Abstract
The Theory of Planned Behavior (TPB) served as a framework for analyzing focus group transcripts (N = 43) focused on parents’ perceptions of the challenges of ensuring their children eat a healthy diet. The results suggest that parents consider their beliefs and behaviors as individuals within a society, within families, within cultures, as inheritors of family traditions, and as parents who influence or fail to influence the attitudes and behaviors of their children. The results showed the particular salience of factors related to the TPB concepts of perceived norms and control. Approaches to building theory-driven nursing interventions are suggested.
Keywords: Obesity, Overweight, Intervention, Focus groups, Parents, Theory of planned behavior
TEN YEARS AFTER obesity was declared a global health epidemic by the World Health Organization (1998), nearly one in three U.S. adults is obese. The percentage of U.S. children who are overweight or at risk for becoming overweight is even higher (Ogden et al., 2006). Overweight and obese children are at a higher risk for coronary heart disease (Freedman et al., 2004), asthma (Belamarich et al., 2000; Visness et al., 2009), and Type 2 diabetes (Fagot-Campagna et al., 2000). They are as much seven times more likely than healthyweight children to be obese as adults (Must et al., 2005). They are more vulnerable to low self-esteem and depression and are more likely to face societal stigma (Estabrooks & Shetterly, 2007; Latner & Stunkard, 2003; Pierce & Wardle, 1997; Schwartz & Puhl, 2003; Wallace, Sheslow, & Hassink, 1993). As a result of this epidemic, pediatric nurses increasingly are confronted with the need to address weight-related issues in consultations with parents and caregivers. Broaching weight-related concerns with parents, however, can be challenging because parents often are hesitant to recognize that their own child is overweight or obese (Towns & D’Auria, 2009). As a result, nurses may find themselves negotiating parents’ perceptions and boundaries as they try to offer counseling about a child’s weight.
To help with these counseling challenges, research is underway to isolate the physical and social causes of the obesity epidemic and begin designing health promotion activities and interventions that can help practitioners, parents, and children address weight concerns more successfully. For example, research suggests the promise of interventions that contain a substantial family-behavioral component (Golan & Crow, 2004; Golan, Weizman, Apter, & Fainaru, 1998; Young, Northern, Lister, Drummond, & O’Brien, 2007). Such interventions acknowledge that parents can exert control “over foods purchased and made available to children and meal planning and preparation” and are more likely to produce results that are maintained over follow-up intervals (Young et al., p. 247). Thus, one potential strategy for fighting obesity in children and adolescents is to develop health promotion interventions that improve parents’ capacities for managing their children’s diets. However, before such a strategy can be implemented effectively, we need a better understanding of parents’ perceptions of the barriers they face. A limited body of research has begun isolating those barriers. Among the barriers to surface are a perceived lack of (a) school-based support, (b) positive messages that do not build on weight-related stigmas, and (c) health education tailored to cultural realities and family dynamics (Goodell, Pierce, Bravo, & Ferris, 2008; Styles, Meier, Sutherland, & Campbell, 2007).
Our research study builds on the above efforts by continuing to identify specific beliefs that shape parents’ perceptions of the challenges they face in providing their children with a healthy diet. The Theory of Planned Behavior (TPB) served as the framework for culling relevant beliefs from detailed focus group transcripts. Our driving research questions were twofold: (a) Is TPB an appropriate theory for exploring the beliefs that drive parents behaviors related to their children’s diets? (b) If so, what specific beliefs surface most consistently across individuals? The TPB was chosen for its emphasis on the influence of aggregate beliefs on intended and actual behaviors and because it adds a much-needed theoretical component to the literature on parents’ perceptions of the challenges they face (Adams, Harvey, & Brown, 2008; McGarvey et al., 2006; and Styles et al., 2007).
Theory of Planned Behavior
The health communication and behavior literature contains a substantial body of research focused on the key motivating factors in health-related behaviors (Armitage & Conner, 2000; Glanz, Rimer & Viswanath, 2008). Across behaviors and contexts, TPB surfaces as one of the most generalizable theories (Ajzen & Manstead, 2007; Conner & Sparks, 1996; Godin & Kok, 1996; Werner, 2004). TPB has been used to predict behavioral intentions and account for notable variance in the performance of health behaviors ranging from breast self-examination (Mason & White, 2008) to binge drinking (Cooke, Sniehotta, & Schüz, 2007) to adherence to malaria treatment (Farquharson, Noble, Barker, & Behrens, 2004).
TPB was developed to map determinants of human behavior (Ajzen & Fishbein, 2005; Ajzen, 1988, 1991, 2002). In sum, TPB depicts behavior as guided by three distinct but interrelated macro concepts: (a) behavioral beliefs, (b) normative beliefs, and (c) control beliefs. Behavioral beliefs relate to the perceived outcomes of the target behavior and evaluations of those outcomes; normative beliefs relate to one’s perceptions of others’ expectations regarding the behavior and one’s motivation to respond to those expectations; and control beliefs refer to perceptions regarding factors that work against or facilitate the behavior.
Ajzen (2002) suggests that “behavioral beliefs produce favorable or unfavorable attitudes towards the behavior; normative beliefs result in perceived social pressure or subjective norms; and control beliefs give rise to perceived behavioral control, the perceived ease or difficulty of performing the behavior” (p. 665). Perceived norms are generally manifested as the perceived expectations of, or pressures from, important others such as family and friends. For the purposes of our research, we extended the definition of norms to embrace self-identity related to norms such as perceived roles and role expectations within the family. These perceptions have proven influential in TPB-based investigations of consumer and food-related behaviors (Smith et al., 2008). Perceived control can be manifested as internal control (or self-efficacy) and external control (which is the result of factors outside of one’s own control). These aggregate factors contribute to behavioral intention, which contributes to the actual performance of the behavior.
Although TPB has long guided efforts to predict and explain health behavior (Ajzen & Manstead, 2007), there has been increasing interest in using it to design interventions. Hardeman et al. (2002) reviewed 24 such interventions, which included target behaviors such as practicing testicular self-examination (Brubaker & Fowler, 1990) and improving dental health (Tedesco, Keffer, Davis, & Christersson, 1993). According to Ajzen and Manstead, TPB is a useful tool for designing interventions “provided the necessary preliminary research has been carried out” (p. 51). Ajzen (2006) asserts that only through pilot work can researchers understand beliefs fully enough to design interventions.
Looking at parenting and child behavior specifically, there has been some TPB-related research on the topic of smoking. This research suggests that in addition to TPB concepts, parents’ behaviors (in this case smoking) were among the strongest predictors of adolescent smoking (Harakeh, Scholte, Vermulst, de Vries, & Engels, 2004). There has also been a limited amount of research that looks at TPB related to healthy eating. One such study suggested beliefs and attitudes are strong predictors of the consumption of fatty foods, more so than knowledge about the adverse effects of such foods (Shepherd & Towler, 2007). Another study suggested that TPB serves as a good predictor of behavioral intentions when it comes to healthy eating (Povey, Conner, Sparks, James, & Shepherd, 2000) but does not offer specific beliefs or factors that might resonate with potential audiences. For example, Povey et al. suggest that researchers must now turn their attention to the “social influence variables” that contribute to health behavior (p. 1004). Those variables are the focus of this current effort. The purpose of this pilot research effort was to better explicate and understand these social influence variables. Questions that guided this exploration included who in the family was responsible for ensuring that the children eat well, what challenges parents faced with this responsibility, and how cultural factors or traditions might be impacting the family’s efforts. The overarching intent of this exploration is to provide the field with pilot data to guide the development of more effective nursing interventions for addressing the pediatric obesity epidemic.
Method
Procedure
A qualitative research design using focus groups guided by Krueger and Casey (2000) was used to conduct this study. A series of six focus groups was conducted with parents in a midsized city in the southwestern United States. The purpose of the focus groups was to explore the nutritional challenges parents face in raising their children, as well as perceptions of a pilot Web site (data related to the Website are reported in Mackert, Kahlor, Tyler & Gustafson, 2009). Focus group recruitment, facilitation, hosting, moderation, taping, and transcription were all handled through a research office housed in the authors’ home university. The focus group protocol and participant consent form were approved by the relevant institutional review board. The number of focus groups was limited to six as a result of funding constraints and difficulties recruiting participants; however, consistent with Krueger and Casey (2000), we were able to facilitate three focus groups per gender type (three female parent groups and three male parent groups).
Sample and Setting
Recruitment methods included posting flyers in community centers and advertising in the city’s weekly newspaper and on the city’s Craigslist classifieds Web site. To assist in recruiting African American males specifically, team members visited barbershops that cater to African American clientele. To be eligible, participants had to be parents, 18 years or older, at or below the median income for the area ($53,209 per year), and with no more than a few years of college (and therefore no 4-year degree). All focus groups met on evenings during the week in rooms designed specifically for focus groups (e.g., comfortable seating and lighting, refreshments and restrooms conveniently available). At the end of the focus groups, each participant was compensated $75.
Each group was moderated by the same individual in English using a semistructured, open-ended protocol. The moderator was a professional employed by the research office with extensive experience in focus group facilitation. Given the goals for this study, when designing the moderator’s script and prompts, we sought to concentrate on the following issues related to nutrition: who in the family is responsible for the children’s diet, difficulties faced in making sure children eat right, success of related efforts/tactics, family pressures, whether media messages seem to matter, and whether work schedules were relevant. These issues had been identified in earlier research as important to parents (Styles et al., 2007). The resulting discussions, which were each approximately 90 minutes, were audiotaped and transcribed.
Data Analysis
The unit of analysis for this study was each block of text in the portions of the transcripts that followed nutrition-related prompts. Textual blocks were created during transcription to indicate a shift in speaker; the resulting units ranged from a few words to a full paragraph. In total, our sample included 403 response units.
Analysis of these units proceeded in two phases. The first phase of analysis was a directed content analysis consistent with methods outlined by Krippendorff (2004). This allowed the researchers to isolate emergent themes (which we refer to as factors) that were prevalent in the response units and consistent with core TPB constructs. The second phase of data analysis involved basic quantitative analysis—specifically, tallying the presence of the factors that had emerged.
In the first phase of the analysis, two of the researchers (the first and third authors) independently read the data. Each of the two researchers then generated a list of the factors that respondents perceived as impacting their efforts to ensure their children ate well. To help guide this initial phase of the analysis, the researchers were directed to account for factors related to all three TPB concepts. After generating their independent lists, the two researchers then met to identify common factors and collapse those factors into a single document that could serve as a code guide for further analysis. Factors that did not appear on both lists were discussed further; two were added to the master list, and the remainder was rejected. The final selection of factors was consistent with Ajzen’s (2006) guidelines for operationalizing TPB concepts. The final list was further reviewed by a third member of the research team (the second author). A conceptual representation of the final list is offered in Figure 1, a Venn diagram that shows how the factors fall into distinct TPB concepts, yet are not mutually exclusive. Indeed, if one were to categorize the responses according to this Venn diagram, many would fall within the center segments of the diagram.
Figure 1.
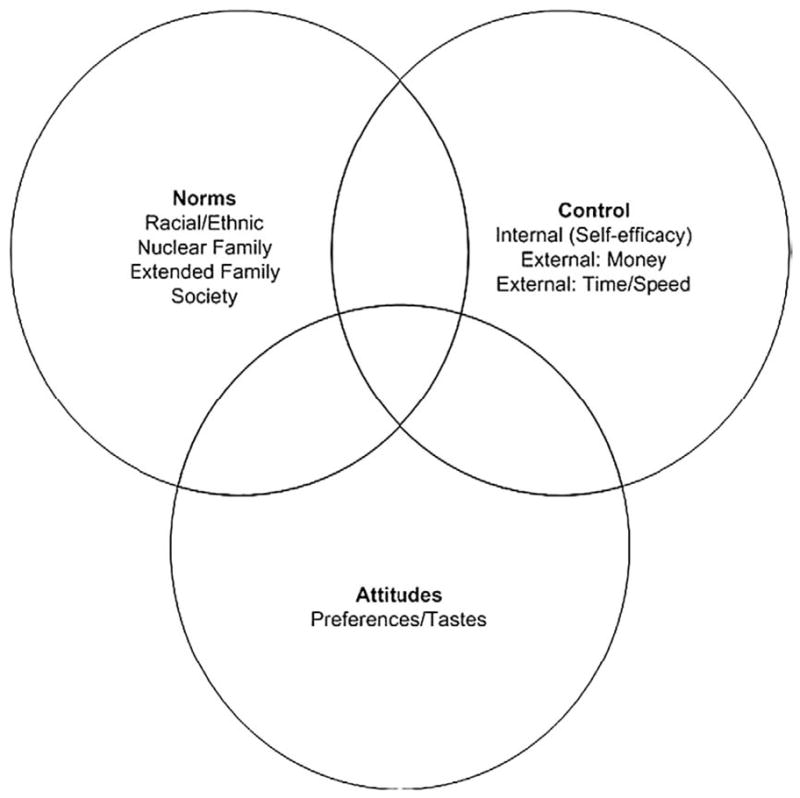
Factors impacting parents’ perceptions: a typology based on TPB.
The second phase of data analysis involved quantitatively measuring the presence of these factors in the units. Using the code guide that emerged above, the same two coders were directed to note the presence of any of the above factors in each unit. A unit could contain multiple factors. However, coders were also asked to only code an individual factor once per unit (e.g., even if racial norms appeared more than once in a unit it would only be coded once). In the case of race/ethnicity, coders were asked to not code the presence of those factors merely because the respondent used Spanish words or named a Mexican food. Coders were also directed to not include units that contained only filler words or incomplete thoughts such as “I’m…” or one-word questions asking for clarification such as “Yeah?” To determine intercoder reliability for the quantitative analysis, the coders analyzed a randomly selected subsample of 47 units. The subsample size is consistent with Lacy and Riffe’s (1996) recommendations for intercoder reliability checks. The reliability check yielded acceptable reliability statistics for all eight factors—Krippendorff’s alpha ranged from .80 to 1 (Krippendorff, 2004). The remaining 356 units were split among the two trained coders who had achieved reliability (178 each). The results reported below reflect all 403 units. Once all the data had been coded, we also ran analysis of variance and means tests to determine if there were differences by gender and/or ethnicity as each related to the three TPB factors.
Results
Each focus group consisted of individuals of the same gender and ethnicity/race to help ensure participants would feel comfortable discussing issues that might vary based on gender, ethnicity, race, or related cultural dimensions. Race and ethnicity appear to be a factor in the obesity epidemic, with Hispanics and non-Hispanic African Americans at higher risk for obesity than non-Hispanic Caucasians (Ogden et al., 2006). Therefore, the focus groups consisted of African American mothers (n = 7) and fathers (n = 3, n = 6), Hispanic mothers (n = 8) and fathers (n = 6), and Caucasian mothers (n = 7) and fathers (n = 6).
As described above, aside from being parents, the participants (N = 43) were 18 years and older (M = 43, SD = 10.6). The participants’ reported that their children ranged in age from 5 months to 36 years. Some participants also had grandchildren. The children did not have to be living with the participant at the time of the focus group. Nearly 70% of the participants had some college (53.5%) or had completed a 2-year college program (16.3%). The remaining participants were high school graduates (25.6%) or had at least some high school (4.7%). Less than half (39.5%) of the participants were married; the rest were single (23.3%), living with a partner but unmarried (18.6%), divorced (14.0%), separated (2.3%), or widowed (2.3%).
In sum, within the 403 units, 4.2% of the units (17 of 403) contained none of the factors listed in Figure 1, 21.1% contained one factor, and the rest contained multiple factors (M = 2.64, SD = 1.48, range = 0–7). Within the 386 units that contained one or more factors, attitudes were present in 171 units, subjective norms were present in 313 units, and perceived control was present in 288 units. Ajzen (1991) suggests that although these three concepts are theoretically distinct, they covary and could be collapsed under a single concept (behavioral disposition); indeed, the results of this study suggest considerable overlap.
Our analysis of variance and means tests suggest that men were more likely than women to mention attitudes related to taste and preference, F(1, 402) = 9.65, p < .01, and less likely to invoke norms, F(1, 402) = 13.41, p < .001, or issues of control, F(1, 402) = 8.76, p < .01. In terms of ethnicity, the results suggest that African Americans were the least likely to mention control, whereas Hispanics were the most likely to mention it, F(2, 402) = 7.26, p < .01. Hispanics were also the most likely to mention norms, whereas Caucasians were the least likely to mention norms, F(2, 402) = 8.32, p < .001. The results also suggest that there were no significant differences for ethnicity by attitude F(2, 402) = 2.43.
The following section discusses the presence of each factor across the sample and offers examples of each. These results are framed qualitatively and joined with a narrative that offers observations made by the researchers as they read and analyzed data. The results are first grouped by TPB concept and then by the factors that emerged related to those concepts. Next, the factors are revisited and pieced together so the reader can see how they played out in unison in some of the more complex response units.
Attitudes Toward Healthy Eating
As mentioned above, attitudes were in evidence in 42% (171 of 403) of the response units. Attitudes were coded as present in a response if it contained at least one explicit reference to food-related taste(s) and/or preferences—whether positive or negative. In terms of healthy eating, respondents rarely expressed positive attitudes directly, but they frequently expressed negative attitudes toward unhealthy eating.
Attitudes were often revealed within the context of family relations, sometimes as points of conflict or affirmations of relationships. One husband said his wife “thought that [he] hated the way she cooked because [he] didn’t gorge out on a lot of food.” Some parents simply identified their children’s food preferences. Positive attitudes toward cooking also came up. One father explained, “With me, every chance I get to see Sam, my daughter, I love to cook.” A mother echoed that statement in relation to her daughter: “I love to cook and she’s picking up on it.”
Fast food was another frequently referenced topic. The belief that children favor fast foods was salient: “They like the little boxes, the juice boxes,” “the only thing that he likes is fast food,” and “the kids, they like the fast food.” Parents were overwhelmingly negative about their children’s preferences for fast foods, about fast foods in general, and about their spouses’ tendencies to indulge their children’s desire for fast food. A mother, who disapproved of her husband indulging their child’s appetite for fast food, complained their child consequently “gets upset when she doesn’t get McDonald’s.”
Subjective Norms Related to Healthy Eating
Norms relate to perceived expectation or pressures felt from important others (friends, family, coworkers, nurses, doctors, and so on). In this context, which emphasized parenting, norms were expected to relate primarily to family and roles within the family. Normative beliefs were evidenced in 78% of the response units (313 of 403). The factors that were coded to capture these normative beliefs were nuclear family (including domestic partners and stepchildren), extended family (including the respondent’s own parents), race/ethnicity, and societal factors such as “society,” the media, restaurants, and schools. Norms were coded as present in a unit if one or more of these factors were noted. These factors were not mutually exclusive. Within the 313 units that contained evidence of normative beliefs, 243 contained a reference to nuclear family, 99 contained a reference to extended family, 29 contained a reference to race/ethnicity, and 97 contained reference to societal factors.
Nuclear Family
Nuclear family was the most salient context for normative beliefs. When talking about their nuclear families, parents often reflected on influence and roles, and related conflicts. (Sometimes the nuclear family was also the context for control beliefs, suggesting that parental roles and parental control are deeply intertwined—this will be touched on later.) One mother explained the normative influence parents have on their children this way: “A lot of it has to do with examples that we as parents set…because that’s the environment that they know.” Parents sometimes expressed awareness of their roles as influencers: “If I had been more adamant about it when he was younger, I think he’d have a lot better eating habits now,” a mother lamented. Roles of spouses were sometimes expressed matter-of-factly: “mom does the cooking,” “my wife takes care of the food,” and “I buy the food.” However, participants also said responsibilities for healthy eating are shared in their families (“I think my husband and I split it pretty well”), which reflects family norms in terms of shared roles.
Spousal conflict emerged when both men and women identified having competing roles as enforcers of good eating practices or enablers of bad eating practices or when role expectations were violated. These conflicts seemed less a result of traditional gender roles than the dynamics of individual families, where one spouse indulges their child’s sweet tooth and the other assumes the role of enforcer or denier. “They know to go to momma if they want to go to the candy store,” a father said. A mother similarly explained, “[My daughter is] like, ‘My daddy gave it to me.’ and I’m like, ‘I know your daddy gave it to you, but Mommy is not going to let you have it.’” That sentiment was echoed by another mother: “Daddy pumps them up with the sugar and Momma puts them to bed.” Such comments also relate clearly to perceptions of control and control-related struggles, suggesting that spousal relations is a key area to explore for better understanding the dynamics of normative and control beliefs in the healthy eating behaviors of families.
Interestingly, parents revealed that children sometimes play a positive role in shaping the family’s eating norms. One mother explained that her 8-year-old daughter is “very conscious…telling us, ‘no, that’s not healthy.’” Another parent described her 9-year-old daughter as a “health nut” who “encourages” other family members. Other parents said their children were involved in food preparation.
Extended Family
Another common theme within normative beliefs was the role of extended family in the eating norms of nuclear families. Some parents said they felt pressure to eat poorly when in the presence of extended family. One father said his extended family finds his buying organic chicken and milk “disrespectful.” Others mentioned feeling obligated to eat “all this food” at family gatherings where there is pressure not to “cook short…so it makes you overcook.” Another said that when around “in-laws or your family, they are always, ‘Oh, it won’t hurt [the children]—just let them have it.’” One mother complained of being criticized for “overreaching” when resisting such pressures. In addition to grandparents, others were cited as having a role. One mother explained, “I’ll take my kids to their uncle’s home, my brother’s house. They’ll eat chips, sodas all day long, candies.” Another mother said, “My sister is the same way. My kids will go to her house and from the moment we walk in the door, ‘what do you kids want to eat?’”
Subjective norms within extended families also emerged as the product of generational difference rather than family roles or relationships:
My kids are after me all the time. They say I eat too much meat. They are right. Partially, that’s the way I was raised. When I was a child, my parents believed that protein was a major part of nutrition. That’s no longer true.
Another father said his mother called him “a kook” after telling her he was on a “vegetarian diet.” Until he “learned otherwise,” he explained, he too once believed in “her concept” of healthy eating.
Parents also had positive things to say, although less frequently, about getting support from extended family. One father explained that his parents “respect” his nuclear family’s choice to avoid meat, “so it’s not a problem.” A mother said “it took that extra support” from extended family to make changes to “our menu,” without which “it probably wouldn’t have happened.” That same mother also recognized how her sister’s focus on “health and nutrition” helped them “all realize so much more” about their diet.
Race/Ethnicity
As noted earlier, race and ethnicity arose solely in the context of social norms, which was only in about 7% of the response units. For example, one father said, “Hispanics, we do a lot of parties, a lot of fiestas. A lot of food.” Another member of that group concurred, “I think food and Hispanic culture goes hand in hand, regardless of whether some of us want to eat healthy or not.” In the African American female group, one woman remarked that “Black people love fried foods.” However, another woman in the same group suggested that that norm can be changed: “If you are like me and you are living in a predominantly black neighborhood…there was a time when we ate all the greasy foods, the fried foods, the fatty foods.” She went on to explain how she had been able to add more vegetables to her family’s diet despite those cultural norms. Conversely, a Hispanic father explained how living in Mexico, as opposed to the United States, facilitated a healthier diet: “Basically we grew up with a lot of vegetables and a lot of fruits.”
References to race and ethnicity also came up in the context of body image for African American women. One African American mother told the group how her 17-year-old daughter is unhappy with her body: “She’ll go all day without eating anything and just drink apple juice. She’s thinking I have to have this certain body, this image.” Another mother in the group raised similar issues: “I went through that with my two daughters who are big boned and they didn’t think they looked how you are suppose to look.”
Society
Normative beliefs were also expressed in reference to larger societal influences such as the presence of fast food (and convenience foods) and mass media. Despite parents’ negative attitudes about their children’s preferences for fast food, they perceived a strong pressure on themselves, their families, and their children to eat fast foods or accept the eating of fast foods as normative practice. Comments such as, “Our fast paced society is geared to fast food,” “we are definitely a fast-food nation,” and “the opportunity to eat poorly is everywhere” demonstrated the belief that fast food is a ubiquitous and influential component of American life and culture. McDonald’s was invoked far more frequently than any other fast-food chain. In one example, a parent stated, “ he is at an age right now where he is interested in the toy, and the toy is what is basically driving him to McDonald’s.” On this topic, some comments suggest parents believe that the pressure to eat McDonald’s is reinforced by a matrix of subjective norms that involve children’s food tastes, family norms, and media and advertising: One mother said her “daughter and her husband are influenced” by “the overall culture, media, McDonald’s, fast food, T.V… Kids, they want McDonald’s, quick, fast, and in a hurry.” Other parents believe that “advertising for fast food and junk food” has a “big effect if you let your kids watch a lot of TV.”
Control Beliefs About Healthy Eating
Control beliefs were present in 72% of the response units (288 of 403), making it the second most common TPB construct to emerge in the responses after subjective norms. The control factors were coded via internal control (self-efficacy), external control related to money, and external control related to time. Control was noted in a unit if one or more of these factors were present. These factors were not mutually exclusive. Internal control was the most common variable to emerge (244 of 288), followed by external control related to money (56 or 288) and time (46 of 288). As mentioned above, the control factors and normative factors were often intertwined such that one phrase contained evidence of both. This overlap will be discussed in more depth later.
Internal Control
The topic of self-efficacy came up in many different contexts and in reference to how parents guide their families’ healthy eating behaviors. Self-efficacy was sometimes invoked when parents explained their agency in determining food choices. A mother recounted how she takes action against her daughter’s sweet tooth: “No more candy,” she tells her. “I’m putting it up high. You are getting no more candy.’” Another mother explained how she controlled her infant son’s diet: “I didn’t give him the fruit first. I started giving him vegetables because I was told that [if you give them fruit]…they are going to want sweets.” One father explained that when his children are with him, “they eat what I eat.” Parents sometimes touted their resourcefulness as food providers as a point of pride and self-empowerment: “I will make you a meal that they serve in a five star restaurant out of whatever is in your cupboard.” A father said, “In my backyard, I started growing a garden…it feeds them better and it makes me feel better.” Claims such as, “I think I instilled that,” “I had to teach my daughter better eating habits,” and “you just do it” are other examples of self-efficacy. However, parents also admitted their influence was not always positive: “I’m usually the corruptor,” said a mother, and a father explained how his own food preferences “make it really hard” to affect his children’s diets positively.
Money and Time
The most salient perceptions of external control were limited time and money. The comment, “without time and money, forget it,” sums up the common belief that parents simply lack the time to prepare healthy foods or the money to buy them:
I wish I had the time. I work 6 days a week…So it’s really challenging to be able to go to the grocery stores that are healthy [and purchase food] that you can make really quick that don’t cost a lot of money.
The quote below is another good example:
It’s hard to find nutritious food that is quick and healthy. Like in my case I’m a full-time student and I work and with my kids in swimming…you come home, it’s late. The best thing is to pop in a frozen pizza.
Parents conveyed a sense of helplessness in the face of such constraints, giving in to the temptation of “quick, easy dinners” or “fast food” when healthy alternatives are perceived to be too time consuming. As these comments reveal, parents perceive “working long hours” and having “hectic … hours all over the place” as barriers to eating healthier diets. Parents also view healthy food as prohibitively expensive, whereas unhealthy foods were viewed as the only alternative because of the perception that they are invariably less expensive. Some examples include the following: “The fruits and vegetables at the store are outrageous,” “good nutrition is going to cost you more than the other frozen meats and hotdogs, and white bread,” “it’s difficult to eat well when you have financial issues…and the cheapest thing is…pork chop, ground beef,” “a gallon of milk at [the grocery store] may be $3.75, but for a gallon of organic milk it like $5.39.”
Interplay Among Factors
Although the above factors could be coded independently, still more insight comes from how these factors often surfaced simultaneously and in mutually reinforcing ways. For example, in many cases, spousal relations were viewed as both subjective norms and control beliefs. Some participants said their ability to get their children to eat healthier was restricted by either their spouse’s behavior or by their own perception of the social norms governing their roles and responsibilities as domestic partners or as husbands and wives. One husband, for example, expressed reluctance to confront his wife about needing to change the diet for their child “because the whole idea of being in a marriage and trying to support and trying to get used to how she was brought up, how she was raised to eat.” This unit invokes nuclear family norms (his wife and children, marriage), extended family norms (how she was raised), and self-efficacy (trying to support his wife). As a result, this husband expresses a degree of confusion about his choices that could lead to a diminished sense of self-efficacy.
Another complex relationship to surface was that between attitudes and control in parents’ views that children tend to dislike healthy foods. In some cases, children’s food tastes were viewed as innate. One mother explained that although her son’s “palette is such that everything tastes good to him,” her daughter’s “palette is such that she has never liked anything green.” Another mother discussed how her efforts to slow her son’s natural affinity for sweets were thwarted by her mother-in-law. Although this unit was excerpted above, it is offered in entirety here:
When I was first introducing foods to my son…I started giving him vegetables because I was told that giving them the fruit has more of a sweet taste to it so they are going to want sweets more than they are going to want their food. I was brought up dinner first, then sweets come next, because they spoil the appetite or they don’t want to eat the dinner. My mother-in-law was always “he can have it, it’s fine. He’ll be ok.” No he’s not. I didn’t like the fact that she did that. She should respect that.
The presence of attitudes (wanting sweets), nuclear-family norms (mother–son relationship), extended-family norms (mother-in-law), and control (the mother describes her self-efficacy) shows a complex web of factors at play. In addition, there is an implication that the mother-in-law’s beliefs about healthy eating may be a barrier the mother must confront on an interpersonal level and within the dynamic of nuclear- and extended-family relationships.
Sometimes parents sympathized with extended family members’ attempts to “help” despite the fact that it often works against parents’ intentions and sense of self-efficacy. One father’s narrative illustrates this complexity and its demands on spousal negotiation:
So Mom will walk in and say “what are you feeding, bread? Why you feeding tortillas? He needs to eat vegetables.” And then her mother comes out and says “look at this guy. He needs a piece of steak,” you know?…In that situation, my wife, my self, we just put that on the side. and that was just for the kids, for the health of the kids…So we had to talk about it and say you know we just have to ignore that.
Other parents who described ways of resisting such pressure still complained of its prevalence and the difficulty of dealing with it. One mother said it is socially awkward to decline unhealthy food when offered to her children because “you still have to follow social rules for being nice and saying thank you when someone gives you something.”
Another factor that demands attention for its presence across beliefs and constructs is fast foods. Parents complained that fast food is a barrier because children have such a strong appetite for it and such a strong resistance to healthier alternatives; fast foods are inexpensive and accessible, and parents may have to confront family norms that deem fast foods acceptable. A mother’s narrative illustrates some of these dynamics:
[My daughter says] “Let’s go to McDonald’s.” and I’m like “no,” I’m like “you are going to sit here and you are going to eat your dinner here.” “No my daddy is going to take me to McDonald’s and I’m going to get a toy.” and I’ll be like, “no you have tons of toys here. You don’t need to go to McDonald’s.” Then she’ll start crying and stuff.
Another parent questioned whether it is “worth the fight” to resist her kids’ demands. Those who did express some degree of control typically acknowledged the difficulty of rebuffing children’s demands or the perception of easy access: “My kids and I seldom ate out and seldom ate fast food, which doesn’t mean they didn’t want it or ask for it all the time…It would have been nice to have fewer McDonald’s around for them to beg to go to. The prevalence is overwhelming.”
Ethnicity and culture also surfaced in combination with lack of control due to time, self-efficacy, and norms related to the nuclear family. As one mother explained:
That’s another thing Black people do, they sit back and say “oh it’s hard, I can’t do it. Show me how to do it.” You just do it. I’m a single mother of five, full-time student, and I work without getting paid. I work to pay my childcare. And we are eating at home as a family almost every night at the table.
This relationship between normative beliefs about eating and time and money frequently overlaps with family eating traditions that participants inherited and later passed on as parents of their own families, whether or not race or ethnicity was explicitly mentioned. One participant said that when she was a child, her mother sometimes had to feed a “family of six” on a budget of $25 for the entire week. As a consequence, she remarked, “you surely were not getting fruits and vegetables.” The excerpt below also suggests how lack of money can shape family norms:
We had to feed 9, 10 people on my dad’s salary. So it was always about what was cheap. Well it’s cheap to make tortillas. It was cheap to make arroz and frijoles…I don’t think I knew what nonground beef was until I was a teenager.
Some participants showed a sense of pride in the accomplishment of feeding a family with very limited means. One mother reveals this pride in her ability to feed many children with few dollars.
If you’ve got four children and you are trying to raise them and even though you may have a two-income family, you’ve got bills, you make too much for any assistance, you don’t make enough for assistance you may need. So that’s why I was called the queen of the one-pot meals.
The heroic ability to feed children on a tight budget could sometimes be seen to transcend the question of whether the diet was healthy. One participant reflected that her mother’s ability to feed her kids was an act of love: “for my mother, she didn’t work; she didn’t make her own money. That’s what she could give to her kids…was enough food to satisfy you.” Another parent responded to that point but took it in a different direction: “I think those are foods we all grew up with and we associate with comfort and love, but to be able to cook it in a healthier way and still maintain that tie, would be helpful.”
Discussion
Meeting the needs of families in the fight against obesity will require a range of pediatric nursing interventions designed to address a myriad of factors. Although prior research suggests parents are invaluable to the success of these interventions, we know very little about the specific areas in which parents need extra help. As a result, this research project was designed to access parents’ beliefs about the social and cultural factors that impact the challenges they encounter and the success they experience when trying to raise children with healthy diets. An important goal of this study was to accomplish the above from a more theoretical perspective than the work that preceded it (e.g., Styles et al., 2007). Therefore, this study used TPB as a framework, which we chose for two reasons: (a) it has shown great promise in the development of health-related interventions and (b) it lends itself to formative research into the beliefs that bolster or undermine healthy attitudes and behaviors. Our intent was to determine whether the theory is appropriate for this context and to identify the TPB beliefs that surfaced most consistently across groups.
Our results suggest that the theory is indeed appropriate; TPB constructs were at play across multiple relationships and contexts, and only 4.2% of the units did not contain evidence of those constructs. Furthermore, a closer look at those 17 units suggested that they typically contained questions asking for clarification (e.g., “What do you call it when they boil all the proteins out of food?”) or statements that affirmed other speakers (“That’s all you can do”), or statements that were too vague to ascertain intended meaning (e.g., “That microwave killed us all”). As a result, we did not find evidence in those units regarding shortcomings in the appropriateness of the model.
The TPB factors that emerged in our analysis touched on nuclear family relationships, extended family relationships, race/ethnicity, society in general, self-efficacy, time, money, and food preferences and tastes. Related to these factors, participants reflected on their attitudes and behaviors as individuals within a society, as individuals within families, as inheritors of family traditions, and as parents who influence, or fail to influence, the attitudes and behaviors of their children and families.
Normative beliefs, which often surfaced in conjunction with control beliefs, far outnumbered the presence of attitudinal beliefs. One potential explanation is that past communication efforts have successfully shaped positive attitudes toward healthy eating. That is, parents may not feel particularly conflicted on this point and therefore did not linger on it as often as other beliefs that were more embedded in conflict. Indeed, conflict was an important subtheme throughout the responses that touched more directly on norms and control.
Parents wrestle with many conflicts in their attempts to influence their children’s eating behaviors. For example, some participants revealed that their own health-conscious actions are often in conflict with the norms of their nuclear family, family traditions, larger sociocultural practices, and the practices they have developed to deal with their lack of time and money. These findings are consistent with previous research that has highlighted family conflicts, as well as time and money pressures, as significant challenges for parents raising healthy children (Adams et al., 2008; McGarvey et al., 2006; Styles et al., 2007). Some parents were explicit in stating that resolving familial tensions and confronting adversarial norms would require more effective coping strategies than they currently possess. Indeed, although some research has highlighted the positive role that extended family can play in raising children with healthy diets (Adams et al., 2008), these participants also focused a great deal on the challenges extended family can present.
Furthermore, the familial conflicts that surfaced repeatedly within the context of norms and perceived control were bound with both positive and negative emotions. For example, a Hispanic woman who expressed admiration for a mother who fed a large family on little money also expressed a desire for healthier alternatives to the foods her mother prepared so lovingly. Her comments resonated with another member of her group who said it would be helpful to have healthy recipes for the comfort foods they loved as children. These parents were not indicting their parents’ unhealthy choices but sought ways to bring tradition into the present—to maintain a link with the past but also address current realities. The emotional dimensions of their families’ food history appeared to be a potential barrier to adopting healthier eating practices. Future research needs to address this complex intergenerational relationship and the myriad sources of conflict that arise when parents try to address their children’s eating habits.
Most responses contained multiple factors that suggest that parents face varied pressures that are likely to shift from situation to situation (e.g., from nuclear to extended family settings). This is perhaps the most compelling area for future research. Such research might work toward identifying effective situational coping strategies and identifying the impact of shifting roles on the efficacy of those strategies as parents move from one situation to the next. Interventions could be developed to empower parents to self-identify with such pressures and develop coping skills for dealing with them. Along those lines, an appropriate intervention might be an interactive one (available online or in workbooks, workshops, or counseling) that helps parents explore and identify the personally relevant conflicts and challenges they find so difficult to resolve. Evidence suggests that interactive interventions, especially Web-based interventions, can be more effective than interpersonal consultations in educating and counseling users—especially when a condition carries with it some degree of societal stigma (Berger, Wagner, & Baker, 2005; Gustafson et al., 2005). Long-term cost effectiveness is also an important consideration when designing interventions to combat childhood obesity (Campbell, Waters, O’Meara, & Summerbelt, 2001), and there is some evidence that online interventions can reduce overall health care costs (Lorig et al., 2002). Once they have identified the most formidable challenges, the interventions can offer various strategies for resolving those conflicts and challenges. Such tailored, interactive interventions could be made available in waiting rooms to supplement the more personal nursing consultations that take place in examining rooms.
On the topic of spousal relations, intervention strategies could encourage parents to share responsibility for family diet and open dialogue about how they might influence their children’s eating behaviors both positively and negatively. Future research could explore how familial roles can be at odds (e.g., mom enforces eating rules, dad gets to break those rules) and how that tension undermines the family’s ability to adhere to a nutrition plan. Indeed, the relationship of roles within the larger TPB framework is an area that deserves additional research attention, particularly in the context of parenting. On a related theme, additional research needs to explore the impact of perceived expectations from spouses and perceptions of whether spouses feel supported in meeting the expectations they feel from others. On the topic of extended family, interventions could emphasize being positively responsive, rather than critical, to traditions and acknowledging the heroism of prior generations. This idea of the heroism of prior generations appears to be unique to research on challenges parents face raising healthy children and merits additional attention. Additional research could lead to a better understanding of this phenomenon and make it possible to leverage this concept in interventions.
Reinforcing the importance of family tradition, parents expressed feeling significant pressure from their extended families to conform to family norms and customs. The topic of family ritual as an influential factor in child health has received some attention in research on pediatric psychology (Fiese & Sameroff, 1989), but more research attention should be paid to this area, particularly in the context of family eating habits. For example, our results suggest that pursuing healthier eating practices was, at times, seen by others as a rejection of family and ethnic heritage or class identity. Therefore, responding to perceived family pressures may require nursing interventions that address these perceptions by affirming them as a significant challenge to parents; by dispelling the notion that choosing to eat healthier means rejecting one’s identity and familial loyalties; by giving parents practical language to negotiate their position; and by offering parents recipes and cooking strategies to help transition family recipes from the past to the present (Tyler, Johnston, Madhukar, & Foreyt, 2005). This could help parents maintain traditions, circumvent perceptions of disloyalty, and improve their children’s diet. Overall, with further development, such interventions could empower nurses to make meaningful connections with parents—which may open the door to acknowledging that their child has a weight problem—while also providing parents with better self-awareness and tools for respectfully managing family influences.
In addition to family norms and conflicts, another theme that surfaced repeatedly was time and financial pressures. Again, this is consistent with previous research investigating parents’ challenges raising healthy children (McGarvey et al., 2006; Styles et al., 2007). An intervention such as the interactive model described above could also help parents develop weekly meal plans based on healthy but familiar recipes and ready-to-print shopping lists for those meals. This could alleviate some of the primary concerns parents have about costs associated with improving their children’s diets. This encouragement to cook meals at home could also help avoid the potential loss of positive food preparation knowledge. These participants viewed their parents as heroic figures who fed them on tight budgets, and they spoke of the love with which their parents provided meals. At the same time, the participants lamented their own reliance on convenience foods as a notable influence on their family’s eating-related norms. As one parent pointed out, this reliance on prepared foods could result in a generation of children who lack the food preparation skills necessary to maintain family traditions and eat well. Broader research could confirm whether or not this is a widespread concern and how this might serve as motivation for parents to improve their children’s food preparation skills.
To respond to this concern, future research may need to locate ways in which nurses and other health communicators might effectively frame food preparation as a rewarding family activity. If parents view the act of preparing a healthy, balanced meal as a viable recreational option when they do have leisure time, their children could learn practical food preparation skills that would empower them as consumers and future parents. Other benefits that could motivate parents include opportunities to bond with their children through food in a way similar to their own experience as children and the simple delights of a tasty home-cooked meal. With recipes that preserve traditional meals by substituting healthier ingredients, parents could also claim solidarity with their families, ease their sense of conflicted loyalties, and proclaim themselves preservers of traditions that might otherwise perish. Indeed, effective interventions of this kind could actually generate a new cycle of generational knowledge and sharing, with grown children reflecting on their own parents’ heroic efforts raising them with a healthy diet.
Even when parents are given adequate tools to empower themselves, it would be unrealistic to expect parents alone to overcome external factors and pressures, and it would be unwise to lead them to believe that if they fail, they fail alone. Therefore, it must be acknowledged that external factors can, at times, supersede the best of intentions and/or personal efficacy. Parents who work two jobs, drive long distances to and from work, and make little money will have a harder time preparing fresh, healthy foods than families with a good income and one working spouse. For the former, cheap, fast, and unhealthy choices like McDonald’s will be more difficult to resist and will continue to be rationalized as a necessary evil. Thus, if the obesity problem is to be fully addressed, it would be remiss not to recommend that public policy efforts continue to push for increased access to healthier, low-cost foods. One example of public policy efforts would include improving meals at schools; although poor meals at schools were not a prominent theme among our respondents, this has been noted in previous research focusing on childhood obesity (Styles et al., 2007). Indeed, we were surprised that school meals did not surface more often in our focus groups. One reason for this absence may be that the local school district has made strides to address lunch quality concerns through its adherence to the Coordinated Approach to Child Health Eat Smart Program, which emphasizes low-fat, highly nutritional choices for children (McCullum-Gomez, Barroso, Hoelscher, Ward, & Kelder, 2006).
Regarding gender and ethnic differences in our results, we found that men were more likely than women to discuss attitudes related to taste and preference but less likely to discuss norms or issues of control. Additional research could help explore the reasons for these trends and isolate ways in which health promotional messages might more effectively reach fathers (e.g., more education about preparing different kinds of foods to find healthy and tasty alternatives to favorite foods). Additional research could also explore ways to better understand (and lessen) the apparent pressure on female caregivers to take control of the family diet and respond to often stressful family normative pressures. Ethnic differences also surfaced in our research and appear to be consistent with other research in this area. For example, our results suggest that Hispanic parents were the most likely to mention control issues in the focus groups. This is particularly notable because prior research (O’Dougherty, Story, & Lytle, 2006) has indicated that control is an important factor in the relationship between parenting styles and unhealthy eating, particularly among Latino families; in sum, that research shows that unhealthy eating is more prevalent among Latino families in which the parents are more controlling. Norms were also more likely to come up in the Hispanic and African American focus groups (when compared to the Caucasian groups). This finding is consistent with research that suggests that norms are an important factor in the food-related decisions among Hispanic and African American parents (Arredondo et al., 2006; Grier, Mensinger, Huang, Kumanyika, & Stettler, 2007).
Although this study was able to isolate constructive factors and subthemes within the data, this study does have limitations. As is the case with all focus group research, the findings reported here provide only a limited snapshot of the phenomena under study. For example, a study featuring additional ethnic groups would allow for a closer examination of how cultural factors might pose barriers not revealed in this study. Indeed, additional research focused on each population (by gender and ethnicity) is necessary to learn more about the most effective strategies for reaching parents who are confronting childhood obesity. All research also was conducted in the same southwestern city, and the results may not reflect the experiences of parents living in other regions or more rural areas.
Given the limitations outlined, this should be considered formative research. Although these findings are not generalizable, the themes and subthemes that surfaced in our analysis are consistent with TPB and therefore suggest ways in which the central concepts of TPB may be manifested in parents’ beliefs systems. In the very least, this effort offers insight into the myriad factors that are currently inhibiting healthy eating behaviors in the United States. Although formative research can best be judged by the pilot projects and interventions that build upon it, this work provides a foundation for future research and exploration of a range of new nursing interventions.
Acknowledgments
This study was supported by the Center for Health Promotion and Disease Prevention Research in Underserved Populations (NIH/NINR P30 NR005051, Stuifbergen, PI) at The University of Texas at Austin School of Nursing.
References
- Adams AK, Harvey H, Brown D. Constructs of health and environment inform child obesity prevention in American Indian communities. Obesity. 2008;16:311–317. doi: 10.1038/oby.2007.71. [DOI] [PubMed] [Google Scholar]
- Ajzen I. Attitudes, personality, and behavior. Milton-Keynes, England: Open University Press; 1988. [Google Scholar]
- Ajzen I. The Theory of Planned Behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the Theory of Planned Behavior. Journal of Applied Social Psychology. 2002;32:665–683. [Google Scholar]
- Ajzen I. Constructing a TpB questionnaire: Conceptual and methodological considerations. 2006 January; Retrieved March 1, 2009, from http://people.umass.edu/aizen/pdf/tpb.measurement.pdf.
- Ajzen I, Fishbein M. The influence of attitudes on behavior. In: Albarracín D, Johnson BT, Zanna MP, editors. The handbook of attitudes. Mahwah, NJ: Erlbaum; 2005. pp. 173–221. [Google Scholar]
- Ajzen I, Manstead ASR. Changing health-related behaviors: An approach based on the Theory of Planned Behavior. In: van den Bos K, Hewstone M, de Wit J, Schut H, Stroebe M, editors. The scope of social psychology: Theory and applications. New York: Psychology Press; 2007. pp. 43–63. [Google Scholar]
- Armitage CJ, Conner M. Social cognition models and health behaviour: A structured review. Psychology & Health. 2000;15:173–189. [Google Scholar]
- Arredondo EM, Elder JP, Ayala GX, Campbell N, Baquero B, Duerksen S. Is parenting style related to children’s healthy eating and physical activity in Latino families? Health Education Research. 2006;21:862–871. doi: 10.1093/her/cyl110. [DOI] [PubMed] [Google Scholar]
- Belamarich PF, Luder E, Kattan M, Mitchell H, Islam S, Lynn H, et al. Do obese inner-city children with asthma have more symptoms than nonobese children with asthma? Pediatrics. 2000;106:1436–1441. doi: 10.1542/peds.106.6.1436. [DOI] [PubMed] [Google Scholar]
- Berger M, Wagner TH, Baker LC. Internet use and stigmatized illness. Social Science & Medicine. 2005;61:1821–1827. doi: 10.1016/j.socscimed.2005.03.025. [DOI] [PubMed] [Google Scholar]
- Brubaker RG, Fowler C. Encouraging college males to perform testicular self-examination: Evaluation of a persuasive message based on the revised theory of reasoned action. Journal of Applied Social Psychology. 1990;17:1411–1422. [Google Scholar]
- Campbell K, Waters E, O’Meara S, Summerbelt C. Interventions for preventing obesity in childhood. A systematic review. Obesity Reviews. 2001;2:149–157. doi: 10.1046/j.1467-789x.2001.00035.x. [DOI] [PubMed] [Google Scholar]
- Conner M, Sparks P. The Theory of Planned Behavior and health behaviors. In: Conner M, Norman P, editors. Predicting health behavior. Buckingham, UK: Open University Press; 1996. pp. 121–162. [Google Scholar]
- Cooke R, Sniehotta F, Schüz B. Predicting binge-drinking behavior using an extended TPB: Examining the impact of anticipated regret and descriptive norms. Alcohol and Alcoholism. 2007;42:84–91. doi: 10.1093/alcalc/agl115. [DOI] [PubMed] [Google Scholar]
- Estabrooks PA, Shetterly S. The prevalence and health care use of overweight children in an integrated health care system. Archives of Pediatrics and Adolescent Medicine. 2007;161:222–227. doi: 10.1001/archpedi.161.3.222. [DOI] [PubMed] [Google Scholar]
- Fagot-Campagna A, Pettitt DJ, Engelgau MM, Burrows NR, Geiss LS, Valdez R, et al. Type 2 diabetes among North American children and adolescents: An epidemiologic review and a public health perspective. Journal of Pediatrics. 2000;136:664–672. doi: 10.1067/mpd.2000.105141. [DOI] [PubMed] [Google Scholar]
- Farquharson L, Noble LM, Barker C, Behrens RH. Health beliefs and communication in the travel clinic consultation as predictors of adherence to malaria chemoprophylaxis. British Journal of Health Psychology. 2004;9:201–217. doi: 10.1348/135910704773891050. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Sameroff AJ. Family context in pediatric psychology: A transactional perspective. Journal of Pediatric Psychology. 1989;14:293–314. doi: 10.1093/jpepsy/14.2.293. [DOI] [PubMed] [Google Scholar]
- Freedman DS, Dietz WH, Tang R, Mensah GA, Bond MG, Urbina EM, et al. The relation of obesity throughout life to carotid intima-media thickness in adulthood: The Bogalusa Heart Study. International Journal of Obesity. 2004;28:159–166. doi: 10.1038/sj.ijo.0802515. [DOI] [PubMed] [Google Scholar]
- Glanz K, Rimer B, Viswanath K. Health behavior and health education: Theory, research, and practice. 4. San Francisco: Jossey-Bass; 2008. [Google Scholar]
- Godin G, Kok G. The Theory of Planned Behavior: A review of its applications to health-related behaviors. American Journal of Health Promotion. 1996;11:87–98. doi: 10.4278/0890-1171-11.2.87. [DOI] [PubMed] [Google Scholar]
- Golan M, Crow S. Targeting parents exclusively in the treatment of childhood obesity: Long-term results. Obesity Research. 2004;12:357–361. doi: 10.1038/oby.2004.45. [DOI] [PubMed] [Google Scholar]
- Golan M, Weizman A, Apter A, Fainaru M. Parents as the exclusive agents of change in the treatment of childhood obesity. American Journal of Clinical Nutrition. 1998;67:1130–1135. doi: 10.1093/ajcn/67.6.1130. [DOI] [PubMed] [Google Scholar]
- Goodell LS, Pierce MB, Bravo CM, Ferris AM. Parental perceptions of overweight during early childhood. Qualitative Health Research. 2008;18:1548–1555. doi: 10.1177/1049732308325537. [DOI] [PubMed] [Google Scholar]
- Grier S, Mensinger J, Huang SH, Kumanyika SK, Stettler N. Fast-food marketing and children’s fast-food consumption: Exploring parents’ influences in an ethnically diverse sample. Journal of Public Policy & Marketing. 2007;26:221–235. [Google Scholar]
- Gustafson DH, McTavish F, Stengle W, Ballard D, Hawkins R, Shaw BR, et al. Use and impact of eHealth system by low-income women with breast cancer. Journal of Health Communication. 2005;10:195–218. doi: 10.1080/10810730500263257. [DOI] [PubMed] [Google Scholar]
- Harakeh Z, Scholte RHJ, Vermulst AA, de Vries H, Engels RCME. Parental factors and adolescents’ smoking behavior: An extension of the Theory of Planned Behavior. Preventative Medicine. 2004;39:951–961. doi: 10.1016/j.ypmed.2004.03.036. [DOI] [PubMed] [Google Scholar]
- Hardeman W, Johnston M, Johnston DW, Bonetti D, Wareham N, Kinmonth AL. Application of the theory of planned behaviour in behaviour change interventions: A systematic review. Psychology and Health. 2002;17:123–158. [Google Scholar]
- Krippendorff K. Content analysis: An introduction to its methodology. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- Krueger RA, Casey MA. Focus groups: A practical guide for applied research. 3. Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- Lacy S, Riffe D. Sampling error and selecting intercoder reliability samples for nominal categories. Journalism and Mass Communication Quarterly. 1996;73:963–973. [Google Scholar]
- Latner JD, Stunkard AJ. Getting worse: The stigmatization of obese children. Obesity Research. 2003;11:452–456. doi: 10.1038/oby.2003.61. [DOI] [PubMed] [Google Scholar]
- Lorig KL, Laurent DD, Deyo RA, Marnell ME, Minor MA, Ritter PL. Can a back pain e-mail discussion group improve health status and lower health care costs? A randomized study. Archives of Internal Medicine. 2002;162:792–796. doi: 10.1001/archinte.162.7.792. [DOI] [PubMed] [Google Scholar]
- Mackert M, Kahlor L, Tyler D, Gustafson J. Designing culturally sensitive technology-based interventions to help parents address obesity. Telemedicine and e-Health. 2009;15(7):672–677. doi: 10.1089/tmj.2009.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason TE, White KM. Applying an extended model of the theory of planned behaviour to breast self-examination. Journal of Health Psychology. 2008;13:946–955. doi: 10.1177/1359105308095069. [DOI] [PubMed] [Google Scholar]
- McCullum-Gomez C, Barroso C, Hoelscher D, Ward J, Kelder S. Factors influencing implementation of the coordinated approach to Child Health (CATCH) Eat Smart School Nutrition Program in Texas. Journal of the American Dietetic Association. 2006;106:2039–2044. doi: 10.1016/j.jada.2006.09.016. [DOI] [PubMed] [Google Scholar]
- McGarvey E, Collie K, Fraser G, Shufflebarger C, Lloyd B, Norman Oliver M. Using focus group results to inform preschool childhood obesity prevention programming. Ethnicity and Health. 2006;11:265–285. doi: 10.1080/13557850600565707. [DOI] [PubMed] [Google Scholar]
- Must A, Naumova EN, Phillips SM, Blum M, Dawson-Hughes B, Rand WM. Childhood overweight and maturational timing in the development of adult overweight and fatness: The Newton Girls Study and its follow-up. Pediatrics. 2005;116:620–627. doi: 10.1542/peds.2004-1604. [DOI] [PubMed] [Google Scholar]
- O’Dougherty M, Story M, Lytle L. Food choices of young African-American and Latino adolescents: Where do parents fit in? Journal of the American Dietetic Association. 2006;106:1846–1850. doi: 10.1016/j.jada.2006.08.011. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of the American Medical Association. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Pierce JW, Wardle J. Cause and effect beliefs and self-esteem of overweight children. Journal of Child Psychology and Psychiatry. 1997;38:645–650. doi: 10.1111/j.1469-7610.1997.tb01691.x. [DOI] [PubMed] [Google Scholar]
- Povey R, Conner M, Sparks P, James R, Shepherd R. The theory of planned behaviour and healthy eating: Examining additive and moderating effects of social influence variables. Psychology & Health. 2000;14:991–1006. doi: 10.1080/08870440008407363. [DOI] [PubMed] [Google Scholar]
- Schwartz MB, Puhl R. Childhood obesity: A societal problem to solve. Obesity Reviews. 2003;4:57–71. doi: 10.1046/j.1467-789x.2003.00093.x. [DOI] [PubMed] [Google Scholar]
- Shepherd R, Towler G. Nutrition knowledge, attitudes and fat intake: Application of the theory of reasoned action. Journal of Human Nutrition and Dietetics. 2007;3:159–169. doi: 10.1111/j.1365-277X.2007.00776.x. [DOI] [PubMed] [Google Scholar]
- Smith JR, Terry DJ, Manstead ASR, Louis WR, Kotterman D, Wolfs J. The attitude–behaviour relationship in consumer conduct: The role of norms, past behaviour, and self-identity. Journal of Social Psychology. 2008;148:311–324. doi: 10.3200/SOCP.148.3.311-334. [DOI] [PubMed] [Google Scholar]
- Styles J, Meier A, Sutherland L, Campbell M. Parents’ and caregivers’ concerns about obesity in young children: A qualitative study. Family and Community Health. 2007;30:279–295. doi: 10.1097/01.FCH.0000290541.02834.e0. [DOI] [PubMed] [Google Scholar]
- Tedesco LA, Keffer MA, Davis EL, Christersson LA. Self-efficacy and reasoned action: Predicting oral health status and behaviour at one, three, and six month intervals. Psychology and Health. 1993;8:105–121. [Google Scholar]
- Towns N, D’Auria J. Parental perceptions of their child’s overweight: An integrative review of the literature. Journal of Pediatric Nursing. 2009;24:115–130. doi: 10.1016/j.pedn.2008.02.032. [DOI] [PubMed] [Google Scholar]
- Tyler C, Johnston CA, Madhukar M, Foreyt JP. Practical strategies for treating obesity in Mexican Americans. Obesity Management. 2005;1:247–250. [Google Scholar]
- Visness CM, London SJ, Daniels JL, Kaufman JS, Yeatts KB, Siega-Riz AM, et al. Association of obesity with IgE levels and allergy symptoms in children and adolescents: Results from the National Health and Nutrition Examination Survey 2005–2006. Journal of Allergy and Clinical Immunology. 2009;123:1163–1169. doi: 10.1016/j.jaci.2008.12.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace WJ, Sheslow D, Hassink S. Obesity in children: A risk for depression. Annals of the New York Academy of Sciences. 1993;699:301–303. doi: 10.1111/j.1749-6632.1993.tb18873.x. [DOI] [PubMed] [Google Scholar]
- Werner P. Reasoned action and planned behavior. In: Peterson SJ, Bredow TS, editors. Middle range theories: Application to nursing research. Philadeliphia, PA: Lippincott, Williams, & Wilkins; 2004. pp. 125–147. [Google Scholar]
- World Health Organization. Obesity: Preventing and managing the global epidemic. World Health Organization Switzerland; Geneva: 1998. [PubMed] [Google Scholar]
- Young KM, Northern JJ, Lister KM, Drummond JA, O’Brien WH. A meta-analysis of family-behavioral weight-loss treatments for children. Clinical Psychology Review. 2007;27:240–249. doi: 10.1016/j.cpr.2006.08.003. [DOI] [PubMed] [Google Scholar]


