Abstract
Odontogenic cutaneous fistula or sinus is an uncommon, but well documented condition, which is often initially misdiagnosed as a sole cutaneous lesion and inappropriately treated. The misdiagnosis as a skin infection often results in inappropriate management. We here present two cases of odontogenic cutaneous fistula that were seen after being treated unnecessarily with antibiotics.
Keywords: Odontogenic, Cutaneous fistula, Case report, Oman
A fistula is an abnormal pathological pathway between two anatomic spaces or a pathway that leads from an internal cavity or organ to the surface of the body. A sinus tract is an abnormal channel that originates or ends in one opening. An odontogenic cutaneous fistula is a pathologic communication between the cutaneous surface of the face and the oral cavity. In the literature, the terms fistulas and sinuses are often used interchangeably. A cutaneous fistula of dental origin is a rare entity,1 but well documented in medical, dental and dermatological literature.2,3 As the lesion develops, it is usually not thought to be of dental origin and the patient seeks treatment from a dermatologist, a family physician or a general surgeon, often undergoing multiple antibiotic regimens, surgical excisions and biopsies. It has been estimated that half of the patients with odontogenic cutaneous fistulas are submitted to multiple dermatological surgical operations and long-term antibiotic therapy before the correct diagnosis is established.4 Delay in diagnosis adds to the chronicity of the lesion and sometime leads to cosmetic deformities secondary to cutaneous scarring.
An odontogenic cutaneous fistula usually arises as a sequel to bacterial invasion of the dental pulp through a breach in the enamel and the dentine by a carious lesion, trauma, or other causes.3,5 If treatment is not initiated at this stage, the pulp becomes necrotic and infection spreads beyond the confines of the tooth into the peri-radicular area resulting in apical periodontitis that subsequently dissects along the path of least resistance and erupts through the skin.4 Once diagnosed, the treatment is simple and effective, consisting of removal of the infected pulp tissue and filling of the root canal with biocompatible material resulting in minimal scarring of skin.
CASE ONE - DESCRIPTION
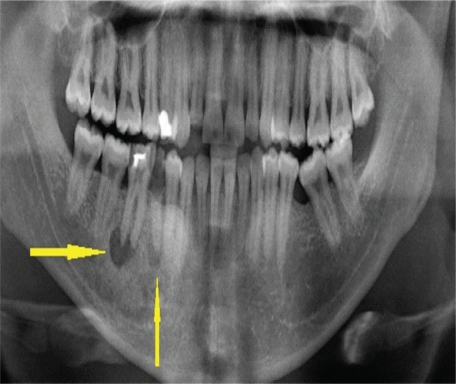
A 25 year-old man with no known co-morbidity presented to the Family Medicine Clinic of Sultan Qaboos University Hospital (SQUH), Oman, for the evaluation of a chronically draining, dimpled, crusted small nodule on his right cheek. The lesion was initially diagnosed as a superficial skin infection and was treated for several months with a number of systemic and topical antibiotics which provided only temporary relief. Physical examination revealed a small retracted skin lesion on lower part of right cheek of about 5 mm in diameter. The skin opening of the lesion was crusted, but with minimal swelling. Gentle pressure on the surrounding tissue elicited a scanty non-purulent bloody discharge on the surface. There was also a cord-like palpable tract extending from the cutaneous lesion to the oral cavity inside. Intra-oral examinations showed poor oral hygiene and dental caries in the right lower premolar and first permanent molar (teeth nos. 45 and 46). The patient was referred to an oral and maxillofacial surgeon. His orthopantomogram (OPG) demonstrated well defined radiolucency around the apex of teeth 45 and 46 [Figure 1].
Figure 1:
Orthopantomogram of patient 1. Arrows indicate radiolucency around the apex of right lower second premolar and first permanent molar.
CASE TWO - DESCRIPTION
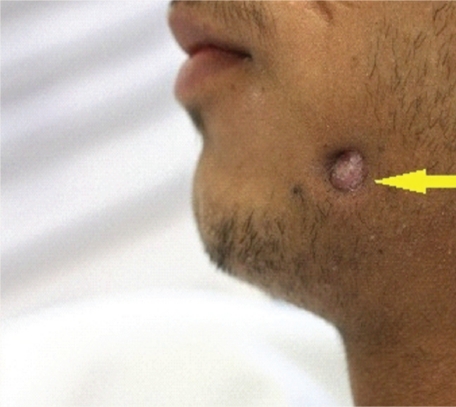
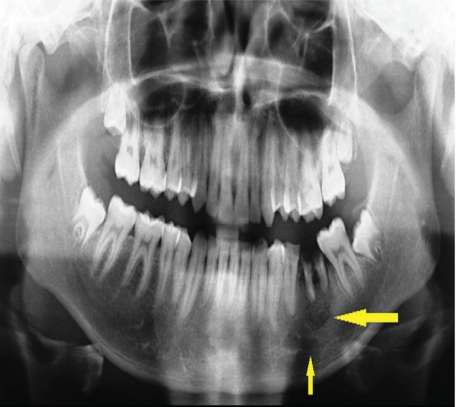
An 18 year-old male student was referred from the SQUH Surgery Department to an oral and maxillofacial surgeon in the Oral Health Department regarding a chronic, but painless, draining lesion on the left side of the cheek. Like the first case, this patient had also been treated for several months with antibiotics. On examination, there was a crusted skin lesion of about 0.8 cm in diameter on left side of the face [Figure 2]. Again, non-purulent discharge was expressed on pressing the surrounding skin. Intra-oral examination showed poor oral hygiene and caries in the lower left second premolar (tooth no. 35) and lower left first permanent molar (tooth no. 36). His OPG also showed radiolucency at the apex of teeth numbers 35 and 36 [Figure 3].
Figure 2:
Photograph of patient 2. Arrow indicates odontogenic cutaneous fistula and retracted skin.
Figure 3:
Orthopantomogram of patient 2. Arrows indicate radiolucency around the apex of the left lower second premolar and first permanent molar.
CASES ONE AND TWO – TREATMENT
The intra-operative findings for both patients showed a fluid-filled cyst around diseased teeth with a draining tract extending from the cyst to the outside skin. Both patients were booked for surgery under general anaesthesia (GA), as not only was the extraction of diseased teeth required, but also the excision and repair of the skin lesions. To excise the fistula, first an elliptical incision was made on the skin layer only. In this way, the facial nerve was protected as it lies in the deeper fascia. Then the dissection was made below the skin until the fistula tract was reached. The dissection was continued through the muscle until the intraoral origin of the tract was reached. The affected teeth were removed and the cystic lesion and granulation tissue were completely enucleated. The incision site was irrigated and closed in layers (muscles and oral mucosa with 3.0 vicryl suture and skin with 4.0 nylon suture). The elliptical shape of the incision has the effect of minimising post-surgical scar formation as compared to the disfiguring scar which may result if the lesion is left to heal on its own by granulation. Both patients were followed up postoperatively and both showed significant improvement [Figure 4].
Figure 4:
Postoperative photograph of patient 2. Arrow indicates scarring after surgery.
Discussion
The clinical cases of odontogenic cutaneous lesions described in this study had been previously misdiagnosed and managed inappropriately. The cutaneous fistula of dental origin is an uncommon, but well documented, condition in the literature. Diagnosis is challenging for many reasons. This can be due to the fact that these lesions do not always arise in close proximity to the underlying dental infection and only about half of patients ever recall having had toothache.6 A clinician’s high index of suspicion can lead to early and correct diagnosis. A thorough history taking and intraoral examination are critical for making the appropriate diagnosis and may spare the patient much unnecessary treatment. In suspected cases, early consultation with a dentist is of great importance in providing appropriate differential diagnosis and clinical care.2
The classic lesion is an erythematous, smooth, symmetrical nodule, 1–20 mm in diameter with or without drainage. The chronic lesion often leads to retraction of skin secondary to scarring. A cord like tract can be felt attached to the underlying bony structure. Many of above mentioned typical findings were present in the two cases described in this report. Patients may experience intermittent remission of the symptoms. Intraoral examination may reveal dental caries or restorations and periodontal disease, but the examiner should keep in mind that even the tooth involved can appear normal.7 The initial working diagnosis is confirmed by radiographs and pulp vitality tests, diseased teeth responding negatively to the latter. In the clinical cases described here, the radiographs clearly revealed obvious periapical radiolucencies which are associated with diseased teeth. As far as definitive treatment is concerned, root canal therapy or surgical extraction is the treatment of choice.7,8
Usually, no systemic antibiotics need to be prescribed as the lesion is a localised entity, but they should be considered in patients with diabetes, immunosuppression, or signs of systemic infection.4 Most authors believe that once the primary cause is removed the cutaneous lesion heals without treatment, usually resolving in 1 to 2 weeks. The residual scarring can be surgically revised if it is cosmetically unappealing for the patient.4
Delay in the treatment of dental infections can sometimes lead to the infection spreading to fascial spaces in the orofacial area or deep in the head and neck (peripharyngeal space infections). In addition, odontogenic infections may cause osteomyelitis of the jaw or systemic illness.
Many patients seek evaluation from several physicians before an accurate diagnosis is made. It has been estimated that half of all patients undergo multiple surgeries and trials of antibiotics before definitive diagnosis.4 This emphasises the importance of communication between medical sub-specialists and dentists in the evaluation of patients with head and neck lesions.
Conclusion
These cases highlight the fact that dental aetiology should be considered as a part of a differential diagnosis for any orofacial skin lesions. It also serves to underline the importance of communication between medical subspecialties. Although many non-odontogenic disorders may also produce an extra-oral fistula, the opinion of a dentist in cases of a cutaneous sinus tract is of great importance in providing appropriate clinical care. Endodontic treatment or dental extraction may eliminate the infection and lead to resolution of the lesion and prevent unnecessary ineffective antibiotic therapy and/or surgical intervention. These cases would also suggest that dentists may need to educate their medical colleagues and medical students on the importance of oral examination and role of the dentist in the management of oro-facial infections
References
- 1.Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous sinus tract: an odontogenic etiology. J Am Acad Dermatol. 1986;14:94. doi: 10.1016/s0190-9622(86)70012-1. [DOI] [PubMed] [Google Scholar]
- 2.Yasui H, Yamaguchi M, Ichimiya M, Yoshikawa Y, Hamamoto Y, Muto M. A case of cutaneous odontogenic sinus. J Dermatol. 2005;32:852–5. doi: 10.1111/j.1346-8138.2005.tb00859.x. [DOI] [PubMed] [Google Scholar]
- 3.Mittal N, Gupta P. Management of extra oral sinus cases: a clinical dilemma. J Endod. 2004;30:541–7. doi: 10.1097/00004770-200407000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Cantatore JL, Klein PA, Lieblich LM. Cutaneous dental sinus tract, a common misdiagnosis: a case report and review of the literature. Cutis. 2002;70:264–7. [PubMed] [Google Scholar]
- 5.Stoll HL, Solomon HA. Cutaneous sinuses of dental origin. JAMA. 1963;184:120–4. doi: 10.1001/jama.1963.03700150074012. [DOI] [PubMed] [Google Scholar]
- 6.Winstock D. Four cases of external facial sinuses of dental origin. Proc R Soc Med. 1959;52:749–51. [PMC free article] [PubMed] [Google Scholar]
- 7.Ong ST, Ngeow WC. Medial mental sinus in twins. Dent Update. 1999;26:163–5. doi: 10.12968/denu.1999.26.4.163. [DOI] [PubMed] [Google Scholar]
- 8.Swift JQ, Gulden WS. Antibiotic therapy: managing odontogenic infections. Dent Clin N Am. 2002;46:623–33. doi: 10.1016/s0011-8532(02)00031-9. [DOI] [PubMed] [Google Scholar]