Abstract
Rett Syndrome (RTT) is an X-linked neurodevelopmental disorder caused by mutations in the MECP2 gene. In 49 female RTT children, ages 1.9–17 years, bone mass was assessed and correlated with clinical parameters and mutations involving the MECP2 gene. We also studied 5 adult females, ages 20–33 years, and one male, age 6 years. Lumbar spine bone mineral content (BMC) and bone mineral density (BMD) were correlated with weight, height, body mass index, clinical severity, degree of scoliosis, use of anticonvulsants and ambulatory status. L1–L4 BMD and BMC showed that 48.9% of them had BMD values greater than 2 SD below age-related norms. BMD values were in the osteoporotic range in the 5 adult females with RTT. Eleven percent of the children and adults with RTT experienced fractures. Low bone mass was correlated with marginal significance to clinical severity and ambulation, but not to scoliosis or anticonvusant use. Lowest bone mass occurred in patients with T158M or R270X mutations but without statistical significance. Studies in a murine model of RTT confirmed low bone mass as an inherent component of this syndrome. MECP2 mutations and clinical parameters impact bone mass in RTT but an association with a specific mutation was not demonstrable.
Introduction
Rett syndrome (RTT) is an X-linked dominant neurodevelopmental disorder associated with mutations in MECP2 encoding methyl-CpG-binding protein 2 (1, 2). The incidence is 1:22,000 live female births (3). The majority of patients are females. Males are more severely affected than females. The relationship of MECP2 mutations to the neurologic disease has been confirmed in humans and in murine models of the disorder (1,4,5).
Clinical features of RTT include early onset of neurologic signs with cognitive defects, deceleration of head growth, and stereotypic movements (6, 7). Seizures are a common feature of the disorder and the use of anticonvulsant drugs is frequent. Although a decrease in bone mass was first reported in RTT patients in 1995, information is limited about the age-dependent pattern of bone loss, the fracture incidence and the relationship of bone mass to associated clinical features. (8). Neurological disability in RTT patients evolves over several years with co-morbidities that together limit the development of normal bone mass. These include limited weight bearing, poor nutrition due to swallowing difficulties and the negative effects of anticonvulsant medications. Availability of the murine RTT model permits an assessment of the effects of the MECP2 mutations on bone mass independent of these associated factors.
Methods
This study was approved by the Institutional Review Board, Johns Hopkins University. This is a cross-sectional observational study of the relation of lumbar spine bone mineral content and bone mineral density (BMC and BMD) and related clinical parameters to X-linked MECP2 mutations in 49 girls with RTT syndrome, ages 1.9 to 17 years, one male, age 6 years, and 5 women, ages 20–33 years. Informed consent was obtained from the parent or guardian of the participants enrolled in the study. The diagnosis of RTT was made on the basis of criteria established by the RTT Diagnostic Criteria Work Group (6) and by MECP2 mutation analysis. Patients were scored for severity based on the Rett Syndrome Severity Scale (RSSS) as described in Hoffbuhr et.al. (9). Z-scores for weight-for-age (kg) and stature for age (cm) were obtained for gender and age using the Centers for Disease Control and Prevention ZWTAGE and ZSTATAGE charts for ages 2 to 20 years (cdcinfo@cdc.gov)
Bone mineral density measurements were performed at the Pediatric Clinical Research Unit of Johns Hopkins Hospital using a Hologic Discovery A Dual Energy Absorptiometer (DXA) equipped with pediatric software. The coefficient of variation (CV) for these DXA measurements was 3 %. Lumbar L1–L4 bone mineral content (BMC, gm) and areal bone mineral density (BMD, gm/cm2 ) and Z-scores were obtained. The Hologic database provides Z-scores for ages 3 years and above. BMD Z-scores < −2.0 were considered significant (10). Z-scores are not currently available for lumbar BMC measurements in this pediatric age group. Data is illustrated on modified Hologic machine printouts for five female adult patients. To compare RTT BMC measurements to normal, we employed reference curves developed by Kalkwarf et al. that report the 10, 50 and 90 percentile values for age, gender and race for BMC in 1554 healthy girls ages 7–17 years (11). However, BMC values for children younger than 7 years are plotted in Figure 1 for reference only. For comparison of BMD to normal, we used the Hologic Discovery A database that starts at 3 years of age (Hologic Inc., Bedford MA.) Patient lymphocytes, lymphoblasts or fibroblast cell lines were utilized for identifying mutations in the MECP2 gene, as described by Hoffbuhr et.al. (9). Serum 25(OH) vitamin D levels that were measured at baseline were performed by liquid chromatography/ mass spectroscopy (Quest Diagnostics Nichols Institute, Chantilly, VA). Normal values are 20–100 ng/mL with CV of 10 % ranging from 4–120 ng/ml. Serum total alkaline phosphatase was performed using the spectroscopic para-nitrophenol method.at the Clinical Pathology Laboratory, Johns Hopkins Hospital. Normal values and CV for children and adolescent females are: 100–320 with a 2.8% CV at a level of approximately 80 U/L and 2.3% CV at a level of 360 U/L.
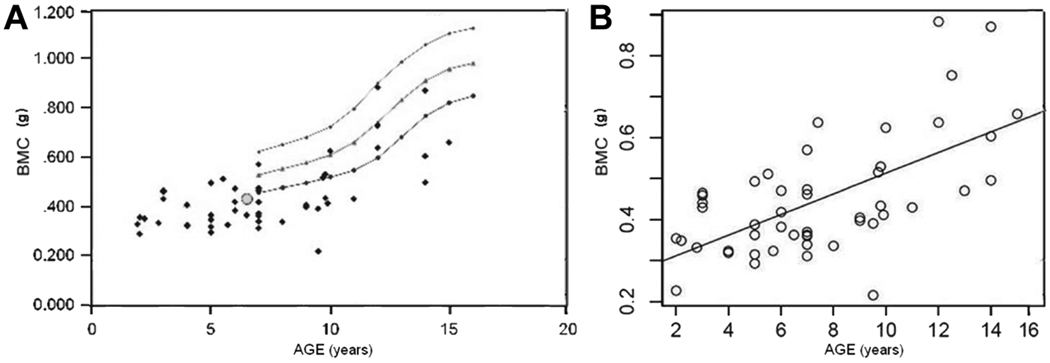
Figure 1.
(A) DXA L1-L4 BMC values compared to age related normal. The 10 th, 50 th and 90 th percentiles for normal females are illustrated. The hollow circle shows BMC for the 6 year old RTT male. (B)Bone mineral content (BMC) is plotted against age, ages 2 to 16 years. There is a linear relationship with a correlation coefficient of r =0.617.
The murine RTT model lacking MECP2 as a result of deletion of exons 3 and 4 of the MECP2 gene was developed by A. Bird in C57BL/6 mice using Cre-loxP technology (4). Heterozygous female MECP2 tm1.1Bird mice (Jackson Laboratory, Bar Harbor, Maine) on a C57BL/6 background were backcrossed with C57BL/6 males for at least 9 generations. Radiographs of the mice were taken using a Faxitron MX20 Specimen Radiography System (Lincolnshire IL).
Statistical analysis
We examined relationships between BMC and BMD and age, and the relationships of age-corrected BMC and BMD to clinical severity, scoliosis, anticonvulsant use and extent of ambulation. These were assessed by general linear model analysis using the R Statistical package (R version 2.10.1, 2009). The relationships of the mean BMC and BMD to various MECP2 mutations were analyzed using Mann-Whitney U tests and chi-square analysis.
Results
Demographics of this RTT Population
This RTT cohort, consisting of 49 girls ages of 1.9 and 17 years (mean age 7.6 ± 3.8 years), included a 6 year old male and 5 females, ages 20 to 33 years.
Bone Mineral Content (BMC) and Bone Mineral Density (BMD) Values for the Lumbar Spine (L1–L4)
We report BMC and BMD L1–L4 values but not total hip or whole body measurements because of the difficulty in positioning these patients who may have continuous upper extremity motion and/or lower extremity contractures. Total hip measurements were available in selected adult patients. Figure 1 shows age vs. L1–L4 BMC for 44 RTT females, and the single RTT male subject, using the 10th, 50th and 90th-percentile normative data for female children. (9). BMC data plotted for children from ages 1.9 to 6 11/12 years is not within the graph line as this data is not currently available for those younger ages. In 15 children aged 7–18 years the BMC scores were < 10 th percentile and in 10 others of the same ages it was above the 10 th percentile. Thus, 66% of the patients with RTT aged 7–18 years had BMC values that were below the 10th percentile for age (Figure 1(a). However, Figure 1(b) shows a linear relationship between BMC and age 2–16 years (r= 0.61).
Figure 2(a) presents BMD measurements plotted against normal female values as provided in the Hologic 4500 database. Although these are cross sectional data, the distribution indicates low bone mass may occur at all ages and continues into adulthood. As with BMC measurements, BMD vs. age shows a linear increase to age 16 years (r= 0.65) [Figure 2(b)]. It is of interest, because of the impact of patient size on DXA measurements, that the correlation coefficient for BMC plotted against BMD in this population was 0. 87 (data not shown).
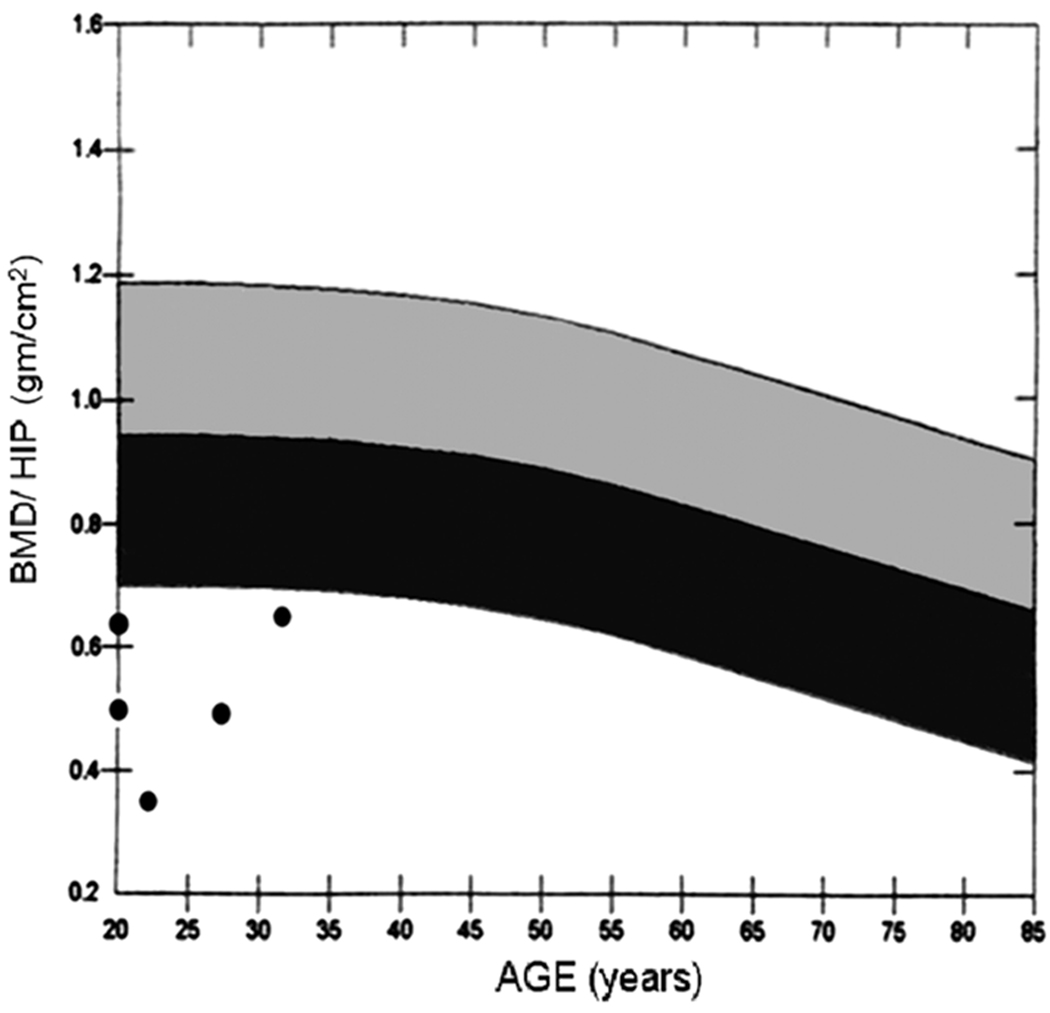
Figure 2.
(A) DXA L1-L4 BMD results plotted on the Hologic 4500 database. The chart shows mean values ± 2 standard deviations.(B) Bone mineral density (BMD) is plotted against age, 2 to 14 years. There is a linear relationship with a correlation coefficient of r= 0.651.
L1–L4 BMD Z-scores were < 2.0 in 24 of 49 children (48.9 %) to age 17 years. However, 11 of 49 children (22%) had Z-scores for the lumbar spine within normal reference range, between 0.0 and −1.5 SD. Partial DXA studies were obtained in 5 adult women because of prior spine fusion or hip surgery. L1–L4 BMD Z-scores for 4 of 5 adult females ages 20 to 33 years, whose BMD is shown in Figure 3, were −3.6, −4.4, and −2.3, but −0.2 in a patient with prior spine surgery. Total hip BMD Z-scores (age) available in 4 of 5 females were: −3.4 (20), −3.0 (27), −1.9 (29) and −2.3 (33).
Figure 3.
DXA values for L1–L4 plotted against the Hologic 4500 data base for 5 females with RTT syndrome. The chart shows mean values + or − 2 standard deviations.
MECP2 Mutations, Bone Mineral Content and Bone Mineral Density
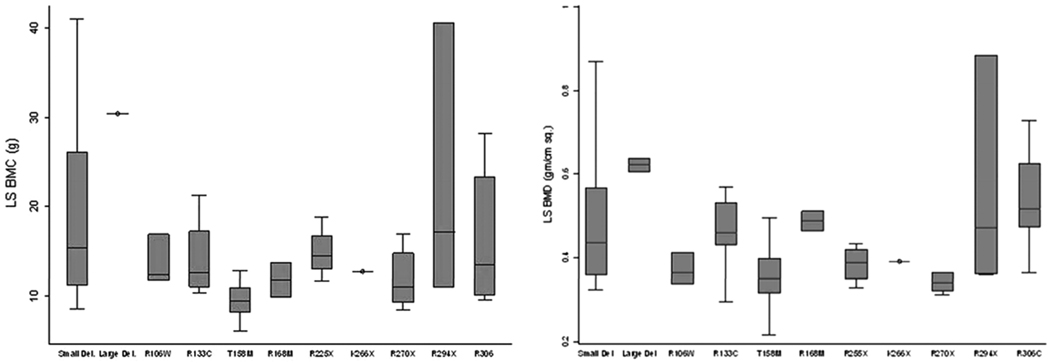
Mutations in MECP2 were confirmed in all patients: 3 cases involved R 106 W, 5 subjects had R133C, 2 had R 168X, 13 had T158M mutations, 4 had R255X, 1 had K266X, 6 had the R270X mutation, 3 had 294X, 3 had R306C, 1 had R306H and 1 had 306P. Seven patients had a small deletion and one had a large deletion. L1–L4 BMD values are plotted for specific mutations (Figure 4). We did not find a statistically significant relationship between specific MECP2 mutations and the median lumbar spine BMC or BMD. However, the lowest BMD values were observed in patients with either the T158M or R270X mutations.
Figure 4.
(A): L1–L4 BMC, and (S): BMD is shown for individual MeCP2 mutations. The bars represent the range ± 2 standard deviations for lumbar spine BMD. The differences in BMC and BMD were not statistically different for any mutation.
Contributory Factors Related to Bone Mass
Poor nutrition and diminished growth are frequent among children with RTT (12). The average body mass index was 16.4 ± 3.6 in children to age 18. Height and weight Z-scores adapted from CDC ZWTAGE and ZSTATAGE_tables were obtained for age groups 1.9–7.0 years, 7.1–11 years, and over 11 years. These CDC tables only provide Z-scores to < 2.0 but they do not provide specific Z-score for values less than − 2.0. For the group with ages 1.9–7 years, 4/22 children had both height and weight Z-scores < 2.0. For girls with RTT ages 7–11 years, 6/20 had height Z scores < 2.0 and 2/20 had weight scores < 2.0. For children ages 11–18, 5/10 had height Z-scores <2.0 as did 5/10 have weight Z-scores more than 2 SD below the mean for age. However, height and weight Z-scores were not statistically related to each other or to BMC or BMD.
Baseline 25(OH) D levels were available in 25 children. The values ranged from <14 to 54ng/ml: mean = 33. 8 ± 9.9 ng/ml. In 13 the serum 25(OH) D levels were within normal range, > 32 ng/ml, 12 were between 20 and 31 ng/ml (D insufficiency) and 1 value was < 14 ng/ml or vitamin D deficient. Serum total alkaline phosphatase values ranged from 29.3 to 117.0 (41–134.6). Neither serum 25(OH) D nor alkaline phosphatase were related to BMD (data not shown).
The mean clinical RSSS score was 7.5 (range 3–15) on a scale of 0–15. Severity scale scores were available for 45 patients less than 18 years of age. Fifteen patients had BMD Z-scores higher, and 20 patients had BMD Z-scores < 2.0. Chi-squared analysis showed a relationship of marginal significance between clinical severity score and BMD (p=0.057)
In estimating the amount of independent ambulation required for the maintenance of lumbar bone mass we defined the ability to walk independently for more than 2 consecutive hours/day, as ambulatory. 34 patients were defined as ambulatory and 15 patients were considered non-ambulatory. Of the non ambulatory patients, 6/15 (40 %) had BMD Z-scores −2.0 SD or below the mean for age, while 21/34 (62%) of the ambulatory patients had BMD Z-scores below 2.0 SD.. Figure 5 illustrates the difference in lumbar spine BMD vs. age for ambulatory and non-ambulatory patients.
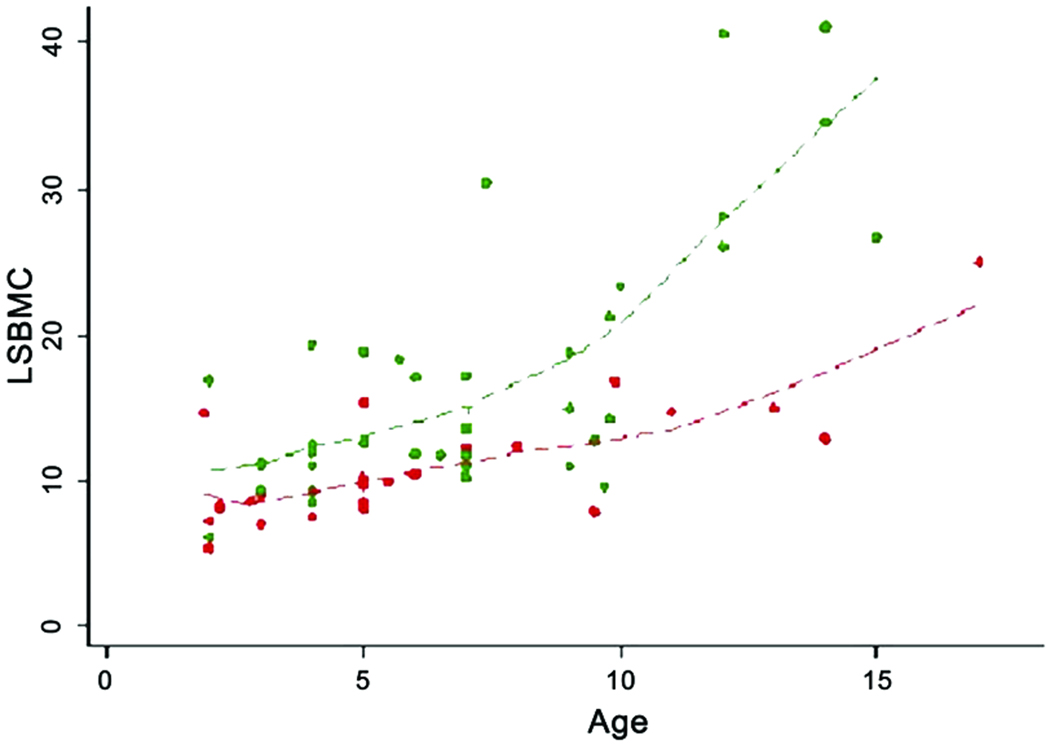
Figure 5.
Trendlines relating age- associated effects of ambulation (green) vs. non ambulation (red) on Lumbar Spine (LS) BMC (g) in RTT. This illustrates the differences between these groups as well as the trend for increasing BMD (g/cm2 ) with age (years).
Of the non-ambulatory patients, 6/14 (43 %) had BMD Z-scores −2.0 SD or below the mean for age, while 62% of ambulatory patients had BMD Z-scores −2.0 SD or below. Absolute BMC values were marginally different in the ambulatory patients 17.02 g/cm2 as compared to the non-ambulatory group 11.51 g/cm2 (p=0.0507). Similarly, absolute BMD values were significantly different in the ambulatory group, (mean BMD= 0.498 ±0.168 gm/cm2 as compared to non-ambulatory patients (mean BMD = 0.425 ±0.104 ). :(p=0.0423)
To evaluate scoliosis, the vertebral Cobb angle was measured in 49 patients. Scoliosis was graded 1–4 based on the following scales: no scoliosis = 0,; 1 < 20°; 2< 30°,;3 < 40° 4 > 40°. Scoliosis in excess of 20 degrees was present in 30 % of patients under 18 years of age (13). No statistical relationship was observed between BMC or BMD and scoliosis severity grades 1 to grade 4. (BMC: p=0.281; BMD: p= 0.133).
Current use of anticonvulsant drugs known to affect mineral metabolism was reported in (31%) of 49 patients. These included phenytoin, carbamazepine, valproic acid and phenobarbital (14). 5/15 patients taking these anticonvulsants had a BMD Z-score < −2.0, while 10/15 had higher BMD values. Mean BMD Z-score for patients taking anticonvulsant drugs, was −2.3± 1.65. Of the 34 patients taking no anticonvulsant medication the mean BMD Z-score was −2.00 ± 2.21. Thus, no significant difference exists between the two groups. ( p= 0.266).
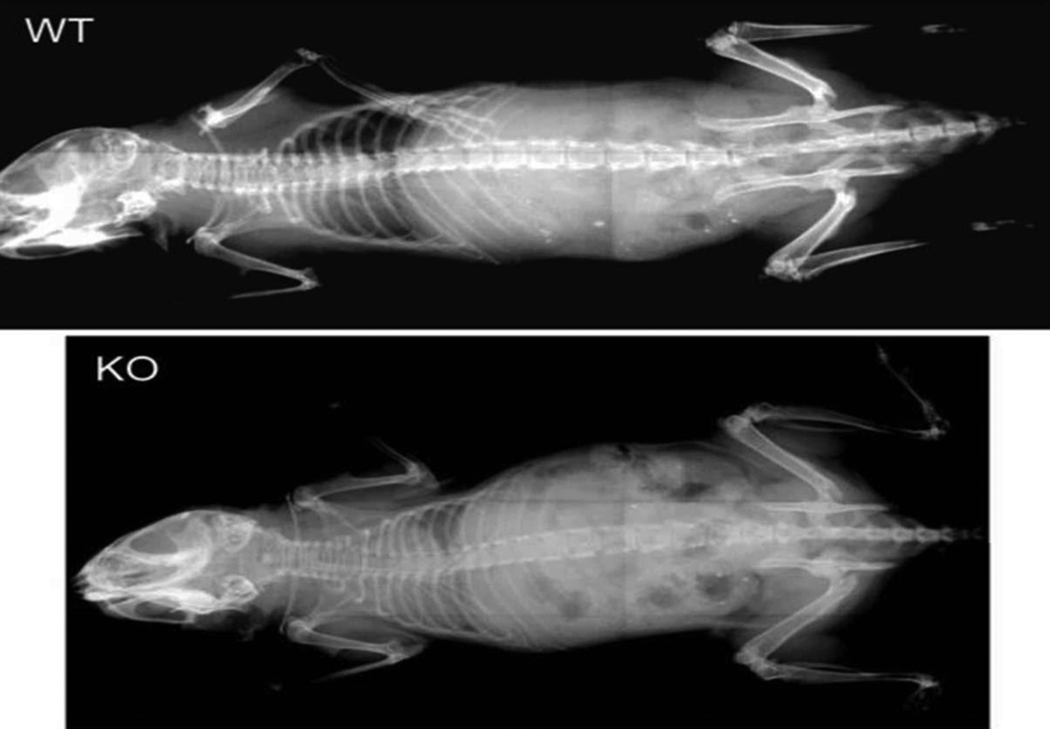
Murine models of RTT permits an initial assessment of the putative contribution of MECP2 mutations independent of confounding factors such as the amount of ambulation and anticonvulsant use. Fig 6 illustrates the difference in bone mass between wild type mice and the male null animal in which exons 3–4 of the MECP2 gene have been deleted (4). Both cortical thickness and medullary mineralization appear decreased in these animals.
Figure 6.
Radiographs of 7 week old mice. Wild type and male null (knock-out mouse) illustrating differences in cortical thickness, mineralization of the medullary cavity in long bones and spine bone density.
Discussion
This study used DXA scans to assess bone mass in children and young adults with mutation-confirmed RTT and to examine the relationships of BMC and BMD to MECP2 mutations. In addition, we examined the relationship of bone mass to associated clinical factors such as anticonvulsant use, scoliosis, ambulation and RSSS.
Obtaining an accurate DXA measurement in RTT patients is difficult because of movement disorders, joint contractures and scoliosis that limit proper positioning and the presence of surgical hardware in the spine or hip. Despite these impediments L1–L4 DXA measurements confirm the presence of decreased BMC and BMD in approximately one-half of the RTT females as early as 3 years of age. The 6 year old non-ambulatory male also had significantly lower BMC and BMD. Each of the 5 adults also had lumbar spine or total hip Z-scores that were in the osteopenic/osteoporotic range.
An age-related decrease in bone mass has been previously reported in RTT. Leonard et al. reported that in their survey of 17 RTT cases 86% showed reduced hand bone density (8). Subsequent studies in 137 Australian RTT girls demonstrated mean metacarpal cortical thickness Z- scores of −1.94 compared with −0.38 for healthy children (P<0.001) (15). Haas observed that spine BMC and BMD were significantly reduced in 20 subjects with RTT syndrome (16). Haas did not find an association between BMC and ambulatory status when in a small cohort of RTT subjects compared to those with cerebral palsy and normal controls (16). In this cohort, 34 % had impaired ambulation, walking less than 2 hours each day. Impaired ambulation was marginally associated with a decreased lumbar spine BMC or BMD in this cohort. Decreased bone mass is frequently observed at the hip and distal femur sites when normal weight bearing is impaired but lumbar spine BMD is usually preserved in non-ambulatory children who spend hours daily in wheelchairs. Here diminished lumbar BMC and BMD, suggests that factors other than impaired mobility were contributing to the low bone mass.
RTT patients in our cohort had markedly decreased height and weight Z-scores. Similarly, Schwartzman reported a height-to-age deficit in 48.1% of RTT girls which was greater in those more severely affected (stage IV) (12). Although, the availability of BMC standards for young girls is limited to over 7 years, BMC was measured because girls with RTT are small for age. Smaller L1–L4 vertebral bone size induces an artifact that may cause areal BMD (gm/cm2) values to appear lower than they actually are when measured as BMC (gm). However, both BMC and BMD confirm the significant association of low bone mass.
Motil et al. indicate that although BMD and BMC increased with age, Z-scores were significantly lower in older compared to younger females with RTT (17). We did not observe this relationship as BMC and BMD values in this cross-sectional study were low in children, tended to increase with age in a linear manner but remained in the osteoporotic range in the 5 older patients. Figure 5, where BMD vs. age is compared for ambulatory vs. non-ambulatory children, illustrates this age- related trend to increased BMD in ambulatory individuals. Larger numbers of patients may be required to define changes in BMD with increasing age.
Low bone mass is associated with increased risk of fracture. Here, 11% of the patients had a history of fracture, all of which occurred before 12 years of age, which is similar to the 14 % incidence, reported by Loder et al. (18). Leonard reported fractures in one-third of 137 Australian cases and estimated that over 40% of girls would sustain a fracture by the age of 15 years (15). A more recent questionnaire survey of 234 girls in the Australian RTT syndrome database revealed a fracture incidence of 43.3 episodes per 1000 person-years, nearly 4 times greater than the population rate. (19). It is not clear why the incidence of fractures in the Australian patients is significantly greater than in our cohort.
We observed that clinical severity as defined by the RSSS is marginally related to BMD (p= 0.057) The scale which includes scoliosis, seizure frequency, and ambulation also includes factors such as head growth and respiratory irregularity which would not be expected to influence lumbar bone mass. A larger data set is required to confirm a relationship between RSSS and BMD.
Scoliosis with onset at a young age occurs frequently in patients with RTT. The early onset of RTT symptoms, decreased mobility at 10 months and non-ambulatory status have been identified as predictors of scoliosis in RTT (20). Also, low BMD has been reported in non-RTT adolescents with scoliosis (21). In agreement with Motil et al, we found that patients with scoliosis in excess of 20° were more likely to have BMC and BMD Z-scores lower than −2.0 but this relationship was not statistically significant. (17)
Bone loss and fractures are common in children with seizure disorders (22). The use of phenobarbital, phenytoin, carbamazapine and valproic acid may alter bone mass. We found that BMD Z-scores were not decreased with anticonvulsant drug use compared to non-users.(14). Leonard et al. reported a decrease in cortical thickness and cortical area in girls with RTT using anticonvulsants (15). Motil et al. reported no relationship to current anticonvulsant use, but did find lower BMC/BMD in individuals reporting prior use of anticonvulsants (17) A review by Gissel et al. of 14 published reports on the effect of anticonvulsant drugs on BMD in children is of interest (22). Six studies found no effect of cambamazepine on bone density, and equivocal results were reported for valproate effects on bone density (23). This suggests that multiple factors may influence the effects of anticonvulsants on bone metabolism: seizure frequency affecting dosage, vitamin D status or combinations of medications differing from those used in this cohort could influence the impact of anticonvulsants on bone mass.
Hypovitaminosis D is common in children with seizure disorders (24). Here, 42 % had serum 25 (OH) D levels in the D-insufficient or D-deficient range. While possibly related to anticonvulsant use, low serum vitamin D levels may be due to a lack of sunlight exposure and the difficulty of administering oral vitamin supplements. Bone biopsies in girls with RTT and mouse models of RTT confirm the impact of MECP2 mutations on bone (25, 26). Figure 6 illustrates the extent to which bone mass is decreased in 6 week old null (male) C57BL/6 RTT mice compared to control. Additional studies in our laboratory have demonstrated that the male homozygote shown in Figure 6 has decreased bone density, decreased bone mass, lower trabecular number and greater trabecular separation (data not shown) (Shapiro JR et al., Rett Syndrome: Bone Mass in Girls and Mice, 2009 ASBMR Meeting, April 27–29, 2009, Bethesda, Maryland, USA, Abstract 22: S499). Iliac crest bone biopsies in 5 RTT children, 9.5 to 14 years, showed decreased bone volume, decreased osteoclast surface and number, and a reduced rate of bone formation suggesting decreased osteoblast function (25). O'Connor et al. have reported histology in the male null mouse modelMECP2 −/yBird, which at postnatal day 60, had reduced skeletal size compared to wild type, decreased mineral apposition rate in trabecular but not cortical bone. and decreased cortical and trabecular bone volume (26). The numbers of calvarial osteoblasts/bone surface were decreased suggesting that osteoblast dysfunction was probably the primary cause of reduced bone volume in RTT syndrome.
In this series, the lowest values for BMC/BMD occurred in children with T158M and R270XMECP2 mutations (Figure 4). However, this did not reach statistical significance for either mutation, and is in keeping with the lack of relationship between MECP2 mutations and BMC or BMD observed by Motil et al. (17). A relation of BMD to the T158M mutation may lie in the observation that individuals with T158M mutations are more neurodevelopmentally affected than those with other mutations (27). In the cohort of 238 patients participating in research studies at the Kennedy Krieger Institute, mutations consisting of T-158M occurred in 12 % of the group. In these, seizures were frequent (60%), 53 % were not ambulatory and 44 % had scoliosis. A marginal relationship of clinical severity to BMD was observed here suggesting that a larger number of observations are required to clarify the role of these mutations. Downs et al. reported a positive relationship between the R270X mutation and fracture risk in Australian RTT individuals (19). We suggest that while factors, such as decreased ambulation, anticonvulsants, and scoliosis, may account for a portion of the decrease in bone mass, the deficiency seen in RTT bone mass may be the result of direct effects of the MECP2 mutations on osteoblast metabolism as suggested in human biopsy studies and observations in mutant mice (25, 26).
Recent studies involving leptin and neuropeptide Y2, have disclosed unrecognized interactions between the central nervous system, peripheral neurotransmitters and osteoblasts. (28, 29). In contrast to agents acting through intermediates such as the sympathetic nervous system or membrane receptors, MECP2 acts as a transcriptional repressor affecting the neural tissue (2). Neuronal tissue studies suggestMECP2 could affect osteoblast function by altering osteoblast chromatin structure as observed with brain chromatin, or by altering cell maturation as observed in RTT neuronal tissues (25, 30). Other CNS neurotransmitters altered in RTT patients could potentially influence osteoblast growth and maturation (31). Thus, the recognition of osteoporosis in RTT syndrome adds yet another dimension to our understanding of the possible role MECP2 and other neural factors might play in the regulation of bone metabolism.
Acknowledgments
Financial Support: This study was funded by grants from NICHD PO1-24448, and the Institute for Clinical and Translational Research, grants UL1RR025005 and FD-R-002408 [to S.N]. J.S. was supported by the Charitable and Research Foundation in Punta Gorda, Florida.
Abbreviation list
- BMD
Bone Mineral Density
- BMC
Bone Mineral Content
- CV
Coefficient of Variation
- DXA
Dual Energy Absorptiometer
- MECP2
methyl-CpG-binding protein 2
- RTT
Rett Syndrome
- RSSS
Rett Syndrome Severity Scale
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kozinetz CA, Skender ML, MacNaughton N, Almes MJ, Schultz RJ, Percy AK, Glaze DG. Epidemiology of Rett syndrome: a population-based registry. Pediatrics. 1993;91:445–450. [PubMed] [Google Scholar]
- 2.Bird A. The methyl-CpG binding protein MeCP2 and neurological disease. Biochem Soc Trans. 2008;36:575–583. doi: 10.1042/BST0360575. [DOI] [PubMed] [Google Scholar]
- 3. [Accessed, June 9, 2010];RettBASE IRSF MECP2 Variation Database. Available at: http://mecp2.chw.edu.au.
- 4.Guy J, Hendrich B, Holmes M, Martin JE, Bird A. A mouse MeCP2-null mutation causes neurological symptoms that mimic Rett syndrome. Nat Genet. 2001;27:322–326. doi: 10.1038/85899. [DOI] [PubMed] [Google Scholar]
- 5.Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nat Genet. 1999;23:185–188. doi: 10.1038/13810. [DOI] [PubMed] [Google Scholar]
- 6.Hagberg B, Hanefeld F, Percy A, Skjeldal O. An update on clinically applicable diagnostic criteria in Rett syndrome. Comments to Rett Syndrome Clinical Criteria Consensus Panel Satellite to European Paediatric Neurology Society Meeting, Baden, Germany, 11 September 2001. Eur J Paediatr Neurol. 2002;6:293–297. doi: 10.1053/ejpn.2002.0612. [DOI] [PubMed] [Google Scholar]
- 7.Trevathan E, Naidu S. The clinical recognition and differential diagnosis of Rett syndrome. J Child Neurol. 1988;3:S6–S16. doi: 10.1177/0883073888003001s03. [DOI] [PubMed] [Google Scholar]
- 8.Leonard H, Thomson M, Bower C, Fyfe S, Constantinou J. Skeletal abnormalities in Rett syndrome: increasing evidence for dysmorphogenetic defects. Am J Med Genet. 1995;58:282–285. doi: 10.1002/ajmg.1320580316. [DOI] [PubMed] [Google Scholar]
- 9.Hoffbuhr KC, Moses LM, Jerdonek MA, Sirianni N, Scacheri C, Giron J, Schuette J, Innis J, Marino M, Philippart M, Narayanan V, Umansky R, Kronn D, Hoffman EP, Naidu S. Associations between MeCP2 mutations, X-chromosome inactivation, and phenotype. Ment Retard Dev Disabil Res Rev. 2002;8:99–105. doi: 10.1002/mrdd.10026. [DOI] [PubMed] [Google Scholar]
- 10.Baim S, Leonard M, Bianchi ML, Hans DB, Kalkwarf H, Langman C, Rauch F. Official positions of the international Society for clinical Densitometry and Executive summary of the 2007 ISCD Pediatric Position Development Conference. J Clin Densitom. 2008;11:6–21. doi: 10.1016/j.jocd.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Kalkwarf HJ, Zemel BS, Gilsanz V, Lappe JM, Horlick M, Oberfield S, Mahboubi S, Fan B, Frederick MM, Winer K, Shepherd JA. The bone mineral density in childhood study: bone mineral content and density according to age, sex, and Race. J Clin Endocrinol Metab. 2007;92:2087–2099. doi: 10.1210/jc.2006-2553. [DOI] [PubMed] [Google Scholar]
- 12.Schwartzman F, Vitolo MR, Schwartzman JS, Morais MB. Eating practices, nutritional status and constipation in patients with Rett syndrome. Arq Gastroenterol. 2008;45:284–289. doi: 10.1590/s0004-28032008000400005. [DOI] [PubMed] [Google Scholar]
- 13.Tan KJ, Moe MM, Vaithinathan R, Wong HK. Curve progression in idiopathic scoliosis: follow-up study to skeletal maturity. Spine. 2009;34:697–700. doi: 10.1097/BRS.0b013e31819c9431. [DOI] [PubMed] [Google Scholar]
- 14.Chou IJ, Lin KL, Wang HS, Wang CJ. Evaluation of bone mineral density in children receiving carbamazepine or valproate monotherapy. Acta Paediatr Taiwan. 2007;48:317–322. [PubMed] [Google Scholar]
- 15.Leonard H, Thomson M, Glasson E, Fyfe S, Leonard S, Ellaway C, Christodoulou J, Bower C. Metacarpophalangeal pattern profile and bone age in Rett syndrome: further radiological clues to the diagnosis. Am J Med Genet. 1999;83:88–95. doi: 10.1002/(sici)1096-8628(19990312)83:2<88::aid-ajmg3>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 16.Haas RH, Dixon SD, Sartoris DJ, Hennessy MJ. Osteopenia in Rett syndrome. J Pediatr. 1997;131:771–774. doi: 10.1016/s0022-3476(97)70113-6. [DOI] [PubMed] [Google Scholar]
- 17.Motil KJ, Ellis KJ, Barrish JO, Caeg E, Glaze DG. Bone mineral content and bone mineral density are lower in older than in younger females with Rett syndrome. Pediatr Res. 2008;64:435–439. doi: 10.1203/PDR.0b013e318180ebcd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loder RT, Lee CL, Richards BS. Orthopedic aspects of Rett syndrome: a multicenter review. J Pediatr Orthop. 1989;9:557–562. doi: 10.1097/01241398-198909010-00010. [DOI] [PubMed] [Google Scholar]
- 19.Downs J, Bebbington A, Woodhead H, Jacoby P, Jian L, Jefferson A, Leonard H. Early determinants of fractures in Rett syndrome. Pediatrics. 2008;121:540–546. doi: 10.1542/peds.2007-1641. [DOI] [PubMed] [Google Scholar]
- 20.Ager S, Fyfe S, Christodoulou J, Jacoby P, Schmitt L, Leonard H. Predictors of Scoliosis in Rett Syndrome. J Child Neurol. 2006;21:809–813. doi: 10.1177/08830738060210091501. [DOI] [PubMed] [Google Scholar]
- 21.Lee WT, Cheung CS, Tse YK, Guo X, Qin L, Lam TP, Ng BK, Cheng JC. Association of osteopenia with curve severity in adolescent idiopathic scoliosis: a study of 919 girls. Osteoporos Int. 2005;16:1924–1932. doi: 10.1007/s00198-005-1964-7. [DOI] [PubMed] [Google Scholar]
- 22.Coppola G, Fortunato D, Auricchio G, Mainolfi C, Operto FF, Signoriello G, Pascotto A, Salvatore M. Bone mineral density in children, adolescents, and young adults with epilepsy. Epilepsia. 2009;50:2140–2146. doi: 10.1111/j.1528-1167.2009.02082.x. [DOI] [PubMed] [Google Scholar]
- 23.Gissel T, Poulson CS, Vestergaard P. Adverse effects of epileptic drugs on bone mineral density in children. Expert Opin Drug Saf. 2007;6:267–278. doi: 10.1517/14740338.6.3.267. [DOI] [PubMed] [Google Scholar]
- 24.Nettekoven S, Strohle A, Trunz B, Wolters M, Hoffmann S, Horn R, Steinert M, Brabant G, Lichtinghagen R, Welkoborsky HJ, Tuxhorn I, Hahn A. Effects of antiepileptic drug therapy on vitamin D status and biochemical markers of bone turnover in children with epilepsy. Eur J Pediatr. 2008;167:1369–1377. doi: 10.1007/s00431-008-0672-7. [DOI] [PubMed] [Google Scholar]
- 25.Budden SS, Gunness ME. Possible mechanisms of osteopenia in Rett syndrome: bone histomorphometric studies. J Child Neurol. 2003;18:698–702. doi: 10.1177/08830738030180100401. [DOI] [PubMed] [Google Scholar]
- 26.O'Connor RD, Zayzafoon M, Farach-Carson MC, Schanen NC. MeCP2 deficinecy decreases bone formation and reduces bone volume in a rodent model of Rett syndrome. Bone. 2009;45:346–356. doi: 10.1016/j.bone.2009.04.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Archer H, Evans J, Leonard H, Colvin L, Ravine D, Christodoulou J, Williamson S, Charman T, Bailey M, Sampson J, Klerk N, Clarke A. Correlation between clinical severity in patients with Rett syndrome with a p.R168X or p.T158M MECP2 mutation, and the direction and degree of skewing of X-chromosome inactivation. J Med Genet. 2007;44:148–152. doi: 10.1136/jmg.2006.045260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allison SJ, Baldock PA, Herzog H. The control of bone remodeling by neuropeptide Y receptors. Peptides. 2007;28:320–325. doi: 10.1016/j.peptides.2006.05.029. [DOI] [PubMed] [Google Scholar]
- 29.Elefteriou F. Regulation of bone remodeling by the central and peripheral nervous system. Arch Biochem Biophys. 2008;473:231–236. doi: 10.1016/j.abb.2008.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chadwick LH, Wade PA. MeCP2 in Rett syndrome: transcriptional repressor or chromatin architectural protein? Curr Opin Genet Dev. 2007;17:121–125. doi: 10.1016/j.gde.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Johnston MV, Blue ME, Naidu S. Rett syndrome and neuronal development. J Child Neurol. 2005;20:759–763. doi: 10.1177/08830738050200091101. [DOI] [PubMed] [Google Scholar]