Abstract
Objectives
The study aimed to identify the important effects of some selected variables in antenatal care (ANC) seeking behaviour among slum mothers.
Methods
The data for the study were collected in 2006 from 700 mothers in the slum areas of Rajshahi City Corporation (RCC), Bangladesh.
Results
The results indicate that tetanus toxoid (TT) is relatively widespread in slum areas of RCC. Serious health implications were observed for the mothers and their children who lived in the study areas because more than half of the respondents (56.1%) were not assisted at their last childbirth by any health professional. The respondents were too poor to buy iron tablets/syrup and vitamin tablets/syrup during their last pregnancy. The application of a logistic regression model suggested that demographic and socio-economic factors were associated with ANC seeking behaviour among slum mothers.
Conclusion
Respondents’ education, place of treatment, husband’s occupation, family’s income, and exposure to mass media had highly significant effects on mothers seeking medical checkups during their last pregnancy.
Keywords: Care, prenatal, Mothers, Slums, Logistic regression, Immunization program, Tetanus toxoid, Bangladesh
Advances in Knowledge
This study found that the following demographic and socio-economic factors were associated with antenatal care-seeking behaviour among slum mothers of Rajshahi City Corporation in Bangladesh: respondent’s education, husband’s occupation, family income, and exposure to mass media.
These factors should be increased in order to boost antenatal care and reduce fertility, morbidity as well as mortality not only in slum areas of Bangladesh, but also in all underprivileged regions of the world.
Application to Patient Care
Government and non-governmental organisations should accelerate medical facilities to increase antenatal care for women in the slum area of Rajshahi City Corporation in Bangladesh.
Mass media has a great role to play in creating awareness about antenatal care among women in the slum areas as well as among underprivileged populations elsewhere.
Bangladesh is a small South Asian country which became independent in 1971 after a bloody war. Rapid urbanisation in Bangladesh (26% of the 147.1 million inhabitants live in urban areas) is fuelling a growth in urban poverty, particularly in the urban slums where the quality of life is extremely poor.1 The average population density in slums was reported in 2005 as 831 persons per acre or 205,415 people per square kilometre.2 Despite significant improvements, the maternal mortality ratio and infant mortality rate remain high (380 and 50 per thousand respectively).1
Antenatal care (ANC) is the medical supervision given to a pregnant woman and her baby starting from the time of conception up to the delivery of the baby by a physician, midwife or obstetrician or a combination of these professionals. It includes regular monitoring of the mother and her baby throughout pregnancy by a variety of routine regular examinations and tests (some routine and some for special circumstances). It also includes planning for pregnancy and continues into the early neonatal and postpartum period. Only 9% of births in Bangladesh take place at a health facility, while almost all others are home deliveries and only 55.9% of mothers receive some form of ANC.3 Ideally, all pregnant women should have regular antenatal checkups either by a paramedic or by a doctor. The Bangladesh Demographic and Health Survey (BDHS) reported that about 44% of the pregnant women, who gave birth during the five years prior to the 2004, did not receive any ANC visit, while 16.1% received only one visit. In rural Bangladesh, the majority (81.6%) of the women had only one ANC visit, while 14.6%, 3% and 0.8% had two, three and more than three visits respectively. The median gestational age at the first antenatal visit was 7 months; 74.3% of the first antenatal visits took place between the sixth and the eighth month of pregnancy. The midwife was present around the time of labour and/or delivery in the case of 3,909 (40.7%) of the women who received ANC compared to only 748 (11.1%) of the women not receiving it (relative risk = 3.73, P = 0.000). About one quarter (26.5%) of the women who received ANC experienced a labour or delivery complication, including the 21 women who died as a consequence of pregnancy.4
A study showed that the odds of having a live birth is 11.807 times higher among women who had good ANC and good health than those who lacked good health and had no ANC services.5 Another study on syphilis in the antenatal period also showed that completed treatment was significantly associated with age of gestation at first visit (P = 0.029), with women attending later in pregnancy less likely to receive all three doses of treatment.6 More recently, the potential of the antenatal period as an entry point for HIV prevention and care, in particular for the prevention of HIV transmission from mother to child, has led to renewed interest in access to and use of ANC services.7, 8
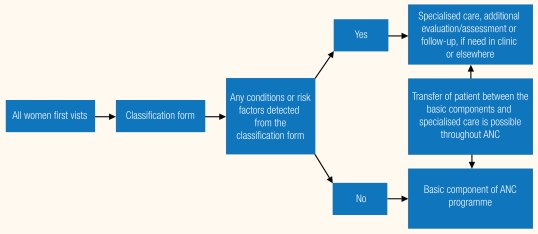
In 2001, the WHO published the conclusions of a randomised controlled trial of a new model of ANC [Figure 1] and also carried out a systematic review of other randomised trials that looked at the effectiveness of different models of ANC.9
Figure 1.
The new WHO antenatal care (ANC) model (2001)9
Pregnancy and childbirth related complications are the leading causes of maternal morbidity and mortality in Bangladesh. This exploratory study was important because it gave a picture of the state of ANC in the slum areas and will help to indicate necessary changes in customs and laws to improve existing ANC programmes with a view to reducing maternal morbidity and mortality in Bangladesh.
Therefore, the main aim and objective of this study was to determine the effects of some selected variables on ANC seeking behaviours among slum mothers.
Methods
The data for this study were collected in 2006 from 8 different slums of 3 wards of RCC, Bangladesh. Seven hundred married women, aged 15–49 years, were selected using a purposive sampling technique and took part in face-to-face interviews. Those women who had no child less than five years of age at the time of the interview were not included in this study. Taking an antenatal check-up, coded as 1 if the mothers took any medical checkup during last pregnancy or 0 if otherwise, was taken as the dependent variable in the logistic regression analysis. The following explanatory variables were considered in this study: type of births, respondent’s education, access to mass media, family’s monthly income, electricity supply in the home, husband’s occupation, household asset index, place of treatment and type of latrine. The 700 respondents were selected from 8 different slums of 3 wards, as shown in the Table 1.
Table 1.
List of selected slum areas and sample size used in this study
| No. of Slums selected | Ward No. | Slum Population | Sample Size |
|---|---|---|---|
| 2 | 28 | 7,260 | 300 |
| 4 | 29 | 7,235 | 300 |
| 3 | 30 | 2,135 | 100 |
| Total | - | 16,630 | 700 |
Legend: Ward 28: Dharompur Nadirdhar, Char Kazla Badurtola; Ward 29: Dashmari Nadirdhar, Khozapur Nadirdhar, Satbaria Nadirdhar, Shympur Nadirdhar; Ward 30: Paschim Para, Boodh Para, Mohonpur
The linear logistic regression model was employed to determine the factors associated with ANC seeking behaviour among the women in the study area and the relative effects of various characteristics on ANC seeking. The independent variables used in the logistic regression model are shown in Table 5.
Table 5.
Logistic regression estimates of regression coefficient and relative odds associated with medical checkup during last pregnancy.
| Background Characteristics | Coefficient (β) | Standard Error of β | Odds Ratio [Exp β] |
|---|---|---|---|
| Respondent’s education | |||
| Illiterate® | - | - | 1.000 |
| Literate | 0.690*** | 0.183 | 1.994 |
| Husband’s occupation: | |||
| Labourer® | - | - | 1.000 |
| Business | 0.076 | 0.297 | 1.078 |
| Service sector | 0.194** | 0.315 | 1.214 |
| Family’s monthly income: | |||
| ≤ 2000® | - | - | 1.000 |
| 2001–2500 | 0.051** | 0.555 | 1.052 |
| 2501+ | 0.388*** | 0.365 | 1.402 |
| Types of latrine: | |||
| Unhygienic® | - | - | 1.000 |
| Hygienic | 0.530 | 0.301 | 1.699 |
| Place of treatment: | |||
| Homeopathic, kabiraj and other® | - | - | 1.000 |
| Hospital and Clinic | 0.506*** | 0.169 | 1.659 |
| Type of birth | |||
| Single® | - | - | 1.000 |
| 2+ | -0.070 | 0.178 | 0.932 |
| Electricity in household: | |||
| No® | - | - | 1.000 |
| Yes | 0.758 | 0.277 | 2.134 |
| Household asset index: | |||
| Lower® | - | - | 1.000 |
| Middle | 0.350 | 0.598 | 1.419 |
| Upper | 0.581 | 0.444 | 1.788 |
| Exposure to mass media | |||
| Not exposed® | - | - | 1.000 |
| Exposed | 0.812*** | 0.472 | 2.253 |
Legend: ® = reference category;
indicate P <0.001 (highly significant);
P <0.01 (significant);
P <0.05 (less significant) respectively; Kabiraj = Bangladeshi medical practitioners without a degree in medical sciences.
The city of Rajshahi stands on the bank of the river Padma. It is basically an administrative centre having a population of 489,514 in 2005 spread over 51.3 square kilometers. There are 641 slum clusters in the city with a population of 156,793 (32% of the total city population). Most of the slum dwellers originate from the immediate vicinity of the city, and were driven to the slums by, among other things, erosion along the river Padma. The large slums are located on the left bank of the river in the city protection embankment.2
The people of Rajshahi city get health services from different hospitals like Rajshahi Medical College Hospital (RMCH), the Christian Mission Hospital, and the T.B. Hospital etc. Other general hospitals are Bangladesh Rifles (BDR) Hospital, Combined Military Hospital (CMH), and the Prison Hospital where there is no access for general public. Non-government (NGO) services addressing health issues of the poor are limited. The RCC is conducting an Asian Development Bank-Government of Bangladesh (ADB-GOB) financed project called the Urban Primary Health Care Project (UPHCP) and a United States Agency for International Development-Government of Bangladesh (USAID-GOB) financed project, the NGO Services Delivery Program (NSDP), within the RCC area with a view to improving the health of the urban poor and reducing preventable mortality and morbidity by increasing access to primary health care. These projects are run by two NGOs, namely Anannya and Tilottoma, under an agreement with RCC. The services provided by these NGOs mainly focus on maternal and infant health care, growth monitoring and feeding, supply of family planning materials etc. and take Taka 10 (= $0.143) as a consultation fee.
Moreover, the Bangladesh Rural Advancement Committee (BRAC) is one of the remarkable NGOs working for the health promotion of the urban poor in Rajshahi. The women can receive pregnancy check up services from BRAC’s health unit by paying Taka 15 (= $0.215). The RCC is also operating the City Hospital to provide preventive, curative and promotional health care services to the poor and taking Taka 5 (= $0.072) as a consultation fee.
Under the Support for Basic Services in Urban Area (SBSUA) project, RCC also provides health services to the urban poor in the form of immunisation against six Expanded Program on Immunization (EPI) diseases to children under one year of age; tetanus toxine (TT) vaccination of women aged 15–49; maternal and infant care; growth monitoring; prevention and treatment of diarrhoea etc. The slum dwellers tend not to choose government facilities as government dispensaries are probably not near their locality and they are often unaware of these facilities. Even when they have heard about government facilities, they do not know what type of treatment is provided and are not sure whether they will get the treatment they require.10 In addition, there are several private clinics, but due to their higher costs low-income people cannot afford their services. They mainly go to local, traditional, mostly untrained, but cheaper, practitioners and sometimes use NGO facilities.
Results
TETANUS TOXOID (TT) VACCINATION
The TT vaccine is given to women during their childbearing age (15–49 years) to protect them from tetanus during their whole reproductive life and their newborns from neonatal tetanus. Neonatal tetanus is a fatal disease, caused by a pathogen transmitted during or after childbirth in unhygienic delivery. A woman needs a total of five TT doses for the protection of the whole reproductive period, and these should be administered according to the following schedule recommended by WHO:11 TT1, the first dose, at the age of 15 years; TT2 four weeks or more, after TT1; TT3 six months or more, after TT2; TT4 one year or more after TT3; and TT5 one year or more, after TT4. For minimum protection, it is recommended that the pregnant women should receive at least two doses of the toxoid.12
Table 2 presents the percentage distribution of women who received the TT1, TT2, TT3, TT4, and TT5 vaccines or not between age of 15 and the data collection period. From the Table 2, we see that the proportion of women who received TT1 dose was 92.6% although nationwide the TT1 dose coverage rate is higher (95%).13 This proportion drops to 83.4 and 72.0 percent for TT4 and TT5 doses respectively [Table 2]. The data indicates that TT coverage is relatively widespread in Bangladesh. Although there has been no change in recent years in ANC coverage, the proportion of women receiving TT injections has risen substantially.
Table 2.
Percentage distribution of women aged 15–49 by TT vaccine
| Receiving TT Vaccine | Proportions Receiving Vaccine |
|---|---|
| TT1 | 92.6 |
| TT2 | 90.3 |
| TT3 | 88.0 |
| TT4 | 83.4 |
| TT5 | 72.0 |
ASSISTANCE DURING LAST DELIVERY
From the standpoint of child survival and maternal health, the first priority is a safe and clean delivery.14 Experience in both developed and developing countries shows that babies delivered under proper medical supervision are significantly less subject to health hazards. Safe delivery is an important element in reducing the health risks for mothers, especially in the case of births to younger mothers. These are often first births which carry higher risks than second, third or fourth births.15 Proper delivery with the assistance of a trained medical practitioner and hygienic conditions reduce the risk of infection and facilitate management of obstetric complications that can endanger the life of the mothers and their newborn. In this context, the respondents were asked about the assistance during their last delivery. We classified the respondents who were helped either by a health worker or nurse, or a doctor with Bachelor of Medicine and Bachelor of Surgery (MBBS), or a traditional birth attendant (TBA) or a combination of these, as ‘taking help from health professionals’ and we identified the remainder as taking help from non-health professionals/untrained birth attendants (UTBA).
Table 3 shows that more than half (56.1%) of the respondents did not receive professional help during their last delivery i.e. they received help from a UTBA or from people outside the health profession. So, we can say that there are serious health implications for the mothers and their children who live in the study areas. This means that the importance of mothers going to a health facility for their childbirth is not properly promoted in the study areas.
Table 3.
Percentage distribution of women by type of assistance during last delivery
| Assistant during Last Delivery | Number of Women | Percentage |
|---|---|---|
| Health professional | 307 | 43.9 |
| Non-health professional/UTBA | 393 | 56.1 |
| Total | 700 | 100 |
TAKING IRON TABLETS/SYRUP AND VITAMIN TABLETS/SYRUP
Iron tablets/syrup and vitamin tablets/syrup are supplements necessary during pregnancy for the health of mothers and their unborn babies. Table 4 shows the percentage distribution of mothers according to whether they took iron tablets/syrup and vitamin tablets/syrup during their last pregnancy period, related to their family’s monthly income. For this purpose, we classified the respondent’s total family income into three groups as Taka ≤2000, Taka 2001–2500 and Taka 2501+ per month (US$ 28.5, $30–36 and over $37 per month respectively)
Table 4.
Percentage distribution of women taking iron tablet/syrup and vitamin tablet/syrup corresponding to their family’s monthly income in Taka (TK).
| Monthly Income (Taka) | Iron Tablets/Syrup | Vitamin Tablets/Syrup |
|---|---|---|
| Percentage not taking | Percentage not taking | |
| ≥2000 | 87.5 | 100.0 |
| 2001–2500 | 81.0 | 90.5 |
| 2501+ | 56.6 | 66.8 |
| Total Percentages not taking the medicines | 58.4 | 68.6 |
Note: N = 700
Although the percentage taking iron tablets/syrup and vitamin tablets/syrup during their last pregnancy increased somewhat with the increase of family’s monthly income, the overall percentage of those taking iron tablets/syrup and vitamin tablets/syrup is only 41.6% and 31.4% respectively, which is unsatisfactory [Table 4]. So, we can say that, irrespective of their level of income, well under half the respondents of the study areas do not take iron tablets/syrup and vitamin tablets/syrup during their pregnancy. This is no doubt because low monthly incomes prevent many from purchasing iron tablets/syrup and vitamin tablets/syrup.
MULTIVARIATE ANALYSIS
The results of the logistic regression analysis, presented in Table 5, show that the respondents’ education, place of treatment, husband’s occupation, family income, and exposure to mass media were significantly associated with going for an ANC checkup during the last pregnancy. Table 5 shows that education was the key factor among slum area mothers in seeking medical checkups during pregnancy; large and statistically significant differences were observed here despite having controlled for other variables. The relative odds ratio for literate mothers was found to be 1.994 indicating that the likelihood of medical checkup during the last pregnancy of literate mothers was 1.994 times higher than for illiterate ones. Husband’s occupation was another significant factor influencing medical checkup during pregnancy. The logistic co-efficient indicated that the highest occurrence of medical checkup during last pregnancy was among wives of service sector workers, followed by businessmen. These women were 1.214 and 1.078 times respectively more likely to go to medical checkup than the wives of labourers [Table 5].
Family income was also significantly associated with antenatal checkups in the last pregnancy. The results shows that women with a monthly family income of TK 2001–2500 and TK 2501+ (US$30–36 and over $37 per month respectively) were 1.052 times and 1.402 times respectively more likely to go for an antenatal medical checkup than the women with a monthly family income of TK ≤2000 (US$ 28.5) [Table 5]. Types of toilet facility had an effect on antenatal medical checkups; mothers with hygienic toilet facilities were 1.699 times more likely to go for antenatal medical checkups, but this effect is not statistically significant.
The result reveals that the mothers who go to hospitals and clinics for general health related problems are 1.659 times more likely to go for antenatal medical checkups than mothers who go to homeopathic, kabiraj (medical practitioners without a degree in medical sciences) and others types of non-medical services [Table 5]. As regards mass media, the results show that the mothers who are exposed to mass media are 2.253 times more likely to go for medical checkup than those not exposed.
Discussion
The study indicates that the proportion of pregnant women in the study area who take TT injections is very high, but is still not 100% despite various measures taken by different authorities against this disease which is fatal to mothers and children. More than half of the births in slum areas take place without the assistance of any health professional. This may indicate that births take place in unhygienic conditions putting both mothers and their new borns at risk. As far as taking iron tablets/syrup and vitamin tablets/syrup is concerned, monthly income plays an important role. The results of the logistic regression indicated that medical checkups increased as the level of mothers’ education increased, as they come to realise the importance of antenatal medical checkups. Place of treatment is an important factor that may strongly affect whether mothers go for antenatal checkups. For this reason, the place of treatment is classified into two categories. In the first category, homeopathic, kabiraj (Bangladeshi medical practitioners without a degree in medical sciences) and others are included, while the secondly category is hospital and clinic. The results showed that the odds are higher for the mothers who go to hospitals and clinics for antenatal medical checkups. Mass media is also shown by this study to play a strong role by creating awareness about the pregnancy related complications and the negative effect these complications can have on the future health of mothers and their new born babies. Therefore, the role of mass media should be enhanced to reduce the overall pregnancy related morbidity and mortality in Bangladesh.
POLICY RECOMMENDATIONS
Effective policies are needed to improve existing ANC seeking behaviour in the slum areas of RCC. The specific recommendations are as follows:
ANC services such as childbirths need the assistance of health professionals; TT vaccination among the women should be enhanced in the study areas. Government, the private sector or NGOs, or all three should do this by increasing their funds and facilities.
The people of the study areas should be made aware of the available local health facilities and pregnant women should be encouraged to have antenatal medical checkups. This could be done by creating awareness among the slum people, especially among women, through mass media campaigns, and the education and employment sectors.
Footnotes
CONFLICT OF INTEREST
The authors report no conflict of interest.
References
- 1.State of World Population. Unleashing the Potential of Urban Growth. New York: United Nations, Fund for Population Activities (UNFPA); 2007. [Google Scholar]
- 2.Center for Urban Studies (CUS) Slums of Urban Bangladesh: Mapping and Census. Dhaka: National Institute of Population Research and Training (NIPORT); 2005. [Google Scholar]
- 3.Mitra SN, et al. Bangladesh Demographic and Health Survey (BDHS) Dhaka: National Institute of Population Research and Training (NIPORT); 2004. [Google Scholar]
- 4.Vanneste AM, Ronsmans C, Chakraborty J, Francisco AD. Prenatal screening in rural Bangladesh: From prediction to care. Health Policy & Planning. 2000;15:1–10. doi: 10.1093/heapol/15.1.1. [DOI] [PubMed] [Google Scholar]
- 5.Yousif EM, Rahman MA, Hafeez A. The effect of antenatal care on the probability of neonatal survival at birth, Wad Medani Teaching Hospital, Sudan. Sudan J Public Health. 2006;1:293–7. [Google Scholar]
- 6.Mullick SM, Beksinksa M, Msomi S. Treatment for syphilis in antenatal care: Compliance with the three dose standard treatment regimen. Sex Transm Infect. 2005;81:220–2. doi: 10.1136/sti.2004.011999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carroli G, Villar J, Piaggio G, Khan-Neelofur D, Gülmezoglu M, Mugford M, et al. WHO Antenatal Care Trial Research Group. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. 2001;357:1565–70. doi: 10.1016/S0140-6736(00)04723-1. [DOI] [PubMed] [Google Scholar]
- 8.Villar J, Bergsjø P. Scientific basis for the content of routine antenatal care: Recent studies and power to eliminate or alleviate adverse maternal outcomes. Acta Obstet Gynecol Scand. 1997;76:1–14. doi: 10.3109/00016349709047778. [DOI] [PubMed] [Google Scholar]
- 9.Villar J, Ba’aqeel H, Piaggio G, Lumbiganon P, Belizán J, Farnot U, et al. WHO Antenatal Care Trial Research Group. WHO antenatal care randomised trial for the evaluation of a new model of routine antenatal care. Lancet. 2001;357:1551–64. doi: 10.1016/s0140-6736(00)04722-x. [DOI] [PubMed] [Google Scholar]
- 10.Government of Bangladesh (GOB), Asian Development Bank (ADB) Bangladesh Urban Primary Health Care Project-2: Midterm Report and Situation Analysis. 2004. [Google Scholar]
- 11.World Health Organization (WHO) Expanded Program on Immunization System, Summary for the South East Asia Region. Geneva: WHO; Apr, 1992. [Google Scholar]
- 12.Mitra SN, et al. Bangladesh Demographic and Health Survey (BDHS) Dhaka: National Institute of Population Research and Training (NIPORT); pp. 1993–1994. [Google Scholar]
- 13.Expanded Programme on Immunization (EPI) Coverage Survey, Bangladesh. Dhaka: Directorate General of Health Services; 2005. [Google Scholar]
- 14.World Health Organization (WHO) Improved Access to Maternal Health Services. Geneva: WHO; 1998. [Google Scholar]
- 15.Population Report. Meeting the Needs of Young Adults. Family Planning Program: Series J. 1995 Oct;(41) [PubMed] [Google Scholar]