Abstract
Stem cells provide an alternative curative intervention for the infarcted heart by compensating for the cardiomyocyte loss subsequent to myocardial injury. The presence of resident stem and progenitor cell populations in the heart, and nuclear reprogramming of somatic cells with genetic induction of pluripotency markers are the emerging new developments in stem cell-based regenerative medicine. However, until safety and feasibility of these cells are established by extensive experimentation in in vitro and in vivo experimental models, skeletal muscle-derived myoblasts, and bone marrow cells remain the most well-studied donor cell types for myocardial regeneration and repair. This article provides a critical review of skeletal myoblasts as donor cells for transplantation in the light of published experimental and clinical data, and indepth discussion of the advantages and disadvantages of skeletal myoblast-based therapeutic intervention for augmentation of myocardial function in the infarcted heart. Furthermore, strategies to overcome the problems of arrhythmogenicity and failure of the transplanted skeletal myoblasts to integrate with the host cardiomyocytes are discussed.
Keywords: heart, myoblast, myocardium, stem cell
Despite the advances in medical and surgical treatment of myocardial infarction, ischemic heart disease remains the leading cause of morbidity and mortality on a global scale [1]. The gravity of the problem can be assessed by the fact that mortality from ischemic heart disease exceeds the mortality from cancer – as the 1-year survival rate is lower than 50%. The immune and inflammatory responses following myocardial infarction are characterized by neutrophil and macrophage accumulation, cytokine secretion, recruitment of T and B cells, and formation of antibodies specific to myosin and actin [2]. The successive biochemical, structural and functional adaptive changes in the infarcted and hibernating myocardium lead to expansion of the infarction zone and scarring, while the hibernating myocardium in the periphery of the infarct become hypertrophic. The hearts of patients who survive the acute phase of myocardial infarction subsequently enter into a vicious cycle of left ventricular remodeling as part of the compensatory mechanism caused by the massive loss of functioning cardiomyocytes. Various therapeutic options including pharmacotherapeutic intervention (e.g., angiotensin-converting enzyme inhibitors, β-blockers, diuretics and angiotensin receptors blockers) are available but only provide a symptomatic relief without addressing the fundamental issue of myocyte loss. Device therapies, specific to heart failure, such as cardiac resynchronization therapy, implantable cardiac defibrillators and ventricular assist devices, are available [3,4]. Similarly, cardiac revascularization procedures, such as coronary angioplasty and coronary artery bypass grafting (CABG), only help to save the reversibly injured cells and restore contractility of the hibernating viable myocardium. Heart transplantation remains the only definitive treatment modality for end-stage heart failure, but the limited availability of donor hearts is a major limitation of this option. Therefore, the limitations of the currently available therapeutic approaches warrant for the development of principally new and efficient strategies for managing chronic heart disease and its related complications.
The regenerative ability of the heart
The heart has always been considered as a postmitotic organ owing to the limited ability of cardiomyocytes to proliferate during postnatal life. In response to injury and increased workload in pathological conditions, cardiomyocytes in the border zone of the injured myocardium become hypertrophic, rather than re-entering into the cell cycle to compensate for the loss of functioning cardiomyocytes. Therefore, loss of functioning cardiomyocytes in the ischemic myocardium is considered to be irreversible owing to the terminally differentiated status of cardiomyocytes, and the postinfarction repair mechanisms are insufficient after myocytes apoptosis [5]. Strategies to re-introduce cardiomyocytes – which constitute approximately 20% of the healthy human myocardium [6,7] – into the cell cycle have had little success [8]. The pioneering work of Anversa and colleagues has challenged the long-standing dogma regarding the terminally differentiated status of the heart, and successfully provided the evidence that the death and growth of cardiomyocytes in response to injury continuously occur in the heart [9,10]. More recent studies support this notion and demonstrate that the turnover of cardiomyocyte is less than 50% during the whole human life span – which is estimated to be 1% at 25 years of age and declines to 0.45% at 75 years of age [7]. Besides limited renewal, the existence of an independent pool of resident cardiac stem cells (CSCs) and cardiac progenitor cells (CPCs) has also been reported in the heart [11,12]. However, the identification of these cells remains an issue owing to the lack of specific surface markers, and cells are generally identified on the basis of cardiomyocyte-specific transcription factors, including NKx2.5, GATA4 and MEF2C, and lack of cardiomyocyte-specific structural protein expression. These resident CSCs/CPCs have the ability to differentiate into all the constituent cell lineages of the myocardium and, therefore, participate in the repair process in the event of myocardial injury [13]. A recent advancement in this regard is the identification of distinct lineages of CSCs/CPCs that may adopt vasculogenic and myogenic phenotypes [14,15]. These resident CSCs/CPCs can be activated to participate in myocardial repair processes [15]. Attempts have also been made to isolate, propagate in vitro and transplant CSCs/CPCs for myocardial repair with encouraging results [16,17]. Although CSCs/CPCs are considered an ideal source of cells for myocardial regeneration, these cells cannot intrinsically repopulate very large infarcts and, thus, warrant an outside therapeutic intervention to compensate for the inept intrinsic repair mechanism.
Stem & progenitor cell transplantation as a new treatment strategy
During nearly two decades of cell therapy research for treatment of ischemic heart disease, stem cell transplantation, either alone or in combination with the other therapeutic interventions, has demonstrated promise as a novel curative strategy [18]. The prime advantage of the heart cell therapy using stem/progenitor cells is its capability to replace the loss-of-functioning cardiomyocytes, attenuation of infarct-size expansion and preservation of the deteriorating left ventricular contractile function [19–22]. Subsequent to the exciting outcome of the first cell transplantation study in an experimental animal model, cells from various sources and with varying differentiation potential have been examined in experimental and clinical studies [17,23–27]. Of all the stem cells used, skeletal muscle-derived myoblasts have been investigated on the largest scale, both experimentally and clinically [28–32]. With the recent changes in the NIH policy regarding the use of embryonic stem cells, enthusiasm for their therapeutic application has increased. However, owing to the ethical considerations and practical limitations, it will take a long time to optimize conditions for their clinical application. The successful induction of pluripotency in somatic cells by nuclear reprogramming with stemness factors has allowed a continuous alternative source of pluripotent stem cells [33,34]. These induced pluripotent stem cells possess embryonic stem cell-like characteristics and are being studied for tumor-free cardio-myogenic differentiation potential [23,26,35,36]. We have successfully transformed mouse skeletal myoblasts into induced pluripotent stem cells and used these induced pluripotent stem cells for myocardial repair in a mouse model of acute myocardial infarction [Ahmed RPH, Haider KH et al., Unpublished Data].
Skeletal myoblasts and bone marrow-derived stem cells remain the most well-characterized and extensively studied therapy for myocardial reparability in the patients with ischemic heart disease [37–42]. There are many features that make skeletal myoblasts an attractive option for clinical applications (Box 1). Skeletal myoblasts constitute the renewable source of progenitor cells in skeletal muscle that participate in the repair process in the event of injury (Figure 1). The most important characteristics of skeletal myoblasts that make them suitable for use are their autologous availability, potential to expand in vitro, resistance to ischemia, low risk of tumorigenesis and myogenic differentiation potential [43,44]. More importantly, when in contact with cardiac myocytes in vitro, such myofibers can contract and form synchronous contractile elements.
Box 1. Characteristics of skeletal myoblasts.
Skeletal myoblasts are located between the basal lamina and sarcolemma and account for 2–5% of sub-laminar nuclei of mature skeletal muscle.
Skeletal myoblasts are activated in response to muscle damage or disease-induced muscle degeneration.
Skeletal myoblasts express desmin, CD56, Pax3, Pax7, c-met, myocyte nuclear factor, M-cadherin, VCAM1, N-CAM, CD34, Leu-19, and syndecan 3 and 4. Activated skeletal myoblasts first express Myf-5 and/or MyoD, and finally myogenin and MRF4 as the cells differentiate into multinucleated myotubes.
They possess high proliferative potential in vitro under appropriate culture conditions and maintain their undifferentiated status.
Skeletal myoblasts are highly resistant to ischemic stress.
Commitment to a well-differentiated myogenic lineage.
Transplantation of skeletal myoblasts has a low risk of tumorgenicity.
Autologous availability without ethical issues.
The use of autologous skeletal myoblasts alleviates the need for immunosuppression.
Figure 1. Phase contrast photomicrograph of a typical rat skeletal myoblast monolayer culture.
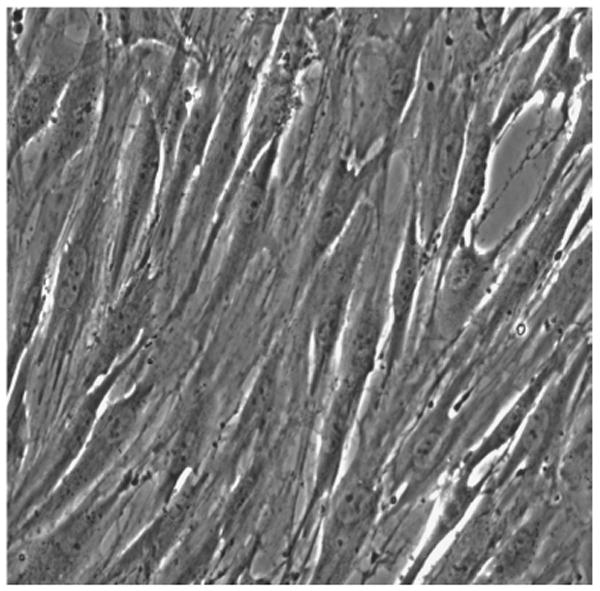
Original magnification: 20×.
Experimental animal studies using skeletal myoblasts for myocardial repair
Extensive and indepth experimental efforts from various research groups have assessed the performance of skeletal myoblasts for the treatment of both ischemic and nonischemic cardiomyopathies both in small mouse [32], rat [28,45], rabbit [46,47], large sheep [40,48], dog [49,50] and pig [22,51–53] models. These studies have demonstrated that skeletal myoblasts effectively prevented left ventricular remodeling and preserved global parameters (ejection fraction and left ventricular pressure) as well as regional parameters (regional stroke work at the infarct site, wall thickness and myocardial tissue velocities) of myocardial contractility. The diastolic properties also demonstrated improvement with increased compliance of the infarcted myocardium [47,54].
Since the pioneering work of Marelli et al., in a dog model of experimental myocardial cryoinjury, survival of the transplanted skeletal myoblasts and their myogenic differentiation postengraftment in the infarcted heart was extensively reported [55]. The transplanted skeletal myoblasts transmurally replace the scar tissue [56]. However, the ability of skeletal myoblasts to adopt cardiac phenotype remained controversial since they failed to electromechanically couple with the host myocytes [57,58]. These observations were further supported by a proof-of-concept study that involved transplantation of autologous skeletal myoblasts in a rabbit heart model of cryoinjury and demonstrated that the transplanted cells were only able to differentiate into mononuclear myocytes surrounded by the scar tissue without integration into the heart tissue [46]. The ability of skeletal myoblasts to limit adverse postinfarction remodeling caused by scaffolding effect and matrix metalloproteinase inhibition predominantly accounts for the functional benefits of skeletal myoblasts transplantation [43,54]. In addition, skeletal myoblasts have paracrine effects on the recipient cardiac tissue [59,60]. Such paracrine mechanisms lead to the preservation of matrix architecture in the remote and infarcted myocardium, enhanced angiogenesis, improved global cardiac function and attenuation of the progressive increase in end diastolic volume [61]. Furthermore, the paracrine mechanism may contribute towards modulation of immune response as well as mobilization and homing-in of stem cells for their participation in the repair process.
Skeletal myoblasts are excellent carriers of therapeutic genes and, thus, have been genetically modified with both viral and nonviral vectors that encode for different cytokines and growth factor genes to improve their functional characteristics in terms of survival, engraftment and differentiation [62–65]. Skeletal myoblasts that were genetically modified with an adeno-viral vector encoding for human VEGF165 continued to secrete human VEGF165 protein in the infarcted heart of a syngenic mouse for 2 weeks as compared with the nontransfected cell transplanted mouse hearts [64]. The cells also demonstrated extensive differentiation into multinucleated myotubes. Comparable effects were also observed with human VEGF165 gene-transduced skeletal myoblasts in a porcine heart model of chronic infarction [22]. These results highlighted the safety, feasibility and effectiveness of skeletal myoblast transplantation with therapeutic gene delivery for myocardial repair. Similarly, cardiotrophin-1, a member of the IL-6 superfamily, has potent hypertrophic and survival effects on cardiomyocytes [66]. It has been demonstrated that transplantation of cardiotrophin-1-expressing skeletal myoblasts into the left ventricular wall alleviated the transition from compensatory hypertrophy to congestive heart failure in Dahl salt-sensitive hypertensive rats. Other targets for the prevention of skeletal myoblast death have also been exploited. The level of IL-1, a proinflammatory cytokine, significantly increases and negatively influences postmyocardial infarction hypertrophy and collagen turnover, and is also implicated in skeletal myoblast death after grafting. Transplantation of skeletal myoblasts that express the secretory IL-1 receptor antagonist specifically attenuated adverse remodeling as a result of the increased survival of skeletal myoblasts [63]. In another interesting study, Formigli et al. genetically modified skeletal myoblasts to overexpress cardiotropic hormone relaxin in order to enhance their morphofunctional integration with cardiomyocytes [67]. The same group of researchers demonstrated enhanced integration and beneficial effects of relaxin-overexpressing skeletal myoblasts in a rat model of myocardial infarction [68]. However, most of these studies involve viral vectors for therapeutic gene transfer, which is not without adverse effects and ethical considerations [69]. Strategies ranging from the deletion of adenovirus replication genes E1 and E3 to the development of gutless adenoviruses with all viral genes removed have been developed to address the safety issues. Similarly, the use of lentiviral vectors has progressed from first generation viruses to safer third generation self-inactivating vectors. Alternatively, several recent studies have demonstrated the successful use of nonviral delivery systems for gene modification of skeletal myoblasts [62,70]. Although less efficient, the use of nonviral vector delivery overcomes the undesired effects of viral vectors. An interesting new development in this regard is the use of nanoparticle-based delivery of the transgenes into human skeletal myoblasts [31].
Besides genetic modification, treatment of skeletal myoblasts with recombinant growth factor proteins can be used to modulate their in vitro culture characteristics and postengraftment behavior [71]. For example, the presence of recombinant IGF-1 and basic FGF in vitro significantly enhanced the expression of the gelatinase matrix metalloproteinase-9 with fibrinolytic system activity focused at the cell membrane [72]. In addition, treatment with IGF-1 or basic FGF improved the in vivo chemokinetic potential of human skeletal myoblasts by modulating their endogenous proteolytic activity. In one of our recent studies, we ischemically preconditioned skeletal myoblasts to promote their resistance to oxidant stress [Kim HW, Haider KH et al., Unpublished Data]. These results were later extrapolated to mesenchymal stem cells to demonstrate that hypoxia inducible factor-1α-dependent miRNA-210 was responsible for the cytoprotective effects of ischemic preconditioning [73]. Using our in vitro as well as experimental animal models, we have also reported that cytoprotective effects of ischemic preconditioning can be duplicated by pharmacological manipulation of skeletal myoblasts using preconditioning mimetics such as diazoxide [74]. Our results demonstrated a remarkable improvement in survival of the preconditioned skeletal myoblasts compared with the native skeletal myoblasts under oxidant stress in vitro. Similar results were obtained when syngenic skeletal myoblasts were transplanted into a rat heart model of acute myocardial infarction with nearly twofold higher survival of preconditioned skeletal myoblasts as compared with their nonpreconditioned counterparts. In view of a direct relation between therapeutic outcome of the heart cell therapy and the number of transplanted cells, these results were significant. We also observed activation of Akt signaling, and elevated expression of secretable growth factors including VEGF, angiopoietin-1, basic FGF and HGF expression in the preconditioned skeletal myoblasts with a concomitant increase in blood vessel density in the recipient animals hearts. These results support the application of diazoxide preconditioning to enhance the therapeutic effectiveness of skeletal myoblasts in the clinical setting as diazoxide is already in clinical use.
Delivery strategy has a significant bearing on efficacy of the transplanted cells. Intramyocardial multisite pressure injections, in the form of microdepots, allow the safe and reliable transplantation of several myoblasts into an infarcted myocardium with improved efficacy compared with the standard technique [75]. Similarly, transplantation of skeletal myoblasts in the periphery of the infarcted myocardium is more effective and safe compared with transplantation in the center of the infarct [47].
Skeletal myoblasts in the clinical studies
After their established safety and efficacy in animal models, skeletal myoblasts were used in postmyocardial patients in clinical settings (Table 1). In the first clinical study, autologous skeletal myoblasts were transplanted into the heart of a 57-year-old male patient, and the transplanted cells survived and differentiated to form islands of skeletal muscle in the infarcted heart [76,77]. The whole transplantation procedure was event free and was performed as an adjunct to the routine revascularization by coronary artery bypass grafting. Results from heart function studies were promising, as confirmed by an increase in left ventricle ejection fraction and an increase in segmental contractility on echocardiography, and, thus, paved the way for multiple sporadic individualized attempts and later Phase I and II clinical trials. Most of these studies have used skeletal myoblast engraftment either as an adjunct to CABG, percutaneous transluminal coronary intervention, left ventricular assist device implantation or, in some cases, as a standalone procedure.
Table 1.
Human studies using skeletal myoblasts for myocardial repair.
| Author | Approach | Patients (n) | Number of cells | Percentage purity | Ref. |
|---|---|---|---|---|---|
| Menasche et al. | Adjunct to CABG | 1 | 8 × 108 | CD56+ (65%) | [76] |
| Menasche et al. | Adjunct to CABG | 10 | Average 8.71 × 108 | CD56 (86%) | [78] |
| Dib et al. | CABG/LVAD | 12 CABG 6 LVAD |
∼10–300 × 106 | CD56 (43–98%) | [80] |
| Herreros et al. | CABG | 12 | Average 2.21 × 108 | CD56 (65.6%) | [81] |
| Sim et al. | Adjunct to CABG | 1 | 3.74 × 108 | Desmin (>98%) | [133] |
| Law et al. | Adjunct to CABG | 3 | 110 and 120 × 106 | Desmin (>98%) | [105] |
| Chachques et al. | Adjunct to CABG | 20 | 300 ± 20 × 106 | CD56+ desmin (78 ± 5%) | [88] |
| Siminiak et al. | Adjunct to CABG | 10 | 4 × 105–5 × 107 | Desmin (65.4 ± 5.5%) | [82] |
| Gavira et al. | Adjunct to CABG | 10 | 2.21 × 108 (105–390 × 106) | CD56 (65.6%, 48–92%) | [41] |
| Biagini et al. | NOGA™ injection | 10 | 217 ± 111 × 106 | Desmin | [134] |
| Menasche et al. The Medical Research Council Adjuvant Gastric Infusional Chemotherapy (MAGIC) trial | Adjunct to CABG | Low dose = 33 High dose = 34 |
Low dose 400 × 106 High dose 400 × 106 |
CD56 (89%) | [29] |
CABG: Coronary artery bypass grafting; LVAD: Left ventricle assist device.
The first Phase I study with skeletal myoblasts was reported in 2003 in a group of ten severe ischemic cardiomyopathy patients (mean age: 60 ± 3 years; range: 38–73) and assessed the feasibility and safety of autologous skeletal myoblast transplantation [78]. Feasibility was defined as the ability of the expansion procedure to yield the target numbers of cells within 2–3 weeks, while safety referred to adverse events related to cell implantation. An average volume of 5.7 ± 0.3 ml, containing 871 ± 62 × 106 cells, was injected in 37 ± 3 sites throughout the scar area without any immediate postoperative complications, except one patient, whose early death was unrelated to the cell transplantation. A short-term follow-up period averaging 10.9 ± 4.5 months showed improvement in patients' clinical symptoms from the New York Heart Association class 2.7 ± 0.2 preoperatively to 1.6 ± 0.1 postoperatively (p < 0.02). Transthoracic echocardiography showed up to 63% improved systolic thickening of the scar area and left ventricular ejection fraction (LVEF) rose from 23.8 ± 3.9% preoperatively to 32.1 ± 7.5% postoperatively (p < 0.02). Long-term follow-up demonstrated that the New York Heart Association class improved from 2.5 ± 0.5 to 1.8 ± 0.4 at myocardial infarction (p = 0.004 vs baseline) and 1.7 ± 0.5 at the end of follow-up (p = 1 vs myocardial infarction: p = 0.0007 vs baseline). There were five hospitalizations for heart failure, in three patients, at 28.6 ± 9.9 months (range: 13–71). Owing to the persistent symptoms, two patients were implanted with a ventricular resynchronization pacemaker, whereas the third patient received automatic cardiac defibrillator with a resynchronization function on the physician's request. This study concluded that both clinical status and LVEF stably improved over time with a remarkably low incidence of hospitalization for heart failure, and the arrhythmic risk can be treated by medical therapy or by automatic cardiac defibrillator implantation.
Pagani et al. adopted an interesting approach to investigate the feasibility and safety of autologous skeletal myoblast transplantation in patients with ischemic heart disease undergoing left ventricular assist device implantation as a bridge to orthotropic heart transplantation [79]. Using this protocol, they were able to report the viability of cell transplants histologically in recipient heart after 68, 91, 144 and 191 days of left ventricular assist device support. Histological examination demonstrated that the transplanted skeletal myoblasts survived and differentiated into mature myofibers in three of the four explanted hearts. These results were later duplicated by Dib et al. in five patients who demonstrated survival, feasibility and safety of autologous skeletal myoblast transplantation, and suggest that this modality offers a potential therapeutic treatment for end-stage heart failure [80].
Subsequent to the first Phase I study, various groups reported skeletal myoblast engraftment in patients as an adjunct procedure to CABG [41,80–82]. Since many of the surviving myocardial infarction patients are not candidates for CABG, and it is difficult to access all myocardial segments via epicardial delivery route, a transcatheter system was assessed in large animal models [83] and subsequently used in patients as an adjunct to percutaneous coronary intervention [84,85]. Despite the technical challenges involved, the results of these clinical studies have been encouraging. A recent study has reported a head-to-head comparison of percutaneous versus surgical delivery techniques in an experimental animal model of acute myocardial infarction in Yucatan minipigs [86]. Magnetic resonance studies revealed that beneficial effects of cell transplantation were independent of the delivery strategy. Both delivery approaches led to the reversal of remodeling, and a comparable improvement in systolic function, regional perfusion and scar characteristics 6 months after cell transplantation. A relative increase in the arrhythmogenic peri-infarct border zone was also observed in both the groups of animals.
Given the difficulties in delineating the beneficial effects of cell therapy from the routine revascularization intervention, it was important to use skeletal myoblast engraftment as a standalone therapy. Smits et al. reported the feasibility and promise of NOGA™-guided catheter-based cell transplantation using autologous skeletal myoblasts as a standalone therapy for the treatment of ischemic heart failure [87]. In comparison with the baseline observations, LVEF increased from 36 ± 11% to 41 ± 9% (3 months, p = 0.009) and 45 ± 8% (6 months, p = 0.23). Regional wall analysis by MRI demonstrated significantly increased wall thickness at the target areas compared with the remote areas (wall thickening at target areas after 3-month follow-up: 0.9 ± 2.3 mm, 1.8 ± 2.4 mm, p = 0.008). Subsequent studies involving transcatheter delivery of skeletal myoblast demonstrated similar results [42,84,87], albeit with postprocedural arrhythmias in three patients [87]. Although Phase I clinical studies clearly demonstrated the safety and feasibility of skeletal myoblast engraftment in postinfarction scars, it was difficult to delineate the functional effectiveness of the intervention where the cell transplantation was carried out as an adjunct to routine revascularization procedures [81,88]. This failure may be attributed to multiple factors, including difference in the purity and quality of the cell preparations used by each research group, the delivery strategy, differences in the methods to evaluate the study end points and, of course, the small number of subjects included in each study.
Menasche et al. started the first Phase II trial – Myoblast Autologous Grafting in Ischemic Cardiomyopathy (MAGIC) trial [29]. This multicenter, randomized, placebo-controlled, three-arm, double-blind study included patients with left ventricular dysfunction (ejection fraction ≤35%), myocardial infarction and indication for coronary surgery. It was conducted in 24 academic hospitals in France, Germany, Belgium, the UK and Italy. A total of 120 patients were included in the study, divided into three groups (high dose, low dose and placebo groups). Of the 120 patients, 97 underwent CABG surgery and received autologous myoblast injections (400 or 800 million). Of these, 34 were assigned to the control group, 33 to the low-dose cell group and 30 to the high-dose cell group. All patients received an implantable cardioverter–defibrillator. Approximately 97, 93 and 98 initially akinetic myocardial segments were injected with autologous myoblasts in the placebo, low-dose and high-dose cell group, respectively. The 6 months follow-up demonstrated that the number of patients having improved segmental contraction by one grade was not affected by myoblast injections, regardless of the dose (placebo group: 48%; low-dose group: 35%; high-dose group: 40%; p = 0.66). Skeletal myoblast transfer did not improve regional or global left ventricular function beyond that seen in the control patients. The absolute change in ejection fraction between 6 months and baseline was 4.4, 3.4, and 5.2% in the placebo, low-dose and high-dose groups, respectively. However, the high-dose cell group had a significant decrease in left ventricular volumes compared with the placebo group. Although a higher incidence of arrhythmic events were observed in myoblast-treated patients, rates of major cardiac adverse events and ventricular arrhythmias at 6 months did not differ significantly between the pooled treatment and placebo groups. Therefore, the study concluded that skeletal myoblast transplantation, in combination with CABG, did not improve heart function, and further investigations are required to investigate the increased number of early postoperative arrhythmic events after skeletal myoblast transplantation, as well as the capability of high-dose injections to revert left ventricular remodeling. Besides the MAGIC trials, some other clinical studies with autologous myoblast implantation using catheter-based delivery in patients with heart failure include the Myogenesis Heart Efficiency and Regeneration Trial (MYOHEART), Safety and Effects of Implanted (Autologous) Skeletal Myoblasts (MyoCell) Using an Injection Catheter (SEISMIC) and Controlled Study Using 3D Guided Catheter-Based Delivery of Autologous Skeletal Myoblasts for Ischemic Cardiomyopathy (CAuSMIC) trials; however, these trials had relatively small numbers of participants.
Challenges in skeletal myoblast-based heart cell therapy
Although skeletal myoblasts have proven efficiency of developing into functionally competent myofibers postengraftment in the infarcted heart, multiple challenges still hamper their acceptance as ideal donor cells for cellular cardiomyoplasty (i.e., a therapeutic strategy based on cell transplantation for myocardial repair). First, the myofibers derived from the transplanted skeletal myoblasts remain electromechanically isolated from the host myocardium. This failure in electromechanical coupling is caused by their failure to develop intercalated discs – a basic functional unit required to accomplish functional integration and synchronization of electrical activity between adjacent myofibers [89]. This consists of the intracellular adhesion molecules, N-cadherin and connexion 43, and is required to accomplish exchange of small metabolites between adjacent cells and provide a low-resistance electrical pathway between myofibers. Isolated skeletal myoblasts, cultured together with neonatal cardiomyocytes in vitro, express cardiac-specific proteins (GATA-4, Nkx2.5 and ANP) as well as N-cadherin and connexion 43 at the cell–cell junctions [90]. Furthermore, a low percentage of myotubes also demonstrate synchronous contractile activity with the surrounding cardiomyocytes. However, the differentiated skeletal myoblasts downregulate expression of both N-cadherin and connexion 43; thus, resulting in no electrical coupling. Genetic modification of skeletal myoblasts for connexion 43 overexpression improved their functional integration and synchronous contractility, and increased the amplitude of gap junction conductance with the host myocytes [91,92]. However, more recent studies have issued a note of caution that such electrical coupling may be insufficient to prevent postinfarct arrhythmias in heart failure patients [93]. Furthermore, cardiac and skeletal muscles differ in expression of the dihydropyridine receptor, which regulates excitation–contraction coupling in myocytes [94]. The arrhythmias arising as a result of the lack of electromechanical integration represents a major problem of skeletal myoblasts transplantation [95–97].
Amongst the other challenges related to skeletal myoblast application for myocardial infarction repair, massive attrition rate of skeletal myoblasts (as high as 90%), especially during the acute phase after engraftment, significantly influence the overall efficacy of the procedure [98]. The high attrition rate of donor cells during the acute phase after transplantation is attributed to multiple factors, including oxidative stress, poor availability of nutrients, lack of adherence with the host tissue and the inflammatory/immune responses in the cytokine-rich ischemic myocardial environment [98]. Multiple strategies have been adopted to increase donor cells survival rate [99]. We have already demonstrated that ischemic preconditioning of cells by exposure to multiple cycles of hypoxia/re-oxygenation primed the cells to withstand the rigors of ischemic myocardium [Kim HW, Haider KH et al., Unpublished Data]. We have extrapolated these results to demonstrate that ischemic preconditioning can effectively improve the survival of cells other than skeletal myoblasts [73]. We have also reported that the cytoprotective effects of preconditioning can be duplicated by manipulation of the cells with preconditioning mimetics and growth factors and pharmacological agents that have clinically proven safety and efficacy [74,100,101].
Another important factor that significantly influences the effectiveness of skeletal myoblasts is the age-related diminution of their growth and differentiation characteristics. Like any other cell in the body, physiological aging also occurs in stem cells. We have previously demonstrated that aging of bone marrow-derived stem cells reduces their differentiation potential [102]. In a direct comparison between young and old donor-derived skeletal myoblasts, in vitro proliferation and myotube formation were significantly greater in skeletal myoblasts from young rats (3 months old) compared with their aging counterparts (24 months old) [103]. The functional deficit, in terms of compromised proliferative kinetics, depleted phenotypic plasticity and reduced regenerative potential of aging skeletal myoblasts are expected to diminish their therapeutic effectiveness, which would be further reduced upon transplantation in the ischemic and aging heart of elderly patients. With these considerations, one has to weigh the advantages and disadvantages of using autologous skeletal myoblasts in clinical situations, especially for elderly patients. In line with our findings that skeletal myoblasts are conditionally immuno-priviledged [104], we have already demonstrated the feasibility of allogenic skeletal myoblasts for the heart cell therapy in animal models with the use of transient immunosuppression [22,105].
From the mechanistic perspective, satellite cell activation and cell fate determination are controlled by the Notch signaling pathway, which is initiated by rapid increase in expression of the Notch ligand, Delta, subsequent to injury [106]. Physiological aging of skeletal muscle is characterized by diminished Delta upregulation in response to injury, which results in diminished satellite cell activation. Induction of Notch activity can restore the regenerative potential of aged satellite cells. Interestingly, aged satellite cells expressed a better response when exposed to serum from young mice, as the authors observed either in vivo by heterochronic parabiotic pairings or in vitro. These data clearly suggest that even very old tissue-specific stem cells retain their ability to participate in tissue maintenance and repair, if provided with the optimal environment. A newer development in this regard is the role of miRNAs (miRs), which effect almost every aspect of cell behavior and functionality [73,107–109]. miRs constitute a class of short (∼22 nucleotides), noncoding RNA molecules, which are important regulators of gene expression via mRNA translational inhibition [107]. A group of miRNAs, including miR-1, -133 and -206, have distinct roles in modulating skeletal and cardiac muscle proliferation and differentiation [110–112]. Using C2C12 myoblasts in vitro, miR-206 and -1 have been demonstrated to significantly alter myogenic differentiation of myoblasts, while miR-133 repressed differentiation but promoted myoblasts proliferation [112]. Other studies have also demonstrated that miR-206 and -1 directly downregulated gap junction coupling after the initiation of myoblast fusion in vitro and in vivo and inhibit Cx43 expression during myoblast differentiation without altering Cx43 mRNA levels [113]. Cx43 mRNA contains two binding sites for miR-206/-1 in its 3′ untranslated region, both of which are required for its efficient downregulation [113]. Clearly, this interesting mechanism of skeletal myoblast regulation needs more research owing to its great therapeutic impact.
Future perspective
Despite promising results from heart cell therapy with skeletal myoblasts both in preclinical and clinical studies, there are issues (i.e., dose of the cells, route of delivery and cell survival) that must be addressed to achieve optimal prognosis. The therapeutic outcome of the procedure is generally considered as a direct function of the number of injected skeletal myoblasts [114]. There is an urgent need to optimize culture conditions such that the required number of cells could be generated without compromising their proliferation and differentiation characteristics. Combined with the strategies to improve their survival postengraftment and an optimal delivery approach, the outcome of the approach can be improved [115]. Intramyocardial injection has been extensively used as a route of cell delivery into the heart and permits engraftment of the cells in selective areas of the myocardium under direct vision. The precision of cell transplantation can be improved by using repetitive cell dispensers [116]. Direct intramyocardial injection of skeletal myoblasts is considered as proarrhythmogenic and less efficient owing to loss of the transplanted cells from the site of injection. Recent studies have explored the safety and feasibility of alternative delivery strategies, and suggested three percutaneous cell delivery methods including intracoronary, transendocardial and coronary transvenous injection. Intracoronary delivery of donor cells is safe and permits global dissemination of the cells to the heart [115,117]. However, the intracoronary route is less specific and, therefore, may reduce therapeutic effectiveness of the procedure. Furthermore, intracoronary delivery of skeletal myoblasts may increase the risk of coronary embolism, leading to myocardial infarction, which may be avoided by myoblast preparations as a single-cell suspension [118]. ECG monitoring of the animals during a comparative study between intramyocardial and intravenous routes of administration revealed that arrhythmias were rarely observed 1 day or more prior to cell transplantation [115]. However, within 24 h of intramyocardial skeletal myoblast injection, ventricular premature contractions frequently occurred and ventricular tachycardia was observed in 50% of the animals, while no ventricular premature contractions or ventricular tachycardia were observed in the animals with intracoronary injection of skeletal myoblasts. The transendocardial route allows selective delivery of cells into the infarcted myocardium under the NOGA electromechanical guidance system [52,119]. However, the functional benefits for transcatheter delivery and transepicardial delivery are similar in terms of improvement in cardiac function [120]. Percutaneous catheter-based cell delivery strategies also allow implantation of multiple skeletal myoblasts. Repeated administration of skeletal myoblasts may be more effective compared with a single dose. Multiple doses of repeated injections of skeletal myoblasts attenuated infarct size and resulted in significantly higher LVEF compared with the single-dose administration in an experimental animal model of chronic myocardial infarction [121,122].
Efforts are underway to promote cell retention at the site of the cell graft to enhance the efficiency of the procedure [123]. A comparison of intramyocardial cell transplantation with cell sheet-based epicardial deposition of skeletal myoblasts have demonstrated that the latter strategy was equally effective but less traumatic [124]. A cell sheet-based epicardial delivery strategy avoids needle injections; it involves covering of the affected area with cell-seeded biocompatible sheets and biodegradable skeletal muscle grafts. Such sheet-shaped skeletal myoblasts are glued on to the epicardium and may be more efficient than injection-delivered skeletal myoblasts, reducing fibrosis, enhancing angiogenesis and, ultimately, improving heart function [125].
Despite the global beneficial outcome of skeletal myoblast engraftment, the inherent incapability of these cells to functionally couple with the host cardiomyocytes after differentiation remains a concern. Although the pathogenesis of arrhythmias with skeletal myoblasts remains unclear, the electromechanical isolation of the differentiated skeletal myoblast-derived neofibers is considered as one of the possible factors for postoperative events during heart cell therapy. Various clinical studies have reported untoward events of ventricular arrhythmias in patients receiving skeletal myoblast therapy [78,82]. However, in all of these reported cases, the problem was pharmacologically treatable. By contrast, optimal mapping in the canine left-ventricular wedge preparation demonstrated that arrhythmia inducibility was not increased by skeletal myoblast transplantation [96]. Lack of arrhythmias with skeletal myoblast engraftment has also been observed in large animal studies [126]. Therefore, these contrasting observations require us to remain aware of the arrhythmogenic nature of not only skeletal myoblasts, but also other types of donor cells. Furthermore, in the future, strategies must be designed to overcome this problem in order to establish stem cell transplantation as a clinically safe and relevant therapeutic modality [91].
Skeletal myoblast transplantation can also be combined with transplantation of other cell types or growth factor administration to enhance their efficacy. A combined therapy based on simultaneous delivery of skeletal myoblasts with bone marrow stem cells may be more effective compared with either cell type alone [127]. Similarly, combined growth factor administration with skeletal myoblasts may allow their dissemination from the site of injection [128]. We have already reported the promising results of pharmacological and genetic modification to improve skeletal myoblast engraftment and their regenerative properties [22,31,74]. It is obvious that the most advantageous strategy would be simultaneous transfection of skeletal myoblasts with several therapeutic genes that significantly improved their paracrine activity [129]. We have recently observed that simultaneous transfection of skeletal myoblasts with multiple growth factors promoted their ability to integrate with host myocytes, besides concomitant involvement of intrinsically available stem and progenitor cells from bone marrow, myocardium and peripheral circulation of the host [Konoplyannikov M, Haider KH et al., Unpublished Data]. Clearly, paracrine mechanisms need to be studied in more detail since these mechanisms, as well as ventricular remodeling limitations, are crucial for heart function improvement after myoblast transplantation.
Fractionation of skeletal myoblasts into their constituent heterogeneous subpopulations of cells is one of the most prospective directions towards developing better cells for cardiac transplantation. Traditionally, the bulk of non-fractionated skeletal myoblasts has been used for transplantation. However, the existence of distinct subpopulations of skeletal myoblasts have been reported, with only the minority of cells that are slowly growing in culture being able to survive and proliferate after grafting [130]. Over the last few years, a number of interesting publications have emerged, which are devoted to certain subpopulations of stem cells in the skeletal muscle that have been characterized for their potential to adopt cardiac as well as endothelial phenotypes [131,132]. These skeletal-based precursors of cardiomyocytes have been demonstrated to possess robust engraftment characteristics and generate beating cardiomyocytes in vitro and after transplantation into the infarcted myocardium.
In conclusion, similar to any other cell types, the use of skeletal myoblasts for myocardial repair is not without its advantages and disadvantages. Skeletal myoblasts remain the most well-studied donor cell type. Indepth mechanistic studies, genetic reprogramming or pharmacological manipulation, and a combinatorial approach involving skeletal myoblast transplantation with other relevant interventions, such as growth factor administration, can help to improve their integration characteristics, safety and therapeutic efficacy in the clinical settings during the next 5 years.
Acknowledgments
This work was supported by NIH grants R37-HL074272, HL-080686 and HL-087246 (M Ashraf), and HL-087288 and HL-089535 (KH Haider).
Footnotes
Financial & competing interests disclosure
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Bibliography
Papers of special note have been highlighted as:
■ of interest
■■ of considerable interest
- 1.Cleland JG, McGowan J. Heart failure due to ischaemic heart disease: epidemiology, pathophysiology and progression. J Cardiovasc Pharmacol. 1999;33(Suppl. 3):S17–S29. doi: 10.1097/00005344-199906003-00003. [DOI] [PubMed] [Google Scholar]
- 2.Frangogiannis NG. The immune system and cardiac repair. Pharmacol Res. 2008;58:88–111. doi: 10.1016/j.phrs.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haqqani HM, Mond HG. The implantable cardioverter-defibrillator lead: principles, progress, and promises. Pacing Clin Electrophysiol. 2009;32:1336–1353. doi: 10.1111/j.1540-8159.2009.02492.x. [DOI] [PubMed] [Google Scholar]
- 4.Alba AC, Delgado DH. The future is here: ventricular assist devices for the failing heart. Expert Rev Cardiovasc Ther. 2009;7:1067–1077. doi: 10.1586/erc.09.86. [DOI] [PubMed] [Google Scholar]
- 5.Soonpaa MH, Field LJ. Assessment of cardiomyocyte DNA synthesis in normal and injured adult mouse hearts. Am J Physiol. 1997;272:H220–H226. doi: 10.1152/ajpheart.1997.272.1.H220. [DOI] [PubMed] [Google Scholar]
- 6.Rubart M, Field LJ. Cardiac regeneration: repopulating the heart. Annu Rev Physiol. 2006;68:29–49. doi: 10.1146/annurev.physiol.68.040104.124530. [DOI] [PubMed] [Google Scholar]; ■ Critical review of heart cell therapy.
- 7.Bergmann O, Bhardwaj RD, Bernard S, et al. Evidence for cardiomyocyte renewal in humans. Science. 2009;324:98–102. doi: 10.1126/science.1164680. [DOI] [PMC free article] [PubMed] [Google Scholar]; ■■ Excellent study demonstrating cardiomyocyte renewal in the postnatal heart.
- 8.Hassink RJ, Pasumarthi KB, Nakajima H, et al. Cardiomyocyte cell cycle activation improves cardiac function after myocardial infarction. Cardiovasc Res. 2008;78:18–25. doi: 10.1093/cvr/cvm101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anversa P, Leri A, Kajstura J, Nadal-Ginard B. Myocyte growth and cardiac repair. J Mol Cell Cardiol. 2002;34:91–105. doi: 10.1006/jmcc.2001.1506. [DOI] [PubMed] [Google Scholar]; ■ Discusses the potential of cardiomyocytes to replicate in the postnatal heart.
- 10.Nadal-Ginard B, Kajstura J, Leri A, Anversa P. Myocyte death, growth, and regeneration in cardiac hypertrophy and failure. Circ Res. 2003;92:139–150. doi: 10.1161/01.res.0000053618.86362.df. [DOI] [PubMed] [Google Scholar]
- 11.Anversa P, Kajstura J, Leri A, Bolli R. Life and death of cardiac stem cells: a paradigm shift in cardiac biology. Circulation. 2006;113:1451–1463. doi: 10.1161/CIRCULATIONAHA.105.595181. [DOI] [PubMed] [Google Scholar]; ■ Discusses the inherent capacity of the mammalian heart for self-renewal.
- 12.Beltrami AP, Barlucchi L, Torella D, et al. Adult cardiac stem cells are multipotent and support myocardial regeneration. Cell. 2003;114:763–776. doi: 10.1016/s0092-8674(03)00687-1. [DOI] [PubMed] [Google Scholar]
- 13.Anversa P, Leri A, Kajstura J. Cardiac regeneration. J Am Coll Cardiol. 2006;47:1769–1776. doi: 10.1016/j.jacc.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Bearzi C, Leri A, Lo Monaco F, et al. Identification of a coronary vascular progenitor cell in the human heart. Proc Natl Acad Sci USA. 2009;106(37):15885–15890. doi: 10.1073/pnas.0907622106. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Rota M, Padin-Iruegas ME, Misao Y, et al. Local activation or implantation of cardiac progenitor cells rescues scarred infarcted myocardium improving cardiac function. Circ Res. 2008;103:107–116. doi: 10.1161/CIRCRESAHA.108.178525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dawn B, Stein AB, Urbanek K, et al. Cardiac stem cells delivered intravascularly traverse the vessel barrier, regenerate infarcted myocardium, and improve cardiac function. Proc Natl Acad Sci USA. 2005;102:3766–3771. doi: 10.1073/pnas.0405957102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matsuura K, Honda A, Nagai T, et al. Transplantation of cardiac progenitor cells ameliorates cardiac dysfunction after myocardial infarction in mice. J Clin Invest. 2009;119:2204–2217. doi: 10.1172/JCI37456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leri A, Hosoda T, Rota M, Kajstura J, Anversa P. Myocardial regeneration by exogenous and endogenous progenitor cells. Drug Discov Today Dis Mech. 2007;4:197–203. doi: 10.1016/j.ddmec.2008.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kajstura J, Rota M, Whang B, et al. Bone marrow cells differentiate in cardiac cell lineages after infarction independently of cell fusion. Circ Res. 2005;96:127–137. doi: 10.1161/01.RES.0000151843.79801.60. [DOI] [PubMed] [Google Scholar]
- 20.Orlic D, Kajstura J, Chimenti S, Bodine DM, Leri A, Anversa P. Transplanted adult bone marrow cells repair myocardial infarcts in mice. Ann NY Acad Sci. 2001;938:221–229. doi: 10.1111/j.1749-6632.2001.tb03592.x. [DOI] [PubMed] [Google Scholar]
- 21.Kudo M, Wang Y, Wani MA, et al. Implantation of bone marrow stem cells reduces the infarction and fibrosis in ischemic mouse heart. J Mol Cell Cardiol. 2003;35:1113–1119. doi: 10.1016/s0022-2828(03)00211-6. [DOI] [PubMed] [Google Scholar]; ┐ Provides evidence that bone marrow stem cells differentiate to adopt cardiac phenotype.
- 22.Haider H, Ye L, Jiang S, et al. Angiomyogenesis for cardiac repair using human myoblasts as carriers of human vascular endothelial growth factor. J Mol Med. 2004;82:539–549. doi: 10.1007/s00109-004-0546-z. [DOI] [PubMed] [Google Scholar]; ┐┐ Large animal study showing the effectiveness of skeletal myoblast (SM)-based angiogenic gene therapy of the infarcted heart.
- 23.Nelson TJ, Martinez-Fernandez A, Yamada S, et al. Repair of acute myocardial infarction by human stemness factors induced pluripotent stem cells. Circulation. 2009;120:408–416. doi: 10.1161/CIRCULATIONAHA.109.865154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siu CW, Moore JC, Li RA. Human embryonic stem cell-derived cardiomyocytes for heart therapies. Cardiovasc Hematol Disord Drug Targets. 2007;7:145–152. doi: 10.2174/187152907780830851. [DOI] [PubMed] [Google Scholar]
- 25.Crisostomo PR, Abarbanell AM, Wang M, et al. Embryonic stem cells attenuate myocardial dysfunction and inflammation after surgical global ischemia via paracrine actions. Am J Physiol Heart Circ Physiol. 2008;295:H1726–H1735. doi: 10.1152/ajpheart.00236.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martinez-Fernandez A, Nelson TJ, Yamada S, et al. iPS programmed without c-MYC yield proficient cardiogenesis for functional heart chimerism. Circ Res. 2009;105:648–656. doi: 10.1161/CIRCRESAHA.109.203109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Halbach M, Pfannkuche K, Pillekamp F, et al. Electrophysiological maturation and integration of murine fetal cardiomyocytes after transplantation. Circ Res. 2007;101:484–492. doi: 10.1161/CIRCRESAHA.107.153643. [DOI] [PubMed] [Google Scholar]
- 28.Ye L, Haider H, Jiang S, et al. Reversal of myocardial injury using genetically modulated human skeletal myoblasts in a rodent cryoinjured heart model. Eur J Heart Fail. 2005;7:945–952. doi: 10.1016/j.ejheart.2005.03.012. [DOI] [PubMed] [Google Scholar]; ┐ Small animal cryoinjury model to show cardiac reparability of SMs.
- 29.Menasche P, Alfieri O, Janssens S, et al. The Myoblast Autologous Grafting in Ischemic Cardiomyopathy (MAGIC) trial: first randomized placebo-controlled study of myoblast transplantation. Circulation. 2008;117:1189–1200. doi: 10.1161/CIRCULATIONAHA.107.734103. [DOI] [PubMed] [Google Scholar]; ┐┐ First randomized, placebo-controlled study using SMs in humans.
- 30.Ye L, Haider H, Tan R, et al. Angiomyogenesis using liposome based vascular endothelial growth factor-165 transfection with skeletal myoblast for cardiac repair. Biomaterials. 2008;29:2125–2137. doi: 10.1016/j.biomaterials.2008.01.014. [DOI] [PubMed] [Google Scholar]; ┐ Nonviral angiogenic gene modification of SMs for myocardial repair.
- 31.Ye L, Haider H, Tan R, et al. Transplantation of nanoparticle transfected skeletal myoblasts overexpressing vascular endothelial growth factor-165 for cardiac repair. Circulation. 2007;116:I113–I120. doi: 10.1161/CIRCULATIONAHA.106.680124. [DOI] [PubMed] [Google Scholar]
- 32.Khan M, Kutala VK, Vikram DS, et al. Skeletal myoblasts transplanted in the ischemic myocardium enhance in situ oxygenation and recovery of contractile function. Am J Physiol Heart Circ Physiol. 2007;293:H2129–H2139. doi: 10.1152/ajpheart.00677.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 34.Yamanaka S. Strategies and new developments in the generation of patient-specific pluripotent stem cells. Cell Stem Cell. 2007;21:39–49. doi: 10.1016/j.stem.2007.05.012. [DOI] [PubMed] [Google Scholar]; ┐ Summary of the role of transcription factors and chromatin remodeling during reprogramming.
- 35.Freund C, Mummery CL. Prospects for pluripotent stem cell-derived cardiomyocytes in cardiac cell therapy and as disease models. J Cell Biochem. 2009;107:592–599. doi: 10.1002/jcb.22164. [DOI] [PubMed] [Google Scholar]
- 36.Mauritz C, Schwanke K, Reppel M, et al. Generation of functional murine cardiac myocytes from induced pluripotent stem cells. Circulation. 2008;118:507–517. doi: 10.1161/CIRCULATIONAHA.108.778795. [DOI] [PubMed] [Google Scholar]
- 37.Mias C, Lairez O, Trouche E, et al. Mesenchymal stem cells promote matrix metalloproteinase secretion by cardiac fibroblasts and reduce cardiac ventricular fibrosis after myocardial infarction. Stem Cells. 2009;27(11):2734–2743. doi: 10.1002/stem.169. [DOI] [PubMed] [Google Scholar]
- 38.Schuleri KH, Feigenbaum GS, Centola M, et al. Autologous mesenchymal stem cells produce reverse remodelling in chronic ischaemic cardiomyopathy. Eur Heart J. 2009;30(22):2722–2732. doi: 10.1093/eurheartj/ehp265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hoashi T, Matsumiya G, Miyagawa S, et al. Skeletal myoblast sheet transplantation improves the diastolic function of a pressure-overloaded right heart. J Thorac Cardiovasc Surg. 2009;138:460–467. doi: 10.1016/j.jtcvs.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 40.Ghostine S, Carrion C, Souza LC, et al. Long-term efficacy of myoblast transplantation on regional structure and function after myocardial infarction. Circulation. 2002;106:I131–I136. [PubMed] [Google Scholar]; ┐ Long-term effectiveness of SM therapy.
- 41.Gavira JJ, Herreros J, Perez A, et al. Autologous skeletal myoblast transplantation in patients with nonacute myocardial infarction: 1-year follow-up. J Thorac Cardiovasc Surg. 2006;131:799–804. doi: 10.1016/j.jtcvs.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 42.Ince H, Petzsch M, Rehders TC, et al. Transcatheter transplantation of autologous skeletal myoblasts in postinfarction patients with severe left ventricular dysfunction. J Endovasc Ther. 2004;11:695–704. doi: 10.1583/04-1386R.1. [DOI] [PubMed] [Google Scholar]
- 43.Menasche P. Skeletal myoblasts as a therapeutic agent. Prog Cardiovasc Dis. 2007;50:7–17. doi: 10.1016/j.pcad.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 44.Haider H, Tan AC, Aziz S, Chachques JC, Sim EK. Myoblast transplantation for cardiac repair: a clinical perspective. Mol Ther. 2004;9:14–23. doi: 10.1016/j.ymthe.2003.10.009. [DOI] [PubMed] [Google Scholar]; ┐ Review of the clinical studies involving SM transplantation.
- 45.Al Attar N, Carrion C, Ghostine S, et al. Long-term (1 year) functional and histological results of autologous skeletal muscle cells transplantation in rat. Cardiovasc Res. 2003;58:142–148. doi: 10.1016/s0008-6363(02)00790-3. [DOI] [PubMed] [Google Scholar]
- 46.Taylor DA, Atkins BZ, Hungspreugs P, et al. Regenerating functional myocardium: improved performance after skeletal myoblast transplantation. Nat Med. 1998;4:929–933. doi: 10.1038/nm0898-929. [DOI] [PubMed] [Google Scholar]
- 47.McCue JD, Swingen C, Feldberg T, et al. The real estate of myoblast cardiac transplantation: negative remodeling is associated with location. J Heart Lung Transplant. 2008;27:116–123. doi: 10.1016/j.healun.2007.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brasselet C, Morichetti MC, Messas E, et al. Skeletal myoblast transplantation through a catheter-based coronary sinus approach: an effective means of improving function of infarcted myocardium. Eur Heart J. 2005;26:1551–1556. doi: 10.1093/eurheartj/ehi151. [DOI] [PubMed] [Google Scholar]
- 49.Hata H, Matsumiya G, Miyagawa S, et al. Grafted skeletal myoblast sheets attenuate myocardial remodeling in pacing-induced canine heart failure model. J Thorac Cardiovasc Surg. 2006;132:918–924. doi: 10.1016/j.jtcvs.2006.01.024. [DOI] [PubMed] [Google Scholar]
- 50.He KL, Yi GH, Sherman W, et al. Autologous skeletal myoblast transplantation improved hemodynamics and left ventricular function in chronic heart failure dogs. J Heart Lung Transplant. 2005;24:1940–1949. doi: 10.1016/j.healun.2005.02.024. [DOI] [PubMed] [Google Scholar]
- 51.Ye L, Haider H, Jiang S, et al. Improved angiogenic response in pig heart following ischaemic injury using human skeletal myoblast simultaneously expressing VEGF165 and angiopoietin-1. Eur J Heart Fail. 2007;9:15–22. doi: 10.1016/j.ejheart.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 52.Chazaud B, Hittinger L, Sonnet C, et al. Endoventricular porcine autologous myoblast transplantation can be successfully achieved with minor mechanical cell damage. Cardiovasc Res. 2003;58:444–450. doi: 10.1016/s0008-6363(02)00834-9. [DOI] [PubMed] [Google Scholar]
- 53.Zhang Z, van den Bos EJ, Wielopolski PA, et al. High-resolution magnetic resonance imaging of iron-labeled myoblasts using a standard 1.5-T clinical scanner. MAGMA. 2004;17:201–209. doi: 10.1007/s10334-004-0054-8. [DOI] [PubMed] [Google Scholar]
- 54.Atkins BZ, Hueman MT, Meuchel J, et al. Cellular cardiomyoplasty improves diastolic properties of injured heart. J Surg Res. 1999;85:234–242. doi: 10.1006/jsre.1999.5681. [DOI] [PubMed] [Google Scholar]
- 55.Marelli D, Desrosiers C, el-Alfy M, Kao RL, Chiu RC. Cell transplantation for myocardial repair: an experimental approach. Cell Transplant. 1992;1:383–390. doi: 10.1177/096368979200100602. [DOI] [PubMed] [Google Scholar]
- 56.Reinecke H, Murry CE. Transmural replacement of myocardium after skeletal myoblast grafting into the heart. Too much of a good thing? Cardiovasc Pathol. 2000;9:337–344. doi: 10.1016/s1054-8807(00)00055-7. [DOI] [PubMed] [Google Scholar]
- 57.Murry CE, Wiseman RW, Schwartz SM, Hauschka SD. Skeletal myoblast transplantation for repair of myocardial necrosis. J Clin Invest. 1996;98:2512–2523. doi: 10.1172/JCI119070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Reinecke H, MacDonald GH, Hauschka SD, Murry CE. Electromechanical coupling between skeletal and cardiac muscle Implications for infarct repair. J Cell Biol. 2000;149:731–740. doi: 10.1083/jcb.149.3.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Peterson JM, Pizza FX. Cytokines derived from cultured skeletal muscle cells after mechanical strain promote neutrophil chemotaxis in vitro. J Appl Physiol. 2009;106:130–137. doi: 10.1152/japplphysiol.90584.2008. [DOI] [PubMed] [Google Scholar]
- 60.Tatsumi R, Hattori A, Ikeuchi Y, Anderson JE, Allen RE. Release of hepatocyte growth factor from mechanically stretched skeletal muscle satellite cells and role of pH and nitric oxide. Mol Biol Cell. 2002;13:2909–2918. doi: 10.1091/mbc.E02-01-0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pouzet B, Ghostine S, Vilquin JT, et al. Is skeletal myoblast transplantation clinically relevant in the era of angiotensin-converting enzyme inhibitors? Circulation. 2001;104:I223–I228. doi: 10.1161/hc37t1.094593. [DOI] [PubMed] [Google Scholar]; ┐ Small animal study supporting clinical relevance of SM therapy for myocardial repair.
- 62.Elmadbouh I, Haider H, Jiang S, Idris NM, Lu G, Ashraf M. Ex vivo delivered stromal cell-derived factor-1α promotes stem cell homing and induces angiomyogenesis in the infarcted myocardium. J Mol Cell Cardiol. 2007;42:792–803. doi: 10.1016/j.yjmcc.2007.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Murtuza B, Suzuki K, Bou-Gharios G, et al. Transplantation of skeletal myoblasts secreting an IL-1 inhibitor modulates adverse remodeling in infarcted murine myocardium. Proc Natl Acad Sci USA. 2004;101:4216–4221. doi: 10.1073/pnas.0306205101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Suzuki K, Murtuza B, Smolenski RT, et al. Cell transplantation for the treatment of acute myocardial infarction using vascular endothelial growth factor-expressing skeletal myoblasts. Circulation. 2001;104:I207–I212. doi: 10.1161/hc37t1.094524. [DOI] [PubMed] [Google Scholar]; ┐ SM-based angiomyogenic repair of the heart.
- 65.Aharinejad S, Abraham D, Paulus P, et al. Colony-stimulating factor-1 transfection of myoblasts improves the repair of failing myocardium following autologous myoblast transplantation. Cardiovasc Res. 2008;79:395–404. doi: 10.1093/cvr/cvn097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Toh R, Kawashima S, Kawai M, et al. Transplantation of cardiotrophin-1-expressing myoblasts to the left ventricular wall alleviates the transition from compensatory hypertrophy to congestive heart failure in Dahl salt-sensitive hypertensive rats. J Am Coll Cardiol. 2004;43:2337–2347. doi: 10.1016/j.jacc.2004.02.048. [DOI] [PubMed] [Google Scholar]
- 67.Formigli L, Francini F, Nistri S, et al. Skeletal myoblasts overexpressing relaxin improve differentiation and communication of primary murine cardiomyocyte cell cultures. J Mol Cell Cardiol. 2009;47:335–345. doi: 10.1016/j.yjmcc.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 68.Bonacchi M, Nistri S, Nanni C, et al. Functional and histopathological improvement of the post-infarcted rat heart upon myoblast cell grafting and relaxin therapy. J Cell Mol Med. 2009;13:3437–3448. doi: 10.1111/j.1582-4934.2008.00503.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim CK, Haider KH, Lim SJ. Gene medicine: a new field of molecular medicine. Arch Pharm Res. 2001;24:1–15. doi: 10.1007/BF02976486. [DOI] [PubMed] [Google Scholar]
- 70.Ye L, Haider HK, Esa WB, et al. Liposome based vascular endothelial growth factor-165 transfection with skeletal myoblast for treatment of ischemic limb disease. J Cell Mol Med. 2010;14(1–2):323–336. doi: 10.1111/j.1582-4934.2008.00454.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chanseaume S, Azarnoush K, Maurel A, et al. Can erythropoietin improve skeletal myoblast engraftment in infarcted myocardium? Interact Cardiovasc Thorac Surg. 2007;6:293–297. doi: 10.1510/icvts.2006.144014. [DOI] [PubMed] [Google Scholar]
- 72.Lafreniere JF, Mills P, Tremblay JP, El Fahime E. Growth factors improve the in vivo migration of human skeletal myoblasts by modulating their endogenous proteolytic activity. Transplantation. 2004;77:1741–1747. doi: 10.1097/01.tp.0000131175.60047.eb. [DOI] [PubMed] [Google Scholar]
- 73.Kim HW, Haider HK, Jiang S, Ashraf M. Ischemic preconditioning augments survival of stem cells via MIR-210 expression by targeting caspase-8 associated protein 2. J Biol Chem. 2009;284(48):33161–33168. doi: 10.1074/jbc.M109.020925. [DOI] [PMC free article] [PubMed] [Google Scholar]; ┐┐ First study to extrapolate the concept of ischemic preconditioning to promote donor cell survival with a mechanistic participation of miRNA-210.
- 74.Niagara MI, Haider H, Jiang S, Ashraf M. Pharmacologically preconditioned skeletal myoblasts are resistant to oxidative stress and promote angiomyogenesis via release of paracrine factors in the infarcted heart. Circ Res. 2007;100:545–555. doi: 10.1161/01.RES.0000258460.41160.ef. [DOI] [PubMed] [Google Scholar]; ┐ First study to use preconditioning mimetic diazoxide to enhance SM survival in the infarcted heart.
- 75.Ott HC, Kroess R, Bonaros N, et al. Intramyocardial microdepot injection increases the efficacy of skeletal myoblast transplantation. Eur J Cardiothorac Surg. 2005;27:1017–1021. doi: 10.1016/j.ejcts.2005.01.065. [DOI] [PubMed] [Google Scholar]
- 76.Menasche P, Hagege AA, Scorsin M, et al. Myoblast transplantation for heart failure. Lancet. 2001;357:279–280. doi: 10.1016/S0140-6736(00)03617-5. [DOI] [PubMed] [Google Scholar]; ┐ First-in-man use of SMs for cardiac repair.
- 77.Hagege AA, Carrion C, Menasche P, et al. Viability and differentiation of autologous skeletal myoblast grafts in ischaemic cardiomyopathy. Lancet. 2003;361:491–492. doi: 10.1016/S0140-6736(03)12458-0. [DOI] [PubMed] [Google Scholar]; ┐┐ First direct evidence from human heart that transplanted SMs differentiated into myofibers in the infarcted heart.
- 78.Menasche P, Hagege AA, Vilquin JT, et al. Autologous skeletal myoblast transplantation for severe postinfarction left ventricular dysfunction. J Am Coll Cardiol. 2003;41:1078–1083. doi: 10.1016/s0735-1097(03)00092-5. [DOI] [PubMed] [Google Scholar]
- 79.Pagani FD, DerSimonian H, Zawadzka A, et al. Autologous skeletal myoblasts transplanted to ischemia-damaged myocardium in humans. Histological analysis of cell survival and differentiation. J Am Coll Cardiol. 2003;41:879–888. doi: 10.1016/s0735-1097(03)00081-0. [DOI] [PubMed] [Google Scholar]; ┐ First human study involving SM transplantation as an adjunct to left ventricle assist device implantation.
- 80.Dib N, McCarthy P, Campbell A, et al. Feasibility and safety of autologous myoblast transplantation in patients with ischemic cardiomyopathy. Cell Transplant. 2005;14:11–19. doi: 10.3727/000000005783983296. [DOI] [PubMed] [Google Scholar]
- 81.Herreros J, Prosper F, Perez A, et al. Autologous intramyocardial injection of cultured skeletal muscle-derived stem cells in patients with non-acute myocardial infarction. Eur Heart J. 2003;24:2012–2020. doi: 10.1016/j.ehj.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 82.Siminiak T, Kalawski R, Fiszer D, et al. Autologous skeletal myoblast transplantation for the treatment of postinfarction myocardial injury: Phase I clinical study with 12 months of follow-up. Am Heart J. 2004;148:531–537. doi: 10.1016/j.ahj.2004.03.043. [DOI] [PubMed] [Google Scholar]
- 83.Dib N, Campbell A, Jacoby DB, et al. Safety and feasibility of percutaneous autologous skeletal myoblast transplantation in the coil-infarcted swine myocardium. J Pharmacol Toxicol Methods. 2006;54:71–77. doi: 10.1016/j.vascn.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 84.Siminiak T, Fiszer D, Jerzykowska O, et al. Percutaneous trans-coronary-venous transplantation of autologous skeletal myoblasts in the treatment of post-infarction myocardial contractility impairment: the POZNAN trial. Eur Heart J. 2005;26:1188–1195. doi: 10.1093/eurheartj/ehi159. [DOI] [PubMed] [Google Scholar]
- 85.Dib N, Dinsmore J, Lababidi Z, et al. One-year follow-up of feasibility and safety of the first U.S., randomized, controlled study using 3-dimensional guided catheter-based delivery of autologous skeletal myoblasts for ischemic cardiomyopathy (CAuSMIC study) JACC Cardiovasc Interv. 2009;2:9–16. doi: 10.1016/j.jcin.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 86.Larose E, Proulx G, Voisine P, et al. Percutaneous versus surgical delivery of autologous myoblasts after chronic myocardial infarction: an in vivo cardiovascular magnetic resonance study. Catheter Cardiovasc Interv. 2010;75:120–127. doi: 10.1002/ccd.22204. [DOI] [PubMed] [Google Scholar]
- 87.Smits PC, van Geuns RJ, Poldermans D, et al. Catheter-based intramyocardial injection of autologous skeletal myoblasts as a primary treatment of ischemic heart failure: clinical experience with six-month follow-up. J Am Coll Cardiol. 2003;42:2063–2069. doi: 10.1016/j.jacc.2003.06.017. [DOI] [PubMed] [Google Scholar]
- 88.Chachques JC, Herreros J, Trainini J, et al. Autologous human serum for cell culture avoids the implantation of cardioverter-defibrillators in cellular cardiomyoplasty. Int J Cardiol. 2004;95(Suppl. 1):S29–S33. doi: 10.1016/s0167-5273(04)90009-5. [DOI] [PubMed] [Google Scholar]; ┐ First study demonstrating the advantage of using autologous serum to support SM culture.
- 89.Ferreira-Cornwell MC, Luo Y, Narula N, Lenox JM, Lieberman M, Radice GL. Remodeling the intercalated disc leads to cardiomyopathy in mice misexpressing cadherins in the heart. J Cell Sci. 2002;115:1623–1634. doi: 10.1242/jcs.115.8.1623. [DOI] [PubMed] [Google Scholar]
- 90.Formigli L, Francini F, Tani A, et al. Morphofunctional integration between skeletal myoblasts and adult cardiomyocytes in coculture is favored by direct cell–cell contacts and relaxin treatment. Am J Physiol Cell Physiol. 2008;288:C795–C804. doi: 10.1152/ajpcell.00345.2004. [DOI] [PubMed] [Google Scholar]
- 91.Suzuki K, Brand NJ, Allen S, et al. Overexpression of connexin 43 in skeletal myoblasts: relevance to cell transplantation to the heart. J Thorac Cardiovasc Surg. 2001;122:759–766. doi: 10.1067/mtc.2001.116210. [DOI] [PubMed] [Google Scholar]
- 92.Roell W, Lewalter T, Sasse P, et al. Engraftment of connexin 43-expressing cells prevents post-infarct arrhythmia. Nature. 2007;450:819–824. doi: 10.1038/nature06321. [DOI] [PubMed] [Google Scholar]
- 93.Fernandes S, van Rijen HV, Forest V, et al. Cardiac cell therapy: overexpression of connexin 43 in skeletal myoblasts and prevention of ventricular arrhythmias. J Cell Mol Med. 2009;13(9B):3703–3712. doi: 10.1111/j.1582-4934.2009.00740.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Garcia J, Tanabe T, Beam KG. Relationship of calcium transients to calcium currents and charge movements in myotubes expressing skeletal and cardiac dihydropyridine receptors. J Gen Physiol. 1994;103:125–147. doi: 10.1085/jgp.103.1.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Abraham MR, Hare JM. Is skeletal myoblast transplantation proarrhythmic? The jury is still out. Heart Rhythm. 2006;3:462–463. doi: 10.1016/j.hrthm.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 96.Fouts K, Fernandes B, Mal N, Liu J, Laurita KR. Electrophysiological consequence of skeletal myoblast transplantation in normal and infarcted canine myocardium. Heart Rhythm. 2006;3:452–461. doi: 10.1016/j.hrthm.2005.12.016. [DOI] [PubMed] [Google Scholar]; ┐┐ Electrophysiological consequences of SM transplantation.
- 97.Eisen HJ. Skeletal myoblast transplantation: no MAGIC bullet for ischemic cardiomyopathy. Nat Clin Pract Cardiovasc Med. 2008;5:520–521. doi: 10.1038/ncpcardio1299. [DOI] [PubMed] [Google Scholar]
- 98.Suzuki K, Murtuza B, Beauchamp JR, et al. Dynamics and mediators of acute graft attrition after myoblast transplantation to the heart. FASEB J. 2004;18:1153–1155. doi: 10.1096/fj.03-1308fje. [DOI] [PubMed] [Google Scholar]
- 99.Haider H, Ashraf M. Strategies to promote donor cell survival: combining preconditioning approach with stem cell transplantation. J Mol Cell Cardiol. 2008;45:554–566. doi: 10.1016/j.yjmcc.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]; ┐ Review of various preconditioning approaches to promote stem cell survival.
- 100.Pasha Z, Wang Y, Sheikh R, Zhang D, Zhao T, Ashraf M. Preconditioning enhances cell survival and differentiation of stem cells during transplantation in infarcted myocardium. Cardiovasc Res. 2008;77:134–142. doi: 10.1093/cvr/cvm025. [DOI] [PubMed] [Google Scholar]
- 101.El Fahime E, Bouchentouf M, Benabdallah BF, et al. Tubulyzine, a novel tri-substituted triazine, prevents the early cell death of transplanted myogenic cells and improves transplantation success. Biochem Cell Biol. 2003;81:81–90. doi: 10.1139/o03-054. [DOI] [PubMed] [Google Scholar]
- 102.Jiang S, Kh Haider H, Ahmed RP, Idris NM, Salim A, Ashraf M. Transcriptional profiling of young and old mesenchymal stem cells in response to oxygen deprivation and reparability of the infarcted myocardium. J Mol Cell Cardiol. 2008;44:582–596. doi: 10.1016/j.yjmcc.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kan CD, Li SH, Weisel RD, Zhang S, Li RK. Recipient age determines the cardiac functional improvement achieved by skeletal myoblast transplantation. J Am Coll Cardiol. 2007;50:1086–1092. doi: 10.1016/j.jacc.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 104.Haider H, Jiang SJ, Ye L, Aziz S, Law PK, Sim EK. Effectiveness of transient immunosuppression using cyclosporine for xenomyoblast transplantation for cardiac repair. Transplant Proc. 2004;36:232–235. doi: 10.1016/j.transproceed.2003.11.001. [DOI] [PubMed] [Google Scholar]; ┐┐ First study to show the immunoprivileged status of SMs after transplantation into the infarcted myocardium.
- 105.Law PK, Fang G, Chua F, Kakuchaya T, Bockeria LA. First-in-man myoblast allografts for heart degeneration. Int J Med Implants Devices. 2003;1:100–155. [Google Scholar]
- 106.Conboy IM, Conboy MJ, Smythe GM, Rando TA. Notch-mediated restoration of regenerative potential to aged muscle. Science. 2003;302:1575–1577. doi: 10.1126/science.1087573. [DOI] [PubMed] [Google Scholar]
- 107.Chen JF, Mandel EM, Thomson JM, et al. The role of microRNA-1 and microRNA-133 in skeletal muscle proliferation and differentiation. Nat Genet. 2006;38:228–233. doi: 10.1038/ng1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Foshay KM, Gallicano GI. Small RNAs, big potential: the role of microRNAs in stem cell function. Curr Stem Cell Res Ther. 2007;2:264–271. doi: 10.2174/157488807782793781. [DOI] [PubMed] [Google Scholar]
- 109.Hime GR, Somers WG. Micro-RNA mediated regulation of proliferation, self-renewal and differentiation of mammalian stem cells. Cell Adh Migr. 2009;3(4):425–432. doi: 10.4161/cam.3.4.9913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Callis TE, Chen JF, Wang DZ. MicroRNAs in skeletal and cardiac muscle development. DNA Cell Biol. 2007;26:219–225. doi: 10.1089/dna.2006.0556. [DOI] [PubMed] [Google Scholar]
- 111.Chen JF, Callis TE, Wang DZ. MicroRNAs and muscle disorders. J Cell Sci. 2009;122:13–20. doi: 10.1242/jcs.041723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kim HK, Lee YS, Sivaprasad U, Malhotra A, Dutta A. Muscle-specific microRNA miR-206 promotes muscle differentiation. J Cell Biol. 2006;174:677–687. doi: 10.1083/jcb.200603008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Anderson C, Catoe H, Werner R. MIR-206 regulates connexin43 expression during skeletal muscle development. Nucleic Acids Res. 2006;34:5863–5871. doi: 10.1093/nar/gkl743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pouzet B, Vilquin JT, Hagege AA, et al. Intramyocardial transplantation of autologous myoblasts: can tissue processing be optimized? Circulation. 2000;102:III210–III215. doi: 10.1161/01.cir.102.suppl_3.iii-210. [DOI] [PubMed] [Google Scholar]
- 115.Fukushima S, Coppen SR, Lee J, et al. Choice of cell-delivery route for skeletal myoblast transplantation for treating post-infarction chronic heart failure in rat. PLoS ONE. 2008;3:e3071. doi: 10.1371/journal.pone.0003071. [DOI] [PMC free article] [PubMed] [Google Scholar]; ┐ Demonstrates the effect of route of administration on the outcome of SM-based therapy.
- 116.Skuk D, Goulet M, Tremblay JP. Use of repeating dispensers to increase the efficiency of the intramuscular myogenic cell injection procedure. Cell Transplant. 2006;15:659–663. doi: 10.3727/000000006783981648. [DOI] [PubMed] [Google Scholar]
- 117.Suzuki K, Murtuza B, Fukushima S, et al. Targeted cell delivery into infarcted rat hearts by retrograde intracoronary infusion: distribution, dynamics, and influence on cardiac function. Circulation. 2004;110:II225–II230. doi: 10.1161/01.CIR.0000138191.11580.e3. [DOI] [PubMed] [Google Scholar]
- 118.Suzuki K, Brand NJ, Smolenski RT, Jayakumar J, Murtuza B, Yacoub MH. Development of a novel method for cell transplantation through the coronary artery. Circulation. 2000;102:III359–III364. doi: 10.1161/01.cir.102.suppl_3.iii-359. [DOI] [PubMed] [Google Scholar]
- 119.Perin EC, Dohmann HF, Borojevic R, et al. Transendocardial, autologous bone marrow cell transplantation for severe, chronic ischemic heart failure. Circulation. 2003;107:2294–2302. doi: 10.1161/01.CIR.0000070596.30552.8B. [DOI] [PubMed] [Google Scholar]
- 120.Gavira JJ, Perez-Ilzarbe M, Abizanda G, et al. A comparison between percutaneous and surgical transplantation of autologous skeletal myoblasts in a swine model of chronic myocardial infarction. Cardiovasc Res. 2006;71:744–753. doi: 10.1016/j.cardiores.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 121.Gavira JJ, Nasarre E, Abizanda G, et al. Repeated implantation of skeletal myoblast in a swine model of chronic myocardial infarction. Eur Heart J. 2009;31(8):1013–1021. doi: 10.1093/eurheartj/ehp342. [DOI] [PubMed] [Google Scholar]
- 122.Premaratne GU, Tambara K, Fujita M, et al. Repeated implantation is a more effective cell delivery method in skeletal myoblast transplantation for rat myocardial infarction. Circ J. 2006;70:1184–1189. doi: 10.1253/circj.70.1184. [DOI] [PubMed] [Google Scholar]
- 123.Martens TP, Godier AF, Parks JJ, et al. Percutaneous cell delivery into the heart using hydrogels polymerizing in situ. Cell Transplant. 2009;18:297–304. doi: 10.3727/096368909788534915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hamdi H, Furuta A, Bellamy V, et al. Cell delivery: intramyocardial injections or epicardial deposition? A head-to-head comparison. Ann Thorac Surg. 2009;87:1196–1203. doi: 10.1016/j.athoracsur.2008.12.074. [DOI] [PubMed] [Google Scholar]
- 125.Giraud MN, Ayuni E, Cook S, Siepe M, Carrel TP, Tevaearai HT. Hydrogel-based engineered skeletal muscle grafts normalize heart function early after myocardial infarction. Artif Organs. 2008;32:692–700. doi: 10.1111/j.1525-1594.2008.00595.x. [DOI] [PubMed] [Google Scholar]
- 126.Sherman W, He KL, Yi GH, et al. Myoblast transfer in ischemic heart failure: effects on rhythm stability. Cell Transplant. 2009;18:333–341. doi: 10.3727/096368909788534933. [DOI] [PubMed] [Google Scholar]
- 127.Ye L, Haider H, Sim EK. Adult stem cells for cardiac repair: a choice between skeletal myoblasts and bone marrow stem cells. Exp Biol Med (Maywood) 2006;231:8–19. doi: 10.1177/153537020623100102. [DOI] [PubMed] [Google Scholar]
- 128.Lafreniere JF, Caron MC, Skuk D, Goulet M, Cheikh AR, Tremblay JP. Growth factor co-injection improves the migration potential of monkey myogenic precursors without affecting cell transplantation success. Cell Transplant. 2009;18(7):719–730. doi: 10.3727/096368909X470900. [DOI] [PubMed] [Google Scholar]
- 129.Mikhail Konoplyannikov M, Jiang S, Ahmed R, Ashraf M, Haider HK. Reversal of ischemic cardiomyopathy using reprogrammed skeletal myoblasts overexpressing multiple therapeutic growth factor genes. Circulation. 2009;120:S773–S774. [Google Scholar]
- 130.Beauchamp JR, Morgan JE, Pagel CN, Partridge TA. Dynamics of myoblast transplantation reveal a discrete minority of precursors with stem cell-like properties as the myogenic source. J Cell Biol. 1999;144:1113–1122. doi: 10.1083/jcb.144.6.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]; ┐ Demonstrates the dynamics of SM transplantation.
- 131.Winitsky SO, Gopal TV, Hassanzadeh S, et al. Adult murine skeletal muscle contains cells that can differentiate into beating cardiomyocytes in vitro. PLoS Biol. 2005;3:e87. doi: 10.1371/journal.pbio.0030087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Okada M, Payne TR, Zheng B, et al. Myogenic endothelial cells purified from human skeletal muscle improve cardiac function after transplantation into infarcted myocardium. J Am Coll Cardiol. 2008;52:1869–1880. doi: 10.1016/j.jacc.2008.07.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sim EK, Haider HK, Aziz S, Ooi OC, Law PK. Myoblast transplantation on the beating heart. Int Surg. 2005;90:148–150. [PubMed] [Google Scholar]
- 134.Biagini E, Valgimigli M, Smits PC, et al. Stress and tissue Doppler echocardiographic evidence of effectiveness of myoblast transplantation in patients with ischaemic heart failure. Eur J Heart Fail. 2006;8:641–648. doi: 10.1016/j.ejheart.2005.12.004. [DOI] [PubMed] [Google Scholar]


