the absence of left ventricular hypertrophy (LVH) or left bundle branch block (LBBB).
ST elevation at the J-point in 2 contiguous leads with the cutoff points:≥0.2mV in men or ≥0.15mV in women in leads V2-V3 and/or ≥0.1mV in other leads
Horizontal or down-sloping ST depression ≥0.05mV in 2 contiguous leads; and/or T inversion ≥0.1mV in 2 contiguous leads with prominent R waves or R/S ratio >1
These new criteria differed from the prior standard criteria (2) by: a) reducing the cutoff point for ST elevation in lead V1 from ≥0.2 mV to ≥0.1mV in both men and women, b) lowering the threshold for ST elevation in women in leads V2-V3 to ≥0.15 mV, and c) lowering the cutoff point for ST depression (0.05 mV) that was previously assumed to be 0.1 mV.
The goal of the revised criteria was to improve the sensitivity of the initial ECG for acute myocardial ischemia and infarction, especially in women. However, the diagnostic performance of these revised criteria is unknown. Therefore, to assess the incremental value of these new ECG criteria in the diagnosis of acute coronary syndrome (ACS), we studied a cohort of patients presenting to the Emergency Department (ED) with symptoms of possible ischemia but a nondiagnostic initial ECG by the older standard criteria (2).
Methods
Data for this analysis were drawn from the IMMEDIATE AIM study (Ischemia Monitoring & Mapping in the Emergency Department In Appropriate Triage & Evaluation of Acute Ischemic Myocardium), a prospective clinical trial funded by NIH (RO1HL69753) which sought to improve noninvasive ECG diagnosis of patients who present to the ED with ACS (3–5). Patients (n=1308) were enrolled in the study from 2002–04 and underwent one-year clinical follow-up, completed in December, 2005.
Patients presenting to the ED with chest pain or anginal equivalent at the University of California, San Francisco Medical Center Monday through Friday between 7 am and 7 pm, were approached for enrollment in the IMMEDIATE AIM Study. Patients with left bundle branch block or ventricularly paced rhythms were excluded. Data on clinical factors, initial and serial 12-lead ECGs and continuous Holter monitoring for arrhythmia and ST segment deviation were collected. To avoid delay, institutional review board approval was granted for application of Holter monitors with an initial verbal assent followed by informed written consent when the patient was stable.
For this analysis, we studied 154 patients presenting to the Emergency Department (ED) with symptoms of possible ischemia but a nondiagnostic initial ECG. We subsequently excluded patients with electrocardiographic evidence of left ventricular hypertrophy (LVH), resulting in a final cohort of 120 patients. Final diagnostic categories identified from subjects’ discharge records included acute MI (n=37), unstable angina (UA) (n=36) and noncardiac chest pain (n=47). The 3 groups were similar in age and gender. MI was diagnosed in the presence of chest pain or anginal equivalent associated with significantly elevated troponin levels as outlined in the American College of Cardiology consensus document on measuring outcomes in patients with acute coronary syndromes (6). Unstable angina was defined as a clinical history consistent with a diagnosis of unstable angina, in whom ischemia was confirmed by presence of ST changes on the initial ECG or in association with recurrent rest pain, or presence of small elevations of troponin that do not meet infarction criteria. In addition, in the unstable angina subset, 19 of 36 patients underwent angiography on clinical grounds, and 17 of 19 had evidence of angiographic epicardial coronary artery disease.
ECG Procedures/Analysis
Standard 12-lead electrocardiograms were obtained for clinical purposes as ordered by the treating physician. In addition, for the study, trained research nurses applied Holter monitors as soon as possible after ED arrival, using the Mason-Likar lead configuration (7). They recorded an initial 12-lead Holter ECG, supervised the Holter recordings over the 24 hour period, and down-loaded stored 12-lead Holter ECGs for subsequent analysis. All 12-lead Holter ECGs were analyzed by a single board-certified cardiologist (KEF) using the H-Scribe System (Mortara Instruments, Milwaukee, WI). Clearly defined operational definitions were used after an initial period where two experts (BD and KEF) reached consensus on their application. ECGs were read in a blinded fashion several months apart, using first the standard criteria and then the revised criteria. This analysis utilized only data from the initial 12-lead Holter ECG and did not utilize continuous Holter data. In the older criteria, myocardial ischemia was defined as: a) ST elevation at the J point of ≥ 0.2 mV in leads V1 - V3 or ≥ 0.1 mV in all other leads, b) ST depression at the J point of ≥ 0.1 mV with horizontal or down-sloping ST segments and, c) inverted T waves of ≥ 0.1 mV in depth. For all criteria (ST elevation, depression or T wave inversion), the changes had to be present in 2 contiguous leads. Limb lead contiguity was considered the following sequence: aVL, I, minus (inverted) aVR, II, aVF, and III. Use of minus aVR meant that ST elevation in standard aVR counted as ST depression in minus aVR and vice versa. The initial Holter ECG was deemed diagnostic of ischemia if it met these criteria in the absence of confounders such as ECG evidence of pericarditis or early repolarization.
Follow-up Data
Trained research nurses collected data on one-year mortality as well as ED visits and hospital admissions from telephone calls to subjects, hospital and clinic electronic records, and a public internet-based mortality database (8). One-year follow-up was available for 90% of subjects in this analysis.
Statistical Analysis
All analyses were conducted in SAS statistical software (Version 8, Cary, North Carolina). Baseline characteristics for the cohort were identified using PROC FREQ and PROC UNIVARIATE. Two by three tables and logistic regression (PROC LOG) were used to assess whether new diagnostic criteria for ischemia heightened ability to predict the final diagnosis, except when the presence of zero cells prevented the regression analysis. Chi square statistical analysis was used to determine whether one-year mortality was different between those with and without ECG evidence of ischemia by the revised criteria. Finally, logistic regression was used to gauge the ability of ischemic changes by the revised criteria to predict 1 year mortality, hospital admissions and Emergency Department visits and, if so, whether these changes remained independent predictors of outcome after adjustment for clinical factors.
Results
Baseline characteristics
Average age was approximately 71 years, with a slight male predominance (Table 1). Hypertension was common and approximately one third of patients had a history of diabetes. Fourteen to sixteen percent of the cohort smoked, depending on diagnostic group. A prior history of CAD was significantly more common in those with a final diagnosis of UA (83%), as compared with those with MI (38%) or noncardiac chest pain (36%).
Table 1.
Baseline characteristics of the cohort
| Variable | MI (n=37) | UA (n=36) | Noncardiac CP (n=47) |
|---|---|---|---|
| Age (+/− s.d.) | 70.4 +/−16.2 | 69.7 +/− 12.8 | 71.5 +/− 9.8 |
| Male sex | 19 (51%) | 17 (47%) | 22 (47%) |
| Smoker | 6 (16%) | 5 (14%) | 7 (15%) |
| Diabetes | 14 (38%) | 16 (44%) | 11 (23%) |
| Hypertension | 29 (78%) | 30 (83%) | 36 (77%) |
| History of CAD* | 14 (38%) | 30 (83%) | 17 (36%) |
p<0.0001; all other results p=NS
Effect of revised criteria on diagnosis
In 12 subjects (10%), the initial nondiagnostic ECG was now read as diagnostic of ischemia using the revised criteria (Fig. 1). In most cases (83%), this was because ST depression that had not met previous criteria of 1 mm in 2 contiguous leads reached revised criteria of 0.5 mm in 2 contiguous leads. Five of the 12 subjects in whom the ECG was now diagnostic (42%) were women.
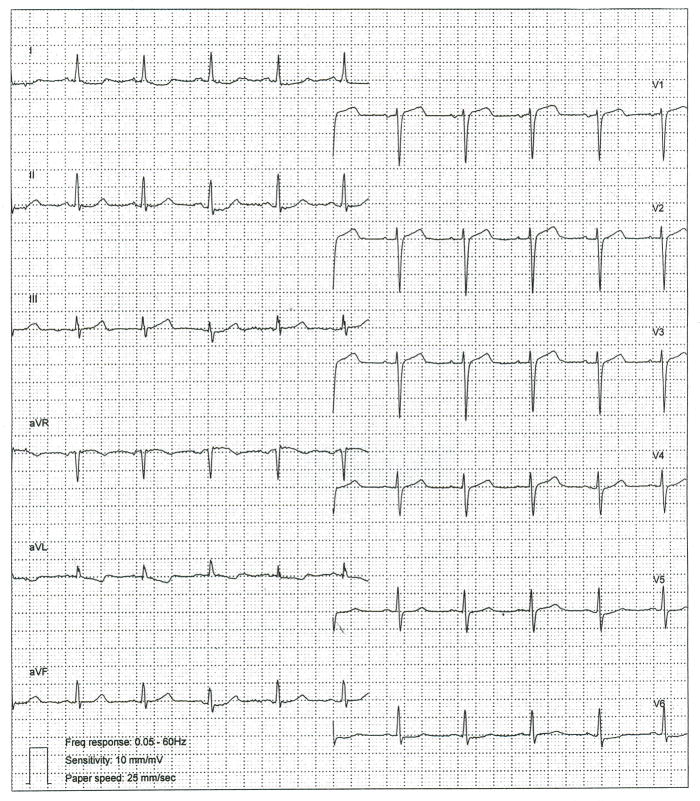
Figure 1.
Impact of Revised ECG criteria: Initial Holter 12–lead electrocardiogram from a female subject showing diffuse, mild ST depression that now exceeds the revised threshold of 0.05mV in two contiguous leads.
All twelve (100%) of these subjects left the hospital with a final diagnosis of acute coronary syndrome (11 with MI [92%], 1 with UA [8%]) and none were diagnosed with noncardiac chest pain (Table 2). Electrocardiograms diagnostic of ischemia were strongly associated with a final diagnosis of MI or UA (16% vs. 0%, p=0.003). Electrocardiograms diagnostic for ischemia were also strongly associated with MI itself (30% vs. 0%, p<0.001).
Table 2.
Relation of final diagnosis to new universal criteria for myocardial infarction in 120 patients with non-diagnostic initial ECG by older criteria
| ECG not diagnostic of ischemia by either older or new criteria | ECG diagnostic of ischemia by new revised criteria* | |
|---|---|---|
| Myocardial Infarction (n=37) | 26 (70%) | 11 (30%) |
| Unstable Angina (n=36) | 35 (97%) | 1 (3%) |
| Noncardiac chest pain (n=47) | 47 (100%) | 0 (0%) |
by revised ESC/ACCF/AHA/WHF ECG criteria
Effects of Revised Criteria on Outcomes
At follow-up, 8 (7%) of 108 subjects with 1 year follow-up had died. Having ischemic changes diagnostic of ischemia by the revised criteria was associated with a trend for higher mortality in Chi square analysis (25% vs. 7%, p=0.07), but not of recurrent ED visits (12% vs. 5%, p=0.25) or hospital admission (12% vs. 8%, p=0.5). In multivariate analysis, after adjustment for age, gender, standard cardiac risk factors such as diabetes and smoking, and a history of CAD, ischemic ECG changes were not an independent predictor of mortality. The strongest predictor of both recurrent ED visits and HA was a history of CAD.
Discussion
Electrocardiographic changes in the ST segment and T waves have long been recognized as potent, if imperfect, indicators of ischemia and potential infarction (9–11). Consensus guidelines issued in 2000 recommended useful thresholds for identifying ST and T wave changes as pathologic (2), although multiple confounding factors including early repolarization, LBBB, pre-excitation syndromes, metabolic disturbances and myocarditis may complicate their application (1). However, growing recognition of age and gender differences in ECG patterns and particularly in precordial ST segments (12–16) suggested that ST amplitude was generally maximal in V2 and V3 and greater in men, particularly young men, than in women.
Macfarlane et al. developed criteria for ST elevation MI from a training set of 789 ECGs from patients presenting with chest pain as well as ECGs from a population of 1496 adult normals of both genders (13). Based on their findings, they proposed criteria for ST elevation MI which enhanced both sensitivity and specificity in the test set when compared with the original ACC/ESC criteria. While Macfarlane’s proposed criteria took into account age, gender, and specific ECG leads, it was cumbersome to apply in clinical practice because a formula had to be used to determine unique criteria for each patient.
In 2007, a new joint expert consensus document on the universal definition of MI was issued by the ESC/ACCF/AHA and WHF that incorporated many of Macfarlane’s concepts but without the need to determine patient specific criteria. The new criteria lowered the threshold for ST elevation in lead V1 from greater than or equal to 0.2 mV to greater than or equal to 0.1 mV to diagnose ischemia. They also set different thresholds for ST segment elevation in V2 and V3 compared with all other leads and set lower ST thresholds for women than men in these leads (1). In addition, ST depression of ≥0.05 mV in two contiguous leads was used as a revised criterion for ischemia. Recent recommendations for the standardization and interpretation of the ECG in acute ischemia/infarction go even further, calling for both age and gender specific criteria for ST elevation, as well as lead specific criteria for ST depression (17).
In this analysis of subjects presenting to the ED with symptoms of possible cardiac ischemia and a nondiagnostic ECG, the 2007 ESC/ACCF/AHA/WHF ECG criteria identified substantially more patients ultimately diagnosed with an ACS. Moreover, sensitivity for ACS was increased with minimal or no effect on specificity, as no subjects identified as having diagnostic ischemic changes by revised ECG criteria left the hospital with a final diagnosis of noncardiac chest pain. Patients who had ECGs diagnostic of ischemia by revised, but not prior standard criteria, also had a trend toward increased 1 year mortality, highlighting the importance in accurately identifying these patients.
Our results should be interpreted in light of possible limitations in our study. Electrocardiograms were reviewed by a single cardiologist, although tracings were analyzed several months apart to minimize bias. Holter electrocardiograms were recorded using the Mason-Likar rather than standard lead configuration, although reported differences between the two have centered predominantly on a rightward shift in axis and changes in Q and S wave amplitudes, rather than effects on ST and T wave changes (18,19). Moreover, our analysis used Holter electrocardiograms exclusively, so that the increased yield seen with the revised criteria for ischemia was based on identical tracings with the same lead configuration. Some patients were lost to longer term follow-up. The relatively small sample size may have limited power to detect the effect of the revised criteria on clinical outcomes. Nonetheless, in this analysis, revision of the ECG criteria for ischemia was associated with enhanced diagnostic performance and identified a subset of patients at higher risk. The revised criteria should be retained.
Acknowledgments
This study was supported by a grant from the National Heart, Lung, & Blood Institute (RO1HL69753), and by the General Clinical Research Center, University of California, San Francisco.
ABBREVIATIONS
- ECG
electrocardiogram
- MI
myocardial infarction
- LVH
left ventricular hypertrophy
- LBBB
left bundle branch block
- ACS
acute coronary syndromes
- ED
emergency department
- HA
hospital admissions
- ESC
European Society of Cardiology
- ACCF
American College of Cardiology Foundation
- AHA
American Heart Association
- WHF
World Heart Federation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Thygesen K, Alpert JS, White HD Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007;50 (22):2173–95. doi: 10.1016/j.jacc.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 2.Myocardial infarction redefined: a consensus document of the Joint European Society of Cardiology/American College of Cardiology Committee for the Redefinition of Myocardial Infarction. Eur Heart J. 2000;21:1502–13. doi: 10.1053/euhj.2000.2305. [DOI] [PubMed] [Google Scholar]
- 3.Shusterman V, Goldberg A, Schindler DM, Fleischmann KE, Lux RL, Drew BJ. Dynamic tracking of ischemia in the surface electrocardiogram. J Electrocardiol. 2007 Nov–Dec;40(6 Suppl):S179–86. doi: 10.1016/j.jelectrocard.2007.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Drew BJ, Schindler DM, Zegre JK, Fleischmann KE, Lux RL. Estimated body surface potential maps in emergency department patients with unrecognized transient myocardial ischemia. J Electrocardiol. 2007 Nov–Dec;40(6 Suppl):S15–20. doi: 10.1016/j.jelectrocard.2007.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schindler DM, Lux RL, Shusterman V, Drew BJ. Karhunen-Loève representation distinguishes ST-T wave morphology differences in emergency department chest pain patients with non-ST-elevation myocardial infarction versus nonacute coronary syndrome. J Electrocardiol. 2007 Nov–Dec;40(6 Suppl):S145–9. doi: 10.1016/j.jelectrocard.2007.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cannon CP, Battler A, Brindis RG, et al. ACC Key Data Elements and Definitions for Measuring the Clinical Management and Outcomes of Patients with Acute Coronary Syndromes. J Am Coll Cardiol. 2001;38:2114–30. doi: 10.1016/s0735-1097(01)01702-8. [DOI] [PubMed] [Google Scholar]
- 7.Mason RE, Likar I. A new system of multiple lead exercise electrocardiography. Am Heart J. 1966;71:196–205. doi: 10.1016/0002-8703(66)90182-7. [DOI] [PubMed] [Google Scholar]
- 8.Social Security Death Index (SSDI) http://ssdi.rootsweb.ancestry.com.
- 9.Kleber AG, Janse MJ, van Capelle FJ, Durrer D. Mechanism and time course of ST and TQ segment changes during acute regional myocardial ischemia in the pig heart determined by extracellular and intracellular recordings. Circ Res. 1978;42:603–13. doi: 10.1161/01.res.42.5.603. [DOI] [PubMed] [Google Scholar]
- 10.Birnbaum Y, Herz I, Sclarovsky, et al. Prognostic significance of the admission electrocardiogram in acute myocardial infarction. J Am Coll Cardiol. 1996;27:1128–32. doi: 10.1016/0735-1097(96)00003-4. [DOI] [PubMed] [Google Scholar]
- 11.Bayes de Luna A, Cino JM, Pujadas S, et al. Concordance of electrocardiographic patterns and healed myocardial infarction detected by cardiovascular magnetic resonance. Am J Cardiol. 2006;97:443–51. doi: 10.1016/j.amjcard.2005.08.068. [DOI] [PubMed] [Google Scholar]
- 12.Macfarlane PW. Age, sex, and the ST amplitude in health and disease. J Electrocardiol. 2001;34 (Suppl):235–41. doi: 10.1054/jelc.2001.28906. [DOI] [PubMed] [Google Scholar]
- 13.Macfarlane PW, Browne D, Devine B, et al. Modification of ACC/ESC criteria for acute myocardial infarction. J Electrocardiol. 2004;37 (Suppl):98–103. doi: 10.1016/j.jelectrocard.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 14.Wu J, Kors JA, Rijnbeck PR, et al. Normal limits of the electrocardiogram in Chinese subjects. Int J Cardiol. 2003;87:37–51. doi: 10.1016/s0167-5273(02)00248-6. [DOI] [PubMed] [Google Scholar]
- 15.Surawicz B, Parikh SR. Prevalence of male and female patterns of early ventricular repolarization in the normal ECG of males and females from childhood to old age. J Am Coll Cardiol. 2002;40:1870–6. doi: 10.1016/s0735-1097(02)02492-0. [DOI] [PubMed] [Google Scholar]
- 16.Macfarlane PW, Petryka J, Kaczmarska E. Normal limits of STj in v3R-V6R and V7-V9 (abstr) Eur Heart J. 2006;27 (Suppl):918. [Google Scholar]
- 17.Wagner GS, Macfarlane P, Wellens H, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part VI: acute ischemia/infarction: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. J Am Coll Cardiol. 2009;53:1003–11. doi: 10.1016/j.jacc.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 18.Papouchado M, Walker PR, James MA, Clarke LM. Fundamental differences between the standard 12-lead electrocardiograph and the modified (Mason-Likar) exercise lead system. Eur Heart J. 1987;8:725–33. doi: 10.1093/eurheartj/8.7.725. [DOI] [PubMed] [Google Scholar]
- 19.Gamble P, McManus H, Jensen D, Froelicher V. A comparison of the standard 12-lead electrocardiogram to exercise electrode placements. Chest. 1984;85:616–22. doi: 10.1378/chest.85.5.616. [DOI] [PubMed] [Google Scholar]