Abstract
Oral health is essential to overall health in the prenatal period. Pregnancy is not a time to delay dental care. Several studies have shown an association between periodontal disease and poor pregnancy outcomes including preterm birth. Interventions to provide periodontal treatment to pregnant women yield inconsistent results regarding preterm birth but have established the safety of periodontal therapy during pregnancy. Postpartum, women in poor dental health readily transmit the tooth decay pathogen Streptococcus mutans from their saliva to their infants resulting in increased risk of early childhood caries. Preventive services and treatment for acute problems should be recommended, fears allayed, and women referred. Dental x-rays may be performed safely with the use of appropriate shielding. Non-emergent interventions are best provided between 14 and 20 weeks of gestation for comfort and optimal fetal safety. Most gravid women do not seek dental care. Increased interprofessional communication to encourage dentists to treat pregnant women will reduce the number of women without care. In states where it is available, Medicaid coverage of dental services for pregnant women is typically allowed during pregnancy and for two months postpartum. Women’s health providers should understand the importance of protecting oral health during pregnancy and educate their patients accordingly.
INTRODUCTION
Midwives and other women’s health care providers increasingly recognize dental care as an essential component of health and health care for pregnant women. The American Congress of Obstetricians and Gynecologists and the American Academy of Pediatrics advise pregnant women to continue “usual dental care in pregnancy” including continued brushing and flossing, scheduled prophylactic cleanings, and any necessary dental work.1 The American Academy of Periodontology recommends women receive preventive services and any indicated therapeutic intervention during pregnancy.2 Nevertheless, screening and referral for dental care during pregnancy is often overlooked.3,4
Anecdotally, health care providers report a common reason they do not refer women for dental care during pregnancy is the lack of dentists willing to provide this care, particularly for low-income pregnant women. The situation may be changing. A recent survey of general dentists in Oregon found 91.7% agreed that dental care should be part of prenatal care.5 However, until recently, there were no detailed practice guidelines regarding the safety and appropriateness of dental services for pregnant women. In 2006, the New York State Department of Health developed the first comprehensive, evidenced-based guidelines covering several aspects of dental care during pregnancy. These guidelines were compiled by a multidisciplinary panel of experts with sections specifically written for oral health professionals and prenatal care providers.6 In February 2010, the California Dental Association Foundation, in collaboration with District IX of the American Congress of Obstetricians and Gynecologists, released an updated set of guidelines expanding on the original publication from New York State.7
The purpose of this article is to review why dental care during pregnancy is advisable, describe the most common dental procedures and treatments provided to pregnant women, and provide resources women’s health care providers can share with their patients to help them understand the importance of protecting their oral health during pregnancy and ways to do so.
WHY IS DENTAL CARE ADVISABLE?
Preventive services and therapeutic interventions to arrest tooth decay and alleviate periodontal disease improve the oral health and the overall health of the pregnant woman. Oral problems specific to pregnancy can also be addressed during dental care. In addition, improved maternal oral health decreases the risk of early childhood caries in offspring.
Tooth Decay
Preventing and arresting tooth decay (cavities), a product of acid demineralization of the teeth in the bacterial disease dental caries, is an important goal of dental care. Dental caries remains a prevalent disease in the United States, particularly among vulnerable populations such as racial and ethnic minorities.8 Among pregnant women, changes in eating habits, specifically in the frequency and types of food consumed, and in oral hygiene can exacerbate dental caries and increase the risk of new tooth decay. The organisms that cause tooth decay are acidogenic, and increases in carbohydrates select for such organisms in the biofilm on the teeth. Women who crave carbohydrate-rich food during pregnancy are particularly at risk.9 Frequent vomiting, which is common in pregnancy, can contribute to an acidic environment leading to growth of dental caries pathogens as well as acid demineralization of the tooth enamel. Pregnant women should be encouraged to rinse their mouths with water and use over–the-counter fluoride mouthrinses after vomiting to remove and counteract the effects of stomach acids in the mouth. Tooth decay is not self-limiting. Left untreated, cavities can result in dentoalveolar and head and neck abscesses and cellulitis which can be life threatening. Women with substance abuse, such as those who use methamphetamine, often have serious decay,10 and methamphetamine is a frequently abused substance for which women are treated during pregnancy.11 Therapeutic intervention to arrest tooth decay-including the use of fillings, crowns, and root canal treatments-and repair damaged teeth is safe and appropriate during pregnancy.6,7
Periodontal Diseases
Periodontal diseases are bacterial infections of the gums and bone surrounding the teeth characterized by acute and chronic inflammatory changes and loss of bone support for the teeth. Periodontal infections can be suppurative and painful, or more often, are relatively silent. Changes may occur rapidly over months or progress more slowly. Periodontal diseases of a serious nature are rare among young adults affecting approximately 1% of people 18 to 34 years old, and it is unlikely that pregnancy per se exacerbates pre-existing disease.12 Primary risk factors for serious periodontal infection are smoking and diabetes. Additionally, individuals with untreated HIV infection and other immunocompromising conditions are at high risk for periodontal infections. Poor oral hygiene is often present. Bone loss from periodontal infections is not reversible so early identification and referral is critical to prevent tooth loss. Treatment of periodontal diseases in pregnancy is considered safe13–16 and generally improves maternal oral health.15,16 The most common procedures are scaling and root planing (also known as “deep cleaning”). Scaling and root planing remove calculus (tartar) that is laden with pathogenic bacteria and their toxic metabolic byproducts; curettage of infected gum tissue promotes healing of inflamed gums.
Several studies have suggested an association between periodontal disease and adverse pregnancy outcomes including preterm birth or low birth weight,17–21 gestational diabetes,22 preeclampsia,23 small for gestational age infants,24 and stillbirth.25 Biologic plausibility for triggering preterm labor is thought to be through systemic increases in inflammatory mediators such as prostaglandins (specifically PGE2) and cytokines as a result of endotoxin and lipopolysaccharide release by pathogenic Gram-negative anaerobes.
Nevertheless, large-scale studies to reduce the risk of preterm birth by providing periodontal therapy to pregnant women with preexisting disease have not demonstrated improved pregnancy outcomes.13–16 For example, a blinded, randomized, controlled trial screened 823 pregnant women for periodontal disease.13 Women with disease were randomly assigned to one of two groups. One group received scaling and root planing before 21 weeks of pregnancy and monthly tooth polishing and oral hygiene instruction (n = 413). Women assigned to the second (control) group received brief monthly oral examinations during pregnancy then scaling and root planning after birth (n = 410). Results showed that periodontal treatment during pregnancy significantly improved the periodontal status of study participants. Differences between the two groups in preterm births were not statistically significant (hazard ratio for treatment vs. controls 0.93, 95% confidence interval [CI] 0.63–1.37). Also, there were no significant differences between the treatment and control groups in infant birth weights (3239g vs. 3258g), small for gestational age infants (12.7% vs. 12.3%), or the number of spontaneous abortions or stillbirths (5 vs. 14).
Michalowicz and colleagues reported a study in which 823 women with periodontal disease were randomly assigned to receive scaling and root planing between 13–21 weeks’ gestation (n = 413) or after giving birth until 3 months postpartum (n = 410).14 All study participants were also assessed for moderate to severe caries and fractured or abscessed teeth, and essential dental treatment was provided as needed. There were no statistically significant differences between the study groups in rates of preterm births, fetal anomalies, spontaneous abortions, or stillbirths according to receipt of scaling and root planing and/or essential dental treatment.
In a single-center, randomized, controlled trial conducted in Australia,16 women were assigned to receive periodontal treatment and education beginning at 20 weeks of gestation (n = 542) or 6 weeks after birth (n = 540). Periodontal treatment during pregnancy was associated with improved periodontal health, but there were no significant differences between the treatment and control groups in preterm births (9.3% vs. 9.7%, OR 1.05, 95% CI 0.70–1.58), infant birth weights (3450g vs. 3410g), or preeclampsia (4.1% vs. 3.4%). There were also no differences found between groups with regard to other outcomes including incidence of nonreassuring fetal heart rate tracings, delivery for nonreassuring fetal heart rate patterns, meconium-containing amniotic fluid, cesarean delivery for fetal distress, or Apgar scores less than 7 at 1 minute or 5 minutes.
In a treatment-masked, controlled clinical trial, 1806 women were randomized to receive scaling and root planing before 23weeks and 6 days’ gestation (n = 903) or after birth (n = 903).15 Compared to those who received treatment during pregnancy, those assigned to delay periodontal treatment until after birth showed a worsening of their periodontal status over the course of pregnancy. No significant group differences were found in terms of preterm births (13.1% vs. 11.5%, OR 1.22, 95% CI 0.089–1.66) or other outcomes including preeclampsia (7.6% vs. 8.4%), birth weights (3227g vs. 3241g), small for gestational age infants (11.2% vs. 13.7%), and neonatal intensive care unit admissions (9.6% vs. 9.7%). Additionally, the authors reported no difference between groups in a composite score reflecting neonatal morbidity and mortality that included fetal demise after randomization, neonatal death before hospital discharge, respiratory distress syndrome, sepsis, higher grade intraventricular hemorrhage, necrotizing enterocolitis requiring treatment, and congenital abnormalities.
Dental Conditions Common During Pregnancy
Bleeding and tender gums, including gingivitis, are common dental problems reported by pregnant women. These conditions usually reflect tissue responses to increased levels of progesterone and estrogen and are largely preventable if good oral hygiene is maintained throughout pregnancy. Recommendations include daily brushing and flossing and scheduled prophylactic cleanings performed by a dental professional. Periodic warm saltwater rinses can help ease irritation (1 teaspoon salt to 1 cup of water). Adjunctive therapy with a 0.12% oral chlorhexidine mouthrinse twice daily can provide added benefit. Chlorhexidine is a U. S. Food and Drug Administration (FDA) Pregnancy Class B drug and is safe for use during pregnancy. Gingivitis that arises primarily during pregnancy is self-limiting; however, at the extreme, failure to treat it can result in disfiguring changes to the gums.
Pyogenic granulomas (also known as pregnancy tumors) occur in up to 10% of pregnant women. They may be flat or pedunculated and range from a deep purplish-red to pink in color. They typically occur in the maxillary (upper) gum tissue in inflamed, plaque-laden areas and appear during the second trimester. They tend to grow rapidly during pregnancy and regress postpartum; however, postpartum surgical excision may be necessary for complete resolution. Pyogenic granulomas do not pose a danger during pregnancy, and reassurance should be provided to affected women. If they bleed frequently with chewing or talking, cause discomfort, or affect teeth alignment, excision during pregnancy should be considered. Pregnant women should be advised that lesions removed during gestation can recur, and repeat excision may be required postpartum.9
Oral Health of Infants and Young Children
Poor oral health of mothers leads to poor oral health of children.26 Women in poor dental health have high amounts of Streptococcus mutans in their saliva that can be transmitted readily to their infants through common parenting behaviors such as sharing a spoon or bites of food, or licking a pacifier. Bacteria present in the mother increase the chance of colonization of the infant and consequently the caries (tooth decay) process.26 Infection occurs soon after birth, and the infant’s teeth are colonized as they erupt during the first and second years of life.27 Dental care during pregnancy can benefit both mother and child by eliminating this source of S. mutans transmission and providing anticipatory guidance about infant oral health and how to prevent early childhood caries. Special consideration should be given to pregnant adolescents as a combination of strategies to provide guidance and promote oral health change may be necessary.28
Adjunctive therapy with xylitol chewing gum used three to four times daily is effective in reducing maternal transmission of S. mutans.29 Xylitol is a “generally regarded as safe” (GRAS) sweetener approved and available in the United States.30 Xylitol inhibits bacterial growth and results in decreased acid production and cavity formation. Decreased bacterial load also limits the potential passage of S. mutans from mother to infant after birth. Each piece of chewing gum should be chewed for 5 minutes to have a therapeutic effect. Xylitol-containing mints are also available and may be consumed in lieu of gum. Mints should be allowed to dissolve completely in the mouth. Women may have concerns that xylitol will exert a laxative effect; however, the low dose received with this regimen is highly unlikely to cause any discomfort.31 Starting at a subtherapeutic dose for a week and then increasing the dose allows adaptation and mitigates gas, cramps, and bloating.
DENTAL SERVICES PROVIDED TO PREGNANT WOMEN
Preventive services and treatment for acute dental infections should be provided as early in pregnancy as possible. Diagnosis, including x-rays, and needed dental treatment can be provided safely at any gestational age.2,9,32,33 However, many health care professionals regard the period from 14 to 20 weeks of gestation as the optimal time to perform non-emergent procedures.6 Fetal organogenesis has been completed by this time, and the chance for spontaneous abortion is lower than in the first trimester. This is also the most comfortable time for many women, once nausea and vomiting have subsided and women’s energy has returned. The uterus is below the umbilicus until 20 weeks’ gestation allowing for comfortable and easy positioning in a dental treatment chair. During the third trimester, modifications in positioning are particularly important to avoid the supine position in which uterine compression of the inferior vena cava causes decreased venous return and hypotension, nausea, and vomiting. Emergency services can and should be provided at any time.1,6,7
The American Dental Association (ADA) states that routine or “administrative” x-rays should be avoided during pregnancy, but pregnancy is not a reason to delay clinically indicated dental radiographs.9 According to the ADA and FDA, radiographic examinations should be individualized based on clinical evidence of dental disease or a disease history. New patients should have a panoramic radiograph and posterior bitewing radiographs or a full mouth intraoral radiographic examination. Patients with a clinical evidence of tooth decay or who are at high risk should have posterior bitewing radiographs at 6 to 12 month intervals. Patients at lower risk should have such examinations at 12 to 24 month intervals. Appropriate shielding, consisting of a leaded abdominal apron and thyroid collar, should always be used.9,32 The American Congress of Obstetricians and Gynecologists also recognizes that limited medical x-ray exposure for diagnostic purposes poses no risk to the fetus: “Exposure to less than 5 rad has not been associated with an increase in fetal anomalies or pregnancy loss,” and a single-diagnostic x-ray procedure very early in pregnancy does not harm a developing preembryo or embryo.33 Estimated fetal exposure from a single dental radiograph is 0.0001 rad. Therefore, it would take 50,000 examinations to reach the cumulative 5-rad dose limit.34
Dental care during pregnancy is not very different from care provided for women who are not pregnant. The majority of what occurs consists of visual and indicated radiographic examinations of the teeth; tooth cleaning; repair of decayed teeth using fillings or crowns as required by the amount of tooth damage; and extraction of teeth decayed beyond repair, such as those broken off at the gumline, where there is cellulitis, or where boney support is badly compromised by infection. Root canal treatment (endodontics) is safe and appropriate for teeth with irreversible pulpitis (inflammation of the soft pulp in the center of the tooth containing blood vessels and nerves) if the tooth crown is repairable. More frequent and extensive mechanical tooth cleaning (also called scaling and root planing or non-surgical periodontal treatment) is provided for women with periodontal diseases. Dentists routinely prescribe antibiotics and analgesics and use topical and intraoral local anesthetics with vasoconstrictors, all of which are safe during pregnancy.
FEW WOMEN RECEIVE DENTAL CARE DURING PREGNANCY
Despite the potential benefits of dental care, relatively few women receive dental services during pregnancy. An analysis of four states’ data from the Centers for Disease Control and Prevention (CDC) Pregnancy Risk Assessment Monitoring System (PRAMS) found 23% to 35% of pregnant women received dental care during pregnancy.3 Among women who reported having a dental problem, approximately one-half received professional care. Women with education levels beyond high school and women of higher socioeconomic status were more likely to have seen a dental provider. Likewise, women who began prenatal medical care in the first trimester of pregnancy were more likely to have received dental services during pregnancy. Public insurance was inversely related to receipt of dental care. Pregnant women covered by Medicaid insurance were 24% to 53% less likely to receive dental care than pregnant women covered by private insurance.3
There are a number of reasons why women may not receive dental care during pregnancy. A study conducted in 2004 – 2005 in Ohio surveyed women regarding their perceptions of dental care and dental care practices. Fifty-four percent of women reported dental care was important during pregnancy, yet only 44 percent actually received care during pregnancy. Fewer than half (40%) stated they were advised by their obstetric provider to seek dental care during pregnancy, and 10% reported a dentist refused to provide them care because they were pregnant.4
It is not uncommon for dental and medical professionals to suggest a pregnant woman delay dental treatment until after she gives birth. This is shortsighted. Women served by Medicaid may have dental insurance benefits only during pregnancy and for 2 months post-partum. States that extend Medicaid dental coverage to pregnant women typically provide this benefit for what is, in reality, a very a short period of time. By the time a woman establishes prenatal care and obtains an appointment with an available dentist, she may be near or in her second trimester already, further reducing the optimum period for preventive care and treatment if a series of visits is required. In the first 2 months after birth, a new mother may be less motivated and less able to seek dental care because of the demands of caring for a newborn.
Creative, community-based partnerships can improve access to and receipt of dental care by pregnant women. One intervention in a single county in Oregon was successful in increasing the number of women enrolled in Medicaid who received dental care during pregnancy from 8.8% to 55.8%.35 This dramatic increase was the result of a coordinated interdisciplinary approach designed to educate women and providers about oral health and pregnancy and to increase referral of women for dental care. Eligible pregnant women were identified and referred by the state health program office; prenatal care providers; or Women, Infant, and Children (WIC) program employees working in the county. All women were assigned a dental home under a dental managed care program (DCO). Outreach and education regarding oral health in pregnancy and its connection to infant oral health was first provided to the women by WIC employees. All initial screening dental exams and preventive services were provided by a dental hygiene clinic affiliated with a teaching institution that was under contract with the DCO. Hygienists communicated results of initial screening exams and subsequent oral care plans to women’s prenatal care providers. Dentists then provided indicated restorative, periodontal, and oral surgical services. Continuing education programs were provided to involved dental hygienists, dentists, and prenatal care providers to promote current evidence-based practices regarding dental care in pregnancy and improve interprofessional communication.
INTERPROFESSIONAL COMMUNICATION
Attitudes among dentists regarding the appropriateness of dental care during pregnancy are changing.5 Nevertheless, there is often inadequate interprofessional communication. Formal referral processes from the prenatal care provider to the dentist can increase appropriate care. Referral, in writing, for women with uncomplicated pregnancies should state that all necessary care is indicated. This informs the dentist that a woman is receiving prenatal care and her provider is supportive of indicated dental care during pregnancy. Referral for the woman with pregnancy complications should list her condition(s), specify limitations on the period when care can be given, and note any need to avoid particular medications.
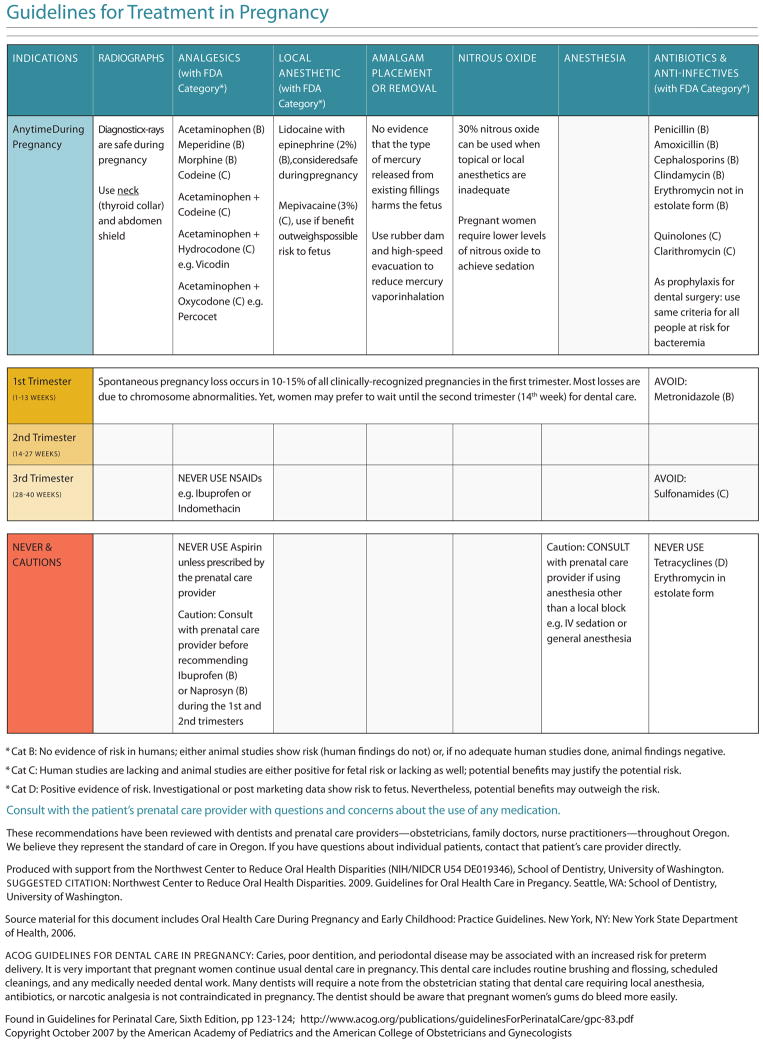
In order to improve communication and increase safety, the authors have developed a reference card regarding dental care during pregnancy (Figure 1). The card was developed primarily for oral health providers; however, the information contained can benefit prenatal care providers by familiarizing them with common dental procedures, medications, and precautions applicable to pregnant women. The card provides guidelines for both routine and emergency oral health care in pregnancy and addresses the provision of dental care to women with hypertensive disorders, gestational diabetes, and thrombophilias. Indications and precautions regarding the use of radiographs, analgesics, nitrous oxide, and select antibiotics during pregnancy are also delineated.
Figure 1. Guidelines for Oral Health Care in Pregnancy.
PATIENT EDUCATION
Online resources regarding dental care during pregnancy are available from several organizations and can help pregnant women learn more about protecting their oral health. A sample of these organizations and links to their Web sites are included in Appendix 1. Women should be encouraged to consult with a dentist before and during pregnancy. It is important to note that routine professional dental care will have a limited effect unless it is accompanied by changes in personal oral hygiene (Box 1).
Box 1. Hygiene Practices to Improve Oral Health in Pregnancy.
Brush at least twice daily.
Brush with a soft toothbrush to lessen gum irritation.
Floss at least once daily.
Use periodic warm salt-water rinses to sooth tender gums.
Swish with an over-the-counter fluoride mouthrinse after vomiting to protect teeth.
Consider chewing xylitol-containing gum three to four times daily.
CONCLUSION
The childbearing year, including the preconception period, provides an opportunity for preventive dental health care to improve the health of a mother and subsequently her infant. Midwives and other women’s health clinicians play an important role in recommending pregnant women receive dental care and making referrals. Greater awareness of the importance of oral health in pregnancy among clinicians, women, and dental care specialists, can have a significant impact on improving overall health of women and their families.
Acknowledgments
Supported by grant no. R40MC03622 from the Maternal and Child Health Bureau, HRSA and grant no. 1U54DE019346 from the National Institute of Dental and Craniofacial Research, NIH.
Appendix 1: Online Patient Resources Regarding Dental Care in Pregnancy
-
The American Dental Association
-
The American Academy of Periodontology
-
The American Pregnancy Association
http://www.americanpregnancy.org/pregnancyhealth/dentalwork.html
-
The New York State Department of Health
http://www.health.state.ny.us/prevention/dental/prenatal_oral_health.htm
-
The California Dental Association
-
The American Congress of Obstetricians and Gynecologistsa
http://www.acog.org/publications/patient_education/ab012.cfm
Footnotes
The views expressed in this manuscript are those of the authors and do not reflect the official policy or position of Madigan Army Medical Center, the Department of the Army, the Department of Defense, or the U.S. Government.
This is a pregnancy planning pamphlet for women that notes dental x-rays are safe and specifically reinforces that a limited number of x-rays will not harm a fetus during pregnancy.
Contributor Information
Megan K. Kloetzel, Physician, Department of Preventive Medicine at Madigan Army Medical Center, Joint Base Lewis-McChord, Washington.
Colleen E. Huebner, Associate professor, Department of Health Services, and director, Maternal and Child Health Program, University of Washington School of Public Health, Seattle, Washington.
Peter Milgrom, Professor, Dental Public Health Sciences, and director, Northwest Center to Reduce Oral Health Disparities, University of Washington School of Dentistry, Seattle, Washington.
References
- 1.The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care. 6. 2007. pp. 123–4. [Google Scholar]
- 2.Task Force on Periodontal Treatment of Pregnant Women, American Academy of Periodontology. American Academy of Periodontology statement regarding periodontal management of the pregnant patient. J Periodontol. 2004;75(3):495. doi: 10.1902/jop.2004.75.3.495. [DOI] [PubMed] [Google Scholar]
- 3.Gaffield ML, Gilbert BJ, Malvitz DM, Romaguera R. Oral health during pregnancy: an analysis of information collected by the pregnancy risk assessment monitoring system. J Am Dent Assoc. 2001;132:1009–16. doi: 10.14219/jada.archive.2001.0306. [DOI] [PubMed] [Google Scholar]
- 4.Strafford KE, Shellhaas C, Hade EM. Provider and patient perceptions about dental care during pregnancy. J Matern Fetal Neonatal Med. 2008;21(1):63–71. doi: 10.1080/14767050701796681. [DOI] [PubMed] [Google Scholar]
- 5.Huebner C, Milgrom P, Conrad D, Lee R. Providing dental care to pregnant women: a survey of Oregon general dentists. J Am Dent Assoc. 2009;140:211–22. doi: 10.14219/jada.archive.2009.0135. [DOI] [PubMed] [Google Scholar]
- 6.New York State Department of Health. Oral health care during pregnancy and early childhood: Practice Guidelines. New York State Department of Health; 2006. [Google Scholar]
- 7.The California Dental Association Foundation. Oral Health During Pregnancy and Early Childhood: Evidenced-based Guide for Health Professionals. California Dental Association; 2010. [March 10, 2010]. Accessed at http://www.cdafoundation.org/learn/perinatal_oral_health. [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services. Oral health in America: a report of the surgeon general. Rockville, (MD): U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [Google Scholar]
- 9.American Dental Association Council on Access, Prevention, and Interprofessional Relations. Women’s Oral Health Issues. Chicago: American Dental Association; 2006. [February 27, 2010]. pp. 3–8. Accessed at http://www.ada.org/prof/resources/topics/healthcare_womens.pdf. [Google Scholar]
- 10.Morio KA, Marshall TA, Qian F, Morgan TA. Comparing diet, oral hygiene and caries status of adult methamphetamine users and nonusers: a pilot study. J Am Dent Assoc. 2008 Feb;139(2):171–6. doi: 10.14219/jada.archive.2008.0133. [DOI] [PubMed] [Google Scholar]
- 11.Terplan M, Smith EJ, Kozloski MJ, Pollack HA. Methamphetamine use among pregnant women. Obstet Gynecol. 2009;113(6):1285–91. doi: 10.1097/AOG.0b013e3181a5ec6f. [DOI] [PubMed] [Google Scholar]
- 12.Borrell LN, Crawford ND. Social disparities in periodontitis among United States adults 1999–2004. Community Dent Oral Epidemiol. 2007;36(5):383–91. doi: 10.1111/j.1600-0528.2007.00406.x. [DOI] [PubMed] [Google Scholar]
- 13.Michalowicz BS, Hodges JS, Diangelis AJ, et al. Treatment of Periodontal disease and the risk of preterm birth. N Engl J Med. 2006;355:1885–94. doi: 10.1056/NEJMoa062249. [DOI] [PubMed] [Google Scholar]
- 14.Michalowicz BS, DiAngelis AJ, Novak MJ, et al. Examining the safety of dental treatment in pregnant women. J Am Dent Assoc. 2008;139:685–95. doi: 10.14219/jada.archive.2008.0250. [DOI] [PubMed] [Google Scholar]
- 15.Offenbacher S, Beck JD, Jared HL, et al. Effects of periodontal therapy on rate of preterm delivery. A randomized controlled trial. Obstet Gynecol. 2009;114:551–9. doi: 10.1097/AOG.0b013e3181b1341f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Newnham JP, Newnham IA, Ball CM, et al. Treatment of periodontal disease during pregnancy: A randomized controlled trial. Obstet Gynecol. 2009;114(6):1239–48. doi: 10.1097/AOG.0b013e3181c15b40. [DOI] [PubMed] [Google Scholar]
- 17.Offenbacher S, Katz V, Fertik G, et al. Periodontal infection as a possible risk factor for preterm low birth weight. J Periodontol. 1996;67:1103–13. doi: 10.1902/jop.1996.67.10s.1103. [DOI] [PubMed] [Google Scholar]
- 18.Offenbacher S, Lieff S, Boggess KA, et al. Maternal periodontitis and prematurity. Part I: Obstetric outcome of prematurity and growth restriction. Ann Periodontol. 2001;6:164–174. doi: 10.1902/annals.2001.6.1.164. [DOI] [PubMed] [Google Scholar]
- 19.Vergnes JN, Sixou M. Preterm low birth weight and maternal periodontal status: A meta-analysis. Am J Obstet Gynecol. 2007;196:135.e1–7. doi: 10.1016/j.ajog.2006.09.028. [DOI] [PubMed] [Google Scholar]
- 20.Jeffcoat MK, Geurs NC, Reddy MS, Cliver SP, Goldenberg RL, Hauth JC. Periodontal infection and preterm birth: results of a prospective study. J Am Dent Assoc. 2001;132:875–80. doi: 10.14219/jada.archive.2001.0299. [DOI] [PubMed] [Google Scholar]
- 21.Xiong X, Buekens P, Vastardis S, Yu SM. Periodontal disease and pregnancy outcomes: state of the science. Obstet Gynecol Surv. 2007;62(9):605–15. doi: 10.1097/01.ogx.0000279292.63435.40. [DOI] [PubMed] [Google Scholar]
- 22.Xiong X, Buekens P, Vastardis S, Pridjian G. Periodontal disease and gestational diabetes mellitus. Am J Obstet Gynecol. 2006;195:1086–9. doi: 10.1016/j.ajog.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 23.Boggess KA, Lieff S, Murtha AP, Moss K, Beck J, Offenbacher S. Maternal periodontal disease is associated with an increased risk for preeclampsia. Obstet Gynecol. 2003;101:227–231. doi: 10.1016/s0029-7844(02)02314-1. [DOI] [PubMed] [Google Scholar]
- 24.Boggess KA, Beck JD, Murtha AP, Moss K, Offenbacher S. Maternal periodontal disease in early pregnancy and risk for small-for-gestational-age infant. Am J Obstet Gynecol. 2006;194:1316–22. doi: 10.1016/j.ajog.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 25.Mobeen N, Jehan I, Banday N, et al. Periodontal disease and adverse birth outcomes: a study from Pakistan. Am J Obstet Gynecol. 2008;198:514.e1–514.e8. doi: 10.1016/j.ajog.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boggess KA, Edelstein BL. Oral health in women during preconception and pregnancy: implications for birth outcomes and infant oral health. Matern Child Health J. 2006;10:S169–S174. doi: 10.1007/s10995-006-0095-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caufield PW, Cutter GR, Dasanayake AP. Initial acquisition ofmutans streptococci by infants: evidence for a discrete window of infectivity. J Dent Res. 1993;72(1):37–45. doi: 10.1177/00220345930720010501. [DOI] [PubMed] [Google Scholar]
- 28.Murphey C, Rew L. Three intervention models for exploring oral health in pregnant minority adolescents. J Spec Pediatr Nurs. 2009;14(2):132–41. doi: 10.1111/j.1744-6155.2009.00189.x. [DOI] [PubMed] [Google Scholar]
- 29.Nakai Y, Shinga-Ishihara C, Kaji, Moriya K, Murakamai-Yamanaka K, Takimura M. Xylitol gum and maternal transmission of mutans streptococci. J Dent Res. 2010;89(1):56–60. doi: 10.1177/0022034509352958. [DOI] [PubMed] [Google Scholar]
- 30.Milgrom P, Ly KA, Rothen M. Xylitol and its vehicles for public health needs. Adv Dent Res. 2009;21:44–7. doi: 10.1177/0895937409335623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.California Dental Association. Xylitol: The Decay-Preventive Sweetener. California Dental Association; [February 27, 2010]. Accessed at http://www.cda.org/popup/xylitol. [Google Scholar]
- 32.American Dental Association, U.S. Dept of Health and Human Services. [February 27, 2010];The selection of patients for dental radiographic examinations. Revised 2004. Accessed at http://www.ada.org/sections/professionalResources/pdfs/topics_radiography_examinations.pdf.
- 33.ACOG Committee Opinion. Number 299, September 2004. Guidelines for diagnostic imaging during pregnancy. Obstet Gynecol. 2004;104(3):647–651. doi: 10.1097/00006250-200409000-00053. [DOI] [PubMed] [Google Scholar]
- 34.Toppenberg KS, Hill DA, Miller DP. Safety of radiographic imaging during pregnancy. Am Fam Physician. 1999 Apr 1;59(7):1813–8. [PubMed] [Google Scholar]
- 35.Milgrom P, Ludwig S, Shirtcliff M, et al. Providing a dental home for pregnant women: A community program to address dental care access. J Public Health Dent. 2008;68(3):170–173. doi: 10.1111/j.1752-7325.2007.00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]