Abstract
Aim
To describe the nutritional status of children under-five years of age in Libya.
Population and methods
A secondary analysis of data of 5348 children taken from a national representative, two-stage, cluster-sample survey that was performed in 1995. Results: Prevalence rates of underweight, wasting, stunting, and overweight were determined using standard definitions in reference to newly established WHO growth charts. The study revealed that 4.3% of children were underweight, 3.7% wasted, 20.7% stunted, and 16.2% overweight. Seventy percent of children had normal weight. Undernutrition was more likely to be found in males, in rural areas, and in underprivileged groups. Overweight was more likely found in urban, privileged groups. Wasting was more common in arid regions; stunting was more common in mountainous regions of Al-Akhdar, Al-Gharbi, and in Sirt. Al-Akhdar had the highest prevalence of overweight.
Conclusion
The country had a low prevalence of underweight and wasting, moderate prevalence of stunting, and high prevalence of overweight. The country is in the early stages of transition with evidence of dual-burden in some regions. Similar surveys are needed to verify secular trends of these nutritional problems, particularly overweight.
Keywords: Libya, preschool children, nutritional status, underweight, wasting, stunting, overweight
Introduction
Malnutrition is one of the leading causes of disease [1]. Globally, undernutrition is an underlying or associated cause in at least half of all childhood deaths [2, 3]. This makes prevention of undernutrition in children one of the top priorities in efforts to reduce childhood mortality [4]. The effects of malnutrition on children are not limited to physical health, but extend to mental, social and spiritual wellbeing. They could be transmitted from one generation to another, constituting a vicious spiral [5].
Contrary to common use, the term malnutrition refers not only to deficiency states, but also to excess or imbalance in the intake of calories, proteins and/or other nutrients [6]. Developing nations are not exempt from the upward secular trend in the pandemic of obesity. Obesity is now considered by WHO as the biggest unrecognized public health problem [7]. The prevalence of obesity in some developing countries has reached even higher levels than in many industrialized nations [8].
Stunting can coexist with underweight or with overweight/obesity [9]. The WHO recommends that developing countries monitor the co-existence of stunting and overweight in children, because these are risk factors for chronic disease in adulthood [5, 10]. Management of many chronic diseases that may develop due to the increased incidence of obesity would be beyond the capacity of many nations [11].
It is equally important to identify the coexistence of both undernutrition and overnutrition, as an intervention that is designed to prevent only one problem could exacerbate the other. For example, combating undernutrition could exacerbate overnutrition and displace the whole population curve to the right, generating a significant proportion of overweight and obese children [9, 12].
The newly published growth charts from the WHO Multiple Centre Growth Reference Study, which includes children from diverse countries, is unique in that it documents children's growth under optimal conditions, rather than merely describing growth at a particular time or place. This establishes a standard rather than just a reference population [13].
Although some small “regional” surveys have been performed in Libya [14–16], there is no nationally representative peer-reviewed data on nutritional status of preschool children. In addition, overweight and/or obesity have not been specifically examined. The Libyan maternal and child health survey (LMCHS), undertaken as part of the Pan Arab project for child development (PAPChild), is the first and only national representative survey of its type ever done in Libya [17, 18]. The main report of LMCHS contains data on the prevalence of underweight and stunting; however, the data and its analysis are limited. We carried out a secondary analysis to give a clearer picture of the nutritional status of preschool children.
Population & methods
Design: This is a stratified, two-stage, cross-sectional, nationally representative, probability-cluster sample survey. It was performed during the summer of 1995. The country was divided into seven regions, each subdivided into urban and rural areas. The regions were as follows (maps are available on request):
two mountainous areas, Al-Djabal Al-Akhdar (Al-Akhdar) in the northeastern part, and Al-Djabal Al-Gharbi (Al-Gharbi) in the northwestern part;
two large and mainly desert areas with low population density: Khalij-Sirt (Sirt) and Sabha regions;
three coastal regions, (a) Sahel Benghazi (Benghazi), a narrow coastal strip southwest of the eastern Al-Akhdar Mountains, (b) Tripoli region, the most densely populated region in Libya, which contains the capital and two of the five major cities, and (c) Al-Zawia region, a littoral area west of Tripoli.
In the first stage, 307 sampling units were selected from the seven regions. Each sampling unit was then divided into five segments of equal size, of which one was randomly selected. All households in the selected segment were included in the sample, and all children aged <60 months were recruited in the study.
Outcome measures
Weight, height, and age data were used to calculate z-scores of the four different nutritional indicators in comparison to the newly published WHO growth curve. These indicators were underweight defined as weight-for-age (W/A) z-score <−2, wasting defined as weight-for-height (W/H) z-score <−2, stunting defined as height-for-age (H/A) z-score <−2, and overweight defined as body mass index (W/H2) for age (BMI/A) z-score >2.
Socioeconomic classification was based on a combination of asset index of households with its area characteristics, and a locally validated socioeconomic classification that incorporates parental occupation and education [15]. Independent variables were age, gender, socioeconomic status, geographical region and urban/rural residence.
Statistical analysis
Data were analyzed using WHO anthro 2005 software (WHO, Geneva, Switzerland), and SPSS version 13 (SPSS Inc., Chicago, Illinois, USA). The WHO anthro 2005 program considers z-score values for W/H and BMI/A of <−5 as outliers, whereas for H/A and W/A, it considers z-score values <−6 as outliers. A geographical display was made using Epi Map 2 of Epi InfoTM (CDC, Atlanta, USA). When appropriate, statistical assessment was made by comparing mean and 95% confidence intervals (CI95%). Level of significance was set at P<0.05.
Results
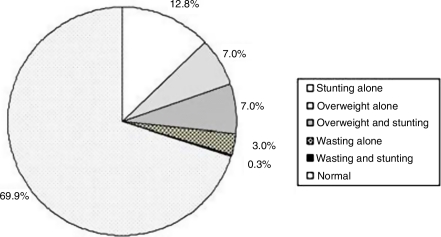
A total of 5348 children were recruited from 6707 households. Characteristics of these children are shown in Table 1. Anthropometric measures were available for 83.6% (W/H) to 87.8% (W/A) of the children. Of these children, 202 (4.3%) were underweight, 163 (3.7%) were wasted, 929 (20.7%) were stunted, and 724 (16.2%) were overweight. Wasting alone affected 3% of children, while stunting alone affected 12.8%. Prevalence rates of overweight alone and overweight associated with stunting were both 7% (Figure 1).
Table 1.
Basic attributes of children participating in the study.
| Variable | Frequency (%) |
|---|---|
| Socio-economic classification | |
| Advantaged | 1879 (35.1) |
| Intermediate | 1833 (34.3) |
| Disadvantaged | 1635 (30.6) |
| Gender | |
| Boy | 2702 (50.5) |
| Girls | 2646 (49.5) |
| Section | |
| Urban | 3756 (70.2) |
| Rural | 1591 (29.8) |
| Region | |
| Tripoli & Khoms | 1769 (33.1) |
| Sert Golf | 845 (15.8) |
| Benghazi | 663 (12.4) |
| Al-Djabal Al-Akhdar | 645 (12.1) |
| Al-Zaouia | 558 (10.4) |
| Al-Djabal Al-Gharbi | 525 (9.8) |
| Sabha | 343 (6.4) |
| Age (months) | |
| 0–<6 | 420 (7.9) |
| 6–<12 | 563 (10.5) |
| 12–<18 | 492 (9.2) |
| 18–<24 | 579 (10.8) |
| 24–<30 | 554 (10.4) |
| 30–<36 | 605 (11.3) |
| 36–<42 | 562 (10.5) |
| 42–<48 | 582 (10.9) |
| 48–<54 | 525 (9.8) |
| 54–<60 | 466 (8.7) |
Figure 1.
Proportional distribution of single and combined forms of malnutrition among under-five children in Libya in 1995.
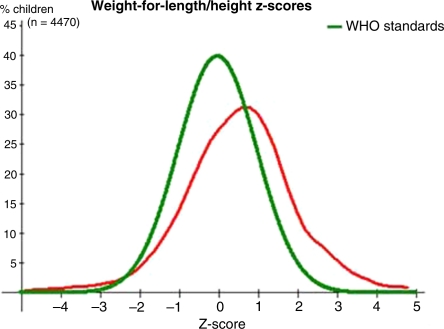
The mean and standard deviation (SD) of the z-scores was −0.07±1.12 for W/A, 0.58±1.42 for W/H, −0.90±1.48 for H/A, and 0.65±1.53 for BMI/A (Figures. 2 a–d). Equivalent curves comparing boys to girls were similar to those of the whole population; no gender differences were found. Examination of mean z-score and CI95% for all these indicators for boys versus girls, even within different subgroups (regional, urban/rural, and socioeconomic status), also showed no statistically significant differences between sexes.
Figure 2a.
Comparison of the distribution of z-score for weight-for-age of Libyan under-five children to WHO child growth standards.
Figure 2d.
Comparison of the distribution of z-score of BMI-for-age of Libyan under-five children to WHO child growth standards.
Figure 2b.
Comparison of the distribution of z-score for weight-for-length of Libyan under-five children to WHO child growth standards.
Figure 2c.
Comparison of the distribution of z-score of height-for-age of Libyan under-five children to WHO child growth standards.
Rural areas had lower mean H/A z-scores than urban areas (−1.01 versus −0.83). The more underprivileged groups had lower H/A z-scores than privileged groups (−1.04 versus −0.72). Mean z-score and CI95% for H/A showed statistically significant differences between regions. The two mountain regions had the lowest H/A z-scores (Figure 3a).
Figure 3a.
Mean and 95% Confidence Interval (95% CI) of height for age (H/A) z-scores in different regions.
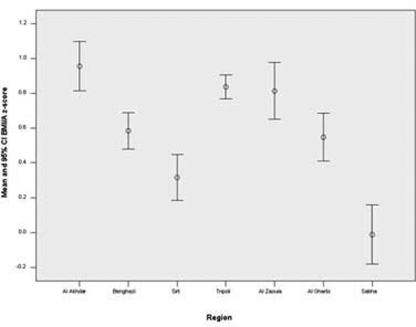
All regions had positive BMI/A z-score values, especially Al-Akhdar region, with the exception of the arid Sabha region, which had a score of about zero (Figure 3b).
Figure 3b.
Mean and 95% Confidence Interval (95% CI) of body mass index for age (BMI/A) z-scores in different regions.
The prevalence of malnutritional problems was higher in boys, in rural areas, and in underprivileged groups. The only exception was overweight, which was more common in urban areas and in privileged groups (Table 2). The higher prevalence of overweight in urban and in privileged groups was even more prominent when overweight alone was considered (data not shown).
Table 2.
Prevalence rates of nutritional indicators according to basic demographic attributes
| Category | Number of cases (Prevalence rates%) | |||
|---|---|---|---|---|
| Underweight | Wasting | Stunting | Overweight | |
| Socio-economic Class | ||||
| Advantaged Intermediate | 63 (3.9) | 56 (3.6) | 283 (18.4) | 273 (17.7) |
| Disadvantaged | 57 (3.6) | 45 (3.0) | 320 (20.8) | 239 (15.6) |
| 82 (5.6) | 62 (4.4) | 325 (23.0) | 212 (15.0) | |
| Gender | ||||
| Boys | 111 (4.7) | 86 (3.9) | 495 (22.2) | 389 (17.5) |
| Girls | 91 (3.9) | 77 (3.4) | 434 (19.1) | 335 (14.8) |
| Area | ||||
| Urban | 133 (4.1) | 102 (3.3) | 613 (19.6) | 502 (16.2) |
| Rural | 69 (4.9) | 60 (4.4) | 316 (23.2) | 221 (16.1) |
| Geographical region | ||||
| Al-Akhdar | 24 (4.0) | 15 (2.7) | 154 (27.9) | 128 (23.1) |
| Benghazi | 22 (3.6) | 18 (3.0) | 89 (14.7) | 67 (11.2) |
| Sirt gulf | 37 (5.7) | 43 (6.8) | 157 (24.9) | 80 (12.8) |
| Tripoli & Khoms | 52 (3.4) | 32 (2.1) | 268 (17.7) | 272 (18.2) |
| Al-Zaouia | 22 (4.8) | 18 (4.3) | 86 (21.1) | 76 (18.6) |
| Al-Gharbi | 27 (5.3) | 19 (3.9) | 122 (24.9) | 74 (15.1) |
| Sabha | 19 (6.0) | 19 (6.4) | 52 (17.3) | 26 (8.7) |
The prevalence of these malnutritional problems varied with geographic area (Table 2). Underweight was more common in arid areas, such as Sirt and Sabha, and in mountain areas of Al-Akhdar and Al-Gharbi.
This was mainly due to a high prevalence of wasting in the arid areas and stunting in mountain areas. Interestingly, the mountainous areas also had high prevalence of overweight (Table 3).
Table 3.
Ranking of different geographical regions according to importance of different malnutrition problems. For undernutrition: ○ Low level, ○○ Intermediate level, ○○○ high level. For Overnutrition: ● Low level, ●●Intermediate level, ●●● High level.
| Level of the malnutritional problem | ||||
|---|---|---|---|---|
| Geographical region | Underweight | Wasting | Stunting | Overweight |
| Al-Akhdar | ○ | ○ | ○○○ | ●●● |
| Benghazi | ○ | ○ | ○ | ● |
| Sirt gulf | ○○ | ○○○ | ○○○ | ● |
| Tripoli & Khoms | ○ | ○ | ○○ | ●● |
| ○ | ○○ | ○○ | ●● | |
| Al-Zaouia | ○○ | ○○ | ○○○ | ●● |
| Al-Gharbi | ○○ | ○○○ | ○ | ● |
| Sabha | ○ | |||
| ○○ | ||||
| ○ | ||||
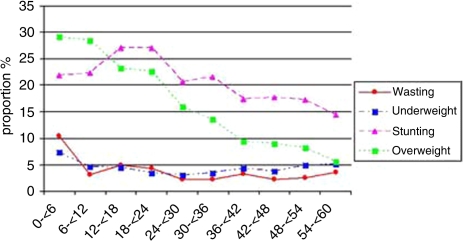
In the youngest children, overweight and stunting were the most common malnutritional problems (Figure 4). Overweight decreased by age, but stunting peaked in the second year of life and then decreased, though it continued to be an important malnutritional problem.
Figure 4.
Changes in the prevalence of main forms of malnutrition with age.
When mild stunting was added to the pool of stunted cases, the proportion of stunted children increased substantially. The prevalence of mild, moderate, and severe stunting was 25.9%, 13.2%, and 7.2%, respectively, with mild stunting accounting for more than half of all stunting. The contribution of mild cases increased with age, while that of moderate cases remained fairly constant and severe cases decreased almost to half by five years of age (Figure 5).
Figure 5.
Prevalence rates of different degrees of stunting according to age.
In early infancy, the prevalence of stunting was higher among boys, but by the end of five years of age, the prevalence became higher in girls (Figure 6). Although prevalence rates were higher in rural areas, the contribution from urban areas and larger cities, such as Tripoli, to the overall pool of malnutrition was quantitatively more important. As an example, in spite of increased prevalence of stunting in rural areas, 60.5% of stunted children lived in urban areas. These urban areas also contained 63.6% of overweight children.
Figure 6.
Gender differences in prevalence rates of stunting by age.
Discussion
Knowing the prevalence rates of underweight, wasting, and stunting is important for determining the overall health of the community and for monitoring achievements toward mid-decade goals for nutrition and child health set by international organizations [19, 20]. Based on the main report of the LMCHS, which used the NCHS/WHO reference population (according to WHO criteria), Libya was considered as a low prevalence area for underweight, wasting, and stunting. Currently, using the newly published WHO standards, we found that 70% of children had normal weight, 4.3% were underweight, 3.7% were wasted, 20.7% were stunted, and 16.2% were overweight. The 20.7% prevalence rate of stunting classifies the country as a moderate prevalence area rather than a low prevalence area. When the data was collected in 1995, almost half of the children in the disadvantaged parts of the world were underweight and/or moderately or severely stunted [2, 5, 21]. In the same year, the average prevalence of overweight children in the developing countries, as revealed by weight for hight in reference to NCHS/WHO standards was 3.3% (0.1%–14.4%) [22].
In developing countries and marginalized groups in affluent societies, undernutrition is increasing as a result of the debt crisis and consequent economic adjustment policies [9]. On the other hand, the rapid growth of some economies and changes in lifestyles, including diet and physical activity patterns, contribute to other malnutritional problems at the other end of the spectrum [9]. In fact, obesity is no longer considered a disease of industrialized nations only. Libya is a middle-income country, and improving the nutritional status and reducing health inequalities were at the centre of the government health policy during the seventies. Efforts were made to secure food for all populations by short and intermediate term measures, such as food subsidy programs and free distribution of breast milk substitutes to mothers., One of the important aspects of this survey, besides being the first of its kind, is that it was performed during the peak of political and economic difficulties that faced the country in the 1990s due to UN sanctions.
In contrast to many African and Asian countries where rates of wasting were reported, in 2000, to be 2.5–3.5 times higher than rates of overweight [22], from the current study, both stunting and overweight are important public health nutritional problems in Libya, In the Libyan population as a whole, both W/H and BMI/A z-score curves were shifted to the right, the W/A z-score curve was about zero, and the H/A z-score curve was shifted to the left. Low prevalence of undernutrition and high prevalence of overweight in children indicates a population-wide shift and nutritional transition. The wide difference in the prevalence rates of wasting and stunting in Libya indicates an early phase of transition [23]. The most disadvantaged countries usually have higher prevalence rates of both wasting and stunting. In middle income countries, acute forms start to decrease first, whereas the most advantaged countries show lower prevalence rates of both acute and chronic forms [24, 25].
Stunting (low H/A) is a public health problem worldwide. It is a measure of cumulative deficient growth and a feature of a complex syndrome including developmental delay, impaired immune function, reduced cognitive development, metabolic disturbance leading to accumulation of body fat, loss of lean mass, and risk of hypertension [3, 26]. Several nutritional deficiencies occur simultaneously in stunted children and all may be responsible for stunting [27], but these were not studied in the current survey. Though mild forms of stunting have a lower risk of death than moderate/severe undernutrition [28], we included mild stunting in our analysis because of its impact on mild and moderate undernutrition, and on the overall disease burden at the community level [29, 30].
Disaggregated data in this analysis showed that the prevalence rates of indicators of undernutrition were higher among boys, in underprivileged groups of the population, and in rural areas. Equity is one of the four basic principles of primary health care as declared in the Alma Ata declaration [32]. Beside socioeconomic classes, an important dimension of equity is gender equity. An equal degree of undernutrition among boys and girls less than age of five by the year 2020 is accepted internationally as a mean for evaluating equity in different societies [19, 20]. As in previous regional studies in Libya, girls were at less risk of undernutrition. Similar observations in other African countries have shown that all forms of undernutrition were higher among boys [33]. However, disaggregated data showed that by age five, there were more stunted girls than boys. This was due to a decrease in the prevalence of stunting among older boys rather than an increase among girls (Figure 6).
As seen in the current analysis, the second year of life is a critical period for undernutrition, because the child is dependent on someone for nutritional intake, complimentary foods are introduced, and the child is exposed to food-borne pathogens [35, 36]. As shown in the current study, stunting is known to decrease by age four to five. This seems to be true for moderate and severe stunting, but not for mild stunting. Other studies have shown increased stunting with age [37–39]. This could signify that while the detrimental environmental effects diminish with age, they do not completely disappear. The high prevalence of mild stunting would still be considered even if the accepted theoretical ≈13% of cases from the normal distribution curve were excluded.
An important finding from the disaggregated data was the variable geographical distribution, especially the high incidence of both stunting and overweight in mountainous regions and wasting in arid areas, and low prevalence of stunting in the arid area of Sabha. These regional differences could be related to climate, altitude, dietary habits, ethnic origins, or sociocultural factors [37, 40]. Inhabitants in the more arid areas of Sabha and Sirt traditionally have diets that consist primarily of food of animal origin, which could explain their low rates of stunting. Inhabitants of both mountainous areas rely heavily on cereals. People in the eastern parts of the country consume considerable amounts of food of animal origin, while in western mountainous areas they consume a wide range of whole grain cereals and dried fruits. Further studies are needed to verify possible regional differences.
In this analysis, the highest dual burden (stunting combined with overweight) at the individual level was seen in Al-Akhdar Mountains. Combined overweight and stunting is more likely to be associated with central obesity and its metabolic effects. Regionally, the highest dual burden was seen in Al-Zaouia, Al-Gharbi and Al-Akhdar regions. It is in these regions that interventions designed for one form of malnutrition might exacerbate another. We found that the proportion of stunting among overweight children was quite high in comparison to data from other transitional countries [41].
The reported undernutrition indicators from previous regional studies were comparable to our data [14–16]. Overweight was reported in only one of these studies [16], but that study was not representative as only two regions were included (3% in Al-Gharbi and 7% in Tripoli). The definition used for overweight was not the same (W/H z-score rather than BMI/A z-score).
The proportional contribution of each category to the burden of these problems is different from the prevalence of each malnutrition factor. Most cases of malnutrition were among urban dwellers. This has implications in service delivery planning. In many countries the nutritional status of lower socioeconomic children is worse among all urban groups and poorer than the rural average [21]. Slums have not existed in Libya since the late 1970s, but urban areas remain unequal in living conditions. The relative division in urban areas living conditions was not incorporated in this study. An equity-motivated policy during the 1970s had driven the authorities in Libya to expand services horizontally, with the advantage to rural areas. It may be time to reconsider horizontal equity in urban regions similar to vertical equity in rural areas. There was a low prevalence of underweight and wasting, moderate levels of stunting, and high levels of overweight. Although this makes the nutritional status of preschool children in Libya better than that in many developing countries, there is room for much improvement. A particular finding was the pattern of obesity together with stunting, more common in certain regions. It is important to monitor nutritional status over time to assess the effects of major socioeconomic changes in the country, and to evaluate micronutrient status of our population. The consequence of failing to do so will likely produce negative outcomes.
References
- 1.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 2.de Onis M, Blossner M, Borghi E, Frongillo EA, Morris R. Estimates of global prevalence of childhood underweight in 1990 and 2015. Jama. 2004;291:2600–6. doi: 10.1001/jama.291.21.2600. [DOI] [PubMed] [Google Scholar]
- 3.Branca F, Ferrari M. Impact of micronutrient deficiencies on growth: the stunting syndrome. Ann Nutr Metab. 2002;46(Suppl 1):8–17. doi: 10.1159/000066397. [DOI] [PubMed] [Google Scholar]
- 4.Caulfield LE, de Onis M, Blossner M, Black RE. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am J Clin Nutr. 2004;80:193–8. doi: 10.1093/ajcn/80.1.193. [DOI] [PubMed] [Google Scholar]
- 5.Gillespie S, Mason J, Martorell R. State of the Art series. Geneva: United Nations Administrative Committee on Coordination-Subcommittee on Nutrition (ACC/SCN):; 1993. How Nutrition Improves. [Google Scholar]
- 6.Child Growth Standards. World Health Organization. 2006. http://who.int/childgrowth.
- 7.James PT, Leach R, Kalamara E, Shayeghi M. The worldwide obesity epidemic. Obes Res. 2001;9(Suppl 4):228S–233S. doi: 10.1038/oby.2001.123. [DOI] [PubMed] [Google Scholar]
- 8.Obesity. Report No.: 894. 2000. Preventing and Managing the Global Epidemic: World Health Organization. [PubMed] [Google Scholar]
- 9.Doak CM, Adair LS, Bentley M, Monteiro C, Popkin BM. The dual burden household and the nutrition transition paradox. Int J Obes (Lond) 2005;29:129–36. doi: 10.1038/sj.ijo.0802824. [DOI] [PubMed] [Google Scholar]
- 10.Geneva: WHO; 2002. World Health Organization. The World Health Report: Reducing Risk, Promoting Healthy Life. [Google Scholar]
- 11.Moore TR. Adolescent and adult obesity in women: a tidal wave just beginning. Clin Obstet Gynecol. 2004;47:884–9. doi: 10.1097/01.grf.0000135667.23543.4b. discussion 980–1. [DOI] [PubMed] [Google Scholar]
- 12.Uauy R, Kain J. The epidemiological transition: need to incorporate obesity prevention into nutrition programmes. Public Health Nutr. 2002;5:223–9. doi: 10.1079/PHN2001297. [DOI] [PubMed] [Google Scholar]
- 13.MGRS. Enrolment and baseline characteristics in the WHO Multicentre Growth Reference Study. Acta Paediatr Suppl. 2006;450:7–15. doi: 10.1111/j.1651-2227.2006.tb02371.x. [DOI] [PubMed] [Google Scholar]
- 14.Budejaja A SR, Amanullah Khan, Gupta BS. Anthropometric measurements in children up to five years of age in Bouhadema area, Benghazi. Garyounis Med J. 1980;3:163–73. [Google Scholar]
- 15.EL-Tajouri RF. Cross sectional study of growth in urban pre-school children in Libya [Ph.D. Dissertation] University of Zurich; 1979. [Google Scholar]
- 16.Hameida J, Billot L, Deschamps JP. Growth of preschool children in the Libyan Arab Jamahiriya: regional and sociodemographic differences. East Mediterr Health J. 2002;8:458–69. [PubMed] [Google Scholar]
- 17.Arab Maternal and Child Health Survey. League of Arab States; The Pan Arab Project for Child Development (PAPChild); League of Arab States; 2007. Aug 28, Last accessed. [Google Scholar]
- 18.The Arab Libyan Maternal and Child Health Survey. League of Arab States-The Pan Arab Project for Child Development: Principle Report: The General People's Committee for Health and Social Affaires; 1996. [Google Scholar]
- 19.Bloss E, Wainaina F, Bailey RC. Prevalence and predictors of underweight, stunting and wasting among children aged five and under in western Kenya. J Trop Pediatr. 2004;50:260–70. doi: 10.1093/tropej/50.5.260. [DOI] [PubMed] [Google Scholar]
- 20.Measuring Progress towards the Health Millennium Development Goals. World Health Organization; 2006. [Google Scholar]
- 21.Ghosh S, Shah D. Nutritional problems in urban slum children. Indian Pediatr. 2004;41:682–96. [PubMed] [Google Scholar]
- 22.de Onis M, Blossner M. Prevalence and trends of overweight among preschool children in developing countries. Am J Clin Nutr. 2000;72:1032–9. doi: 10.1093/ajcn/72.4.1032. [DOI] [PubMed] [Google Scholar]
- 23.Martorell R TJH. Child Survival: Strategies for Research. Malnutrition, Morbidity and Mortality. Popul Dev Rev. 1984;10(Supp 84):49–68. [Google Scholar]
- 24.Mamabolo RL, Alberts M, Mbenyane GX, Steyn NP, Nthangeni NG, Delemarre-Van De Waal HA, et al. Feeding practices and growth of infants from birth to 12 months in the central region of the Limpopo Province of South Africa. Nutrition. 2004;20:327–33. doi: 10.1016/j.nut.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 25.Shgair H AA, Sharshoor S. Arab Congress for Maternal & Child Health. Vol. 1999. PAPChild-League of Arab States: 1999. Nutritional Status of Children in some Arab Countries. [Google Scholar]
- 26.Martins PA, Hoffman DJ, Fernandes MT, Nascimento CR, Roberts SB, Sesso R, et al. Stunted children gain less lean body mass and more fat mass than their non-stunted counterparts: a prospective study. Br J Nutr. 2004;92:819–25. doi: 10.1079/bjn20041274. [DOI] [PubMed] [Google Scholar]
- 27.Ibrahim SA, Abd el-Maksoud A, Nassar MF. Nutritional stunting in Egypt: which nutrient is responsible? East Mediterr Health J. 2002;8:272–80. [PubMed] [Google Scholar]
- 28.Schroeder DG, Brown KH. Nutritional status as a predictor of child survival: summarizing the association and quantifying its global impact. Bull World Health Organ. 1994;72:569–79. [PMC free article] [PubMed] [Google Scholar]
- 29.de Onis M, Garza C, Habicht JP. Time for a new growth reference. Pediatrics. 1997;100:E8. doi: 10.1542/peds.100.5.e8. [DOI] [PubMed] [Google Scholar]
- 30.Pelletier DL. The potentiating effects of malnutrition on child mortality: epidemiologic evidence and policy implications. Nutr Rev. 1994;52:409–15. doi: 10.1111/j.1753-4887.1994.tb01376.x. [DOI] [PubMed] [Google Scholar]
- 31.Armstrong J, Dorosty AR, Reilly JJ, Emmett PM. Coexistence of social inequalities in undernutrition and obesity in preschool children: population based cross sectional study. Arch Dis Child. 2003;88:671–5. doi: 10.1136/adc.88.8.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Declaration of Alma-Ata; International Conference on Primary Health Care; Alma-Ata: USSR; 1978. [Google Scholar]
- 33.Wamani H, Astrom AN, Peterson S, Tumwine JK, Tylleskar T. Boys are more stunted than girls in sub-Saharan Africa: a meta-analysis of 16 demographic and health surveys. BMC Pediatr. 2007;7:17. doi: 10.1186/1471-2431-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caputo A, Foraita R, Klasen S, Pigeot I. Undernutrition in Benin-an analysis based on graphical models. Soc Sci Med. 2003;56:1677–91. doi: 10.1016/s0277-9536(02)00162-4. [DOI] [PubMed] [Google Scholar]
- 35.Neumann CG, Harrison GG. Onset and evolution of stunting in infants and children. Examples from the Human Nutrition Collaborative Research Support Program. Kenya and Egypt studies. Eur J Clin Nutr. 1994;48(Suppl 1):S90–102. [PubMed] [Google Scholar]
- 36.Frongillo EA., Jr. Symposium: Causes and Etiology of Stunting. Introduction. J Nutr. 1999;129(2S Suppl):529S–530. doi: 10.1093/jn/129.2.529S. [DOI] [PubMed] [Google Scholar]
- 37.Behrman JR, Skoufias E. Correlates and determinants of child anthropometrics in Latin America: background and overview of the symposium. Econ Hum Biol. 2004;2:335–51. doi: 10.1016/j.ehb.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 38.Khuwaja S, Selwyn BJ, Shah SM. Prevalence and correlates of stunting among primary school children in rural areas of southern Pakistan. J Trop Pediatr. 2005;51:72–7. doi: 10.1093/tropej/fmh067. [DOI] [PubMed] [Google Scholar]
- 39.El-Sayed N, Mohamed AG, Nofal L, Mahfouz A, Zeid HA. Malnutrition among pre-school children in Alexandria, Egypt. J Health Popul Nutr. 2001;19:275–80. [PubMed] [Google Scholar]
- 40.Dang S, Yan H, Yamamoto S. High altitude and early childhood growth retardation: new evidence from Tibet. Eur J Clin Nutr. 2007 Mar 7; doi: 10.1038/sj.ejcn.1602711. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 41.Jinabhai CC, Taylor M, Sullivan KR. Implications of the prevalence of stunting, overweight and obesity amongst South African primary school children: a possible nutritional transition? Eur J Clin Nutr. 2003;57:358–65. doi: 10.1038/sj.ejcn.1601534. [DOI] [PubMed] [Google Scholar]