Abstract
Context
Anxiety disorders commonly present in primary care where evidence-based mental health treatments often are unavailable or suboptimally delivered.
Objective
Compare evidence-based treatment for anxiety disorders to usual care in primary care, for principal and comorbid generalized anxiety disorder (GAD), panic disorder (PD), social anxiety disorder (SAD) and posttraumatic stress disorder (PTSD). We hypothesized superiority of CALM for principal anxiety disorders and comorbid disorders.
Design
A randomized, controlled trial comparing CALM intervention with Usual Care, at baseline, 6-month, 12-month and 18-month follow-ups.
Setting
17 primary care clinics in the United States.
Patients
Referred primary care sample, 1004 patients, with principal DSM-IV diagnoses of GAD (n=549), PD (n=262), SAD (n=132), or PTSD (n=61), mean 43.7 years (SD=13.7), 70.9% female,. 80% completed 18-month follow-up.
Interventions
CALM (computer-guided CBT and/or pharmacotherapy recommendations) and Usual Care.
Main Outcome Measures
Generalized Anxiety Disorder Severity Scale, Panic Disorder Severity-Self Report scale, Social Phobia Inventory, and PTSD Checklist-Civilian Version.
Results
CALM was superior to Usual Care for principal GAD at 6-month (−1.61; 95% CI = −2.42 to −.79), 12-month (−2.34; 95% CI = −3.22 to −1.45) and 18-month (−2.37; 95% CI = −3.24 to −1.50), PD at 6-month (−2.00; 95% CI = −3.55 to −0.44) and 12-month (−2.71; 95% CI = −4.29 to −1.14), and SAD at 6-month (−7.05; 95% CI = −12.11 to −2.00) outcomes. CALM was superior to Usual Care for comorbid SAD at 6-month (−4.26; 95% CI = −7.96 to −0.56), 12-month (−8.12, 95% CI = −11.84 to −4.40) and 18- month (−6.23, 95% CI = −9.90 to −2.55) outcomes. Effect sizes favored CALM, but were not statistically significant for other comorbid disorders.
Conclusions
CALM (CBT and psychotropic recommendations) is more effective than Usual Care for principal anxiety disorders, and to a lesser extent, comorbid anxiety disorders that present in primary care.
Anxiety disorders are common, costly and debilitating.1,2,3,4 Although effective evidence-based psychosocial (i.e., cognitive behavioral therapy, CBT) and pharmacological treatments for anxiety disorders exist, these treatments often are not available (i.e., CBT), or sub-optimally delivered (i.e., pharmacotherapy). Since most persons with anxiety disorders present for treatment in primary care,5,6,7,8 we conducted a randomized controlled trial of a collaborative care intervention designed to improve evidence-based treatment for anxiety disorders common in primary care. In addition to comparing disorder-specific outcomes between the intervention and usual care over an 18-month follow up period, we aimed to evaluate treatment effects at the level of the individuals in the study who most often have a constellation of disorders and symptoms, rather than a single anxiety disorder.
In order to implement evidence-based treatments in primary care, innovative approaches were required to overcome the limitations of current models of delivery. For example, CBT has evolved into specific applications for specific anxiety disorders, yet separate, uniquely tailored CBT manuals for each and every principal anxiety disorder are unlikely to be implemented in most treatment settings and especially in primary care. To provide a treatment for multiple anxiety disorders, we created a model of CBT that addressed the four most common anxiety disorders in primary care settings (panic disorder with or without agoraphobia, generalized anxiety disorder, social anxiety disorder, and posttraumatic stress disorder;5 in one program. Furthermore, given the relative dearth of highly trained mental health providers available within primary care settings, we designed our CBT program to be used by persons with minimal or no training in mental health. Specifically, we developed a computerized program to guide the mental health provider (as well as the patient), thereby reducing the amount of expertise and training needed. Computer-assisted programs have been used in training in CBT,9,10 and in self-directed CBT,11 but they have not before been used for ongoing assistance of the mental health provider in the delivery of CBT.
The approach to delivery of pharmacotherapy was also modified to suit the needs of primary care settings. That is, since it is well-known that delivery of pharmacotherapyin primary care is often of suboptimal quality,12 we used a “collaborative care model”,13 in which patients remained under the care of their primary care physician, while psychiatrists’ advice for pharmacotherapy optimization was relayed to primary care physicians by health care managers, or Anxiety Clinical Specialists (ACS). Patients in the intervention arm had the option of choosing CBT, pharmacotherapy, or both, and ACSs were responsible not only for delivering CBT but also for assisting primary care providers to manage medications.
We have presented data elsewhere showing that CALM was superior to usual care using general outcome measures of anxiety that span disorders, rather than disorder-specific measures.14 The purpose of this paper is to address disorder-specific outcomes for each participant’s constellation of anxiety disorders. The overwhelming majority of individuals with an anxiety disorder meet diagnostic criteria for at least one other diagnosis, most commonly another anxiety and/or mood disorder, in community-based or population-based samples1,15 as well as in samples drawn from treatment settings.16 Evidence-based treatment efficacy studies, including pharmacotherapy and psychotherapy studies, typically select participants on the basis of a principal disorder, often operationalized as the disorder that is most troubling to the individual, or associated with the most distress or interference with functioning. Evaluation of outcome based solely on improvement in this principal disorder means that treatment effects are estimated from only one feature, albeit the most pressing, of the entire symptom constellation in each individual. This approach is at variance with the demands of real world clinical practice where individual persons with co-occurring disorders, rather than the specific individual disorders, must be treated. To address this issue, we evaluated outcomes not only in terms of the principal disorder, but also for comorbid disorders.
Our approach in the CALM intervention was to target the principal anxiety disorder. Since previous research has indicated that adequate CBT treatment of a principal anxiety disorder simultaneously improves rates of comorbid disorders,17,18,19,20,21,22 we hypothesized that the CALM intervention would benefit comorbid disorders as well. Prior studies compared CBT to no-treatment comparisons in restricted samples, and limited their assessment of comorbidity to diagnostic assignment. The current study represents the investigation of the effects of targeted CBT treatment upon comorbidity in a generalizable sample, relative to a usual care comparison, and using sensitive dimensional measures of comorbid anxiety disorder symptom severity.
Methods
Design
Our randomized controlled effectiveness trial compared the CALM intervention (ITV) to UC in 17 primary care clinics in 4 US cities. Between June 2006 and August 2008, 1004 patients with anxiety disorders (with or without major depression) were randomized, and those randomized to ITV received treatment for up to 12 months. Blind assessments occurred at 6, 12, and 18 months after baseline.
Participants
Between June 2006 and April 2008, 1004 primary care patients with panic disorder with or without agoraphobia (PD), generalized anxiety disorder (GAD), social anxiety disorder (SAD), and/or posttraumatic stress disorder (PTSD), were enrolled. Participating research institutions were: University of Washington (Seattle), University of California-Los Angeles, University of California-San Diego, University of Arkansas for Medical Sciences, and the RAND Corporation (an assessment site only).23
Recruitment
Primary care providers (PCPs) and clinic nursing staff directly referred potential participants (Ps).. At some sites, a five-question anxiety screener, the Overall Anxiety Severity and Impairment Scale (OASIS)24 was used to identify potential Ps. A trained study clinician, the Anxiety Clinical Specialist (ACS), functioned as the main care manager/interventionist, as well as the diagnostician who met with referred Ps to determine eligibility. All Ps gave informed, written consent to participate in this study, which was approved by each institution’s Institutional Review Board.
Inclusion Criteria
An eligible P had to be a patient at a participating clinic, 18–75 years old, meet DSM-IV criteria for one or more of GAD, PD, SAD, or PTSD (based on the Mini International Neuropsychiatric Interview (MINI)25 administered by the ACS after formal training and diagnostic reliability testing), and score at least 8 (moderate and clinically significant anxiety symptoms on a scale ranging from 0–20) on the OASIS.24 Within the MINI, Ps indicated which of the disorders for which they met diagnostic criteria was currently ‘most troubling’ to them; this disorder became their principal anxiety disorder; other assigned diagnoses became their comorbid anxiety disorders.
Exclusion Criteria
Ps with unstable or life-threatening medical conditions, marked cognitive impairment, active suicidal intent or plan, psychosis, or bipolar I disorder were excluded. Alcohol and/or marijuana abuse (but not dependence) was permitted, but other drug abuse or dependence was exclusionary. Ps already receiving ongoing CBT (N = 7) were excluded, as were Ps who could not speak English or Spanish (n=2).
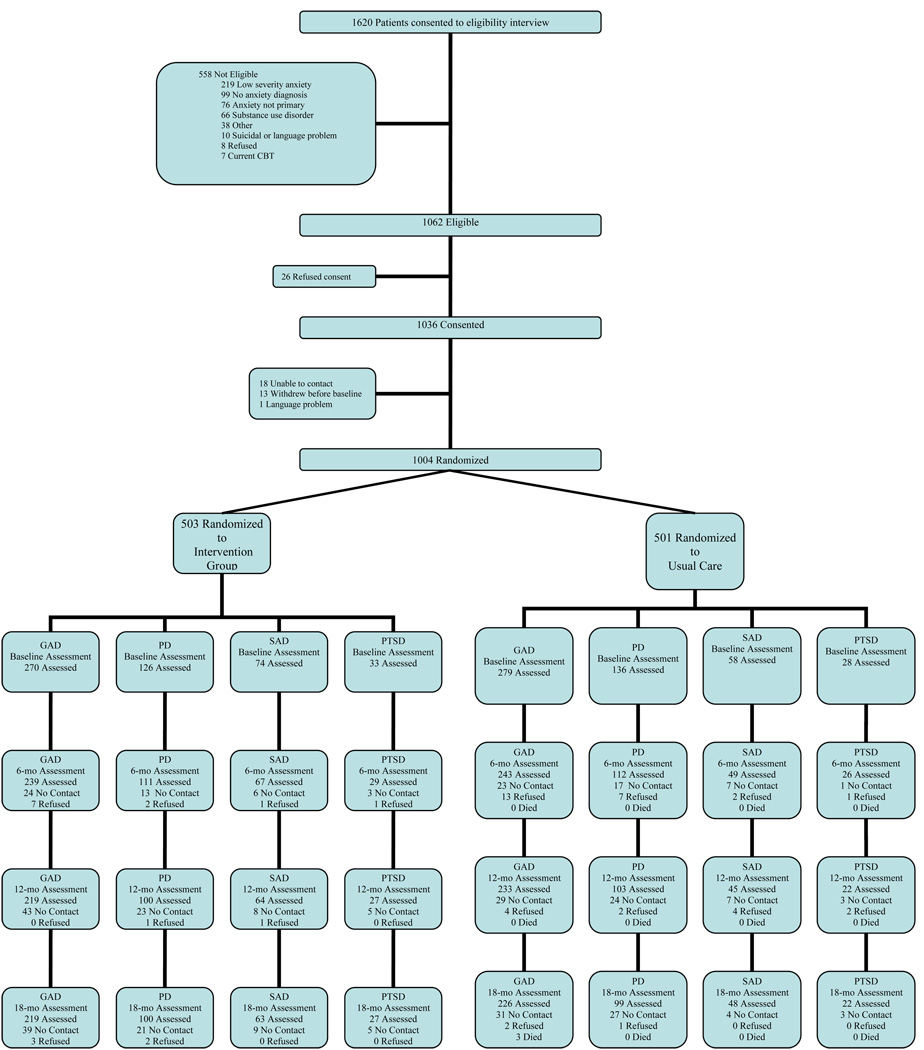
Randomization
After baseline assessment, Ps were randomized, using stratified (by clinic and presence of co-morbid major depression) permuted block randomization, to ITV or UC by an automated program at RAND. Block size was masked to all clinical site study members. The Consort Diagram describes patient flow from referral, through eligibility screening, consent and randomization for each principal anxiety disorder group (Figure 1).
Figure 1. Consort Diagram.
Intervention (ITV)
ITV Ps received a treatment involving pharmacotherapy, computer-assisted CBT, or both, depending on their preference.
CBT
The CBT program (called CALM Tools for Living, English and Spanish versions) contained 8 modules. The cognitive restructuring and two exposure modules were tailored to each of the four anxiety disorders through branching mechanisms, whereas the remaining modules (i.e., self monitoring, psychoeducation, fear hierarchy, breathing retraining, relapse prevention) were mostly generic.26 Ps selected their most distressing and disabling of the four anxiety disorders as the primary target in the first CBT session (this corresponded with the principal anxiety disorder designated in the MINI interview in the majority (74–89% across disorders) of cases)1. Then, some CBT modules were tailored to the principal disorder (e.g., exposure to trauma reminders for PTSD versus interoceptive exposure for PD), whereas the content of other modules was the same regardless of the principal disorder (e.g., breathing retraining).
The ACS sat side by side with the P as they both viewed the program on screen. Throughout, the program provided prompts to ACSs to engage in specific tasks, such as helping Ps to establish a fear hierarchy, demonstrating breathing skills, practicing cognitive skills, conducting interoceptive exposure, or designing in vivo exposure assignments. Occasionally, the ACS used additional strategies, such as behavioral activation and cognitive restructuring for depressed mood, and motivational enhancement strategies to maintain patient engagement.
Medication
For Ps who selected medication management only or combined with CBT, the ACS provided (56% in person, 43% by phone) adherence monitoring, counseling to avoid alcohol and caffeine and to optimize sleep hygiene and behavioral activity, and relayed feedback to PCPs about medication from the supervising psychiatrist. Medication was prescribed by the primary care provider (PCP). Medication consultation was available from a local study psychiatrist who provided single-session medication management training to PCPs using a simple algorithm.12 The same algorithm was applied across all four anxiety disorder, and emphasized first line use of SSRI or SNRI antidepressants, with the goal of increasing the dose to the maximum tolerable dose. Lack of response prompted substitution of a different antidepressant. Sub-optimal improvement prompted addition of another antidepressant or a benzodiazepine (in select cases, excepting PTSD). More elaborate interventions were considered after consultation with the expert study psychiatrist
Collaborative Care
ACSs interacted regularly with PCPs in person and over the phone. PCPs remained the clinician of record and prescribed all medications. Psychiatrist consultation to PCPs was readily available by phone, and more complex or treatment refractory cases could be seen by the psychiatrist for in person consultation.
Web-Based Tracking
The ACS tracked P outcomes using a web-based tracking system14 that allowed for real time monitoring of recruitment, enrollment, diagnoses, ineligibility, patient contact information and continuous, and session symptom assessments using the OASIS24 and a 3-item version of the PHQ-9, assessing depressed mood, loss of interest and fatigue.27
Treatment Steps
The treatment goal was either clinical remission, defined as an OASIS score<5 (=”mild”), sufficient improvement such that the P did not want further treatment, or improvement with residual symptoms or problems requiring a different kind of treatment not offered in the protocol. After the first 10–12 weeks, symptomatic Ps could receive more of the same modality (CBT or medication) or the alternative modality, for up to 3 more steps (i.e., another 10–12 weeks) of treatment. After completion of acute treatment, Ps were entered into "continued care" and received monthly follow-up phone calls to reinforce CBT skills and/or medication adherence for up to a year from study enrollment.
Anxiety Clinical Specialist
ACSs (n = 14; 6 social workers, 5 registered nurses, 2 masters level psychologists, 1 doctoral level psychologist)had some patient care experience (although only 8 had prior mental health care experience) and some exposure to primary care settings, but did not have expertise in anxiety management or CBT.23 All ACSs were located within the participating primary care clinics.
ACS training involved three full days of didactic presentation of the CBT program, motivational interviewing, evidence-based medications for anxiety, the medication algorithm, and common pitfalls that contribute to medication non-adherence. CBT training additionally included recommended readings, a detailed content manual2, in-person or telephone-administered role-plays, successful completion of two training patients, and demonstrated proficiency as evaluated by expert psychologists3.
Throughout the study, ACSs received ongoing group telephone supervision for approximately 1 hour per week from an expert psychologist and psychiatrist for diagnostic, CBT, and medication management issues.
Usual Care (UC)
UC Ps continued to be treated by their physician with medication, whatever counseling they were able to provide, or referral to a mental health specialist.23 Their only contact with study personnel was for assessment.14
Measures
The assessment battery was administered at baseline, 6, 12, and 18 months via a centralized phone survey by the RAND survey research group, blinded to group assignment.
Disorder-Specific Measures
Disorder-specific scales were administered for every anxiety disorder assigned at baseline assessment. Each scale possesses good to excellent psychometric properties. For PD, the 7-item (0–4 scale) Panic Disorder Severity - Self Report scale (PDSS-SR)28 was used. For GAD, the 6-item (0–4 scale) Generalized Anxiety Disorder Severity Scale (GADSS)29,30,31 was used. For SAD, the 17-item (0–4 scale) Social Phobia Inventory (SPIN)32 was used. For PTSD, the 17-item (1–5 scale) PTSD Checklist-Civilian Version (PCL-C)33,34 was used. Criteria for response and remission were consistent across disorders, to facilitate comparisons. Given that published rates range from 30–50%,35 ‘response’ was defined as a reduction of 40% or more on each scale, or meeting the definition of remission. For ‘remission’, published definitions for cut-off scores were used where available (PDSS: ≤ 7; SPIN: ≤ 18) and a similar strategy (i.e., indicating no more than mild severity averaged across items) was used to derive cutoff scores for the remaining scales (PCL-C: ≤ 34; GADSS: ≤ 6).
CBT integrity
For the CALM CBT program, digital recordings of each ACS session at each site (n=259) were randomly selected for adherence/competency monitoring using a set of 1–7 point Likert-scales (higher scores represents better performance), completed by 2 PhD level independent raters who initially demonstrated inter-rater reliability. Ratings were made of adherence to the content of each module and overall therapist competency.4
Statistical Analysis
All statistical analyses were performed at RAND. We compared demographics and other baseline characteristics between ITV and UC groups using t-tests and chi-square tests for continuous and categorical variables respectively. To estimate the intervention effect over time for each principal anxiety disorder and each comorbid anxiety disorder group separately, we jointly modeled the outcomes using a repeated measures analysis over the four assessments (baseline and 3 follow-ups at 6, 12 and 18 months)by time, intervention, the interaction of time and intervention, site, and those patient characteristics that were found to be unbalanced (p<.1) between intervention and control at baseline (see Table 1). Time was treated as a categorical variable. To avoid restrictive assumptions, the covariance of the outcomes at the four assessment times was left unstructured. We fitted the proposed model using a restricted maximum likelihood approach, which produces valid estimates under the missing-at-random assumption.36 This approach correctly handles the additional uncertainty arising from missing data and uses all available data to obtain unbiased estimates for model parameters.37 This is an efficient way for conducting an intent-to-treat analysis since it includes all Ps with a baseline assessment: 94 Ps (9.4%) completed baseline only; 63 (6%) completed baseline and one follow-up; 112 (11.1%) completed baseline and two follow-ups; and 735 (73%) completed baseline and all three follow-up assessments. For cross-sectional analyses (such as percentage of responders at the 3 follow-up times), we used attrition weights to correctly account for those Ps that missed one or more follow-up assessments.38 The statistical software used was SAS version 9. All P values were 2-tailed and are adjusted within outcome measures using Hochberg’s39 correction method to account for multiple comparisons.
Table 1.
Baseline Patient Characteristics by Principal Anxiety Disorder
| GAD (n=549) | PD (n=262) | SAD (N=132) | PTSD (N=61) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n=270 ITV |
n=279 UC |
P | n=126 ITV |
n=136 UC |
P | n=74 ITV |
n=58 UC |
P | n=33 ITV |
n=28 UC |
P | |
| Women % | 71.48 | 73.48 | 0.60 | 71.43 | 65.44 | 0.30 | 64.86 | 67.24 | 0.78 | 84.85 | 78.57 | 0.53 |
| Mean age | 43.99 | 46.02 | 0.366 | 40.60 | 38.75 | 0.24 | 39.81 | 42.09 | 0.35 | 47.45 | 47.32 | 0.97 |
| Education % | 0.58 | 0.09 | 0.04 | 0.99 | ||||||||
| < High School | 5.56 | 6.47 | 6.35 | 2.96 | 5.41 | 3.45 | 6.06 | 7.14 | ||||
| 12 y | 15.19 | 17.99 | 15.87 | 8.89 | 13.51 | 32.76 | 21.21 | 21.43 | ||||
| > 12 y | 79.26 | 75.54 | 77.78 | 88.15 | 81.08 | 63.79 | 72.73 | 71.43 | ||||
| Ethnicity % | 0.04 | 0.04 | 0.88 | 0.16 | ||||||||
| Hispanic | 23.33 | 15.77 | 14.29 | 25.74 | 20.27 | 20.69 | 24.24 | 3.57 | ||||
| African American | 8.52 | 13.26 | 15.08 | 11.76 | 4.05 | 6.90 | 18.18 | 28.57 | ||||
| White | 55.19 | 60.57 | 54.76 | 55.15 | 63.51 | 58.62 | 42.42 | 39.29 | ||||
| Other | 12.96 | 10.39 | 15.87 | 7.35 | 12.16 | 13.79 | 15.15 | 28.57 | ||||
| No. of Chronic Medical Conditions % | 0.20 | 0.80 | 0.85 | 0.29 | ||||||||
| 0 | 21.56 | 15.77 | 22.22 | 24.26 | 25.68 | 25.86 | 12.12 | 3.57 | ||||
| 1 | 20.07 | 20.77 | 22.22 | 24.26 | 28.38 | 24.14 | 15.15 | 28.57 | ||||
| 2 | 58.36 | 64.16 | 55.56 | 51.47 | 45.95 | 50.00 | 72.73 | 67.86 | ||||
| Anxiety Disorder % | ||||||||||||
| Panic | 27.04 | 27.60 | 0.88 | 100.00 | 100.00 | 0.23 | 29.73 | 25.86 | 0.62 | 42.42 | 42.86 | 0.97 |
| Generalized Anxiety | 100.00 | 100.00 | 0.90 | 53.97 | 39.71 | 0.02 | 50.00 | 36.21 | 0.11 | 45.45 | 42.86 | 0.84 |
| Social Phobia | 29.63 | 31.54 | 0.63 | 34.13 | 27.21 | 0.23 | 100.00 | 100.00 | 0.11 | 39.39 | 42.86 | 0.78 |
| Post-traumatic Stress | 12.22 | 12.54 | 0.91 | 15.08 | 11.76 | 0.43 | 9.46 | 17.24 | 0.19 | 100.00 | 100.00 | 0.97 |
| Major Depressive Disorder % | 67.41 | 66.67 | 0.85 | 63.49 | 55.88 | 0.21 | 52.70 | 55.17 | 0.78 | 87.88 | 85.71 | 0.80 |
| No. of Anxiety Disorders % | ||||||||||||
| 1 | 46.30 | 46.95 | 0.88 | 32.54 | 43.38 | 0.07 | 35.14 | 43.10 | 0.35 | 27.27 | 17.86 | 0.39 |
| 2 | 39.63 | 37.28 | 0.57 | 38.10 | 38.24 | 0.98 | 43.24 | 36.21 | 0.41 | 30.30 | 46.43 | 0.20 |
| 3 | 12.96 | 12.90 | 0.98 | 23.02 | 14.71 | 0.09 | 18.92 | 18.97 | 1.00 | 30.30 | 25.00 | 0.65 |
| 4 | 1.11 | 2.87 | 0.16 | 6.35 | 3.68 | 0.33 | 2.70 | 1.72 | 0.71 | 12.12 | 10.71 | 0.86 |
Analyses were conducted to evaluate the degree to which ITV was more effective than UC for each principal anxiety disorder: GAD N = 549; PD N = 262; SAD N = 132; and PSTD N = 61. We additionally analyzed the degree to which ITV was more effective than UC for each comorbid anxiety disorder, after excluding Ps for whom the disorder in question was the principal anxiety disorder, resulting in the following cell sizes: GAD N = 207; PD N = 213; SAD N = 273; and PTSD N = 120. For the principal anxiety disorder analyses, we computed the effect sizes (as defined by Cohen)40 at all waves and compared them across disorders using a t-test.
Results
Sample Selection, Attrition, and Description
Figure 1 depicts study subject flow and reasons for non-eligibility. Two-thirds of referred Ps (1062/1620 [66%]) were eligible for the study, a majority of which (1036/1062 [98%]) consented to participate, and a majority of which (1004/1036 [97%]) were randomized. Study retention was high. Specifically, non-response rates (“no contact” and “cumulative refusals”) ranged from 9.8–14.9 across all four principal anxiety disorders at 6 months, 17.4–22.5 at 12 months and 15.9–24.0 at 18 months. Table 1 shows that most demographic characteristics were similar across ITV and UC within each principal anxiety disorder group. There was some imbalance (at p<.10) in education, ethnicity, number of comorbid anxiety disorders and GAD for PD only, which were used as covariates in the analyses. The sample was about 70% female, with somewhat lower rates for SAD and slightly higher rates for PTSD. The mean age was late 30’s to late 40’s, slightly older in the PTSD group. The majority (64–88%) had 12 years or more of education. The sample was ethnically diverse (36–60% non-white). Many Ps (46–73%) had at least two chronic medical conditions (self- reported), and the majority (53–82%) had more than one anxiety disorder as well as major depressive disorder (53–88%). Those with PTSD had more physical and mental health co-morbidities compared to the other groups.
CALM Participation
Over the one-year intervention, rates of CBT only (32–43%), medication/care management only (3–11%), and CBT plus medication (46–65%) were similar across the four principal anxiety disorder groups, as were the percentage of visits dedicated to CBT versus medication management (X2 (3) = 2.9, ns). Ps who elected CBT were encouraged to complete 6 to 8 CBT sessions over 10 to 12 weeks, but flexibility was permitted. The average number of CBT visits (6.7–8.2) and medication visits (2.1–2.9), and the percentage who completed all visits by 3 months (35–52%) and by 6 months (85–92%), were similar across the four groups.
CBT Integrity
Average ACS adherence to the CALM CBT protocol was 5.0 (+/− 1.3) (on a 7-point scale) with no differences across the four principal anxiety disorder groups, F(3,258)=.62, ns. Similarly, average ACS competency was 5.3 (+/− 1.4) (on a 7-point scale), with no differences across the four principal anxiety disorder groups, F(3, 258)=2.7, ns.
Outcomes
Principal Anxiety Disorder
Table 2 examines trajectories of adjusted means over time for disorder specific measures (GADSS, PDSS, SPIN and PCLC) for each group. For GAD, GADS scores were significantly lower in ITV than UC at 6 (Effect Size or ES=−.33), 12 (ES=−.51) and 18 (ES=−.64) months. For PD, PDSS scores were significantly lower in ITV than UC at 6 (ES=−35) and 12 (ES=−.46) months. For SAD, SPIN scores were significantly lower in ITV than UC at 6 (ES=−.53) months. For PTSD, PCLC scores were not significantly different between ITV and UC at any follow-up assessment, although ESs were of similar magnitude to those of the other disorders: −.29 (6 months), −.43 (12 months) and −.48 (18 months). Effect sizes did not differ significantly across the four groups at any of the follow-up assessments, with one exception; the effect size for GAD was significantly larger than for PD at the 18 month assessment, p < .01.
Table 2.
Adjusted Mean Disorder-Specific Outcome Scores by Principal Anxiety Disorder
| Intervention | Usual Care | Difference(95% CI) | P Value | Effect Size Difference |
|
|---|---|---|---|---|---|
| GADS SCALE (GAD N = 548,481,452,444) | |||||
| Baseline | 13.36(12.91 to 13.80) | 13.72(13.28 to 14.16) | −0.36(−0.99 to 0.27) | 0.260 | −0.08(−0.21 to 0.06) |
| 6 mo | 8.85(8.27 to 9.43) | 10.46(9.89 to 11.03) | −1.61(−2.42 to −0.79) | <.001 | −0.33(−0.50 to −0.16) |
| 12 mo | 7.66(7.03 to 8.29) | 9.99(9.38 to 10.61) | −2.34(−3.22 to −1.45) | <.001 | −0.51(−0.70 to −0.32) |
| 18 mo | 7.27(6.66 to 7.89) | 9.64(9.04 to 10.25) | −2.37(−3.24 to −1.50) | <.001 | −0.64(−0.87 to −0.40) |
| PDSS SCALE (PD N = 262,223,203,199) | |||||
| Baseline | 13.83(12.88 to 14.78) | 13.76(12.85 to 14.68) | 0.07(−1.26 to 1.40) | 0.919 | 0.01(−0.20 to 0.22) |
| 6 mo | 6.05(4.96 to 7.14) | 8.05(6.97 to 9.14) | −2.00(−3.55 to −0.44) | 0.036 | −0.35(−0.62 to −0.08) |
| 12 mo | 5.64(4.53 to 6.75) | 8.35(7.26 to 9.44) | −2.71(−4.29 to −1.14) | 0.003 | −0.46(−0.73 to −0.19) |
| 18 mo | 6.13(4.91 to 7.35) | 7.37(6.15 to 8.59) | −1.24(−2.98 to 0.50) | 0.320 | −0.23(−0.56 to 0.09) |
| SPIN SCALE (SAD N = 132,116,109,111) | |||||
| Baseline | 40.94(38.05 to 43.83) | 41.84(38.55 to 45.13) | −0.90(−5.34 to 3.55) | 0.690 | −0.06(−0.39 to 0.26) |
| 6 mo | 27.42(24.18 to 30.66) | 34.48(30.69 to 38.26) | −7.05(−12.11 to −2.00) | 0.026 | −0.53(−0.91 to −0.15) |
| 12 mo | 25.34(22.13 to 28.55) | 31.05(27.26 to 34.83) | −5.71(−10.74 to −0.68) | 0.080 | −0.42(−0.80 to −0.05) |
| 18 mo | 24.28(20.90 to 27.65) | 28.74(24.84 to 32.65) | −4.46(−9.70 to 0.77) | 0.188 | −0.36(−0.78 to 0.06) |
| PCLC SCALE (PTSD N = 61,55,49,49) | |||||
| Baseline | 57.15(52.86 to 61.43) | 56.90(52.25 to 61.56) | 0.24(−6.24 to 6.72) | 0.941 | 0.01(−0.36 to 0.39) |
| 6 mo | 41.79(35.17 to 48.41) | 46.84(39.79 to 53.89) | −5.05(−14.82 to 4.72) | 0.609 | −0.29(−0.85 to 0.27) |
| 12 mo | 40.31(33.71 to 46.91) | 48.01(40.84 to 55.19) | −7.70(−17.55 to 2.15) | 0.491 | −0.43(−0.99 to 0.12) |
| 18 mo | 40.40(33.95 to 46.85) | 46.07(39.08 to 53.07) | −5.67(−15.29 to 3.95) | 0.609 | −0.48(−1.30 to 0.33) |
Models control for site, education, ethnicity and number of comorbid anxiety disorders. The model for PDSS also controls for presence of co-morbid GAD.
Abbreviations: CI, confidence interval
Intervention by time effects based on the WALD test were significant at p=.007 for PDSS and p <.001 for GADS.
All p-values come from the longitudinal models (e.g., given the estimates of the longitudinal model we obtained the predicted means at the four time points by group and tested their difference at every time point using the correct t-test).
Data are presented as adjusted mean (95% confidence interval)
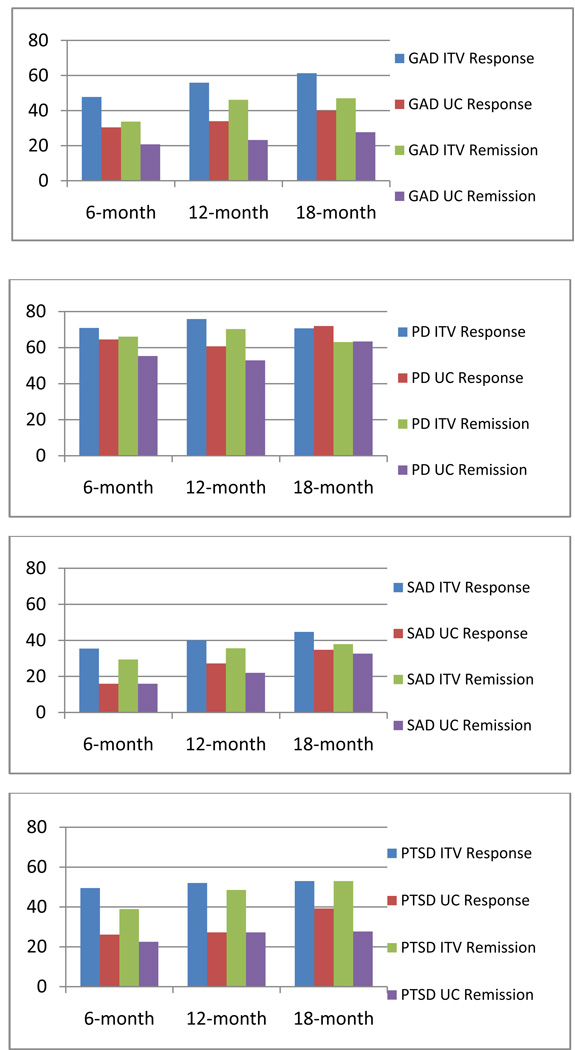
Response and remission rates are presented in Figure 2. For GAD, response rates were significantly greater in ITV than UC at 6 months (p<.001, number needed to treat (NNT) = 5.8; 95% CI = 4.2–9.2), 12 months (p<.001, NNT = 4.6; CI = 3.5–6.5), and 18 months (p<.001, NNT = 4.7; CI = 3.6−6.9). The same pattern occurred for GAD remission rates, at 6 months (p<.01, NNT = 7.7; 95% CI = 5.1−15.4), 12 months (p<.001, NNT = 4.4; CI = 3.4−6.1), and 18 months (p<.001, NNT = 5.2; CI = 3.8−7.9).
Figure 2. Response and remission rates for principal anxiety disorder of GAD, PD, SAD and PTSD.
| GAD | PD |
 GAD ITV Response GAD ITV Response |
 PD ITV Response PD ITV Response |
 GAD UC Response GAD UC Response |
 PD UC Response PD UC Response |
 GAD ITV Remission GAD ITV Remission |
 PD ITV Remission PD ITV Remission |
 GAD UC Remission GAD UC Remission |
 PD UC Remission PD UC Remission |
| SAD | PTSD |
 SAD ITV Response SAD ITV Response |
 PTSD ITV Response PTSD ITV Response |
 SAD UC Response SAD UC Response |
 PTSD UC Response PTSD UC Response |
 SAD ITV Remission SAD ITV Remission |
 PTSD ITV Remission PTSD ITV Remission |
 SAD UC Remission SAD UC Remission |
 PTSD UC Remission PTSD UC Remission |
Description: Figure 2 examines the response and remission rates of the ITV (intervention condition) and the UC (usual care condition). Response was defined as a reduction of 40% or more on each of the scales used. Remission was defined by using cut-off scores when available (PDSS: ≤ 7; SPIN: ≤ 18) or an indication of no more than mild severity averaged across items (PCL-C: ≤ 34; GADSS: ≤ 6; OASIS: ≤ 5).
For PD, response rates were not significantly greater in ITV than UC, although remission rates were significantly greater in ITV than UC at 12 months (p<.03, NNT = 5.7; CI = 3.7–13.3). For SAD, the response rates differed at 6 months (p<.05, NNT = 5.1; CI = 3.1–15.6), although remission rates did not differ at any assessment. Finally, neither response nor remission rates to ITV vs. UC differed significantly for PTSD, although they were numerically comparable to rates for GAD at 6 and 12 months.
Comorbid Anxiety Disorders
Table 3 examines trajectories of adjusted means over time for disorder specific measures (GADSS, PDSS, SPIN and PCLC) for each comorbid anxiety disorder group. There was some imbalance (at p<.10) in age, ethnicity, and number of chronic medical conditions, which were used as covariates in the analyses. Although ESs always favored ITV, scores on the disorder specific measures did not differ significantly between ITV and UC at any follow-up assessment for GAD (ESs=−.18 to −.24), PD (ESs = −.21 to −.33) and PTSD (ESs = −.18 to −.33). Only for SAD were there significant differences, favoring ITV, at 6, 12 and 18 months (ESs = −.29 to −.55).
Table 3.
Adjusted Mean Disorder-Specific Outcome Scores by Comorbid Anxiety Disorders
| Intervention | Usual Care | Difference(95% CI) | P Value | Effect Size Difference |
|
|---|---|---|---|---|---|
| GADS SCALE (GAD N = 207,171,159,162) | |||||
| Baseline | 14.72(14.06 to 15.38) | 14.78(14.00 to 15.56) | −0.06(−1.08 to 0.97) | 0.911 | −0.01(−0.22 to 0.20) |
| 6 mo | 9.74(8.80 to 10.69) | 10.91(9.76 to 12.07) | −1.17(−2.67 to 0.33) | 0.389 | −0.24(−0.54 to 0.07) |
| 12 mo | 9.18(8.23 to 10.14) | 10.37(9.17 to 11.56) | −1.18(−2.71 to 0.35) | 0.389 | −0.24(−0.55 to 0.07) |
| 18 mo | 8.92(7.95 to 9.88) | 9.59(8.40 to 10.78) | −0.67(−2.20 to 0.86) | 0.781 | −0.18(−0.60 to 0.24) |
| PDSS SCALE (PD N = 213,185,165,162) | |||||
| Baseline | 12.73(11.58 to 13.88) | 13.22(12.05 to 14.38) | −0.49(−2.14 to 1.17) | 0.563 | −0.09(−0.38 to 0.21) |
| 6 mo | 6.84(5.64 to 8.05) | 8.46(7.22 to 9.70) | −1.62(−3.37 to 0.13) | 0.210 | −0.25(−0.52 to 0.02) |
| 12 mo | 5.45(4.11 to 6.79) | 7.41(6.04 to 8.78) | −1.96(−3.90 to −0.02) | 0.191 | −0.33(−0.65 to 0.00) |
| 18 mo | 4.73(3.54 to 5.91) | 5.97(4.76 to 7.18) | −1.24(−2.97 to 0.48) | 0.312 | −0.21(−0.50 to 0.08) |
| SPIN SCALE (SAD N = 271,236,207,203) | |||||
| Baseline | 37.31(35.10 to 39.52) | 36.26(34.06 to 38.46) | 1.05(−2.08 to 4.18) | 0.510 | 0.07(−0.15 to 0.29) |
| 6 mo | 25.29(22.67 to 27.92) | 29.55(26.97 to 32.14) | −4.26(−7.96 to −0.56) | 0.048 | −0.29(−0.55 to −0.04) |
| 12 mo | 21.14(18.50 to 23.78) | 29.26(26.66 to 31.86) | −8.12(−11.84 to −4.40) | <.001 | −0.55(−0.80 to −0.30) |
| 18 mo | 20.35(17.73 to 22.96) | 26.57(24.01 to 29.13) | −6.23(−9.90 to −2.55) | 0.003 | −0.48(−0.77 to −0.20) |
| PCLC SCALE (PTSD N = 120,102,91,92) | |||||
| Baseline | 55.27(51.87 to 58.67) | 55.48(52.21 to 58.75) | −0.21(−5.03 to 4.61) | 0.932 | −0.01(−0.30 to 0.28) |
| 6 mo | 41.97(37.78 to 46.15) | 47.64(43.46 to 51.83) | −5.67(−11.69 to 0.34) | 0.256 | −0.33(−0.68 to 0.02) |
| 12 mo | 41.00(36.14 to 45.87) | 45.19(40.35 to 50.04) | −4.19(−11.14 to 2.76) | 0.705 | −0.28(−0.73 to 0.18) |
| 18 mo | 40.07(35.33 to 44.82) | 42.32(37.58 to 47.06) | −2.24(−9.04 to 4.55) | 0.932 | −0.18(−0.71 to 0.36) |
Intervention by Time effects based on the WALD test were significant for SPIN at p <.0001.
All p-values come from the longitudinal models (e.g., given the estimates of the longitudinal model we obtained the predicted means at the four time points by intervention group and tested their difference at every time point using the correct t-test).
Data are presented as adjusted mean (95% confidence interval)
Models control for site, age, ethnicity, and number of chronic medical conditions.
Comment
The primary goals of this study were to evaluate the relative effectiveness of CBT and/or psychotropic medication recommendations compared to UC for each of four anxiety disorders when each presented as a principal anxiety disorder, and the degree to which treatment effects extended beyond the principal disorder to symptoms of comorbid anxiety disorders. The effect sizes indicated that our intervention was superior to usual care at one or more time points in the treatment of each principal anxiety disorder, although effects were not statistically significant for PTSD. Also, effect sizes indicated that our intervention was superior to usual care for comorbid anxiety symptoms, although the only comorbid anxiety to statistically benefit from our intervention over and above usual care was SAD.
The sample was ethnically diverse, medically ill, and highly comorbid in terms of anxiety disorders and major depressive disorder. GAD was the most common principal anxiety disorder (55%), followed by PD (26%), then SAD (13%) and PTSD (6%). Retention in the study and participation in the CALM intervention were relatively similar across the four anxiety disorders. Also, the majority of each anxiety disorder group selected CBT with or without medication. Furthermore, non-expert clinicians (ACSs) were equally successful in adhering to and competently applying CBT across the anxiety disorders when guided by our computerized program. That they were equally capable with PTSD compared to the other disorders highlights the value of the computer-guided program, since it is often generally assumed that PTSD is more difficult than other anxiety disorders for inexperienced therapists. Since most ITV participants completed their treatment by 6 months, the 12 and 18 month follow-up assessments largely assessed sustainability of treatment effects.
In terms of principal anxiety disorder outcomes, ITV was statistically superior to UC across 6 months for GAD, PD and SAD, at 12 months for GAD and PD, and at 18 months for GAD. For PTSD, the results were nonsignificant at each follow-up time point. However, the statistical significance for PTSD comparisons was mitigated by the relatively small sample size, as the effect sizes for PTSD were actually equivalent to the effect sizes for the other principal anxiety disorders, including GAD.
The effect sizes for differences between ITV and UC were low to moderate. However, they are in the range of effect sizes for differences between CBT and other active treatments (such as psychodynamic, interpersonal and supportive therapies) for anxiety disorders (d=.43) 41. Effectiveness trials typically yield lower effect sizes even with the very same treatment protocol because they tolerate more “noise” in attempting to recreate the “real world.” Furthermore, our comparison was made more stringent by the fact that many of the UC group received active CBT or medication treatment: that is, as described in our prior paper, mental health services received were assessed at 6 month, 12 month and 18 month follow-up time points in both ITV and UC groups, and 27–34% of the UC reported receiving CBT with at least 3 elements, and 36–42% reported any appropriate anti-anxiety medication at an appropriate dose for at least 2 months.14 The active nature of UC in this study likely contributed to the low to moderate between-group effect sizes, the pattern of mostly continued improvement in the UC group over time, and the lack of differences between ITV and UC for PD and SAD groups at the 18 month time point. At the same time, these effects likely represent what would be achieved in real world practice, where therapeutic alternatives must realistically be compared with other therapeutic options patients might pursue.
Nonetheless, the effect sizes indicated that our evidence-based intervention tailored to primary care was more effective than UC for each principal anxiety disorder, at least out to 12 months after study entrance. The results with GAD were the strongest both statistically and in terms of effect sizes, which is particularly important since GAD is among the most commonly presenting anxiety disorders in primary care.5,42 The GAD effects were confirmed when analyzing response and remission rates where ITV was significantly superior to UC at each time point.
This is the first study to evaluate differences in intervention effects relative to UC on comorbid disorder outcomes in a generalizable sample and using dimensional measures of comorbidity. Measures of comorbid symptom severity typically improved over time. Also, the effect sizes of differences between ITV and UC (e.g., .24 to .55) indicated that comorbidity decreased more in ITV than UC at 6 and 12 months. However, only in the case of SAD in CALM did the changes statistically exceed improvements in UC. Conceivably, study participation itself served as an effective treatment for comorbid SAD, since regular contact with study personnel and particularly the ACS probably functioned as exposure therapy to social situations. Also, statistical significance between ITV and UC for GAD, PTSD and PD symptoms may have been mitigated by sample size, and/or an overall improvement in comorbid symptoms due to either nonspecific treatment effects shared between ITV and UC or the passage of time alone. By relying upon no-treatment control comparisons, prior studies of CBT17,18,20,21,22,26 were unable to attribute the effects on comorbidity specifically to CBT versus treatment in general. Overall, the current comorbidity findings are promising and encourage further investigation. Since this study was designed to compare the CALM intervention to UC while mimicking “real world” conditions, the data have some limitations. For example, independent diagnostic assessments were not made at each follow-up. The disorder-specific symptom scales may have been differentially sensitive to change, thus rendering comparisons across disorders problematic. Furthermore, the design does not permit dismantling of the degree to which intervention effects were attributable to specific components of the CALM intervention, such as CBT and psychotropic medications.
In summary, the CALM intervention had a greater positive effect on symptoms of principal anxiety disorders relative to UC in this primary care sample. In addition, the CALM intervention tended to have a greater positive effect on all comorbid symptoms, but the effects were only statistically significant for comorbid social anxiety symptoms. While the overall improvement in comorbid symptoms is good news for clinical practice, future research may address whether sequential treatment initially targeting a principal anxiety disorder followed by targeting comorbid disorders yields even stronger benefits for comorbid symptoms. An alternative option of simultaneous delivery of more than one targeted CBT program has not been supported in the treatment of comorbid anxiety disorders26 or comorbid anxiety and substance use disorders43 although unified CBT protocols44 may prove more effective. These are questions for future research.
Acknowledgment
Funding/Support: This work was supported by the following National Institute of Mental Health grants: U01 MH070018, U01 MH058915, U01 MH057835, UO1 MH057858, U01 MH070022, K24 MH64122, and K24 MH065324. The NIMH (as part of the U01 mechanism) was responsible for monitoring the operations and conduct of the study and reviewing and approving the manuscript.
Scientific Advisory Board: Frank Verlain deGruy III, MD, MSFM (Department of Family Medicine, University of Colorado Denver School of Medicine, Aurora); Wayne Katon, MD, and Jürgen Unützer, MD, MPH, MA (Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine, Seattle); Lisa V. Rubenstein, MD, MSPH (Department of Medicine, David Geffen School of Medicine and VA Greater Los Angeles Center of Excellence for the Study of Healthcare Provider Behavior, University of California, Los Angeles; and RAND Corporation, Santa Monica, California); Kenneth Wells, MD, MPH (Jane and Terry Semel Institute for Neuroscience and Human Behavior and Department of Psychiatry and Biobehavioral Sciences, David Geffen School of Medicine, University of California, Los Angeles; Department of Health Services, UCLA School of Public Health; and RAND Corporation, Santa Monica, California). These board members received compensation for their consultation.
Ethnic Advisory Board: Peter J. Guarnaccia, PhD (Department of Human Ecology and the Institute for Health, Health Care Policy and Aging Research, Rutgers University, New Brunswick, New Jersey); Maga Jackson-Triche, MD, MSHS (VA Northern California Health Care System and University of California Davis School of Medicine, Sacramento);Jeanne Miranda,PhD (Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles); David T. Takeuchi, PhD (School of Social Work and Department of Sociology, University of Washington, Seattle). These board members received compensation for their consultation.
Anxiety Clinical Specialists: Skye M. Adams, LMSW, and Sandy Sanders, MSW, LCSW (University of Arkansas for Medical Sciences, Little Rock); Michelle Behrooznia, MA, Shadha Hami Cissell, MSW, and Michele S. Smith, PhD (University of California, San Diego); Cindy Chumley (High Desert Medical Group, Lancaster, California); Laura Constantinides, RN (Southern California Permanente Medical Group, San Diego County); Margie Fort, MSW, LICSW, Alice S. Friedman, MSN, ARNP, Kelly H. Koo, MS, Molly Roston, MSW, and Jodi Rubinstein, LICSW (University of Washington, Seattle); James W. Miller, MA, CRC (Desert Medical Group, Palm Springs, California); Angelica Ruiz, CCRC (Desert Oasis Healthcare, Palm Desert, California). These individuals were compensated for their work on the project.
Supervising Psychiatrists: C. Winston Brown, MD, Mohit Chopra, MD, and Dan-Vy Mui, MD (University of Arkansas for Medical Sciences, Little Rock); James W. Gaudet, MD (Southern California Permanente Medical Group, San Diego County); Stuart Levine, MD, MHA (University of California, Los Angeles, and HealthCare Partners, Torrance, California); R. ChristopherSearles, MD (University of California, San Diego); Jason P. Veitengruber, MD (University of Washington at Harborview Medical Center, Seattle). These individuals were compensated for their work on the project.
Primary Care Clinic Champions: Lee C. Abel, MD (Little Rock Diagnostic Clinic, Little Rock, Arkansas); Basil Abramowitz, MD, and Stacey Coleman, DO (Sharp Rees Stealy, San Diego County, California); Lisa D. Chew, MD, MPH, and Robert Crittendon, MD (Harborview Medical Center, Seattle, Washington); Matthew G. Deneke, MD (University of Arkansas for Medical Sciences, Little Rock); Anne M. Eacker, MD (University of Washington Medical Center Roosevelt, Seattle); Erwin Guzman, MD (Southern California Permanente Medical Group, San Diego County); Ralph Joseph, MD (St. Vincent’s Family Clinic, Little Rock, Arkansas); Gene A. Kallenberg, MD (University of California, San Diego); Richard Kovar, MD, FAAFP, and Carrie Rubenstein, MD (Country Doctor Community Health Centers, Seattle, Washington); T. Putnam “Putter” Scott, MD (Neighborcare Health, Seattle, Washington); Ivan Womboldt, CRCC (Desert Medical Group, Palm Springs, California). These individuals were compensated for work on this project either directly or via administrative fee payments to their clinics.
RAND Survey Research Group: Barbara Levitan, BA (RAND Corporation, Santa Monica, California. Ms. Levitan was compensated for work on this project.
Translators:
Velma Barrios, MA (University of California, Los Angeles); Avelina Martinez, MAT, ATA-Certified Translator from English into Spanish (Austin, Texas). These individuals were compensated for their work on this project.
Proficiency Raters:
Laura B. Allen, PhD, and Ancy E. Cherian, PhD (University of California, LosAngeles). These individuals were compensated for their work on this project.
Analysis: Bernadette Benjamin, MS (RAND Corporation, Santa Monica, California); Jutta M. Joesch, PhD, and Imara I. West, MPH (University of Washington, Seattle). These individuals were compensated for their work on the project.
Programming of Web-based Outcomes System: Youlim Choi, MS (University of Washington, Seattle). Mr Choi was compensated for his work on this project.
Programming of Computer CBT Program: Vivid Concept LLC (http://www.vividconcept.com).
Study Coordinators:
Kristin Bumgardner, BS (University of Washington, Seattle and central coordination of overall study); Daniel Dickson, BA, Daniel Glenn, BA, and Michael E. J. Reding, MA (University of California, Los Angeles); Christina Reaves, MPH (University of Arkansas for Medical Sciences, Little Rock). These individuals were compensated for their work on the project.
National Institute of Mental Health:
Matthew V. Rudorfer, MD (Adult Treatment and Preventive Interventions Research Branch, Division of Services and Intervention Research, National Institute of Mental Health, National Institutes of Health, Bethesda, MD) and Elizabeth Zachariah, MS (Clinical Trials Operations and Biostatistics Unit, Division of Services and Intervention Research, National Institute of Mental Health, National Institutes of Health, Bethesda, Maryland).
Footnotes
The discrepancy between the MINI “most troubling disorder” and first CBT session primary target is unclear, although unreliability in patient ratings and/or waxing and waning of symptoms from the time of the MINI interview to the first CBT session may account for the differences.
The content manual is available upon request from the first author
The proficiency manual is available upon request from the first author
Adherence manual is available upon request from the first author
Author Contributions: Dr. Craske had full access to the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, Severity, and Comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saarni SJ, Suvisaari J, Sintonen H, Pirkola S, Koskinen S, Aromaa A, Lonnqvist J. Impact of psychiatric disorders on health-related quality of life. Br J Psychiatry. 2005;190:326–332. doi: 10.1192/bjp.bp.106.025106. [DOI] [PubMed] [Google Scholar]
- 3.Sareen J, Jacobi F, Cox BJ, Belik SL, Clara I, Stein MB. Disability and poor quality of life associated with comorbid anxiety disorders and physical conditions. Arch Intern Med. 2006;166:2109–2116. doi: 10.1001/archinte.166.19.2109. [DOI] [PubMed] [Google Scholar]
- 4.Stein MB, Roy-Byrne PP, Craske MG, Bystritsky A, Sullivan G, Pyne JM, Wayne K, Sherbourne C. Functional Impact and Health Utility of Anxiety Disorders in Primary Care Outpatients. Medical Care. 2005;43(12):1164–1170. doi: 10.1097/01.mlr.0000185750.18119.fd. [DOI] [PubMed] [Google Scholar]
- 5.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez A, Haro JM, Martinez-Alonso M, Demyttenaere K, Brugha TS, Autonell J, De Girolamo G, Bernert S, Lepine JP, Alonso J. Treatment adequacy for anxiety and depressive disorders in six European countries. Br J Psychiatry. 2007;190(2):172–173. doi: 10.1192/bjp.bp.106.023507. [DOI] [PubMed] [Google Scholar]
- 7.Weisberg RB, Dyck I, Culpepper L, Keller MB. Psychiatric treatment in primary care patients with anxiety disorders: A comparison of care received from primary care providers and psychiatrists. Am J Psychiatry. 2007;164(2):276–282. doi: 10.1176/appi.ajp.164.2.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 9.Carroll KM, Rounsaville BJ. A vision of the next generation of behavioral therapies research in the addictions. Addiction. 2007;102(6):850–862. doi: 10.1111/j.1360-0443.2007.01798.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gega L, Norman IJ, Marks IM. Computer-aided vs. tutor-delivered teaching of exposure therapy for phobia/panic: Randomized controlled trial with pre-registration nursing students. Int J Nurs Stud. 2007;44(3):397–405. doi: 10.1016/j.ijnurstu.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet-based congnitive behaviour therapy for symptoms of depression and anxiety: A meta-analysis. Psychol Med. 2007;37(3):319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- 12.Roy-Byrne P, Veitengruber JP, Bystritsky A, Edlund MJ, Sullivan G, Craske MG, Welch SS, Rose R, Stein MB. Brief intervention for anxiety in primary care patients. J Am Board Fam Med. 2009;22(2):175–186. doi: 10.3122/jabfm.2009.02.080078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagner EH, Glasgow RE, Davis C, Bonomi AE, Provost L, McCulloch D, Carver P, Sixta C. Quality improvement in chronic illness care: a collaborative approach. JT Comm J Qual Improv. 2001;27:63–80. doi: 10.1016/s1070-3241(01)27007-2. [DOI] [PubMed] [Google Scholar]
- 14.Roy-Byrne P, Craske MG, Sullivan G, Rose RD, Edlund MJ, Lang AJ, Bystritsky A, Welch SS, Chavira DA, Golinelli D, Campbell-Sills L, Sherbourne CD, Stein MB. Delivery of Evidence-Based Treatment for Multiple Anxiety Disoders in Primary Care. JAMA. 2010;303(19):1921–1928. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jacobi F, Wittchen H-U, Holting C, Hofler M, Pfister H, Muller N, Lieb R. Prevalence, co-morbidity and correlates of mental disorders in the general population: Results from the German Health Interview and Examination Survey (GHS) Psychol Med. 2004;34(4):597–611. doi: 10.1017/S0033291703001399. [DOI] [PubMed] [Google Scholar]
- 16.Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. J Abnorm Psychol. 1998;107(2):179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- 17.Borkovec TD, Abel JL, Newman H. Effects of psychotherapy on comorbid conditions in generalized anxiety disorder. J Consult Clin Psychol. 1995;63(3):479–483. doi: 10.1037//0022-006x.63.3.479. [DOI] [PubMed] [Google Scholar]
- 18.Brown TA, Barlow DH. Long-term outcome in cognitive-behavioral treatment of panic disorder: Clinical predictors and alternative strategies for assessment. J Consult Clin Psychol. 1995;63(5):754–765. doi: 10.1037//0022-006x.63.5.754. [DOI] [PubMed] [Google Scholar]
- 19.Craske MG, Farchione TJ, Allen LB, Barrios V, Stoyanova M, Rose R. Cognitive behavioral therapy for panic disorder and comorbidity: More of the same or less of more? Behav Res Ther. 2007;45(6):1095–1109. doi: 10.1016/j.brat.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 20.Stanley MA, Beck JG, Glasco JD. Treatment of generalized anxiety in older adults: A preliminary comparison of cognitive-behavioral and supportive approaches. Behav Ther. 1996;27(4):565–581. [Google Scholar]
- 21.Tsao JCI, Lewin MR, Craske MG. The effects of cognitive-behavior therapy for panic disorder on comorbid conditions. J Anxiety Disord. 1998;12(4):357–371. doi: 10.1016/s0887-6185(98)00020-6. [DOI] [PubMed] [Google Scholar]
- 22.Tsao JCI, Mystkowski JL, Zucker BG, Craske MG. Effects of cognitive-behavioral therapy for panic disorder on comorbid conditions: Replication and extenstion. Behav Ther. 2002;33(4):493–509. [Google Scholar]
- 23.Sullivan G, Craske MG, Sherbourne C, Edlund MJ, Rose RD, Golinelli D, Chavira DA, Bystritsky A, Stein MB, Roy-Byrne PP. Design of the Coordinated Anxiety Learning and Management study: Innovations in collaborative care for anxiety disorders. Gen Hosp Psychiat. 2007;29(5):379–387. doi: 10.1016/j.genhosppsych.2007.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Campbell-Sills L, Norman SB, Craske MG, Sullivan G, Lang AJ, Chavira DA, Bystritsky A, Sherbourne C, Roy-Byrne P, Stein MB. Validation of a brief measure of anxiety-related severity and impairment: The Overall Anxiety Severity and Impairment Scale (OASIS) J Affect Disorders. 2009;112:92–101. doi: 10.1016/j.jad.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 26.Craske MG, Rose RD, Lang A, Welch SS, Campbell-Sills L, Sullivan G, Sherbourne C, Bystritsky A, Stein MB, Roy-Byrne PP. Computer-assisted delivery of cognitive behavioral therapy for anxiety disorders in primary-care settings. Depress Anxiety. 2009;26(3):235–242. doi: 10.1002/da.20542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Houck PR, Speigel DA, Shear MK, Rucci P. Reliability of the self-report version of the Panic Disorder Severity Scale. Depress Anxiety. 2002;15(4):183–185. doi: 10.1002/da.10049. [DOI] [PubMed] [Google Scholar]
- 29.Andreescu C, Belnap BH, Rollman BL, Houck P, Ciliberti C, Mazumdar S, Shear MK, Lenze EJ. Generalized Anxiety Disorder Severity Scale validation in older adults. Am J Geriat Psychiatry. 2008;16(10):813–818. doi: 10.1097/JGP.0b013e31817c6aab. (2008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weiss BJ, Calleo J, Rhoades H, Novy DM, Kunik ME, Lenze EJ, Stanley MA. The utility of the Generalized Anxiety Disorder Severity Scale (GADSS) with older adults in primary care. Depress Anxiety. 2009;26(1):E10–E15. doi: 10.1002/da.20520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shear K, Belnap BH, Mazumdar S, Houck P, Rollman BL. Generalized anxiety disorder severity scale (GADSS): A preliminary validation study. Depress Anxiety. 2006;23(2):77–82. doi: 10.1002/da.20149. [DOI] [PubMed] [Google Scholar]
- 32.Connor KM, Davidson JRT, Churchill LE, Sherwood A, Foa E, Weisler RH. Psychometric properties of the Social Phobia Inventory (SPIN): New self-rating scale. Br J Psychiatry. 2000;176:379–386. doi: 10.1192/bjp.176.4.379. [DOI] [PubMed] [Google Scholar]
- 33.Weathers PL, Furlong MJ, Solorzano D. Mail survey research in counseling psychology: Current practice and suggested guidelines. J Couns Psychol. 1993;40(2):238–244. [Google Scholar]
- 34.Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric Properties of the PTSD Checklist--Civilian Version. J Trauma Stress. 2003;16(5):495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- 35.Ravindran L, Stein MB. The pharmacological treatment of anxiety disorders: A review of progress. J Clin Psychiatry. 2010;71(7):839–854. doi: 10.4088/JCP.10r06218blu. [DOI] [PubMed] [Google Scholar]
- 36.Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS System for Mixed Models. Cary, NC: SAS Publications; 1996. [Google Scholar]
- 37.Little RJA, Rubin DB. Statistical analysis with missing data. New York: John Wiley & Sons; 1987. [Google Scholar]
- 38.Brick JM, Kalton G. Handling Missing Data in Survey Research. Stat Methods Med Res. 1996;5(3):215–238. doi: 10.1177/096228029600500302. [DOI] [PubMed] [Google Scholar]
- 39.Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometnika. 1988;75(4):800–802. [Google Scholar]
- 40.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Vol. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 41.Tolin DF. Is cognitive-behavioral therapy more effective than other therapies? A meta-analytic review. Clinical Psych Review. 2010 doi: 10.1016/j.cpr.2010.05.003. (in press) [DOI] [PubMed] [Google Scholar]
- 42.Weisberg RB. Overview of generalized anxiety disorder: epidemiology, presentation, and course. J Clin Psychiatry. 2009;70 suppl 2:4–9. [PubMed] [Google Scholar]
- 43.Randall CL, Thomas S, Thevos AK. Concurrent alcoholism and social anxiety disorder: A first step toward developing effective treatments. Alcoholism. 2001;25(2):210–220. [PubMed] [Google Scholar]
- 44.Barlow DH, Allen LB, Choate ML. Toward a Unified Treatment for Emotional Disorders. Behav Ther. 2004;35(2):205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]