Abstract
Purpose
The purpose of this study is to better understand the utilization of anterior acromioplasty over time – in the absence of rotator cuff repair, to examine the relationship to patient characteristics (age, sex) and types of rotator cuff pathology (inflammation or fibrosis, partial thickness tearing, full thickness tearing undergoing debridement), and to assess the utilization of arthroscopy in this procedure.
Methods
Using the resources of the Rochester Epidemiology Project, cataloging medical records of residents in Olmsted County, Minnesota, we identified 246 patients who underwent anterior acromioplasty between 1980 and 2005. It has previously been shown that rarely does a resident of Olmsted County undergo an orthopedic procedure at a facility outside the county.
Results
The incidence of anterior acromioplasty increased over time (p<0.001) with the crude rate of 3.3 per 100,000 in 1980 to 1985 to 19.0 per 100,000 in 2000 to 2005. Sex, age, and types of rotator cuff pathology did not significantly change over the twenty-six year period. There was a dramatic shift from use of the open to the arthroscopic approach over this time period (p<0.001) and a decrease in the concomitant performance of distal clavicle resection (p<0.001).
Conclusions
The frequency of anterior acromioplasty has dramatically increased over time. Increasing knowledge about this syndrome, including better imaging, has facilitated patient treatment for a stable spectrum of rotator cuff pathology (inflammation or fibrosis, partial thickness tearing, full thickness tearing undergoing debridement), as has the application of endoscopic surgery.
Introduction
Impingement syndrome describes pain related to narrowing of the supraspinatus outlet and lesions of the rotator cuff, subacromial bursa, and long head of the biceps. This crowding of structures creating symptoms of impingement was initially ascribed to changes on the undersurface of the anterior acromion and acromioclavicular joint, with the procedure of anterior acromioplasty commonly performed to surgically address this symptom complex (1). This procedure, anterior acromioplasty, described by Charles Neer in 1972 has been cited over 800 times in various scientific journals (2). Diagnosis is variable with numerous specialized clinic tests and imaging studies; however, there is lack of a gold standard. Clinical findings and correlation with diagnostic studies are not always supportive of the diagnosis of the impingement syndrome (3). At our institution, anterior acromioplasty is used in conjunction with rotator cuff repair but also for the management of chronic symptoms due to bursal thickening with inflammation or fibrosis, chronic focal rotator cuff tendonitis, partial thickness rotator cuff tears not requiring repair, or for a large, unrepairable rotator cuff tear associated with subacromial crepitus.
The purpose of this study is to understand the utilization of anterior acromioplasty over time in the absence of rotator cuff repair, to examine the relationship to patient characteristics (age and sex) and the types of rotator cuff pathology treated and to assess the effect of the advent of arthroscopic techniques on the utilization of this procedure. By applying epidemiologic methods, to include incidence, frequency, and associated patient characteristics who underwent anterior acromioplasty, we hypothesized that patient characteristics and the types of rotator cuff pathology, as outlined above, would remain stable over time, but the frequency of this surgical procedure would increase with the application of arthroscopic techniques.
Materials and Methods
Approval for this project was obtained from the institutional review boards of 2 institutions, the Mayo Clinic and the Olmsted Medical Center. The Mayo Clinic is an academic, tertiary care center. Olmsted Medical Center is a private hospital serving the residents of Olmsted County. Using the resources of the Rochester Epidemiology Project which catalogs medical records of residents of Olmsted County, Minnesota, we were able to identify patients undergoing either open or arthroscopic anterior acromioplasty. Records of procedures performed are also available through the Rochester Epidemiology Project, a cooperative venture by which the incidence and epidemiology of diseases and procedures may be studied (4-9). Previous patient series have demonstrated the Olmsted County experience provides a reasonable estimate for national use of various medical procedures. Likewise, it has been shown that rarely does a resident of Olmsted County undergo an orthopedic procedure at a facility outside the county (4-6,8,9).
For this review, a computer search of procedural coding was conducted for the study years 1980 to 2005 for all acromioplasty procedures performed on patients residing in Olmsted County, Minnesota. Data was abstracted from the medical records. Inclusion criteria were defined as cases in which patients underwent removal of the anteroinferior portion of the acromion process either via an open incision or with the use of an arthroscope. Patients also having debridement of the bursa, the rotator cuff, the glenoid labrum, or distal clavicle excision were included. These procedures were considered adjunctive to the anterior acromioplasty. Patients undergoing more extensive reconstruction including rotator cuff repair, excision of calcific deposits, glenoid labrum repair or biceps tenotomy or tenodesis were excluded. Patients with bilateral acromioplasties were counted once. Two-hundred and forty-six cases were identified fulfilling the inclusion criteria. Patient characteristics, to include age, sex, affected side, bilateral presentation, as well as types of rotator cuff pathology, open versus arthroscopic acromioplasty, and accompanying surgical procedures were obtained from the medical and surgical records of the study patients. Preoperative nonsurgical treatment was not evaluated.
Statistical Methods
Descriptive statistics are reported as percentage or standard deviation as appropriate. The univariate association between type of rotator cuff disease and surgical approach, dependent variable, was assessed using logistic regression, surgical approach defined as open or arthroscopic. Results are reported as odds ratio and 95% confidence interval. This analysis included only shoulder procedures (both open and arthroscopic) from the period 1991 to 2005 since all procedures done prior to 1991 were done in an open manner.
The univariate associations of surgical approach, distal clavicle resection and type of rotator cuff lesion with year of anterior acromioplasty were assessed using the Kruskal-Wallis test.
Annual incidence rates for anterior acromioplasty were estimated by dividing the number of events by the population at risk, with direct standardization to the age and sex distribution of the US White population. The population at risk was estimated by linear interpolation of decennial census data for Olmsted County assuming the entire population of the county to be at risk (10). The 95% confidence intervals were estimated assuming a Poisson distribution for the number of age, sex, and calendar year-specific cases. A Poisson regression analysis was used to assess the association of age, gender, and calendar year with the crude incidence rates.
Results
Two hundred and forty-six patients with 246 operated shoulders had anterior acromioplasty during this period and were included in this study group. Ninety-six patients underwent an open anterior acromioplasty and 150 underwent an arthroscopic anterior acromioplasty. In twenty-one of these patients a contralateral anterior acromioplasty was done at some point in time but are not a part of this analysis. Only the earliest affected side was incorporated into the data analysis. There were 157 men and 89 women in the study group. All patients were greater than 17 years of age. The mean age of patients undergoing acromioplasty was 47 years. There was a median age of 46 years (range 18 to 79 years) in those undergoing open acromioplasty and a median age of 47 years (range 18 to 81 years) in those undergoing arthroscopic acromioplasty.
There were twenty-four surgeons who performed acromioplasty over this 26 year period. The frequency of the procedure changed over time. Between 1980 and 1995, the number of procedures was fairly stable. It increased dramatically thereafter (Fig. 1). The procedure used for anterior acromioplasty changed significantly over the 26 years of this study (p<0.001). One hundred percent of the 20 surgeries done between 1980 and 1990 were in the open manner, while the proportion of surgeries done as an open procedure in the later two time periods, 1996 to 2000 and 2001 to 2005, were only 28 of 72 (38.9%) and 28 of 125 (22.4%) respectively (Fig. 2).
Figure 1.
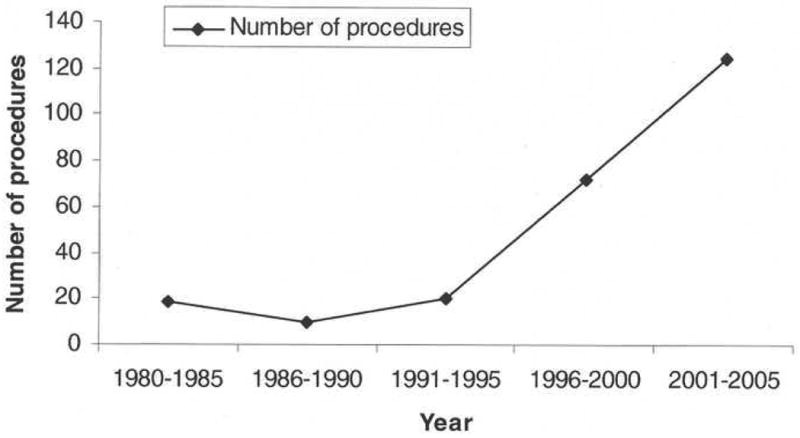
Frequency of anterior acromioplasty in Olmsted County, Minnesota over the period 1980 to 2005.
Figure 2.
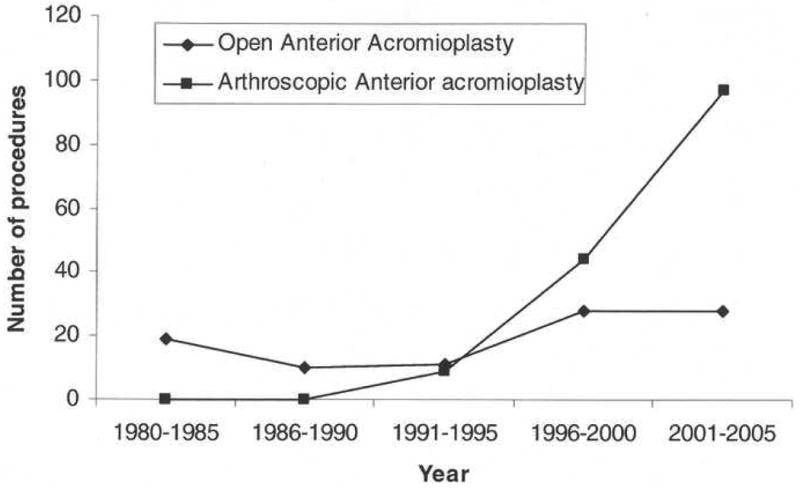
The surgical method of anterior acromioplasty. The frequency of the open procedure increased only slightly over time. Utilization of the arthroscopic method increased dramatically after 1991 and accounts for most of the increased utilization of acromioplasty as a procedure.
Rotator cuff lesions were defined in four categories based on review of the intraoperative report by the surgeon. Definition of rotator cuff lesions was at the discretion of the surgeon. No rotator cuff tearing, inflammation or fibrosis only, was present in ninety-four. The rotator cuff was frayed, or thin, in 79. There was partial thickness rotator cuff tearing in 58 and there was full thickness rotator cuff tearing that underwent debridement but not repair in 15. Of those with no rotator cuff tearing but inflammation or fibrosis only the procedure was done open in 48 and arthroscopically in 46. Of those with rotator cuff fraying the procedure was done open in 33, and arthroscopically in 46. Of those with partial thickness rotator cuff tearing the procedure was done open in 10 and arthroscopically in 48. Of those with full thickness rotator cuff tears not undergoing repair the procedure was done open in 6 and arthroscopically in 9. For each type of rotator cuff lesion, the number increased over the period of the study; however, the distribution among types of rotator cuff lesions did not change significantly with time (p<0.31) (Fig. 3).
Figure 3.
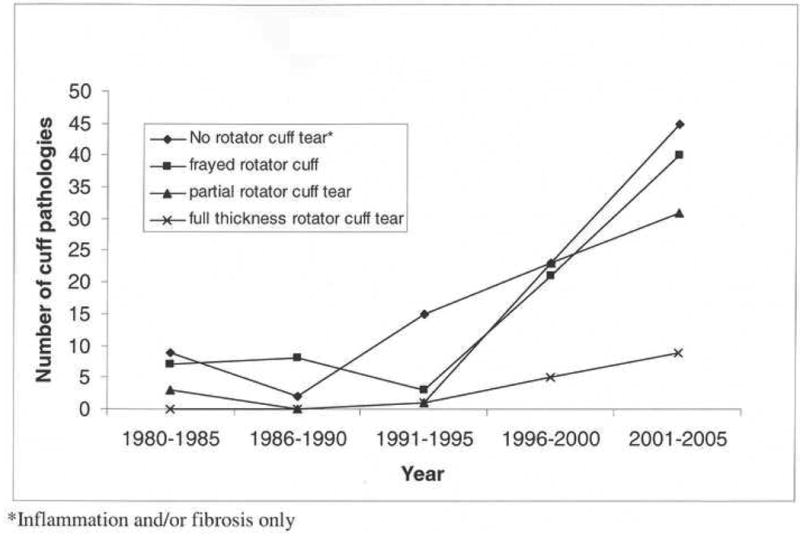
The type of rotator cuff pathology observed at the time of anterior acromioplasty. The frequency of acromioplasty with each type of lesion increased over time without a change in the distribution of problems encountered (p<0.31).
The frequency of use for each type of rotator cuff lesion encountered increased over time with a dramatic change in frequency beginning in 1991. There was significant association between type of rotator cuff tear and the surgical procedure employed (p<0.001), restricting this assessment to only those years, 1991 to 2005. There was a significantly greater odds of a shoulder with a partial cuff tear, relative to a shoulder with no tear, to have an arthroscopic procedure, odds ratio of 5.3. The odds were increased, though not significantly, for a patient with a frayed tendon as well as a full thickness tear (relative to a shoulder with no tear) to have an arthroscopic procedure, odds ratio 2.0 and odds ratio 1.1 respectively.
In 101 shoulders there was simultaneous distal clavicle resection. This adjunctive procedure was performed in 51% of the open group and 49% of the arthroscopically treated group. The frequency of combined acromioplasty and distal clavicle excision remained fairly stable between 1980 and 1991. Thereafter the frequency of distal clavicle excision increased but to a lesser extent than the increase in frequency of anterior acromioplasty (Fig. 4). Over the study period, the proportion of shoulders having a concomitant distal clavicle resection significantly decreased with time (p<0.01), from 63% and 70% of surgical procedures in the periods 1980 to 1985 and 1986 to 1990 to only 32% of surgical procedures in the last 5 years of the study.
Figure 4.
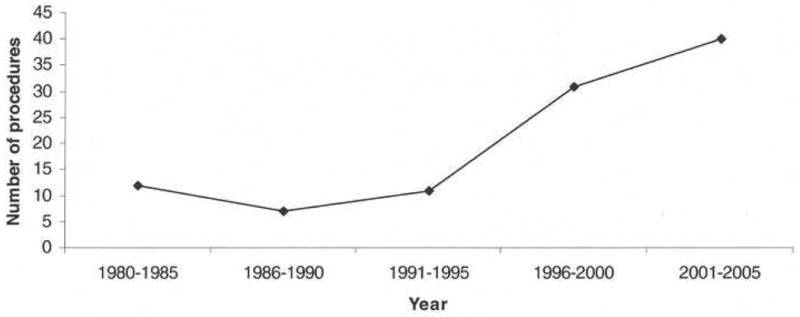
The number of shoulders undergoing distal clavicle excision increased over time but to a lesser extent than the increase in the number of acromioplasty procedures. Thus, the proportion of shoulders undergoing concomitant distal clavicle excision decreased over time (p<0.01).
A significant association with gender was observed (p<0.001) (Fig. 5) with overall age-adjusted annual incidence among males (12.3 per 100,000, 95% confidence interval 10.4 to 14.3) significantly higher than among females (6.7 per 100,000, 94% confidence interval 5.3-8.1). A significant association with age was also seen (p<0.001), the highest incidence rate (19.1 per 100,000 person years) was observed in the patients aged 41 to 64 years (Fig 6).
Figure 5.
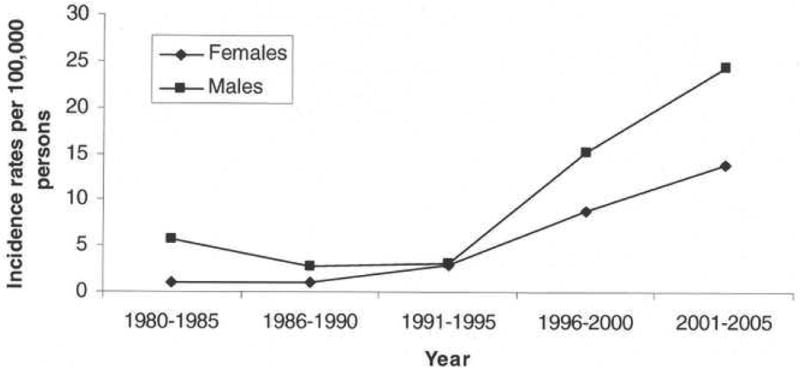
The overall incidence among men was higher than among women (p<0.001).
Figure 6.
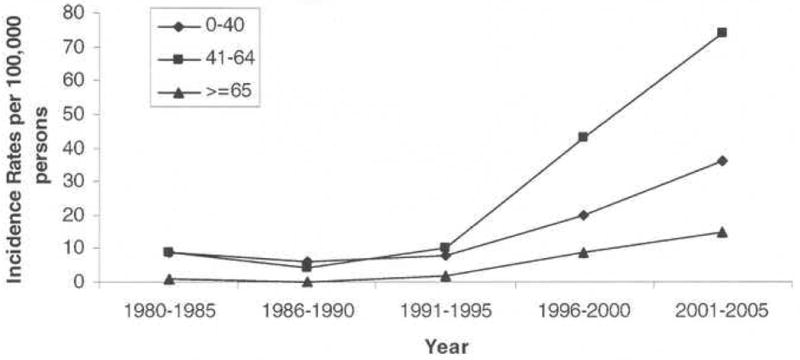
The overall incidence differed amongst age groups with the highest incidence in patients age forty-one to sixty-four years.
There was a significant increase in the incidence of anterior acromioplasty over the 26 year period (p<0.001). The overall age and sex adjusted incidence rate of acromioplasty in Olmsted County between 1980 and 2005 was 9.4 per 100,000 person years. Based on the nature of the population of Olmsted County, the incidence rate was projected for the United States white population using the 2000 census (Table 1). When age and sex was adjusted to the 2000 U.S. white population, the rate of acromioplasty in the first 16 years was relatively stable and then increased to a rate of 20.0 per 100,000 person years for 2001 to 2005.
Table I. Incidence rates of anterior acromioplasty for the five time periods by sex and age groups.
| Incidence of anterior acromioplasty per 100,000 persons | 1980-1985 | 1986-1990 | 1991-1995 | 1996-2000 | 2001-2005 | |
|---|---|---|---|---|---|---|
| Olmsted County Total* | 3.3 | 1.9 | 3.0 | 11.9 | 19.0 | |
| Sex | Male | 5.8 | 2.8 | 3.1 | 15.2 | 24.5 |
| Female | 1.0 | 1.1 | 2.9 | 8.8 | 13.8 | |
| Age | ≤40 | 2.3 | 1.7 | 1.8 | 5.4 | 9.0 |
| 41-64 | 7.3 | 3.4 | 6.1 | 25.8 | 39.4 | |
| ≥65 | 1.8 | 0.0 | 2.9 | 14.0 | 21.2 | |
| US White Population Total** | 3.8 | 2.0 | 3.3 | 12.8 | 20.0 | |
Crude incidence per 100,000 person years for Olmsted County
Incidence per 100,000 person year age- and sex-adjusted to 2000 US White Population
Discussion
The impingement syndrome is accepted to be relatively common; however, no information is available regarding the incidence of surgical treatment, namely open or arthroscopic anterior acromioplasty. It has also not been known how this treatment has changed over time. The purpose of this study was to better understand the utilization of anterior acromioplasty over the past quarter of a century, its relationship to surgical technique, patient characteristics, and shoulder disease. Over the past 26 years the incidence of anterior acromioplasty regardless of procedure method has increased more than six-fold in overall utilization in this study. The landmark article on anterior acromioplasty was by Neer in 1972 describing the open procedure (1). Earlier surgical procedures including acromioplasty or acromionectomy had inconsistent results and were infrequently performed. Ellman in 1987 published the results of the arthroscopic approach to anterior acromioplasty (11). In this study both open and arthroscopic acromioplasty increased over time, but the frequency of the arthroscopic approach has increased dramatically (p<0.001). Early in the study none of the acromioplasties were performed arthroscopically. By the early 2000's approximately 78% of the acromioplasties were performed by an arthroscopic approach.
Although the clinical use of anterior acromioplasty for the treatment of shoulder pain has changed, the distribution of the types of rotator cuff lesions treated over time has remained relatively constant whether treated by the open or arthroscopic method. In our study, the definition of rotator cuff lesions was at the discretion of the surgeon. Arthroscopy allowed for visualization of both extra- and intra-articular rotator cuff pathology, whereas interpretation of the extent of rotator cuff tearing on open procedures was limited to observation of the rotator cuff tearing at surgery plus the surgeon's knowledge of the findings on MRI (becoming commonly used in the early 1990's) or contrast arthrography. In Neer's subsequent article in 1982, he further classified the progressive three stages of impingement syndrome to include edema and hemorrhage of the rotator cuff, fibrosis and tendonitis of the rotator cuff, and finally varying degrees of tendon rupture often associated with bone spur formation. Physical findings at each of these stages are similar (12). As such, anterior acromioplasty, regardless of approach has been employed in each of these stages. The diagnosis of impingement syndrome of all patients treated both nonoperatively and operatively in Olmsted County roughly increased sevenfold from 1980 to 2005. This increase is similar to the six-fold increase in anterior acromioplasty in this time period.
The surgical treatment of the distal clavicle has also changed. Although the absolute numbers of resection has increased over time, the frequency has significantly decreased.
The frequency of the surgical procedure anterior acromioplasty remained fairly stable between 1980 and 1991 but thereafter has dramatically increased in frequency (p<0.001). This is not a reflection of the types of rotator cuff lesions treated, patient sex, or patient age. The method of performing this procedure has shifted dramatically to the use of arthroscopy. This is due to multifactorial reasoning. One can speculate this may have contributed to the increase in the number of procedures performed due to the limited postoperative morbidity for arthroscopic acromioplasty, the shortening of the time period for postoperative arm support, the ease of rehabilitation due to maintenance of the deltoid insertion, and a more cosmetic scar (13-15). The number of orthopedic surgeons have additionally increased within the past 20 years, which may potentially increase patient access and availability to a shoulder and elbow specialist. This may indirectly increase the number of patients with a new diagnosis of impingement syndrome. However, at our institution, the number of surgeons participating in shoulder procedures was relatively constant over time with 10 surgeons participating in 1971-1980, 12 in 1981-1990, 12 in 1991-2000, 13 in 2001-2008. Lastly, it is also likely surgeons have come to appreciate that inflammation with fibrosis and tendon fraying or incomplete rotator cuff tearing are important components of the subacromial impingement syndrome, current imaging procedures can better identify these changes preoperatively, and surgical resolution of these aspects of the clinical condition may be more effectively addressed using the arthroscopic method.
Limitations
There are a number of characteristics of the study population in our institutions that may limit our findings. Notably in comparison to the United States population, Olmsted County is disproportionately white with 89% being non-Hispanic white. There are more women than men and the level of education is higher than the U.S. white population in general (12). Residents are primarily of Northern European descent and disease characteristics of other ethnic groups may be underrepresented (16). In addition there is no assurance that our practice patterns are identical to that elsewhere with other regions being more or less conservative in treatment. There are a large number of orthopedic surgeons in our community and a well-developed shoulder and elbow service. At our institution, the number of faculty in the shoulder and elbow service performing shoulder procedures remained stable. The fellowship program was initiated in the early 1980s. So it is unlikely that procedural numbers were at any time limited by the availability of treating surgeons. The majority of acromioplasty procedures were performed at a major tertiary referral center, and it is possible that our approach to this surgical procedure may be different than that found elsewhere. Given the retrospective nature of the study, it is unclear whether arthroscopy was used for the primary intent of performing anterior acromioplasty or as a tool to refine the diagnosis with resultant anterior acromioplasty. An MRI protocol for the diagnosis of rotator cuff tears was not present at our institution until the late 1980s and early 1990s. Prior to this, a shoulder arthrogram protocol existed. Imaging modality of each patient was not reviewed. Correlation between the emergence of MRI and rise of arthroscopy cannot be drawn. Regardless, the result is a dramatic increase in anterior acromioplasty.
Conclusions
The frequency of anterior acromioplasty has dramatically increased over time. Increasing knowledge about this syndrome, including better imaging, has facilitated patient treatment for a stable spectrum of rotator cuff pathology (inflammatory or fibrosis, partial thickness tearing, full thickness tearing undergoing debridement), as has the application of endoscopic surgery.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Neer CS., II Anterior acromioplasty for the chronic impingement syndrome in the shoulder. A preliminary report. J Bone Joint Surg. 1972;54A:41–50. [PubMed] [Google Scholar]
- 2.Isi Web of Science. Philadelphia, PA: Institute for Scientific Information; c1998. [January 15, 2008]. electronic resource. www.isiknowledge.com. [Google Scholar]
- 3.Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: Is it time for a new method of assessment? Br Journal of Sports Medicine. 2009;43(4):259–264. doi: 10.1136/bjsm.2008.052183. [DOI] [PubMed] [Google Scholar]
- 4.Fletcher DD, Andrews KL, Hallett JW, Butters MA, Rowland CM, Jacobsen SJ. Trends in rehabilitation after amputation for geriatric patient's with vascular disease: implications for future health resource allocation. Arch Phys Med Rehabil. 2002;83:1389–93. doi: 10.1053/apmr.2002.34605. [DOI] [PubMed] [Google Scholar]
- 5.Madhok R, Lewallen DG, Wallrichs SL, Ilstrup DM, Kurland RL, Melton LJ., III Trends in the utilization of primary total hip arthroplasty, 1969 to 1990: a population-based study in Olmsted County, Minnesota. Mayo Clin Proc. 1993;68:11–8. doi: 10.1016/s0025-6196(12)60013-5. [DOI] [PubMed] [Google Scholar]
- 6.Madhok R, Lewallen DG, Wallrichs SL, Ilstrup DM, Melton LJ., III Utilization of upper limb joint replacements during 1972-1990: the Mayo Clinic experience. Proc Inst Mech Eng H. 1993;207(4):239–44. doi: 10.1243/PIME_PROC_1993_207_302_02. [DOI] [PubMed] [Google Scholar]
- 7.Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–74. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 8.Melton LJ, III, Stauffer RN, Chao EY, Ilstrup DM. Rates of total hip arthroplasty: a population-based study. N Engl J Med. 1982;307:1242–5. doi: 10.1056/NEJM198211113072004. [DOI] [PubMed] [Google Scholar]
- 9.Quam JP, Michet CJ, Jr, Wilson MG, et al. Total knee arthroplasty: a population-based study. Mayo Clin Proc. 1991;66(6):589–95. doi: 10.1016/s0025-6196(12)60517-5. [DOI] [PubMed] [Google Scholar]
- 10.Bergstralh EJ, Offord KP, Chu CP, Beard CM, O'Fallon WM, Melton LJ., III . Section of Biostatistics, Technical report series No 49. Rochester (MN): Section of Biostatistics, Mayo Clinic; 1992. Calculating incidence, prevalence and mortality rates for Olmsted County, Minnesota: an update. [Google Scholar]
- 11.Ellman H. Arthroscopic subacromial decompression: analysis of one to three year results. Arthroscopy. 1987;3:173–81. doi: 10.1016/s0749-8063(87)80061-0. [DOI] [PubMed] [Google Scholar]
- 12.Neer CS., II Impingement lesions. Clin Orthop. 1983;173:70–7. [PubMed] [Google Scholar]
- 13.Altchek DW, Carson EW. Arthroscopic acromioplasty Current Status. Orthop Clinics NA. 1997;28:2. doi: 10.1016/s0030-5898(05)70276-5. [DOI] [PubMed] [Google Scholar]
- 14.Hawkins RJ, Plancher KD, Saddemi SR, Brezenoff LS, Moor JT. Arthroscopic subacromial decompression. J Shoulder Elbow Surg. 2001;10(3):225–30. doi: 10.1067/mse.2001.114679. [DOI] [PubMed] [Google Scholar]
- 15.Lindh M, Norlin R. Arthroscopic subacromial decompression versus open acromioplasty: A two-year follow-up study. Clin Orthop. 1993;290:174–6. [PubMed] [Google Scholar]
- 16.US National Census Data. Edited 2000. Available at: www.census.gov.


