Abstract
Objectives:
Femoral artery access is the standard approach for coronary procedures; however, the radial approach has gained sound recognition as an alternative to femoral access. We present our early experience with the transradial approach.
Methods:
A prospective, non-randomised study of 221 candidates for diagnostic coronary angiography was carried out at Sultan Qaboos University Hospital, Oman between December 2008 and April 2009. The patients had their procedure performed from radial or femoral access according to operator discretion and the results were compared. Femoral and radial groups included 116 and 105 patients respectively.
Results:
Radial access was associated with a significantly higher rate of procedural failure (17.1%) versus 0% in femoral group (p = 0.001). There were no local vascular complications in the radial group as opposed to 12.1% in the femoral group (p < 0.01). Hospital length of stay was significantly reduced in the radial group (4.06 versus 23.5 hours, p < 0.01). Total procedure time was longer in the radial group (23.7 ± 13.7 min versus 20.1 ± 7.4 min, p < 0.001), but radiation exposure was similar in both groups. There was a trend for a higher risk of major adverse cardiac events noticed in the femoral group; however, it did not reach statistical significance.
Conclusion:
The transradial approach for coronary angiography is associated with significantly reduced local vascular complications and shorter hospital stays. The femoral approach is the standard access site for coronary angiography; however, interventional cardiologists should acquire experience in the radial approach as an alternative in specific situations.
Keywords: Coronary angiography, Radial, Femoral, Local vascular complications, Crossover, bleeding, Hospital stay
Advances in Knowledge
This study sheds light on the feasibility of using the radial route as an alternative access for diagnostic coronary angiography.
It highlights the advantages and disadvantages of this procedure and compares our results with the available literature.
Application To Patient Care
The radial route reduces the complications rate, is convenient for patients as they can be mobilised immediately and cuts down the hospital stay so relieving pressure on limited bed space.
The radial approach is sometimes the route of choice in the presence of contraindications to using the standard femoral route.
In our Muslim population, the radial route is highly preferred by females in general and especially during menstruation, as some of them are reluctant to undergo procedure by the femoral route.
This article stresses the importance of all interventional cardiologists having the skills required to perform left heart catheterisations through the radial route.
The transradial approach for diagnostic and interventional coronary angiography was introduced by Campeau et al. in 1989.1 The transradial access has several advantages over the transfemoral approach. Being an easily compressible artery, any bleeding is controllable and local vascular haemorrhagic complications are virtually eliminated.2–4 Patients may ambulate immediately after the procedure and hospital length of stay is significantly reduced.5–7 There is a substantial economic benefit to the transradial approach, and this can be demonstrated by either evaluation of hospital costs or total hospital charges.3–6 Despite these proven benefits, the transradial approach is more demanding than transfemoral access and requires a longer learning curve for the operator.8–9 Furthermore, it does not allow the use of other devices such as intraaortic balloon pumps or coronary interventions requiring larger 8F catheters.10 The femoral approach is still considered by many as the standard technique because of its optimal catheter control and immediate access to large diameter devices, however, such advantages are partially offset by bleeding complications.11 We therefore present our early experience with the transradial approach for diagnostic coronary angiography.
Methods
The study population was drawn from 221 patients admitted to Sultan Qaboos University Hospital for diagnostic coronary angiography between December 2008 and April 2009. Written informed consent was obtained from every patient. The study was prospective and non-randomised. The patients had their procedure performed either from the radial or femoral access according to operator discretion and the results were compared. The femoral group included 116 patients and the radial group 105. All patients who underwent the radial approach had an Allen’s test.12 If the test suggested incomplete palmer arch flow, the procedure was performed through transfemoral access and counted as radial access failure (crossover). The study group included patients who underwent coronary angiography for stable angina, post revascularisation angina and for assessment of coronary anatomy before valvular surgery. Patient were excluded if they had acute coronary syndrome, unexplained fever, untreated infection, severe anaemia with haemoglobin less than 8g/dl, severe electrolyte imbalance, severe active bleeding, acute renal failure, or international normalised ration (INR) > 1.4.
All patients were prepared according to the American College of Cardiology/American Heart Association (AHA/ACC) task force on Cardiac Catheterization Laboratory Standards,13 and were sedated by diazepam 1.5mg orally the night before the procedure. Patients at high risk for contrast induced allergic reaction had premedications by IV hydrocortisone. Routine laboratory investigations including urea and electrolytes, full blood counts, liver and renal function tests, coagulation profile, HIV and hepatitis status were performed. The technique of radial artery cannulation has been described previously.14 Left heart catheterisation through the radial approach was performed with a dedicated 5 French sheath, 5 French diagnostic catheters (TIG) for both left and right coronaries and 5 French pigtail catheter if left ventriculuography and/or aortography was required. A cocktail of 100mg glyceryl trinitrate and verapamil 2mg was injected after sheath insertion followed by 5000 international units heparin inside the sheath. All femoral catheterisations were performed using 6 French sheath and diagnostic catheters, usually Judkins catheters. In the radial group, the radial artery sheath was immediately removed at the completion of the procedure and haemostasis was obtained by local compression and a tight pressure bandage for 3 hours. Patients were allowed to ambulate immediately unless their clinical status dictated otherwise. In the femoral group, patients were transferred to the recovery room where the sheath was removed and haemostasis was obtained using manual compression for at least 10 minutes. These patients remained in bed rest for 6–8 hours.
The need to puncture a second access site due to any procedural failure (inability to puncture the entry site artery, failure to cannulate the coronary artery, impossibility to perform the procedure due to major access site complication) was defined as a “crossover”. Outcomes measures collected conformed to the ACC database definitions for vascular complications. Minor vascular complications were defined as any of the following: haematoma >10 cm, arteriovenous fistulae, or pseudoaneurysm. Major vascular complications were defined as death caused by vascular complications, vascular repair, major vascular bleeding (> 3g haemoglobin decrease because of access site bleeding or retroperitoneal bleeding), vessel occlusion, or loss of pulse.15 Cerebrovascular stroke was classified into: either a) minor cerebrovascular accident: any new motor disability post procedure that improved within one week; b) major cerebrovascular accident: any new motor disability post procedure that continued beyond one week. The diagnosis of ST elevation myocardial infarction (MI) was based on: a) a clinical history of prolonged ischaemic chest pain ≥ 30 minutes in duration; b) evolution of typical changes in at least two adjacent leads of the electrocardiogram (ECG); c) appearance of ST segment elevation > 2 mm 0.08 seconds after J point persisting for at least 24 hours with or without Q waves, and a time-dependent rise in troponins and subsequent fall.16
The statistical analysis was carried out using the Statistical Package for the Social Sciences (SPSS), Version 15 for Windows. Continuous data are expressed as mean value ± SD and categorical data as percentages. Continuous variables were compared using the Student’s paired t-Test. Categorical data were compared using chi-square (X2) analysis. A p value of 0.05 or less was considered to be statistically significant. The main primary outcome was to assess crossover, and to evaluate local vascular complications. The secondary procedural outcomes were: 1) procedural time; 2) fluoroscopy time; 3) any major adverse cardiac events and 4) length of hospital stay.
Results
Out of the 105 patients assigned to the radial approach, 18 (17.1%) patients had procedure failure. Three of the latter patients (2.8%) had a positive Allen’s test suggesting an incomplete palmer arch flow. There were 10 cases of access site failures (9.5%); 2 radial artery spasms (1.9%) and 3 cases of extensive subclavian artery tortuosity (2.8%) [Figures 1, 2, and 3] These 18 patients were included in the femoral group. The remaining 87 patients constituted the final radial group. The final femoral group consisted of 116 patients who had their procedures performed via the femoral approach plus 18 radial crossovers giving a total of 134. There were no crossover patients from the femoral to the radial approach. The baseline demographic characteristics are shown in Table 1. Radial group patients were significantly younger than the femoral group (ρ = 0.03). The majority of these patients were males: 74.7% versus 67.1%, in the radial and femoral groups respectively.
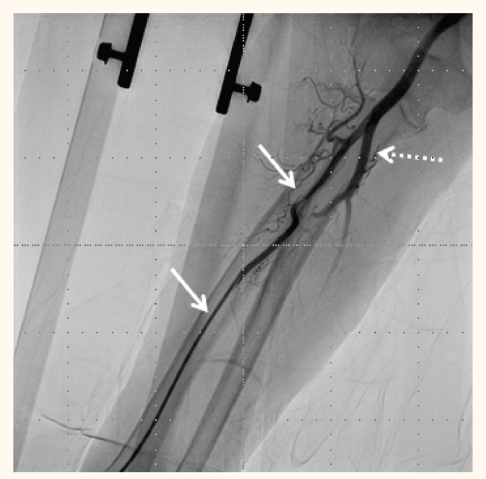
Figure 1:
Intense radial artery spasm (continuous arrows) relieved by an additional dose of the vasodilatory cocktail. Dashed arrow shows normal ulnar artery.
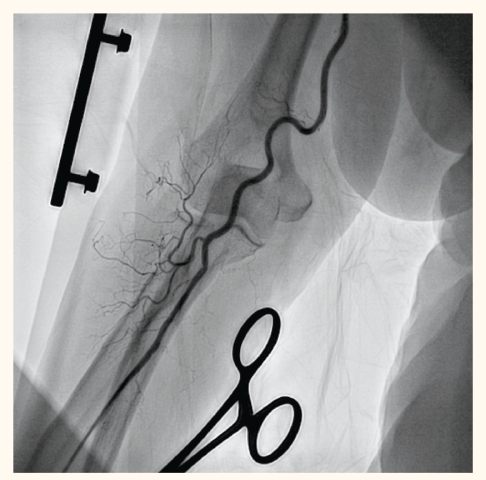
Figure 2:
Spasm of radial artery and tortuous brachial artery are evident. The most interesting finding is the absent ulnar artery despite a well perfused palmar arch, well felt pulsations at the ulnar artery and a positive Allen’s test
Figure 3:
Marked tortuosity of the right subclavian artery making manipulation of the catheter difficult.
Table 1:
Demographic characteristics of both groups
| Femoral group | Radial group | ρ Value | |
|---|---|---|---|
| Age (years) | 56.1 ± 12.3 | 52.6 ± 12.4 | 0.03 |
| Male gender | 67.1 | 74.7 | ns |
| HTN (%) | 46.2 | 40.2 | ns |
| DM (%) | 41.0 | 35.6 | ns |
| Dyslipidaemia (%) | 14.2 | 19.5 | ns |
| Old MI (%) | 20.9 | 16.1 | ns |
| Prior PCI (%) | 20.8 | 19.5 | ns |
| Prior CABG (%) | 7.4 | 5.0 | ns |
| Old CVA (%) | 0.7 | 3.4 | ns |
Legend: HTN = hypertension; DM = diabetes mellitus; MI = myocardial infarction, PCI = percutaneous coronary intervention; CABG = coronary artery bypass graft; CVA = cerebrovascular accident; ns = not significant
The angiographic data are shown in Table 2. The vessel distribution between the two groups was almost the same. The procedure outcomes are illustrated in Table 3. Crossover occurred in 17.1% of patients in the radial group compared to 0% in the femoral group (p = 0.001). Additional analysis was performed in the radial cohort of patients and showed the following: 13 patients (12.38%) were crossed over in the first half of the study, whereas only 4 patients (3.8%) were crossed over in the second half of the study. This diminution in the crossover rate as the study progressed highlights the experience acquired during the study.
Table 2:
Angiographic characteristics of both groups
| Femoral group % | Radial group % | p value | |
|---|---|---|---|
| Left main | 4.5 | 5.7 | ns |
| Left anterior descending | 62.9 | 53.3 | ns |
| Diagonals | 34.8 | 29.9 | ns |
| Left circumflex | 30.3 | 26.7 | ns |
| Obtuse marginal | 24.6 | 28.3 | ns |
| Ramus intermedius | 3.8 | 7.7 | ns |
| Right coronary artery | 48.5 | 44.8 | ns |
| Posterior descending | 9.1 | 8.3 | ns |
| Posterolateral | 4.5 | 3.3 | ns |
| Right dominance | 75.8 | 70.1 | ns |
| Number of diseased vessels | 1.52 ± 1.18 | 1.45 ± 1.04 | ns |
Table 3:
Procedure outcome
| Femoral group | Radial group | p value | |
|---|---|---|---|
| Crossover (%) | 0 | 17.1 | 0.001 |
| Local vascular complication (%) | 8.2 | 0 | 0.001 |
| Procedure time (minutes) | 20.1 ± 7.4 | 23.7 ± 13.7 | 0.001 |
| Radiation exposure (minutes) | 10.1 ± 7.6 | 11.3 ± 8.4 | ns |
| MACE (%) | 1.5 | 0 | ns |
| Hospital stay (hours) | 23.8 ± 2.2 | 4.1 ± 1.1 | 0.001 |
Legend: MACE = major adverse cardiac event discussion
The total local vascular complications rate (8.2%) in the femoral group was significantly higher than the radial group (p = 0.01). These local vascular complications included minor bleeding in 9 patients (6.7%), major bleeding in one patient (0.74%) and major right iliac artery dissection requiring urgent stenting in one patient (0.74%). The procedure time was significantly longer in the radial group (23.7 versus 20.1 minutes, p = 0.001), however, the radiation exposure time was not significantly different indicating that the extra time was used to prepare and canulate the radial artery. In the present study, there were no deaths and no patients were referred for emergency percutaneous coronary intervention (PCI) or bypass surgery. In the femoral group, one patient developed documented acute ST elevation myocardial infarction 22 hours post-procedure requiring thrombolytic therapy which was complicated by severe bleeding from the right groin necessitating blood transfusion. Another patient in the femoral group experienced an acute cerebrovascular accident (CVA) immediately postprocedure complicated by a left-sided haemiplegia which improved dramatically over several weeks. The total length of hospital stay was significantly shorter in the radial group (4.1 hours) compared to the femoral group (23.8) hours with p = 0.001.
Discussion
Our early experience with the transradial approach shows that this access site for diagnostic coronary angiography has many advantages and some disadvantages over the standard transfemoral approach. The most obvious advantage is the almost total elimination of local vascular complications and a shorter hospital stay which is of paramount importance in an overcrowded hospital. However, this approach was associated with a high crossover rate not reported in the literature. There were four reasons for crossover to the transfemoral approach. First, a positive Allen’s test before the procedure that indicated limited palmar arch blood flow in three patients. Second, an inability to puncture successfully the radial artery in 10 patients, mostly because of early operator skills; these improved markedly by the end of the study. Third, the artery was cannulated, but failed to proceed because of persistent radial artery spasm in two patients [Figures 1 & 2]. Fourth, inability to manipulate the catheter toward the coronary ostia due to marked brachial, axillary and/or subclavian artery tortuosity in three patients [Figure 3]. All of these problems were clearly mentioned in prior studies, but in our study the percentage of failures was slightly higher than elsewhere.17–19 It was noticed that brachial, axillary and right subclavian artery tortuosity is not uncommon. Despite this, we failed in three cases to canulate the coronary ostia. We negotiated many of these tortuosities by: 1) the use of terumo wire (0.035 inch) and asking the patient to take a deep breath and hold it during continuous gentle catheter advancement and 2) the use of long exchange guide wires (260 cm, 0.032 inch) to exchange catheters once the aortic root was reached.
The radial artery is superficial and easily compressible, achieving adequate haemostasis with a pressure device or bandage without active manual compression. For that reason the radial approach abolished entry site complications in comparison to significantly higher rates of local vascular complications in patients undergoing transfemoral catheterisation.
In our study, 8.2% of the femoral group patients experienced some complications. Although the vast majority of these complications were minor haematomas and echymoses (6.8%), one patient (0.74%) developed flow limiting acute right iliac artery dissection; it was successfully managed immediately by deployment of two peripheral stents. Another patient (0.74%) developed acute ST elevation myocardial infarction requiring thrombolytic therapy (Reteplase). Postthrombolysis, she developed massive right groin bleeding requiring blood transfusion. Such local vascular complications were eliminated by the radial approach which is consistent with virtually all studies.20–21
The actual percentage of local vascular complications in our study was high compared to the literature. This may be explained by our sensitive definition of minor bleeds as small ecchymoses. This higher rate may also be affected by the limited experience of some of our nurses who were managing sheath removal. In addition, the radial group included patients who were younger and this may have contributed some bias to the results.
The procedural time for the transradial approach was significantly longer than that for the transfemoral one (23.7 versus 20.1 minutes respectively, p < 0.001). Achieving access to the radial artery is technically more challenging and time-consuming than gaining femoral access, but when the right skills are grasped, the technique is much easier and more reliable as we experienced towards the end of our study.
Despite the statistically significant longer duration in the transradial group, the total radiation exposure time was similar, suggesting that the wasted time was consumed in radial artery entry. The radiation time in our study was a combination of fluoroscopy and cine-fluoroscopy. In addition, some of our cardiac technicians have limited experience in this technique and require more fluoroscopy time for positioning imaging detectors. Unfortunately, both factors may have contributed to the prolonged radiation exposure time.
Fortunately, there were no deaths or need for emergency revascularisation by either PCI or coronary artery bypass graft (CABG) in our study. One patient in the femoral group (0.74%) experienced an acute major cerebrovascular stroke immediately after the procedure. This patient was elderly with angiographic evidence of heavily calcific aortic valve and extensive multi-vessel coronary artery disease requiring surgical intervention. Left ventriculography was accomplished to assess left ventricular function as well as any gradient across the aortic valve. Dislodgement of fibrocalcific plaque during aortic valve crossing could be the underlying aetiology. Interestingly, a 42 year-old lady was admitted for coronary and renal angiography with non-invasive documented evidence of coronary artery disease and resistant hypertension. This lady developed menstruation early as the morning of the procedure, so she refused to do the procedure from the femoral approach. The decision was made to perform both coronary and renal angiography through the radial approach which was done successfully.
The ability to rapidly ambulate patients after the transradial approach is extremely convenient for the patients and is a significant benefit, especially in overcrowded hospitals. In the present study, we decided to discharge radial group patients 4 hours post procedure. It was not feasible to discharge femoral group patients 8 hours after sheath removal even if they achieved full haemostasis. It has been the routine in our hospital to keep femoral patients overnight. The reasons are mainly to ensure reduced activity and complete haemostasis as most of our patients come from far away and travel back home by air. All femoral group patients stayed overnight. The total hospital length of stay was significantly shorter in the radial group. As a result, patients preferred the radial approach as consistent with prior studies.
There are some limitations to the current study, with it being single centre and a relatively small sample size. However, the study represents our early experience in radial access as an alternative to the femoral approach for diagnostic coronary angiography. A larger sample size is warranted in future studies.
Conclusion
The radial access site for coronary angiography is an appealing approach that eliminates the local vascular complications and significantly shortens the hospital stay. Despite these advantages, radial vascular access is still more challenging. The significant crossover from the radial to femoral approach can be improved as experience with the technique grows. The femoral approach is the standard access site for coronary angiography. However, interventional cardiologists should acquire the experience to cannulate the radial artery as an alternative in specific situations.
Footnotes
CONFLICT OF INTEREST
The authors report no conflict of interest.
References
- 1.Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989;16:3–7. doi: 10.1002/ccd.1810160103. [DOI] [PubMed] [Google Scholar]
- 2.Cooper CJ, El-Shiekh RA, Cohen DJ, Blaesing L, Burket MW, Basu A, et al. Effect of transradial access on quality of life and cost of cardiac catheterization: a randomized comparison. Am Heart J. 1999;138:430–6. doi: 10.1016/s0002-8703(99)70143-2. [DOI] [PubMed] [Google Scholar]
- 3.Kiemeneij F, Laarman GJ, Odekerken D, Slagboom T, van der Wieken R. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol. 1997;29:1269–75. doi: 10.1016/s0735-1097(97)00064-8. [DOI] [PubMed] [Google Scholar]
- 4.Mann JT, 3rd, Cubeddu MG, Schneider JE, Arrowood M. Right radial access for PTCA: A prospective study demonstrates reduced complications and hospital charges. J Invasive Cardiol. 1996;8:40–4D. [PubMed] [Google Scholar]
- 5.Valsecchi O, Musumeci G, Vassileva A, Tespili M, Guagliumi G, Gavazzi A, et al. Safety, feasibility and efficacy of transradial primary angioplasty in patients with acute myocardial infarction. Ital Heart J. 2003;4:329–34. [PubMed] [Google Scholar]
- 6.Achenbach S, Ropers D, Kallert L, Turan N, Krähner R, Wolf T, et al. Transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter Cardiovasc Interv. 2008;72:629–35. doi: 10.1002/ccd.21696. [DOI] [PubMed] [Google Scholar]
- 7.Hildick-Smith DJ, Walsh JT, Lowe MD, Petch MC. Coronary angiography in the fully anticoagulated patient: the transradial route is successful and safe. Cathet Cardiovasc Intervent. 2003;58:8–10. doi: 10.1002/ccd.10374. [DOI] [PubMed] [Google Scholar]
- 8.Louvard Y, Pezzano M, Scheers L, Koukoui F, Marien C, Benaim R, et al. Coronary angiography by a radial artery approach: feasibility, learning curve: one operator’s experience. Arch Mal Coeur Vaiss. 1998;91:209–15. [PubMed] [Google Scholar]
- 9.Goldberg SL, Renslo R, Sinow R, French WJ. Learning curve in the use of the radial artery as vascular access in the performance of percutaneous transluminal coronary angioplasty. Cathet Cardiovasc Diagn. 1998;44:147–52. doi: 10.1002/(sici)1097-0304(199806)44:2<147::aid-ccd5>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 10.Campeau L. Entry sites for coronary angiography and therapeutic interventions: from the proximal to the distal radial artery. Can J Cardiol. 2001;17:319–25. [PubMed] [Google Scholar]
- 11.Lo TS, Nolan J, Fountzopoulos E, Behan M, Butler R, Hetherington SL, et al. Radial artery anomaly and its influence on transradial coronary procedural outcome. Heart. 2008;95:410–15. doi: 10.1136/hrt.2008.150474. [DOI] [PubMed] [Google Scholar]
- 12.Gilchrist C. Is the Allen’s test accurate for patients considered for transradial coronary angiography? J Am Coll Cardiol. 2006;48:1287. doi: 10.1016/j.jacc.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 13.Scanlon PJ, Faxon DP, Audet AM, Carabello B, Dehmer GJ, Eagle KA, et al. ACC/AHA Guidelines for Coronary Angiography: Executive Summary and Recommendations. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) Developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation. 1999;99:2345–57. doi: 10.1161/01.cir.99.17.2345. [DOI] [PubMed] [Google Scholar]
- 14.Schneider JE, Mann T, Cubeddu MG, Arrowood ME. Transradial coronary stenting: a United States experience. J Invasiv Cardiol. 1997;9:569–74. [PubMed] [Google Scholar]
- 15.Applegate RJ, Sacrinty MT, Kutcher MA, Kahl FR, Sanjay K, Gandhi SK, Renato M, Santos RM, et al. Trends in vascular complications after diagnostic cardiac catheterization and percutaneous coronary intervention via the femoral artery, 1998 to 2007. J Am Coll Cardiol Intv. 2008;1:317–26. doi: 10.1016/j.jcin.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 16.Alpert JS, Thygesen K. Myocardial Infarction Redefined - A consensus document of the Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of Myocardial Infarction. Eur Heart J. 2000;21:1502–13. doi: 10.1053/euhj.2000.2305. [DOI] [PubMed] [Google Scholar]
- 17.Mont‘alverne Filho JR, Assad JA, Zago Ado C, da Costa RL, Pierre AG, Saleh MH, et al. Comparative study of the use of diltiazem as an antispasmodic drug in coronary angiography via the transradial approach. Arq Bras Cardiol. 2003;81:54–8. doi: 10.1590/s0066-782x2003000900005. [DOI] [PubMed] [Google Scholar]
- 18.McEntegart MB, Dalzell JR, Lindsay MM. An unusual complication of transradial coronary angiography. J Invasive Cardiol. 2009;21:E91–2. [PubMed] [Google Scholar]
- 19.Agostoni P, Biondi-Zoccai GG, de Benedictis ML, Rigattieri S, Turri M, Anselmi M, et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures. Systematic overview and meta-analysis of randomized trials. J Am Coll Cardiol. 2004;44:349–56. doi: 10.1016/j.jacc.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 20.Hamon M, Nolan J. Should radial artery access be the “gold standard” for PCI? Heart. 2008;94:1530–2. doi: 10.1136/hrt.2008.148379. [DOI] [PubMed] [Google Scholar]
- 21.Bertrand F, Arsenault J, Mongrain R. Operator vs. patient radiation exposure in transradial and transfemoral coronary interventions. Eur Heart J. 2008;29:2577–8. doi: 10.1093/eurheartj/ehn394. [DOI] [PubMed] [Google Scholar]