Abstract
Aims
Due to the chronicity of cocaine dependence, practical and effective maintenance interventions are needed to sustain long-term abstinence. We sought to assess the effects of long-term employment-based reinforcement of cocaine abstinence after discontinuation of the intervention.
Design
Participants who initiated sustained opiate and cocaine abstinence during a 6-month abstinence reinforcement and training program worked as data entry operators and were randomly assigned to a group that could work independent of drug use (Control, n = 24), or an abstinence-contingent employment (n = 27) group that was required to provide cocaine- and opiate-negative urine samples to work and maintain maximum rate of pay.
Setting
A nonprofit data entry business.
Participants
Unemployed welfare recipients who persistently used cocaine while in methadone treatment.
Measurements
Urine samples and self-reports were collected every six months for 30 months.
Findings
During the employment year, abstinence-contingent employment participants provided significantly more cocaine-negative samples than controls (82.7% and 54.2%; P = .01, OR = 4.61). During the follow-up year, the groups had similar rates of cocaine-negative samples (44.2% and 50.0%; P = .93), and HIV-risk behaviors. Participants’ social, employment, economic, and legal conditions were similar in the two groups across all phases of the study.
Conclusions
Employment-based reinforcement effectively maintains long-term cocaine abstinence, but many patients relapse to use when the abstinence contingency is discontinued, even after a year of abstinence-contingent employment. Relapse could be prevented in many patients by leaving employment-based abstinence reinforcement in place indefinitely, which could be facilitated by integrating it into typical workplaces.
Keywords: Cocaine, Methadone, Employment, Contingency management, Abstinence reinforcement
INTRODUCTION
The chronicity of drug dependence is well documented,1–8 and suggests a critical need for the development of interventions designed to maintain drug abstinence over time spans that are far longer than those currently delivered in most clinical and research settings.9–11 Toward this end, we have sought to develop a practical long-term contingency management intervention for drug dependence. In contingency management interventions, patients earn reinforcers (e.g., vouchers or privileges) upon meeting objectively observable and measurable criteria set by the clinician. Abstinence reinforcement is a type of contingency management intervention in which patients earn reinforcement contingent upon providing biological samples that confirm recent drug abstinence. Abstinence reinforcement interventions are typically studied as a method for initiating drug abstinence and implemented via outpatient clinics over 12-week periods, but the chronicity of drug dependence suggests that evaluation of an intervention’s success in maintaining long-term drug abstinence is of utmost importance.
Many studies have shown that abstinence reinforcement can effectively increase drug abstinence, and a recent meta-analysis has identified contingency management as a highly effective treatment for drug dependence.12 Prior studies of contingency management interventions also show that increasing the magnitude of reinforcement (i.e., the value of the incentives) can improve outcomes in individuals who initially appear unresponsive to the intervention.13 Other research has shown that arranging long-term exposure to abstinence reinforcement can maintain abstinence over an extended period of time.14 Thus, a potentially effective way to design a contingency management intervention is to arrange long-term, large magnitude reinforcement of drug abstinence. The therapeutic workplace is an employment-based contingency management intervention that is designed to address the practical problem of how to provide large-magnitude, long-term reinforcement of drug abstinence.15,16 In most contingency management interventions, patients earn vouchers exchangeable for goods or services, or a chance of winning a prize, upon submitting biological samples that meet criteria set by the clinician. In the therapeutic workplace, unemployed drug dependent adults are invited to paid job training or employment, and are required to provide drug-free urine samples to maintain access to the workplace and maintain maximum rate of pay. Since employee wages are a standard operating cost of most businesses, the cost of employment-based abstinence reinforcement could be reduced to the cost of urinalysis when applied as a long-term maintenance intervention.
A recent randomized controlled trial evaluated employment-based abstinence reinforcement as a maintenance intervention, and showed that employment-based abstinence contingencies were effective and critical in maintaining long-term cocaine abstinence.17 In that study, welfare recipients who persistently used cocaine while enrolled in methadone maintenance treatment were required to submit urine samples that demonstrated abstinence from opiates and cocaine in order to access paid job training during a six-month abstinence-initiation phase. Participants who initiated sustained abstinence and who completed the training required to become data entry operators were hired as employees of a non-profit data entry business for one year and randomly assigned to one of two groups. Urine samples were collected from all participants, but participants assigned to the employment-only control group could work independent of the results of urinalysis, while participants assigned to the abstinence-contingent employment condition were required to maintain opiate and cocaine abstinence in order to work and maintain maximum pay. The abstinence-contingent employment group submitted significantly more opiate- and cocaine- negative urine samples at monthly assessments throughout the year of employment, indicating that employment-based abstinence contingencies were important in the maintenance of drug abstinence in this population.
Although post-treatment relapse is common across all treatment modalities, at least two studies have shown that abstinence reinforcement increased the probability of cocaine abstinence during post-treatment follow-up,18,19 and the duration of abstinence achieved by participants during an abstinence reinforcement intervention has been associated with long-term outcome.14 Since the participants assigned to the abstinence-contingent employment group in the present study experienced an abstinence reinforcement intervention that exceeded the duration of almost all prior studies, it is possible that we could observe longer-lasting post-intervention effects. The purpose of the present analysis is to determine whether the additional year of abstinence contingencies experienced by the abstinence-contingent employment participants resulted in improved outcomes after discontinuation of the employment-based abstinence reinforcement contingency.
METHOD
Study participants and setting
Participants were 128 unemployed cocaine-dependent methadone maintenance patients who received welfare. Specific inclusion/exclusion criteria have been reported previously.17 The study was conducted in a therapeutic workplace that included a model data entry business in Baltimore, MD.20
Procedures
All participants were enrolled in phase 1 of the therapeutic workplace intervention for 6 months. During this phase, participants trained to become data entry operators. On Monday, Wednesday and Friday, participants provided breath and urine samples under direct observation. Breath samples were tested for alcohol. Urine samples were tested for opiates and cocaine. Participants earned a base pay of $8.00 per hour in vouchers and could earn approximately $2.00 per hour in vouchers based on productivity on the training programs. Earnings accumulated in the participant’s account until exchanged for a gift card or other approved goods and services.
After an initial induction period during which participants could attend the workplace independent of their urinalysis results, a stepped contingency program was introduced to initiate abstinence from cocaine, opiates, and alcohol. Participants were required to provide evidence of abstinence from the substances included in the contingency in order to work and maintain maximum pay. If a participant failed to provide a mandatory sample or provided a sample that tested positive for a substance covered by the contingency, then access to the workplace was denied until the participant could provide evidence of recent abstinence. Upon return to work, the rate of base pay was temporarily reduced and then increased incrementally to the original level as drug abstinence was maintained. The contingencies, stepped contingency program, details of the training, and the results of phase 1 of the program are described in detail elsewhere.21
Participants who attended the workplace on at least 50% of possible days, provided urine samples that met the reinforcement criteria on at least 80% of the collection opportunities during the four weeks prior to evaluation for inclusion in phase 2, and attained minimal typing proficiency qualified to participate in phase 2 and were eligible to be hired as employees of the nonprofit data entry business for one year and randomly assigned to the employment-only group (n = 24) or the abstinence-contingent employment group (n = 27). One participant of the latter group died early in the course of study participation for reasons unrelated to the study and was excluded from all present analyses. The two groups were demographically similar. Overall, the participants’ mean age was 43 years, 77% were female, and 88% were black. Phase 2 participants earned approximately $10 per hour, based partly an hourly wage and partly on pay for productivity (approximately $4.00 per hour as productivity pay given normative performance). Phase 2 participants received regular bi-weekly paychecks instead of vouchers.
Study groups
Participants assigned to the abstinence-contingent employment group were required to continue providing drug negative urine samples to access the workrooms on mandatory collection days, which were initially scheduled as in phase 1, but became random and progressively less frequent as abstinence was sustained. Participants assigned to the employment-only group were required to provide urine samples, but were no longer required to provide drug-negative samples in order to access the workplace or maintain maximum rate of pay. All phase 2 methods are described in greater detail elsewhere.17
After one year in phase 2, employment at Hopkins Data Services ended for all participants. Follow-up assessments were conducted 6 and 12 months after the end of phase 2, which was 24 and 30 months after enrollment in phase 1, respectively.
Outcome measures
The primary outcome measure was cocaine-negative urine samples (urinary benzoylecgonine concentration of <300 ng/mL). Secondary measures were opiate-negative urine samples (urinary morphine concentration of <300 ng/mL), and self-reported HIV-risk behaviors, and social, employment, economic, and legal conditions. HIV-risk behaviors were assessed using the Risk Assessment Battery.22 Other self-report measures were assessed using the Addiction Severity Index – Lite (ASI-Lite),23 and the Treatment Services Review.24 Primary and secondary measures based on assessments conducted at six-month intervals during phase 2 and the follow-up period.
Data analysis
The two groups were compared on dichotomous outcome measures assessed at a single time point (i.e., at intake to the study or at the end of phase 1) using logistic regression and on dichotomous outcome measures assessed twice during a condition (i.e., the phase 2 employment or follow-up periods) using Generalized Estimating Equation (GEE). For each group, a Spearman’s rank correlation analysis was used to assess the relationship between the percentage of cocaine negative urine samples collected from group participants during the employment period and the percentage of cocaine negative urine samples collected during follow-up. Exploratory analyses were conducted to identify predictors of post-treatment abstinence outcomes. Specifically, logistic regression was used to determine if a minimal set of participant characteristics and baseline measures collected prior to random assignment were associated with cocaine abstinence in the post-intervention follow-up period. Missing urine samples and missing self-report measures of drug use were treated as indicating drug use. Analyses in which missing data were ignored were also conducted but are not reported because they yielded similar outcomes in all cases. No assessments were missing at intake or at the end of phase 1. During phase 2, 100 and 94.4 percent of assessments were collected for employment-only and abstinence-contingent employment groups, respectively. At the 24-month follow-up time point, 100 and 92.3 percent of assessments were collected, and at the 30-month follow-up time point, 87.5 and 80.8 percent of assessments were collected for employment-only and abstinence-contingent employment groups, respectively. All analyses were conducted using SAS 9.1, were two-tailed, and were considered significant at p < .05.
RESULTS
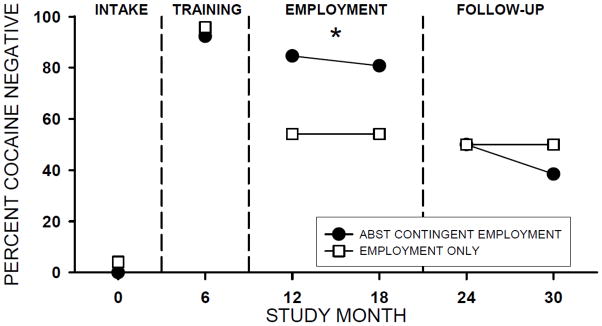
Figure 1 shows that almost all participants in both groups provided cocaine positive urine samples at intake to the study and cocaine negative urine samples at the end of phase 1. The figure also shows that abstinence-contingent employment participants maintained significantly higher rates of cocaine abstinence during phase 2 relative to the employment only group, but that this difference was not apparent during the follow-up period. Analysis of urine samples collected during phase 2 employment (at the 12- and 18-month time points) showed that abstinence-contingent employment participants provided significantly more cocaine-negative urine samples than employment-only participants [82.7% and 54.2%, respectively; P = .01, odds ratio (OR) = 4.61, 95% confidence interval (CI) = 1.38 – 15.38]. At the follow-up time points, the two groups were not significantly different (P = .93, OR = 0.96, 95% CI 0.37 – 2.52), and the percentage of cocaine negative samples observed during follow up for abstinence-contingent employment (44.2%) and employment-only (50.0%) groups was similar to the proportion of cocaine negative samples observed for the employment-only group during phase 2. As reported previously, opiate use was very low in both groups and not significantly different at any time point throughout the study.
Figure 1.
Percent of cocaine-negative samples collected at intake (Study Month 0), the end of the abstinence initiation and training phase (Study Month 6), during employment (Study Months 12 and 18), and at post-treatment follow-up (Study Months 24 and 30). Missing samples were counted as positive. The asterisk indicates that the groups are significantly different (p < .05) based on GEE analysis.
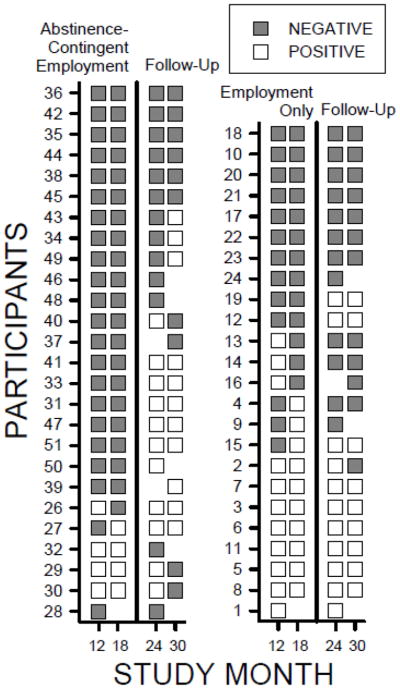
Figure 2 shows individual participants’ cocaine urinalysis results at six-month intervals during the year of phase 2 employment and at the follow-up time points during the year after phase 2. Overall, the figure shows that the pattern of cocaine-negative urine samples of individual participants across the phase 2 and follow-up time points is fairly stable for employment-only participants, whereas it is not stable for abstinence-contingent employment participants. Most importantly, of the ten employment-only participants who provided cocaine-negative urine samples in study months 12 and 18 (i.e., during phase 2), 70% maintained that pattern during follow-up. In contrast, only 30% of the 20 abstinence-contingent employment participants who provided cocaine-negative urine samples in study months 12 and 18 maintained that pattern during follow-up. Statistical analyses confirmed these general observations by showing that the percentage of cocaine-negative urine samples obtained at 12- and 18-month time points were significantly correlated with the percentage of cocaine-negative urine samples obtained at follow-up time points (24 and 30 months) in the employment-only group (P = .001; r = .63), but they were not correlated in the abstinence-contingent employment group (P = .59; r = .11).
Figure 2.
Dichotomous results of cocaine urinalysis for individual participants at four time points. The left panel shows the results for the abstinence-contingent employment group, and the right panel shows results for the employment-only group. Rows represent individual participants and columns represent time points. In each panel, the two columns to the left of the vertical midline represent data obtained during the year of employment (Study Months 12 and 18), and the two columns to the right of the line show represent follow-up data obtained after the discontinuation of the study (Study Months 24 and 30). Filled squares indicate cocaine-negative urine samples, open squares indicate cocaine-positive samples, and blank spaces indicate missing data. The numbers on the vertical axes correspond to participant numbers reported in DeFulio et al. (2009).
During the follow-up period, self-reported rates of HIV risk behaviors were relatively low in both groups and no significant differences were obtained. No injection drug use was reported by any participant during the follow-up period, and abstinence from crack was reported by 75% and 66.7% of employment-only and abstinence-contingent employment group participants, respectively. We previously reported a significant effect on trading sex for drugs or money during the intervention period, but this difference was not maintained during follow-up; 8.3% and 3.8% of participants in the employment-only and abstinence-contingent employment groups reported trading sex for drugs or money, respectively.
Analyses of the relationship between pre-treatment participant characteristics and post-treatment cocaine abstinence (defined by the submission of 2 cocaine negative samples during the follow up year; Y/N) showed that being younger (Wald χ2(1) 5.39, P = 0.02, OR = 1.17, 95% CI = 1.02–1.33) and male (Wald χ2(1) 4.12, P = 0.04, OR = 0.16; 95% CI = 0.03–0.94) were associated with abstaining from cocaine use during the follow-up period, Income from all sources (including welfare) in the 30 days prior to study participation, completion of HS or GED (Y/N), and days of self-reported cocaine use in the month prior to joining the study were not significantly associated with post-treatment outcome. Analyses of the relationship between baseline measures obtained during the first 30 days of induction in phase 1 (when no contingencies were applied) and post-treatment cocaine abstinence were also conducted. These analyses showed the proportion of cocaine negative samples obtained during this period (missing = positive) was positively correlated with post-treatment cocaine abstinence (Wald χ2 (1) 4.12, P = 0.04, OR = 23.14, 95% CI = 1.11–481.26), but the percent of days attended in the first 30 days of induction was not predictive of post-treatment abstinence.
The data in Table 1 characterizes social, employment, economic and legal conditions of the lives of participants in the two groups over the course of participation in the study. Overall, the table shows that the lives of participants in the two groups were fairly similar throughout the study. The participants in the two study groups were not significantly different on any of these measures at intake, at the end of training, during the year of employment, or during the year of follow-up. More participants reported earning at least some money from employment during the year of follow-up compared to at study intake, but only about 40% of participants earned any money from employment during the year after employment in therapeutic workplace. Similarly, a lower percentage of study participants were on welfare or living in poverty during the year of follow-up compared to at study intake, but the majority of participants were on welfare and in poverty during the year of follow-up. Social stability indices showed that a large majority of participants were satisfied with their living situation and still in drug treatment during the year of follow-up. Reported rates of illegal activity and new involvement with the criminal justice system were low at all points throughout the study.
TABLE 1.
EMPLOYMENT, ECONOMIC, SOCIAL, AND LEGAL OUTCOMES
| Percentage | Chi Square* | p | ||
|---|---|---|---|---|
| Employment Only | Abstinence- Contingent Employment | |||
| Employment Outcomes | ||||
| Earned any money from work | ||||
| Intake | 12.5 | 0 | 3.46 | 0.06 |
| Training | 20.8 | 15.4 | 0.25 | 0.62 |
| Employment | 100 | 100 | - | - |
| Follow-up | 41.7 | 42.3 | 0.002 | 0.96 |
| Received job/academic training a | ||||
| Intake | - | - | - | - |
| Training | 100 | 100 | - | - |
| Employment | 0 | 0 | - | - |
| Follow-up | 8.3 | 11.5 | 0.14 | 0.71 |
| Economic Outcomes | ||||
| Received welfare | ||||
| Intake | 100 | 100 | - | - |
| Training | 83.3 | 80.8 | 0.06 | 0.81 |
| Employment | 66.7 | 65.4 | 0.01 | 0.92 |
| Follow-up | 75 | 69.2 | 0.21 | 0.65 |
| Employment income below poverty threshold b | ||||
| Intake | 100 | 100 | - | - |
| Training | 95.8 | 100 | 0.002 | 0.97 |
| Employment c | 75 | 88.5 | 1.53 | 0.22 |
| Follow-Up | 87.5 | 88.5 | 0.01 | 0.92 |
| Social Stability Outcomes | ||||
| Satisfied with living arrangement | ||||
| Intake | 54.2 | 69.2 | 1.20 | 0.27 |
| Training | 79.2 | 92.3 | 1.79 | 0.18 |
| Employment | 70.8 | 84.6 | 1.38 | 0.24 |
| Follow-up | 95.8 | 96.2 | 0.003 | 0.95 |
| Received drug treatment a | ||||
| Intake | 100 | 100 | - | - |
| Training | 100 | 100 | - | - |
| Employment | 100 | 100 | - | - |
| Follow-up | 87.5 | 80.8 | 0.42 | 0.517 |
| Legal Outcomes | ||||
| Any illegal activity for profit | ||||
| Intake | 20.8 | 15.4 | 0.25 | 0.62 |
| Training | 8.3 | 0 | 2.26 | 0.13 |
| Employment | 4.2 | 0 | 1.11 | 0.29 |
| Follow-up | 12.5 | 0 | 3.46 | 0.06 |
| Charges, trial, or sentence pending | ||||
| Intake | 4.2 | 0 | 1.11 | 0.29 |
| Training | 4.2 | 0 | 1.11 | 0.29 |
| Employment | 12.5 | 0 | 3.46 | 0.06 |
| Follow-up | 16.7 | 3.9 | 2.28 | 0.13 |
DF = 1
All items based on ASI-Lite assessment unless otherwise noted
From the Treatment Services Review
Based on 2005 US Department of Health and Human Services Poverty Guidelines
Includes income earned from employment at the therapeutic workplace.
DISCUSSION
Employment-based abstinence reinforcement effectively maintained cocaine abstinence throughout a year of employment; however, maintenance of employment-based abstinence reinforcement throughout the year of employment was not effective in promoting abstinence after the reinforcement intervention was discontinued. Abstinence-contingent employment participants maintained significantly and substantially higher rates of cocaine-negative urine samples than employment-only participants during phase 2, whereas the two groups provided very similar rates of cocaine negative urine samples during the follow-up year after the intervention was discontinued. Twenty of the 27 abstinence-contingent employment participants (74%) provided cocaine-negative urine sample at both of the assessment time points during the year in phase 2 (while the employment-based abstinence reinforcement contingencies were in effect), but only six (22% of participants) provided cocaine-negative urine samples at both assessment time points during the follow-up year. These results provide additional compelling evidence of the chronicity of cocaine dependence and support the common observation that many patients relapse to drug use after leaving treatment.1–11
The present findings provide strong support for our view that ongoing intervention is required to maintain cocaine abstinence in many cocaine-dependent methadone patients who initiate abstinence during an abstinence reinforcement intervention. The data from phase 2 of this study suggests that employment-based abstinence reinforcement can be an effective maintenance intervention. One of the greatest potential benefits of employment-based contingency management interventions is that they offer a method of harnessing a large magnitude and widely available reinforcer, wages from work, for therapeutic benefit. Since wages from work are a standard operating cost for any business, the cost of implementing employment-based contingency management as a maintenance intervention could potentially be reduced to the cost of the urinalysis program. Thus, it may be economically and logistically feasible to sustain employment-based abstinence reinforcement indefinitely. The long-term delivery of methadone maintenance in the treatment of opioid dependence offers a precedent and a model for the long-term delivery of employment-based abstinence reinforcement. Evaluating methods of achieving economic and logistical feasibility should be a primary focus of future studies of employment-based abstinence reinforcement.
It is also possible that novel techniques could be developed that will enhance the long-term effectiveness of abstinence reinforcement interventions; however no effective technique has been identified to date. One technique that has been tested in previous clinical trials is combining cognitive behavior therapy with abstinence reinforcement interventions,25–27 but none of the studies in which this combined approach was tested reported significant improvements in long-term cocaine abstinence outcomes relative to abstinence reinforcement alone. It is possible that an alternative therapeutic approach to relapse prevention will enhance the long-term outcomes of abstinence reinforcement more effectively than cognitive-behavior therapy. It is also clear from the present study that continuation of employment alone will be insufficient to maintain cocaine abstinence for many people, as shown by the relatively high rate of cocaine use in the employment only group during the year of employment. Although the contingency is clearly necessary, it may be possible to reduce the frequency of urine testing substantially while maintaining the effectiveness of the intervention. In the employment phase of the present study the testing schedule was thinned from thrice weekly to once bi-weekly on average as drug abstinence was maintained over the course of six months. Whether still more infrequent testing would be sufficient to maintain abstinence should be evaluated in future studies.
Interestingly, about 25% of participants maintained consistent cocaine abstinence use after the abstinence reinforcement contingencies were discontinued, whether those contingencies were discontinued after only 6 months (employment-only participants) or after 18 months (abstinence-contingent employment participants). The design of this study does not allow us determine whether initial exposure to the employment-based abstinence reinforcement contributed to the long-term abstinence outcomes for those individuals. However, other studies have shown that voucher-based abstinence reinforcement can produce increases in cocaine abstinence that persist after abstinence reinforcement is discontinued.18,19 The results of this study indicate that maintenance of post-treatment cocaine abstinence was most likely when baseline cocaine use was less severe. This finding indicates that patients who exhibit high rates of cocaine use during the early stage of treatment are especially likely to need ongoing maintenance intervention to sustain drug abstinence over an extended period of time. Importantly, the results from the employment phase of the study show that cocaine abstinence can be sustained even in those heavy cocaine users when employment-based abstinence reinforcement is maintained.
By common standards, the 30-month duration of this study is fairly long. Yet for most drug users, a 30-month period represents a small fraction of their struggle with drug dependence. Our treatments should seek to promote abstinence that lasts far longer than 30 months, and ideally for the remainder of patients’ lives. The results of this study illustrate the difficulty in promoting life-long abstinence. However, the results of this study also suggest that employment-based abstinence reinforcement has the potential to be a very valuable method for promoting lifelong drug abstinence, particularly if the abstinence reinforcement contingencies are maintained.
Acknowledgments
This work was supported by National Institute on Drug Abuse grants R01DA13107 and T32DA07209. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health. The authors report no conflict of interest. The first author had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Additional contributors include: Paul Nuzzo (data analysis and statistical testing), Karly Diemer (study protocol and trial management), Jackie Hampton (assessments), and Lauren Long (data management).
Footnotes
DECLARATION: The authors declare no conflict of interest.
TRIAL REGISTRATION: clinicaltrials.gov. Identifier: NCT00249496
References
- 1.Galai N, Safaeian M, Vlahov D, Bolotin A, Celentano DD ALIVE Study. Longitudinal patterns of drug injection behavior in the ALIVE study cohort, 1988–2000: Description and determinants. Am J Epidemiol. 2003;158(7):695–704. doi: 10.1093/aje/kwg209. [DOI] [PubMed] [Google Scholar]
- 2.Hser YI, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Arch Gen Psychiatry. 2001;58(5):503–508. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- 3.Hser YI, Huang D, Chou CP, Anglin MD. Trajectories of heroin addiction: growth mixture modeling results based on a 33-year outcome study. Eval Rev. 2007;31(6):548–563. doi: 10.1177/0193841X07307315. [DOI] [PubMed] [Google Scholar]
- 4.Hser YI, Huang D, Brecht ML, Li L, Evans E. Contrasting trajectories of heroin, cocaine, and methamphetamine use. J Addict Dis. 2008;27(3):13–21. doi: 10.1080/10550880802122554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Brien CP. Review. evidence-based treatments of addiction. Philos Trans R Soc Lond B Biol Sci. 2008;363(1507):3277–3286. doi: 10.1098/rstb.2008.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Penberthy JK, Ait-Daoud N, Vaughn M, Fanning T. Review of treatment for cocaine dependence. Curr Drug Abuse Rev. 2010;3(1):49–62. doi: 10.2174/1874473711003010049. [DOI] [PubMed] [Google Scholar]
- 7.Simpson DD, Joe GW, Fletcher BW, Hubbard RL, Anglin MD. A national evaluation of treatment outcomes for cocaine dependence. Arch Gen Psychiatry. 1999;56(6):507–514. doi: 10.1001/archpsyc.56.6.507. [DOI] [PubMed] [Google Scholar]
- 8.Vaillant GE. A 20-year follow-up of New York narcotic addicts. Archives of General Psychiatry. 1973;29(2):237–241. doi: 10.1001/archpsyc.1973.04200020065009. [DOI] [PubMed] [Google Scholar]
- 9.Dennis M, Scott CK. Managing addiction as a chronic condition. Addict Sci Clin Pract. 2007;4(1):45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment insurance and outcomes evaluation. JAMA. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 11.Silverman K, Svikis D, Wong CJ, Hampton J, Stitzer ML, Bigelow GE. A reinforcement-based therapeutic workplace for the treatment of drug abuse: three-year abstinence outcomes. Exp Clin Psychopharmacol. 2002;10(3):228–240. doi: 10.1037//1064-1297.10.3.228. [DOI] [PubMed] [Google Scholar]
- 12.Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165(2):179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- 13.Silverman K, Chutuape MA, Bigelow GE, Stitzer ML. Voucher-based reinforcement of cocaine abstinence in treatment-resistant methadone patients: effects of reinforcement magnitude. Psychopharmacol. 1999;146(2):128–138. doi: 10.1007/s002130051098. [DOI] [PubMed] [Google Scholar]
- 14.Silverman K, Robles E, Mudric T, Bigelow GE, Stitzer ML. A randomized trial of long-term reinforcement of cocaine abstinence in methadone-maintained patients who inject drugs. J Consult Clin Psychol. 2004;72(5):839–854. doi: 10.1037/0022-006X.72.5.839. [DOI] [PubMed] [Google Scholar]
- 15.Silverman K, Svikis D, Robles E, Stizer ML, Bigelow GE. A reinforcement-based therapeutic workplace for the treatment of drug abuse: six-month abstinence outcomes. Exp Clin Psychopharmacol. 2001;9(1):14–23. doi: 10.1037/1064-1297.9.1.14. [DOI] [PubMed] [Google Scholar]
- 16.Silverman K. Exploring the limits and utility of operant conditioning in the treatment of drug addiction. The Behav Anal. 2004;27(2):209–230. doi: 10.1007/BF03393181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeFulio A, Donlin WD, Wong CJ, Silverman K. Employment-based abstinence reinforcement as a maintenance intervention for the treatment of cocaine dependence: A randomized controlled trial. Addiction. 2009;104(9):1530–1538. doi: 10.1111/j.1360-0443.2009.02657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins ST, Wong CJ, Badger GJ, Ogden DE, Dantona RL. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. J Consult Clin Psychol. 2000;68(1):64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- 19.Higgins ST, Badger GJ, Budney AJ. Initial abstinence and success in achieving longer term cocaine abstinence. Exp Clin Psychopharmacol. 2000;8(3):377–386. doi: 10.1037//1064-1297.8.3.377. [DOI] [PubMed] [Google Scholar]
- 20.Silverman K, Wong CJ, Grabinski MJ, et al. A web-based therapeutic workplace for the treatment of drug addiction and chronic unemployment. Behav Modif. 2005;29(2):417–463. doi: 10.1177/0145445504272600. [DOI] [PubMed] [Google Scholar]
- 21.Donlin WD, Knealing TW, Needham M, Wong CJ, Silverman K. Attendance rates in a workplace predict subsequent outcome of employment-based reinforcement of cocaine abstinence in methadone patients. J Appl Behav Anal. 2008;41(4):499–516. doi: 10.1901/jaba.2008.41-499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Navaline HA, Snider EC, Petro CJ, Tobin D, Metzger D, Alterman AI, Woody GE. Preparations for AIDS vaccine trials. An automated version of the Risk Assessment Battery (RAB): enhancing the assessment of risk behaviors. AIDS Res Hum Retroviruses. 1994;10(Suppl 2):S281–3. [PubMed] [Google Scholar]
- 23.McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr HL, et al. New data from the Addiction Severity Index: Reliability and validity in three centers. J Nerv Ment Dis. 1985;173(7):412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- 24.McLellan AT, Alterman AI, Cacciola J, Metzger D, O’Brien CP. A new measure of substance abuse treatment. Initial studies of the treatment services review. J Nerv Ment Dis. 1992;180(2):101–110. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Epstein DH, Hawkins WE, Covi L, Umbricht A, Preston KL. Cognitive-behavioral therapy plus contingency management for cocaine use: Findings during treatment and across 12-month follow-up. Psychol Addict Behav. 2000;17(1):73–82. doi: 10.1037/0893-164X.17.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rawson RA, Huber A, McCann M, Shoptaw S, Farabee D, Reiber C, Ling W. A comparison of contingency management and cognitive-behavioral approaches during methadone maintenance treatment for cocaine dependence. Arch Gen Psychatry. 2002;59(9):817–824. doi: 10.1001/archpsyc.59.9.817. [DOI] [PubMed] [Google Scholar]
- 27.Rawson RA, McCann MJ, Flammino F, Shoptaw S, Miotto K, Reiber C, Ling W. A comparison of contingency management and cognitive–behavioral approaches for stimulant-dependent individuals. Addiction. 2006;101(2):267–274. doi: 10.1111/j.1360-0443.2006.01312.x. [DOI] [PubMed] [Google Scholar]