Abstract
In the last four decades, there has been a substantial horizontal expansion of health services in Libya. This resulted in improvement in morbidity and mortality, in particularly those related to infectious disease. However, measures such as the national performance gap indicator reveal an underperforming health system. In this article, we discuss aspects related to the Libyan health system and its current status including areas of weakness. Overcoming current failures and further improvement are unlikely to occur spontaneously without proper planning. Defining community health problems, identifying unmet needs, surveying resources to meet them, establishing SMART (specific, measurable, achievable, and realistic and time specific) objectives, and projecting administrative action to accomplish the proposed programs, are a must. The health system should rely on newer approaches such as management-by-objectives and risk-management rather than the prevailing crisis-management attitude.
Keywords: Libya, Health Services, Health crisis, Health reform, Management-Quality
Introduction
Health systems in different countries vary widely in performance and their ability to attain key health goals [1]. In many countries, despite expansion of medical knowledge and the use of increasingly sophisticated technology and training, the quality of care as a return on expenses reveals under-performing systems. Health care delivery in these circumstances is considered to be in crisis [2, 3]. To achieve higher standards of health care, both wealthy and poor health systems should continually strive to improve efficiency, equity and effectiveness of their programs [3, 4]. There is no simple stereotyped formula for the organization of health services. Appropriate policies may differ widely across settings, but no country has discovered an ideal model [5]. Much remains to be learned about what makes a good health system, what makes it fair, and how do we evaluate the performance of existing systems in different settings.
The aim of the current study is to discuss some of the most important aspects concerning Libyan National Health Services (LNHS), its current status, areas of weakness, and how to overcome current failures in the light of present views of the best known methods of health service organization. We are adopting a qualitative approach based on interviews with decision makers, active personnel with academic experience, and from analyses of data from archived documents from different sources published by health and/or general authorities. This qualitative approach is widely used and is increasingly accepted in health research [6]. Known shortcomings include subjective experience which may alter appreciation, interpretation, or judgment.
Settings and background
Libya is an intermediate level income country. The per capita income is more than $7000 US per annum [7]. The main source of income is from oil revenue, petro-chemical industry, and agricultural activities. Eighty five percent of its approximately five million inhabitants live in urban areas. They are, however, distributed over a large surface area, making it one of the most sparcely populated countries in the world. The annual population growth has dropped to less than 2.9% in recent years. The share of public health expenditure from total gross domestic product (GDP) expenditure is around 3% [8]. Healthcare and education services are provided free to all citizens. Education became compulsory in the early 1970s. Libya boasts some of the highest literacy and educational enrollment in developing countries. The net enrollment rate in basic education is 96% with only a 1% absence rate. Female youth illiteracy is <7% [9]. Ninety five percent of the population has access to safe drinking water and 86% have adequate sewage disposal [8].
Health status in Libya
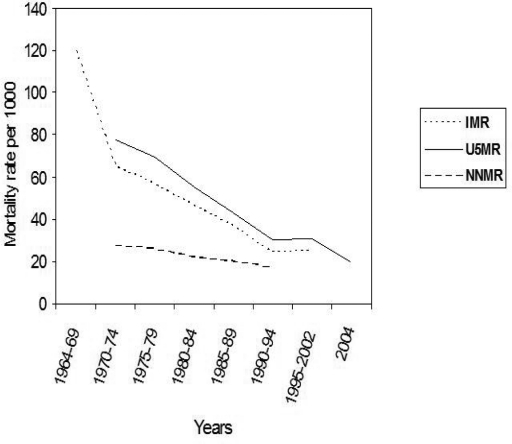
There is a strong component of public health in LNHS. The distribution of inhabitants in the country's large surface area puts a strain on the availability of infrastructure to provide for all the population. Overall the health status has changed from a high prevalence of infectious diseases and significant mortalities, to one where morbidity and mortality is more often linked to noncommunicable chronic disease (NCD) [8]. As elsewhere, today's survival and death rates in Libya are a reflection of the quality of earlier health care [10]. It is noteable that during the 70s and 80s, there was a substantial expansion of social services, such as health, education, and sanitary services. There are now 102 public hospitals and specialized centers, 1177 primary health care facilities, and 14 physicians and 39 beds per 10,000 population [7]. The immunization coverage for tuberculosis is >97%, and measles is >95% [8]. The proportion of low birth weight infants is <5% while 99% of deliveries are attended by healthcare personnel [11]. Life expectancy at birth is 70 years [12]. The crude death rate is 7 per 1000 inhabitants. Under- five (U5MR) and infant (IMR) mortality rates have significantly dropped with the U5MR being 20 per 1000 live births for 2004 (Figure 1) [11, 12].
Figure 1.
The steady decline in child mortalities indicators related to overall socioeconomic conditions [IMR Infant mortality rate and U5MR underfive mortality rate] versus nearly constant level of child mortality indicator related to quality of health service [NNMR neonatal mortality rate] in Libya during the period 1964–2004.
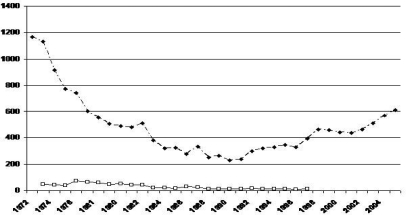
For many years there were no reports on poliomyelitis, diphtheria, neonatal tetanus, or cholera. The number of notified cases of tuberculosis and leprosy reported to the secretariat of health had significantly dropped during the 70s and 80s (Figure 2). In fact, 11 of 12 global indicators of Health for All by 2000 were believed to be achieved by the end of last century in Libya [13].
Figure 2.
Secular trend in notified cases of tuberculosis and leprosy in Libya during the period 1972–2005.
However, U5MR and IMR, which are reflections of overall socioeconomic status, nearly reached a plateau state. Meanwhile, neonatal mortality, which is a reflection of quality of healthcare services, only slightly dropped from 21.9 to 17 per 1000 live births during the whole period (Figure 1). As elsewhere, the unfinished agenda of communicable disease control is complicated by the emergence of new diseases, notably the NCD diseases [14]. Figure 2 shows that tuberculosis is a re-emerging disease as it increased threefold over the last fifteen years. In addition, the general public remains unsatisfied with the hospital based health services. The LNHS are facing rough competition from emerging medical tourism in the region [15]. In spite of obvious improvements in the overall health of Libyans in the last generation, it is clear that further improvements will not occur due to progress in socioeconomic conditions or other non specific measures alone. It is an ongoing effort to maintain our current ability to care for our citizens while we seek new methods to improve present healthcare delivery as well as having a keen awareness of changing needs.
Regulations
The most important health legislation in Libya was the Public Health Code No 106 (1973), further detailed in the decree 654/1975 issued by the General People's Committee. The code defined the responsibility of the state to provide free health services to all citizens. Other legislation includes the Health Act No24 of 1994/1423 that gave a fundamental position for primary healthcare within the LNHS, the Medical Responsibility Act (17/1986), and a series of legislations (No9/1992, No6/1430, and 535/1993) that regulated the involvement of the private sector in healthcare. Another important strategic legislation was issued by the General People's Committee 828/1423 that targeted the self-dependence in human resources [8]. In reality, there have been no real major changes in health legislation since the Public Health Code No 106/1973. For example, the list of additives or contaminants that should be examined in the food supply remains limited. The methods specified for their detection are outdated.
Decentralization and Community participation
Until recently, the organization of LNHS was characterized by a vertical and horizontal integration. There are obvious attractions in moving away from the highly centralized approach adopted in the early years [16, 17]. Frequently, administrators complain that managers in peripheral units of administration do not follow decisions made by central authorities. The organization has changed to that of vertical segmentation and horizontal integration that is aimed at by most of the current reform proposals for health systems in the world [1]. With the recent changes, Libya is now made up of 32 Shaabia (municipality) and three administrative districts containing 350 basic peoples’ congresses. Health is managed through the people's committees in the municipalities (Shaabiat). In each Basic Peoples’ Congress there is a member responsible for the management and follow-up of health within the administrative borders of the congress. In each Shaabia, there is a secretary for health who is selected from among the members of health in the basic peoples’ congresses. The Shaabia's Secretary is responsible for the implementation of health policy within the borders of the Shaabia. The supposedly decentralized administration and decision-making (Alshaabiat and Almahalaat) should theoretically be unique opportunity since the community is not only informed, involved, or participate in health, but is empowered in making decisions. Empowerment is the highest level of participation. However, useful decision requires well-informed people. Absence of information and explanation from professionals, uncertainty about level of awareness and education level could undermine the participation of the community.
Intersectoral cooperation and advocacy
Health care is a joint effort [18]. It involves other sectors such as agriculture, animal husbandry, food, industry, education, housing, public works, communication, transportation etc. This involvement is a part of the stewardship function of the state. National comprehensive programs that coordinate these different sectors are absent from both legislative and executive levels. Nutrition, for example, where adequate food supplies rely on agriculture, industry, and transport while its utilization is related to education and economy. Since the 1970s, short and intermediate term solutions for subsidizing policies on imported food items have been extensively applied to improve the nutritional status of the population and improve nutrition.
These actions had many disadvantages even from the health point of view. Besides discouraging local production, they encourage consumption of nutritional goods of low nutritional values by consumers who have enough calories, thus increasing the prevalence of different forms of malnutrition. In fact, overnutrition is a public health problem in Libya and is due to poor quality rather than inadequate feeding [15]. Another example is that the main cause of death in children after the first year of life is road traffic accidents [19]. In this condition, the role of intersectoral cooperation and coordination with the education, transport, circulation and civil engineering sections cannot be emphasized enough.
Conceptual framework in healthcare and implications for Libya
Health services should have an essential broad category package. An example of this package is shown in Table 1 [20]. The main goals of any health system should be: better health, responsiveness to the population's expectations and fair financing. Underpinning the entire workings of the system are four key functions that explain variation in performance; stewardship (a broader concept than regulation); financing (including revenue collection, fund pooling and purchasing); service provision (for personal and non-personal health services); and resource generation (including personnel, facilities and knowledge) [1]. The configuration and the application of state authority in the health sector should be re-aligned so as to achieve desired policy objectives [21]. Current opinions favour a substantial role for the State in the health sector [22, 23]. In LNHS, the blurred global vision for health services is evident in the absence of distinction in what constitutes a research centre and its difference from research council. This has even worsened with the national health and pharmaceuticals research center taking actions in service delivery [8]. Current opinions favour a substantial role for the State in the health sector [22, 23]. There is a rising role of the private medical practice (PMP) in the LNHS. However, this is leading to a situation where health care is delivered through a fragmented system of independent practitioners. It is of most importance to determine the role of government in regulation of PMP, the public-private interface and the role of the private sector in public health [22, 24]. Reform and privatization are not clearing the State from its responsibility towards its citizens. The State has to keep its stewardship role including intersectoral advocacy [1]. In LNHS, the blurred global vision for health services is evident in the absence of distinction in what constitutes a research centre and its difference from research council. This has even been worse where the national health and pharmaceuticals research center taking actions in service delivery [8].
For an organization to become and remain viable in a complex and rapidly changing environment, it must carry out certain functions. First, it should provide a product or a service that addresses particular needs in the organization's environment; second, it should ensure that the operational units work together and communicate effectively; and it should support and have a control especially with regard to distributing resources, providing training, gathering and distributing information about quality, etc. The fourth essential function is intelligence where it should forecast future needs, opportunities, and threats. The organization should set a policy with long-term goals and objectives [20]. Neither clinical nor health policy can be comfortably based on opinion alone [25]. Public health practices are likely to be shaped by the resources available, the ways in which the resources are organized, and the characteristics of the community or market served. Services should not be based on the availability of doctors or an empiric study where a questionnaire is distributed by convenience to doctors met in congresses as we have seen, but should be based on whether we need this particular service or not. Services should be determined according to disease burden studies derived from morbidity and mortality patterns which would identify the needs of the population and taking into account the populations’ demands. Basic amenities of health services, such as clean waiting rooms or adequate beds and food in hospitals are aspects of care that are often highly valued by the population [1], but are very poorly assured by the public national hospital services.
Various attempts and procedures had been tried in the past but were not sustained. Too many changes, especially when not well introduced, might lead to loss of credibility and to loss of the cooperation of service consumers, who are the most important element of change. Cooperation would be even worse if consumers are asked to contribute financially without clear perceived benefits. This occurred in the mid nineties when some pilot hospitals imposed a conceptually poorly defined payment scheme system. To facilitate change and make effective improvement in the health services we need a dedicated, internal change agent; clear purpose, benefits and expected results; clear responsibilities assigned; long-term support for staff; and an organizational environment that is open to change [26]. Designing a national strategy for healthcare is not the difficult part. It is the implementation of that strategy and making it “work” which is the most difficult task [27].
Some policies, introduced with the best of intentions, have the opposite effects of those that are desired. In the mid nineties, an urgent mass vaccination program was advocated for managing the presumed meningitis outbreak inspite of the absence of evidence of an outbreak. The proposed action probably not only increased exposure to other pathogens, but it also raised unnecessary fears, and frustration among the population that could not be vaccinated due to absence of enough stock of the vaccine. There is a need to introduce system thinking and system dynamics for studying and managing complex feedback systems, and to anticipate counter-intuitive effects of public health initiatives. Measures taken should thoroughly examine the objective of concern, be appropriate, and forecast possible disturbance that could result from unbalancing the system. Other examples include legislation that the national supplier of salt in Bukammash should iodize salt. It has neglected other restructural economic activities and consumptions patterns which encouraged local small scale production of non-iodized salts that were cheaper. It neglected also, the source of salt in some rural areas in the south where salt is readily available in nearby valleys. A decree forbidding practicing in public and private sectors concomitantly should aim a wide package of interventions rather than merely summarizing all health problems to this particular issue.
With the increasing role of PMP and medical tourism in the region, public policy should not ignore the need to organize the private sector and address such issues as ambulatory care. Family physicians had been accepted as the backbone of the LNHS and as the clinical arm of primary health care. It was implemented as a pilot project in a few sites. However, the concept and its application are facing many difficulties that are also seen in other parts of the world [28, 29].
Planning and management
Proper planning and management are needed for primary, secondary or tertiary level establishments as well as for public, private or non-profitable organizations [30]. For years, the mission of projects and planning department in health was limited to building and construction. Unless planning is provided, required achievements would become more and more difficult by just spontaneous improvement in overall socioeconomic conditions. Health planning is a cycle, and a check on our abilities to achieve our objectives/targets should be made. Many vertical programs endorsed by international and/or regional organizations as the WHO or the UNICEF were accepted and adopted by health authorities in Libya. Examples are health for all program, national programs for accidents; national immunization; maternal and child health; drug policy; breastfeeding and the baby friendly hospital initiative; diarrheal diseases; and respiratory infections control programs. However, there is obvious failure to institutionalize most of these programs. No objectives are stated and no proper assessment or formal follow-up is performed so that achievements can be evaluated. Good objectives should be SMART and related programs must be closely integrated with these objectives.
Libya's highest legislative authority had adopted the primary health care approach. The official position of health authorities is still to be committed to its adoption and application [18]. However, talking now about Alma-Ata declaration and our intention to adopt it and to adopt the primary health care strategy is outdated [18]. Intentions or willingness should give its place to plans, and evaluation should be expressed in figures. What should be raised now is; what was our initial position? What were our objectives at that time? What had been done since? What is our status now? How to interpret our position? Was this satisfactory? Why is it as such? Whether there had been some changes in our priorities with the time? And what is our next step to overcome obstacles?
The predominant form of management in the Libyan health sector is crisis -management. An example of this type of management is the Ejdabia Cholera outbreak that occurred in 1995. In this event, both owners and inhabitants of an old part of the city refused to pay a small fee to be connected to a new water pipeline system to the city. Inhabitants (all are immigrants) thought that it was cheaper for them to dig individual wells for themselves inside their houses. More than 290 of the unauthorized 300 wells were unsuitable for human use due to fecal contamination. The problem with crisis management is that when a crisis occurs, damages are inevitable. These would include for example; mortality and morbidity; material damage; allocation of human and financial resources; public insatisfaction; loss of confidence in the system; and other intangible losses. This outbreak should have been anticipated by setting appropriate objectives. The objective should have been safe water supply to all residents. The occurrence of the outbreak in the city cost more losses than actions that were needed to insure the aforementioned objective. There are other lessons that could be drawn from this outbreak. Examples include the value of intersectoral cooperation and advocacy, equity, and the concept of global approach to development [18]. In fact, the next change in the government was to combine health, education, environment, facilities and construction sectors in one secretariat for public services. This approach also failed due to absence of strategic global thinking in health and other executive authorities.
Risks should be managed, picked-up, and dealt with before the occurrence of crises. This is the risk management. Still better, a more comprehensive approach of management is the Performance management. This is a mixture of policy instruments that embraces elements of planning and competition, directives and incentives, and centralization and devolution [16, 17].
Data-information-intelligence cycle and surveillance
A health system that is not able to recognize and continuously assess morbidity and mortality patterns of the population that it serves, is unlikely to meet the needs and demands of its population. Mortality indicators are the most basic tools in epidemiology. While the central role of health authorities is to decrease mortality and morbidity; there is no processed data on causes of death according to region, age and sex in Libya. This occurs in despite the fact that no less than 90% of deaths are reported to civil registration system. In spite of decrees from central health authorities, and that were later re-inforced in mid 90s, concerning forms to be fulfilled by health workers for recording activities and other documentations, there is no proper data collection for health information systems [8]. Forms and legislations are only a part of the system. Neither training is provided, nor output is generated, nor feed-back is guaranteed. Furthermore, data is usually neither comprehensive, nor purposeful, nor organized. Even when it is present, it is not processed to information or related to goals, objectives or targets. Most communications from health authorities is in the form of unprocessed data. This accumulation of purposeless or meaningless data is not only inappropriate but is also harmful as it gives the impression of a movement or that we are doing something.
Intelligence is the transformation of information through integration with experience and perceptions based on social and political values [30]. Information would have no meaning if necessary actions are not taken to tackle these problems and try to solve them. Intelligence would reallocate resources to the changing patterns of mortality and morbidity. Examples include the increasing burden of cardiovascular diseases (37%), cancers (13%), and road traffic accidents (11%) as the current main causes of mortality [8]. The increased disease burden from these NCD should have promoted integrated actions [31]. Yet, there are no national comprehensive programs that are adopted to deal with these diseases. A good and exceptional example of the data-information-intelligence cycle was the mass vaccination campaign that was implemented lately upon realizing the changes in disease patterns due to previous moderate success of the national immunization program.
In surveillance, the list of notifiable diseases now contains more than 40 different infections [8]. However, nothing is programmed to be done specifically for any of these infections.
For a small population scattered over a large surface area as in Libya, the potential of e-health solutions as electronic medical records for health service management and telemedicine are obvious [32, 33]. These are not yet applied in health establishments. These would enhance coordination of clinicians, reduce inefficiency, increase effectiveness and overall quality, and improve safety [32, 34]. It is unfortunate that diseases are not yet reported or coded with international coding systems.
Health knowledge and education
There is a wide criticism to the way how information about outbreaks of infectious diseases such as cholera, HIV/AIDS, etc are handled in most parts of the world. In Libya, a study on the knowledge of females on the basic child health facts showed poor knowledge in various aspects of child health (Personal communication). The knowledge did not increase with educational level. This low level of education in items related to health inspite of the high education enrolment and compulsory education is problematic. The only relatively average reply was that for the role of bottle feeding in diarrhea and infant mortality. The role of media should be strengthened as this particular message was frequently conveyed by the media at that time. In another study, more than one third of children's deaths were related to respiratory infections and diarrheal diseases [19]. Both should be largely prevented by established WHO vertical programs and by using effective and efficient means that rely mainly on maternal health education.
Equity
Reducing health inequalities was at the center of Libyan national health policy during the seventies. There is no evidence for gender discrimination as indicated by the prevalence of undernutrition [11, 35]. Nevertheless, in spite of the horizontal expansion of social services and a resultant bias towards rural areas, some of the indicators are more common in rural areas and in certain regions [11, 35]. These differences may be due to the concentration of local human resources (HR) in certain regions, or may be due to cultural, educational, accessibility, life style or other factors. The horizontal expansion that occurred in the last decades should be now strengthened by vertical equity especially in these district areas.
Every policy within or outside the health sector should be critically examined as to its likely impact on equity in health. Examples include, macroeconomic policies, structural economic readjustment programs through its effect on public investment in health and other social sectors, and the increasing contribution of the private market in health delivery. Procedures for treatment abroad change frequently, and do not usually cover all needed cases. This is a very delicate issue that needs reconsideration in view of the importance of equity associated with it. Furthermore, because the LNHS are delivered free, equity for treatment abroad would be difficult to achieve without payment recovery schemes. The rational for redistribution of income from better-off to less well-off citizens, on the grounds of solidarity and justice, has its roots in early Islamic teachings.
Resources
Physical resources
Severe resource constraint is a major issue in designing and managing health services in developing and industrialized nations alike [14]. Many factors contribute to increases in health expenditure. These include increases in the size of the population, new expensive modes of treatment, changing patterns of disease, discovery of new illnesses, and the expected further wave of high-tech medicine that is coming over the horizon. It is vital to ensure that the limited resources are wisely spent so as to achieve the maximum returns for minimum spending.
The per capita total expenditure on health in Libya in 2003 was 327 $ [12]. The share of public health expenditure was generally about 3% of the total GDP expenditure through-out the first half of the current decade [8]. In absolute terms, this is more than that of most of developing countries, but is low relative to total GDP. Public health expenditure in Libya should ideally be increased in the context of good governance [8, 24]. While oil is the backbone of the Libyan economy, its price is fluctuating. If healthcare spending would have continued to outpace income growth, at a certain theoretical point period, the whole budget would go to healthcare. Similar projections in the USA indicate that with the current trend, healthcare spending would jump from the current 1/6 to 1/3 of American national output by 2040 [36]. In Libya, the main focus in public expenditure has always been on effectiveness and not efficiency. The problem is that effectiveness would be affected sooner or later. Tripoli medical center alone spent 18 of the 250 million Libyan Dinars (7%) that formed the total health budget expenditure in many years throughout the 90s. This should have been assessed in terms of effectiveness, efficiency and efficacy.
Different nations have rationed health care for years by restraining the rate of social spending, setting health care budgets or regulated fees, effectively controlling the numbers of hospitals or the amount of medical equipment, or other devices and thus endangering quality [36]. In the 70s and 80s, the health budget in Libya was prepared centrally according to perceived needs on the bases of data collected from peripheral units. These peripheral units built their budget simply by increasing previous years’ budget by 30%. Growth of health budget had to be restrained in the late 80s, and the number of hospital beds has been arbitrarily limited to 20000 beds in the early 90s to decrease expenditure. It is more important that terms as analytical accounting, efficiency, priorities settings, the contributory principle, risk extrapolation on the budget, and prevention of moral hazards should find their place in LNHS. In the absence of analytical accounting and cost recovery system, financing health expenditure will be more difficult to control.
Another source of financing health comes from PMP. All over the world, in opposite to previous expectations, PMP did not just disappear [37]. Neither this is likely to occur, nor is it beneficial to do so. Libya is not an exception to the growth in PMP. Most payments in PMP in Libya are out of pocket payments. The private market's over reliance on consumer oriented systems should not be the only option. Central authorities should play a constructive and cogent role [38]. Cost recovery schemes should be able to depoliticize treatment abroad.
About $100–200 million are spent annually by the state for medical treatment of Libyan citizens abroad [8]. More is spent as an out of pocket payment by Libyans traveling for treatment to neighboring countries and Europe. Treatment abroad for difficult cases should be anticipated by disease burden and expenditure assessment for maximum cost-benefit. Detrimental effects from the growing market of medical tourism in the region should be monitored and necessary measures should be taken in terms of competitiveness, effectiveness and efficiency of local health services as most of health indicators are in favour of LNHS [12].
Human resources
Weakness of human resources (HR) will limit the impact of any new resources [14]. Unless mechanisms of acquisition of knowledge and practical training of HR are ensured, their quality would be questionable. The proportion of imported HR in Libya has dropped from more than 80% in the seventies to less than 8% in 2005 [8]. It is unlikely that the reliance in Libya on imported HR will stop completely. Efforts should also be strengthened to diversify skills and training of local HR and to develop an evidence base HR for health services [5]. Different medical disciplines grow by about 10% each year. Nevertheless, a system for training on new procedures or techniques is non-existent and when it does, it is non-transparent and not well organized. For years, universities had no subscriptions to periodicals. The educational system behaves as if specialists do not need continuing education. There is no system for attending congresses. Physicians who are given a chance to attend medical conferences abroad, are never accountable to present summaries of such conferences to their departments.
Capacity building with new approaches as problem based learning, value of researches and joint education with other professional disciplines should be instituted to undergraduate medical education [25]. The use of monetary and non-monetary incentives is of crucial importance for all HR [39]. Valuing staff, as by the recent increase in incentives for staff working in public hospitals, is a good start that should be extended and generalized.
The situation is even more critical in paramedical specialties with absence of diversity, narrow range of professions available and the low level of training. There is a large drop-off among graduated nurses in Libya. Reasons for this drop-off should be addressed taking into account factors exogenous to the health system and should be treated appropriately [5].
Training and knowledge acquisition of manpower should be supported by documenting resources using e-health solutions including access to specialist databases [25]. However, there is no national policy for prioritizing and categorizing knowledge resources and linking them together by a central organization in a national or an international projects as HINARI, eIFL.net or similar projects [40].
Quality of health services
Quality of care is a multidimensional concept. It is vital that poor performance is recognized and addressed [25]. Recognition of failures in standards of care surveillance is essential for proper function of health services delivery [25]. Following the previous stage of horizontal expansion in LNHS, a vertical expansion should be installed to improve quality.
Quality of care could also be improved by increasing the role of patients [41]. While there is a rising unsatisfaction of the population with national health services, there is no system for its monitoring as through detection of complaints, audit, untoward incidents, or routine surveillance.
Evaluation should be a continuous process at periodic intervals rather than a sporadic event. It should be practiced by independent external bodies, the functions of which should be inspecting, investigating, advising, supplying expertise, facilitation and accreditation [25]. It is not simply administrative, as we see by the inspection department or the general monitoring and accounting council, but rather should be related to suitable targets and objectives. Quality improvement with punitive approaches should not be encouraged. They should be replaced by a life-long learning attitude [42]. The focus should be on introducing rigorous measurement to the business of improvement, rather than making judgments and scapegoating [43].
Well managed organizations are those in which financial control, service performance, and clinical quality are fully integrated at every level [25]. Managers should not make their decisions in isolation. Practices should be evidence based. Projects should not be limited to buildings and construction but should include goals, objectives and targets. Audit should not be restricted to inspection of administrative procedures but rather performance assessment. Current mass screening programs in Libya as pre-employment medical fitness examination have poor yield and should be re-evaluated. Improvement could be accomplished in different organisms(organizations?) by new approaches such as clinical governance. Clinical governance is not applied in districts or hospitals. Recently, some form of independence was given to some hospitals as Tripoli Medical Center. However, this is far from achieving any standards of clinical governance.
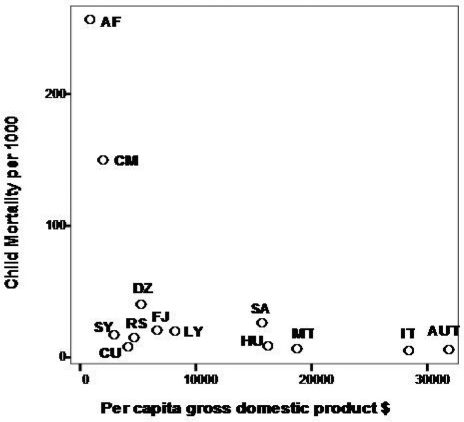
Various performance indicators were developed for monitoring, assessing, and managing health systems so as to achieve effectiveness, equity, efficiency, and quality [44]. These outcome indicators should be properly selected and should be relevant to the objectives of care. Well defined indicators make objectives clear and clarify duties of health services. There should be appropriate selection of useful indicators to monitor progress and assess the effectiveness of proposed projects, programs, and policies in reaching their stated goals. A good example of intelligent indicator is the UNICEF‘s National performance gap where the observed level of the specific health indictor is compared with the rate predicted on the basis of per capita GDP of the country (Figure 3). Best performing countries are those in the left lower corner, while the worst are those in the left upper zone. The figure depicts a low performance system in Libya.
Figure 3.
National performance gap scatter plot showing children mortality in some chosen countries in relation to per-capita gross domestic product. [SY: Syria, SA: Saudi A, RS: Serbia, MT: Malta, LY: Libya, IT: Italy, HU: Hungry, FJ: Fiji, CU: Cuba, CM: Cameroon, UT: Australia, DZ: Algeria, AF: Afghanistan]. Higher mortality or intermediate mortality in spite of higher income depicts low performance systems.
Services should not only be assessed in terms of their effectiveness or the ability to make desired changes, but also in relation to their efficiency or how much does it expend in terms of resources to make the desired change. There is always concern about the use and abuse of publicly available indicators [42]. The evaluation of performance of hospitals as was done in the 90s solely on the basis of proportional mortality is a crude and non-sensitive method and is probably misleading. Mortality is not the best indicator to measure the progress of health facilities in treating those with the disease.
Proportional Mortality is just a part of output indictors. Other output indicators that should be used are the relative survival rate after diagnosis [45], and disability-adjusted life expectancy. Evaluation of health services should also include other aspects of evaluation as structure indicators, and process indicators.
The country is ranked relatively well regarding the infant mortality rate of 24 per thousand in 1995 [11]. This allowed wrong inference as this infant mortality rate was already lower than the international goal, of <60 per 1000 live newborn by the year 2000 [13]. However, a suitable target for Libya should have been 15 per 1000. The same can be said on other targets of health for all by 2000 where the targets and the objectives stated are neither at the level of the country's capacity nor at the level of its ambitions.
Evaluating physician competence is an essential component of quality assurance. It should include areas of responsibility, level of responsibility, and means used for assessment [46]. Competence should include attributes, activities and accomplishments in addition to management of physical illness. But other aspects should also be included as cognitive, psychological and social needs that are expected and to be satisfied in the patient-physician relationship [46]. Apparatus of formal assessment is necessary to assure fairness, predictability, stability and legitimacy. Assessment of in-service physician competence does not really exist. Before employment of HR, mainly an administrative assessment is usually made. It is based mostly on unverified impressions, using private criteria, and is fitfully and selectively applied. Nothing is more destructive to morale than these modes of evaluation [46].
Improving the Situation
With increasing expectation of the society, and the continuous need to curb the cost of services, actions are needed inside and outside the health sector to put it back on track.
As stated earlier, there is no simple stereotyped formula for the organization of health services. We should see methodology as dynamic and evolving, and can learn from others on an ongoing basis. The health system should rely on newer approaches of management as management-by-objectives and risk-management approaches rather than the prevailing crisis -management attitude.
SMART objectives should be established. Administrative actions should be projected to accomplish the purpose of the proposed programs. Health financing systems as third party payment schemes are needed. Inefficient use of budgets allocated to health services should be prevented by tools like performance management and clinical governance. Decision-making, management, monitoring and evaluation should be open and with the participation of the largest number possible from professionals and consumers.
Conflicts of interest from health personnel and workers in or outside the field are an important issue. It should be controlled by more transparency in the sector. Recognized shortcomings must be addressed and not just ignored.
The public should be well informed to be able to make conscious judgments and decisions. Suitable legislations should be introduced including those to ensure coordination between different sectors. Data processed to information and intelligence are needed to deal with changing disease patterns and to encourage policies that could manage with the complex feedback system of health. Health promotion or adoption of healthy life styles programs is needed.
Risk to national health services as medical tourism or bioterrorism should be assessed by risk management approach and by improving competitiveness and quality of ambulatory and hospital services. As the Ejdabia outbreak crisis teaches us, there is a need to build a national approach for the establishment of linkages between the water supply, sanitation and waste management activities, disease control programs, vector control, food safety, and child health programs, in addition to cooperation with other sectors as industry, economy, and agriculture.
More appropriate allocation of health funds for HR development is important. Competent workforce should be given the opportunity to receive lifetime appropriate adequate training. Training and reward systems for healthcare personnel including paramedical and auxiliary personnel are essential. External continuous evaluation using appropriate indicators is vital. e-health solutions such as telemedicine are needed to overcome the scattering of the population over the vast geographical area and to maximize the utility of available HR [32].
Stewardship and credibility of LNHS should not be lost by taken actions (or non-actions) as what occurred with precipitated privatization, the 1995 hospital fees that were imposed by some hospitals, or the unnecessary delays in announcing the 1995 cholera or 1998 HIV outbreaks.
Turning these concepts into reality requires the drawing together of many strands of professional endeavor and managerial commitment into a cohesive program of action in each healthcare field or organization [25]. Changing is not easy, and spontaneous adoption is often slow even when solutions are known. One would find it hard to believe that it took 193 years for lemon juice to become integrated into British sailors’ diet after its effect was known. Even in this era of media publicity, spontaneous adoption of a simple health practice may take more than 20 years [26].
Conclusions
LNHS have a low performance inspite of apparent public health well-being. Most of the improvement that occurred in the last decades is due to public actions including those outside the health sector, such as education and increasing purchasing power. Further improvement will be difficult without proper planning that should be based on performance management and management by objectives rather than the prevailing crisis management.
Acknowledgements
The authors would like to thank Dr Muftah Twilib and Dr Omar Abusnaina for their critiques of the manuscript.
References
- 1.Murray CJ, Frenk J. A framework for assessing the performance of health systems. Bull World Health Organ. 2000;78:717–731. [PMC free article] [PubMed] [Google Scholar]
- 2.Goodman NW. Please give us objectives we can aim at. J R Soc Med. 2002;95:567. doi: 10.1258/jrsm.95.11.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kawabata K. A new look at health systems. Bull World Health Organ. 2000;78:716. [Google Scholar]
- 4.Bar-Yam Y. Improving the effectiveness of health care and public health: a multiscale complex systems analysis. Am J Public Health. 2006;96:459–466. doi: 10.2105/AJPH.2005.064444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diallo K, Zurn P, Gupta N, Dal Poz M. Monitoring and evaluation of human resources for health: an international perspective. Hum Resour Health. 2003;1:3. doi: 10.1186/1478-4491-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ. 2000;320:50–52. doi: 10.1136/bmj.320.7226.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National corpus for information and documentation. Tripoli, Libya: 2003. Statistics Book 2003. [Google Scholar]
- 8.Sert, Libya: General Popular Committee for Health and Environnement; 2005. Annual Statistical Report 2004. [Google Scholar]
- 9.The Libyan National Committee for Education, Culture and Science. The International Conference on Education «Quality Education for all Young People: Challenges, trends and priorities». Geneva; Switzerland: 2004. The Development Of Education In Great Jamahiriya. [Google Scholar]
- 10.Lakhani A, Coles J, Eayres D, Spence C, Sanderson C. Creative use of existing clinical and health outcomes data to assess NHS performance in England: part 2--more challenging aspects of monitoring. BMJ. 2005;330:1486–1492. doi: 10.1136/bmj.330.7506.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The General People's Committee for Health and Social affairs. The Libyan Arab Maternal and child Health Survey. Libya: Sert; 1996. [Google Scholar]
- 12.World Health Organization. Core Health Indicators. available at http://www3.who.Int/whosis last accessed December 2007.
- 13.Singh R, Abudejaja A, Sudani O. Health Services; Current Achievements and Future Challenges. JMJ. 2005;4:157–166. [Google Scholar]
- 14.Beaglehole R, Dal Poz MR. Public health workforce: challenges and policy issues. Hum Resour Health. 2003;1:4. doi: 10.1186/1478-4491-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El Taguri A. Medical Tourism and the Libyan National Health Services. Libyan J Med. 2007 doi: 10.4176/070530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ham C. Improving NHS performance: human behaviour and health policy. BMJ. 1999;319:1490–1492. doi: 10.1136/bmj.319.7223.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ham C. From targets to standards: but not just yet. BMJ. 2005;330(7483):106–107. doi: 10.1136/bmj.330.7483.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Declaration of Alma-Ata. WHO Chron. 1978;32:428–430. [PubMed] [Google Scholar]
- 19.El Taguri A AGH, Al Mgasbi K. Causes of Death among children in Benghazi during 1995; Third Jamahiriya Conference of Medical Sciences; Tripoli, Libya: 1996. [Google Scholar]
- 20.Mays GP, McHugh MC, Shim K, Perry N, Lenaway D, Halverson PK, Moonesinghe R. Institutional and economic determinants of public health system performance. Am J Public Health. 2006;96:523–531. doi: 10.2105/AJPH.2005.064253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saltman RB, Ferroussier-Davis O. The concept of stewardship in health policy. Bull World Health Organ. 2000;78:732–739. [PMC free article] [PubMed] [Google Scholar]
- 22.McPake B, Mills A. What can we learn from international comparisons of health systems and health system reform? Bull World Health Organ. 2000;78:811–820. [PMC free article] [PubMed] [Google Scholar]
- 23.Musgrove P. Health insurance: the influence of the Beveridge Report. Bull World Health Organ. 2000;78:845–846. [PMC free article] [PubMed] [Google Scholar]
- 24.Feachem RG. Health systems: more evidence, more debate. Bull World Health Organ. 2000;78:715. [PMC free article] [PubMed] [Google Scholar]
- 25.Scally G, Donaldson LJ. The NHS's 50 anniversary. Clinical governance and the drive for quality improvement in the new NHS in England. BMJ. 1998;317:61–65. doi: 10.1136/bmj.317.7150.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bahamon C, Dwyer J, Buxbaum A. Leading a change process to improve health service delivery. Bull World Health Organ. 2006;84:658–661. doi: 10.2471/blt.05.0287872. discussion 662–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freeman T, Walshe K. Achieving progress through clinical governance? A national study of health care managers’ perceptions in the NHS in England. Qual Saf Health Care. 2004;13:335–343. doi: 10.1136/qshc.2002.005108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bodenheimer T. Primary care--will it survive? N Engl J Med. 2006;355:861–864. doi: 10.1056/NEJMp068155. [DOI] [PubMed] [Google Scholar]
- 29.Woo B. Primary care--the best job in medicine? N Engl J Med. 2006;355:864–866. doi: 10.1056/NEJMp068154. [DOI] [PubMed] [Google Scholar]
- 30.Park K. Park's Textbook of Preventive and Social Medicine. 14th ed. Jabalpur (India): M/s Banarsidas Bhanot Publishers; 1995. [Google Scholar]
- 31.Bakoush O, Elgzyri T. Do we have a diabetes epidemic in Libya? Libyan J Med. 2006;1 doi: 10.4176/061016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El Taguri A. The need to introduce Telemedicine in Libya; First Libyan conference on medical specialties: 1997; Benghazi: 1997. [Google Scholar]
- 33.Mounir Khalil, Ray Jones. Electronic Health Services; An Introduction to Theory and Application. Libyan J Med. 2007;2(4) doi: 10.4176/071117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giaedi T. The Impact of Electronic Medical records on improvement of health care delivery. Libyan J Med. 2007 doi: 10.4176/071118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El Taguri A, Rolland-Cachera MF, Mahmud Salaheddin M, Elmrzougi N, Abdel Monem A, Betilmal I, Lenoir G. Nutritional status of under-five children in Libya: a national population-based survey. Libyan J Med. 2007 doi: 10.4176/071006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aaron H. Health Policy Issues & Options, Policy Brief # 147. 2005. Health Care Rationing: What it Means. [Google Scholar]
- 37.Beveridge W. Social insurance and allied services. 1942. Bull World Health Organ. 2000;78:847–855. [PMC free article] [PubMed] [Google Scholar]
- 38.Leatherman S, Sutherland K. Quality of care in the NHS of England. BMJ. 2004;328:E288–290. doi: 10.1136/bmj.328.7445.E288. [DOI] [PubMed] [Google Scholar]
- 39.Wyss K. An approach to classifying human resources constraints to attaining health-related Millennium Development Goals. Hum Resour Health. 2004;2:11. doi: 10.1186/1478-4491-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Health InterNetwork Access to Research Initiative (HINARI) project, World Health Organization. 2007. available at http://www.who.int/hinari/en/ last accessed September.
- 41.Wensing M. Evidence-based patient empowerment. Qual Health Care. 2000;9:200–201. doi: 10.1136/qhc.9.4.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thomson R. Quality to the fore in health policy--at last. But the NHS mustn't encourage quality improvement with punitive approaches. BMJ. 1998;317:95–96. doi: 10.1136/bmj.317.7151.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilcock PM, Thomson RG. Modern measurement for a modern health service. Qual Health Care. 2000;9:199–200. doi: 10.1136/qhc.9.4.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Arah OA, Klazinga NS, Delnoij DM, ten Asbroek AH, Custers T. Conceptual frameworks for health systems performance: a quest for effectiveness, quality, and improvement. Int J Qual Health Care. 2003;15:377–398. doi: 10.1093/intqhc/mzg049. [DOI] [PubMed] [Google Scholar]
- 45.Lakhani A, Coles J, Eayres D, Spence C, Rachet B. Creative use of existing clinical and health outcomes data to assess NHS performance in England: Part 1--performance indicators closely linked to clinical care. BMJ. 2005;330:1426–1431. doi: 10.1136/bmj.330.7505.1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Donabedian A. Evaluating physician competence. Bull World Health Organ. 2000;78:857–860. [PMC free article] [PubMed] [Google Scholar]