Abstract
We report a patient with epilepsia partialis continua (EPC) associated with non ketotic hyperosmolar hyperglycemia. EPC is an uncommon presentation of nonketotic hyperglycemia. This case was reported in the Medical Intensive Care Unit in Hamad Medical Corporation, Doha, Qatar.
Keywords: Epilepsia partialis continua, hyperglycemia
Introduction
The association between non-ketotic hyperglycemia (NKG) and epilepsia partialis continua (EPC) is rare but well known. We report a patient who presented with NKG and EPC who was admitted to the Medical Intensive Care Unit (MICU) in Hamad Medical Corporation in Qatar. It is vital to recognize the association between those conditions as correcting the metabolic abnormalities is the main step to treat the seizures [1].
Case report
A 52 years old Pakistani right handed woman presented to Emergency Department with polyuria and polydepsia for four days. Also she had recurrent abnormal movements in the left hand with progressive involvement of the upper limb that started abruptly three days earlier. There was no significant past medical history. She was not taking any medication. The blood sugar was found to be more than 24 mmol/l when tested by glucometer in the emergency department. The vital signs, heart, lung and abdominal examination were normal apart from sinus tachycardia. However, her head was intermittently turning to the left side with abduction and external rotation of the left arm. Glasgow Coma Scale was 10/15.
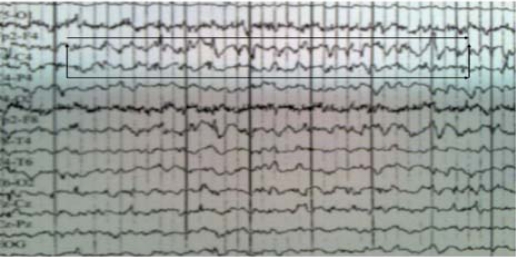
Laboratory results showed that blood sugar of 96 mmol/L (1728 mg), serum sodium of 123 meq/L, potassium level of l 5.6 meq/L and serum osmolarity of 375 mOsm/L. There were negative ketons in blood and urine with bicarbonate level of 24 mmol/L. Blood gases showed normal Ph 7.39. Cerebrospinal fluid analysis showed normal cells, protein and high glucose level (22 mmol/L). Computerized tomography (CT) and Magnetic resonance imaging and (MRI) of brain were normal. Electroencephalogram (EEG) showed frequent epileptiform discharges involving the right frontocentral area which is consistent with EPC (Figure 1). Carbamazepine 400 mg daily was started. Correction of metabolic disorder (Nonketotic hyperglycemia) with proper fluid replacement and insulin intravenous drip resulted in a gradual reduction in the number of seizures until they stopped three days later. The patient stabilized and was transferred to the medical floor. She was seen by a diabetic educator and discharged home in good condition. Carbamazepine was discontinued one month after discharge. No seizures were reported during nine months of follow up.
Figure 1.
Discussion
Seizures may result from any metabolic disorders but are not commonly associated with nonketotic hyperglycemia [1, 3]. The pathogenesis of seizures from metabolic disorders are not completely understood. Hyperglycemia may precipitate EPC by reducing gamma-aminobutyric acid levels leading to a lower seizure threshold [3, 4]. On the other hand, seizures are not usually associated with diabetic ketoacidos as ketosis and intracellular acidosis probably increase the seizure threshold [1]. Hyperglycemia may also precipitate EPC if there is asymptomatic structural cerebral lesion [1]. However, this is not the case in our patient as both CT and MRI brain were normal.
EPC is defined as a clonic muscular twitching repeated at fairly short intervals in one part of the body for a period of minutes, hours, days or weeks [5]. It is a form of focal status epilepticus manifesting as a continuous focal motor seizures [6]. It is usually associated with a wide range of EEG abnormalities including focal spikes and focal slow waves [6]. EEG was reported to be normal in some cases of EPC [7].
Many conditions have been reported as a cause of EPC including structural abnormalities such as central nervous system tumors, trauma, cerebral infarction, intracerebral hemorrhage, cerebral abscess, and vascular malformation [6]. However, in up to 50% of cases conventional brain imaging may be normal [7]. Metabolic abnormalities especially hyperglycemia, hyponatremia, and hepatic encephalopathy are a well known causes of EPC [1]. The majority of cases with EPC are precipitated by hyperglycemia which occurs before impairment of consciousness; therefore it is important to recognize this association [5]. This could lead to the diagnosis of previously undiagnosed diabetes mellitus and early reversal of the neurological condition.
Our patient was treated with insulin, intravenous fluids and a carbamazepine 400 mg daily. Her seizures resolved quickly and she has not had any recurrence.
References
- 1.Singh BM, Strobos RJ. Epilepsia partialis continua associated with nonketotic hyperglycemia: clinical and biochemical profile of 21 patients. Ann Neurol. 1980;8:155–160. doi: 10.1002/ana.410080205. [DOI] [PubMed] [Google Scholar]
- 2.Maccario M, Messis CP, Vastola EF. Seizures as manifestations of hyperglycemia without ketoacidosis. Neurology. 1965;15:195–206. doi: 10.1212/wnl.15.3.195. [DOI] [PubMed] [Google Scholar]
- 3.Hennis A, Corbin D, Fraser H. Focal seizures and non ketotic hyperglycemia. J Neurol Neurosurg Psychiatry. 1992;55:195–197. doi: 10.1136/jnnp.55.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Placidi F, Floris R, Bozzao A, MD, Romigi A, et al. Ketotic hyperglycemia and epilepsia partiais continua. Neurology J. 2001 Aug;57(3):534–537. doi: 10.1212/wnl.57.3.534. [DOI] [PubMed] [Google Scholar]
- 5.Gillian H. B, Julian R, Simon B. An unusual presentation of a common disorder. Postgrad Med J. 2000;76:373–375. doi: 10.1136/pmj.76.896.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schomer DI. Focal status epilepticus and epilepsia partialis continua in adults and children. Epilepsia. 1993;34:29–36. doi: 10.1111/j.1528-1157.1993.tb05904.x. [DOI] [PubMed] [Google Scholar]
- 7.Cockerell OC, Rothwell J, Thompson PD, et al. Clinical and physiological features of epilepsia partialis continua. Brain. 1996;119:393–407. doi: 10.1093/brain/119.2.393. [DOI] [PubMed] [Google Scholar]