Abstract
Background.
To examine the impact of educational attainment on the incidence of preclinical mobility disability (PCD).
Methods.
The Women's Health and Aging II Study is a prospective observational cohort study of 436 initially high-functioning community-dwelling women aged 70–79 years at baseline in Baltimore, Maryland. We measured the association of highest attained education level with preclinical mobility disability (PCD) over an 11-year period. PCD is defined as self-reported modification in any of four tasks without reporting difficulty in those tasks. The tasks were walking ½ mile, climbing up steps, doing heavy housework, and getting in/out of bed or chair.
Results.
Participants with less than 9 years of education were more likely to acquire incident PCD (hazard ratio: 3.1, 95% confidence interval = 1.2–7.7) than their counterparts with more education after adjusting for income, marital status, number of diseases, and high self-efficacy.
Conclusions.
Lower education level is an independent predictor of incident preclinical mobility disability. This association has important implications for primary and secondary prevention and can be easily assessed in clinical encounters.
Keywords: Health disparities, Mobility, Preclinical disability
LOW education is a well-described predictor of poor physical functioning in older adults (1–3). This association is likely due to increased disease burden (4–7), decreased health literacy to manage disabling conditions (8,9), and poorer neighborhood and home environment (10).
Unfortunately, the loss of functional independence triggers a cascade of progressive decline in mobility task performance (11). Establishing risk factors that a primary care practitioner could both easily identify and potentially modify early in the process could enhance the ability to forestall progressive decline. Chaves and colleagues identified key clinical predictors to identify those at risk for functional decline (12). One of these independent predictors is preclinical mobility disability (PCD). PCD is defined as self-reported modification of task performance without perceiving difficulty with the task (13–15). Those with PCD have worse physical performance and are at risk for future mobility disability (16).
Prior evidence indicates that low education is related to decreased mobility(1–10). However, the extent to which low education is related to incident PCD is not known. This article adds to the literature by examining how education affects PCD. The Women's Health and Aging Study is a unique cohort of high-functioning older women where we measured PCD. We hypothesized that among these initially high-functioning older women, those with fewer years of educational attainment would be at higher risk for incident PCD than their more educated counterparts.
METHODS
Sample
The Women's Health and Aging Study II (WHAS II) is a prospective observational cohort study of 436 community-dwelling women aged 70–79 years, with minimal or no disability and no cognitive impairment at baseline. Full details of the sampling and recruitment methodology have been previously described (12,16). Briefly, partcipants were recruited from an age-stratified sample of Medicare beneficiaries in 12 contiguous zip codes of Baltimore City and County, Maryland. They were selected to represent the two thirds least disabled women living in the community in this age group. They were excluded if they reported difficulty in more than one of four functional domains: mobility and exercise tolerance, upper extremity tasks, higher functioning (eg, shopping), and basic self-care (12). Those with Mini-Mental State Examination scores less than 24 were excluded. Among eligible screened women, 49.5% agreed to participate and provided informed consent. Those agreeing to participate were more highly educated and had more diseases than those who refused but did not differ significantly in disability characteristics. Data reported in this artcle were collected at baseline and six follow-up examinations; all were 18 months apart except for the interval between the third and the fourth examination, which was, on average, 3 years. This resulted in a median follow-up time of 10 years between 1994 and 2008.
Risk Factor Characteristics
Education level was ascertained by asking, “What was the highest grade in school or year of college that you have completed?” Educational status was categorized as 8 years or less, 9–11 years, 12 years, or greater than 12 years. These cutpoints were chosen for years of education because the cohort was attending school at the time when public schools were segregated and there were no public high schools in Baltimore County that African Americans could attend. Marital status was classified as married, widowed separated/divorced, or never married. Self-efficacy was included because of the positive effect it had been shown to have on health decisions, such as task modification (17,18). Self-efficacy was ascertained by asking “Do you, in general, feel helpless,” with responses ranging from strongly disagree, disagree, and agree to strongly agree (17). Race and history of physicians’ diagnosis of 14 selected chronic diseases were obtained through self-report (19). Race was binary (African American or white). Count of chronic diseases was treated as continuous data. There were missing data for income (132 of the total 436). These missing data were imputed by a composite hot-deck method using a regression with variables, such as poverty status, receipt of Medicaid, age, race, and number in household to predict income (20).
Definition of Mobility Function for the Current Analysis
Four mobility tasks were the focus of these analyses as self-reported changes in mobility tasks were the primary area of functional change in this initially highly functional cohort. These tasks were walking ½ mile, climbing up steps, doing heavy housework, and getting in/out of a bed or chair. The participants were asked, “For health or physical reasons do you have any difficulty in (doing a specific task).” Then, to identify early functional decrements, we asked each participant, who reported no difficulty, “Have you changed the way or how often you do the task, due to a health or physical condition?” Consistent with previously reported methods (12), each task consists of three levels of mobility function: (a) task difficulty, (b) no task difficulty but modification of method or change in frequency of task performance, or (c) no task difficulty and no modification. We grouped participants into three mutually exclusive functional groups according to their most impaired response for any of the four mobility tasks. Thus, the participants who reported difficulty with at least one mobility task were categorized as “disability” (DIFFICULTY). Those participants who reported no difficulty in any task but stated that they had modified at least one mobility task in the absence of difficulty were categorized as “preclinical disability for mobility” (PCD). Those participants who reported no difficulty and no task modification for all four tasks were categorized as “high function.”
Statistical Analyses
Baseline demographic and health-related characteristics for the 436 study participants were summarized and compared by education level at baseline, using the χ2 test for categorical variables and analysis of variance for continuous variables. We used polytomous logistic regression to examine the association between education and PCD at baseline, including all participants (n = 433). To assess the effect of education on incident preclinical mobility disability, we restricted the survival analyses to women who were high function (n = 174) at baseline. There were 21 women (12.1%) who developed disability before PCD and therefore were treated as censored observations in the time-to-event analyses of incident PCD, with the censoring time being the time of onset of difficulty. Kaplan–Meier survival plots were first used to visually assess the crude association between education status and incident preclinical mobility disability or disability over 11 years, with the onset time being the time at which the participant first reported preclinical disability or mobility disability. To account for the fact that the incidence outcomes were ascertained at each scheduled visit rather than on a continuous time scale, we used discrete-time proportional hazards models (22) to analyze the association between education and preclinical disability incidence, adjusting for the same set of covariates used in the cross-sectional analyses. We also tested for a statistical interaction between race and education. All analyses were performed using SAS statistical software, version 9.2.
RESULTS
Demographics
At baseline, 40.1% of the WHAS II women were categorized as high functioning, 21.7% as having preclinical mobility disability, and 38% as having mobility disability with one or more of the four mobility tasks (Table 1). We examined the distribution of several demographic and health characteristics according to level of education and found stepwise associations of increasing level of education with increasing level of income and decreasing proportion of African Americans. Women with higher levels of education were in general more likely to be married or never married but otherwise comparable to lower education groups with regards to age, number of chronic diseases, and self-efficacy (Table 1).
Table 1.
Demographic Characteristics by Years of Education Attained: Women's Health and Aging Study II
| Total (n = 436) | Education, 0–8 y (n = 59) | Education, 9–11 y (n = 65) | Education, 12 y (n = 134) | Education, >12 y (n = 178) | p Value* | |
| Age | 73.9 (2.8)† | 74.3 (2.8) | 74.0 (3.0) | 73.6 (2.6) | 74.0 (2.9) | .32 |
| Income | 24,502.8(20,305.8) | 17,980.2 (16,586.5) | 21,613.7 (17,972.8) | 25,287.1 (19,727.2) | 27,042.9 (22,101.1) | .022 |
| Income <12,000 | 32.4 (132) | 53.7 (29) | 33.3 (20) | 27.8 (35) | 28.6 (48) | .0072 |
| Income 12,000–36,000 | 44.6 (182) | 29.6 (16) | 51.7 (31) | 49.2 (62) | 43.5 (73) | |
| Income ≥36,000 | 23.0 (94) | 16.7 (9) | 15.0 (9) | 23.0 (29) | 27.9 (47) | |
| African American Race | 18.9 (82) | 40.7 (24) | 32.8 (21) | 13.4 (18) | 10.7 (19) | <.0001 |
| Marital status | ||||||
| Married | 38.1 (166) | 15.3 (9) | 27.7 (18) | 48.5 (65) | 41.6 (74) | <.0001 |
| Widowed | 45.0 (196) | 64.4 (38) | 69.2 (45) | 37.3 (50) | 35.4 (63) | |
| Separate or divorced | 7.8 (34) | 15.2 (9) | 3.1 (2) | 6.7 (9) | 7.9 (14) | |
| Never married | 9.2 (40) | 5.1 (3) | 0.0 (0) | 7.5 (10) | 15.2 (27) | |
| Low self-efficacy‡ | ||||||
| Disagree strongly | 60.5 (262) | 58.6 (34) | 49.2 (32) | 59.0 (79) | 66.5 (117) | .64 |
| Disagree somewhat | 27.5 (119) | 27.6 (16) | 35.4 (23) | 30.0 (40) | 22.7 (40) | |
| Agree somewhat | 3.0 (13) | 3.5 (2) | 3.1 (2) | 3.0 (4) | 2.8 (5) | |
| Agree strongly | 9.0 (39) | 10.3 (6) | 12.3 (8) | 8.2 (11) | 8.0 (14) | |
| Number of diseases | 2.9 (1.4) | 3.3 (1.4) | 2.8 (1.3) | 2.9 (1.5) | 2.8 (1.4) | .12 |
| Baseline mobility status | ||||||
| High function | 40.1 (174) | 28.8 (17) | 38.5 (25) | 37.6 (50) | 46.6 (82) | .091 |
| Preclinical mobility disability | 21.7 (94) | 20.3 (12) | 21.5 (14) | 27.8 (37) | 17.6 (31) | |
| Mobility disability | 38.1 (165) | 50.9 (30) | 40.0 (26) | 34.6 (46) | 35.8 (63) | |
| Chronic diseases | ||||||
| Angina | 60 (13.8) | 10 (17.0) | 6 (9.2) | 25 (18.7) | 19 (10.7) | .12 |
| Arthritis | 249 (57.1) | 39 (66.1) | 39 (60.0) | 74 (55.2) | 97 (54.5) | .41 |
| Cancer | 63 (14.5) | 7 (11.9) | 10 (15.4) | 21 (15.7) | 25 (14.0) | .91 |
| Congestive heart failure | 17 (3.9) | 4 (6.8) | 2 (3.1) | 5 (3.7) | 6 (3.4) | .67 |
| Diabetics | 38 (8.7) | 13 (22.0) | 5 (7.7) | 8 (6.0) | 12 (6.7) | .0015 |
| Hip fraction | 10 (2.3) | 0 (0.0) | 2 (3.1) | 3 (2.4) | 5 (2.8) | .62 |
| Hypertension | 224 (51.4) | 32 (54.2) | 37 (56.9) | 70 (52.2) | 85 (47.8) | .58 |
| Hearing problem | 73 (16.7) | 12 (20.3) | 8 (12.3) | 23 (17.2) | 30 (16.9) | .69 |
| Heart disease | 62 (14.3) | 5 (8.5) | 6 (9.2) | 23 (17.3) | 28 (15.7) | .23 |
| Lung disease | 31(7.1) | 2 (3.4) | 9 (13.9) | 8 (6.0) | 12 (6.7) | .11 |
| Myocardial infarction | 46 (10.6) | 14 (23.7) | 5 (7.7) | 12 (9.0) | 15 (8.4) | .0055 |
| Parkinson’s | 2 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (1.1) | .41 |
| Stroke | 24 (5.5) | 6 (10.2) | 2 (3.1) | 7 (5.2) | 9 (5.1) | .35 |
| Vision problem | 354 (81.2) | 49 (83.1) | 48 (73.9) | 107 (80.0) | 150 (84.3) | .30 |
Notes: *F test for continuous variable and chi-square test for categorical variable.
Mean (SD) for age and number of disease and % (n) for the rest.
Based on the response to the question, “Do you, in general, feel helpless?”
Cross-Sectional Association of Education With Preclinical Mobility Disability at Baseline
Women with 12 years of education were more likely to have higher prevalence of PCD, compared with those with more than 12 years, in both crude and multivariate-adjusted models. (Table 2) However, those with 0–8 or 9–11 years of education and those with more than 12 years were equally likely to report PCD at baseline. Low self-efficacy was not associated with PCD, whereas greater number of diseases was associated with higher prevalence of PCD. Age, race, income, and marital status were not associated with self-reported level of mobility function at baseline.
Table 2.
Cross-Sectional Association of Education Attainment and Preclinical Mobility Disability in Women's Health and Aging Study II (n = 433)
| Characteristics | Model I* |
Model II† |
||
| OR | (95% CI) | OR | (95% CI) | |
| Education (grades completed) | ||||
| 0–8 | 1.80 | (0.75–4.30) | 1.73 | (0.69–4.37) |
| 9–11 | 1.44 | (0.65–3.17) | 1.47 | (0.62–3.52) |
| 12 | 1.95 | (1.08–3.53) | 2.18 | (1.16–4.11) |
| >12 (reference group) | 1 | 1 | ||
| Age | 1.00 | (0.91–1.10) | ||
| African American race | 1.14 | (0.57–2.27) | ||
| Income <12,000 | 1.18 | (0.55–2.50) | ||
| Income 12,000–36,000 | 1.33 | (0.67–2.64) | ||
| Income ≥36,000 | 1 | |||
| Number of diseases | 1.32 | (1.08–1.62) | ||
| High self-efficacy‡ | 1.22 | (0.68–2.19) | ||
| Widowed | 1.07 | (0.58–1.98) | ||
| Separate/divorce | 1.90 | (0.74–4.91) | ||
| Never married | 0.70 | (0.23–2.16) | ||
| Married | 1 | |||
Notes: CI = confidence interval; OR = odds ratio.
Adjusted for age and race.
Adjusted for age, race, income, marital status, number of diseases, and high self-efficacy.
High self-efficacy if responded “strongly disagree” to the question, “Do you, in general, feel helpless?”
Longitudinal Association of Education With Preclinical Mobility Disability
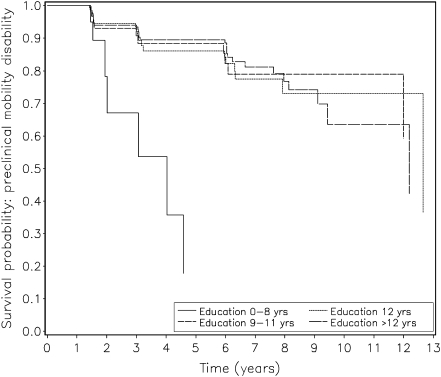
We next examined whether educational level predicted incident preclinical mobility disability. Forty-eight of the 174 women (27.6%) died. The study team was unable to locate an additional 8 (4.6%) and 29 (16.6%) were located but refused a follow-up interview. Participants in all three of these categories were censored in the survival analysis. First, we examined the association of educational attainment with incident PCD in mobility tasks. Of the 174 women who were in the high-function group at baseline, 37.9% (n = 66) developed PCD by the end of the 11 years of follow-up, with a marked increase in risk of developing PCD among those with education below ninth grade (Figure 1). Thus, women with a college education had a 10% risk of developing incident PCD by Year 4 versus a 65% risk among those with less than 9 years of education. The risk for incident PCD was comparable between African Americans and Caucasians (35.7% vs 38.4%, respectively, p = .89).
Figure 1.
Kaplan–Meier survival plot of the association between education attainment and incident preclinical mobility disability among women who were initially high functioning in the Women's Health and Aging Study (WHAS) II study.
In an age- and race-adjusted discrete-time proportional hazard model, compared with those with greater than 12 years of education, education level below ninth grade was an independent predictor of incident PCD (hazard ratio: 2.5; CI = 1.1–5.9; Table 3). After additional adjustment for income, marital status, number of diseases, and high self-efficacy, education level below ninth grade remained a significant predictor for incident PCD (hazard ratio: 3.1; CI = 1.2–7.7). The interaction between race and education was not significant.
Table 3.
Association of Educational Attainment and Incident Preclinical Mobility Disability in Women's Health and Aging Study II (n = 174)
| Characteristics | Model I* |
Model II† |
||
| HR | (95% CI) | HR | (95% CI) | |
| Education (grades completed) | ||||
| 0–8 | 2.5 | (1.1–5.9) | 3.1 | (1.2–7.7) |
| 9–11 | 1.3 | (0.6–2.7) | 2.0 | (0.9–4.4) |
| 12 | 1.2 | (0.6–2.1) | 1.3 | (0.7–2.5) |
| >12 (reference group) | 1 | 1 | ||
| Age | 1.1 | (1.0–1.2) | 1.1 | (1.0–1.2) |
| African American race | 1.1 | (0.5–2.2) | 0.9 | (0.4–1.9) |
| Income <12,000 | 1.4 | (0.7–2.8) | ||
| Income 12,000–36,000 | 1.0 | (0.5–1.9) | ||
| Income 36,000 | 1 | |||
| Number of diseases | 1.3 | (1.1–1.5) | ||
| High self-efficacy‡ | 1.2 | (0.7–2.1) | ||
| Widowed | 0.7 | (0.4–1.3) | ||
| Separate/divorce | 2.1 | (0.8–5.3) | ||
| Never married | 1.0 | (0.4–2.4) | ||
| Married | 1 | |||
Notes: CI = confidence interval; HR = hazard ratio.
Adjusted for age and race.
Adjusted for age, race, income, marital status, number of diseases, and high self-efficacy.
High self-efficacy if responded “strongly disagree” to the question, “Do you, in general, feel helpless?”
DISCUSSION
In this study, we found that among initially high-functioning older women, those with less than 9 years of education had a higher incidence of subsequent PCD independent of disease status, race, income, self-efficacy, and living arrangements. Our findings suggest that PCD may be important to understanding the manifestations of socioeconomic disparities in disability in late life. Furthermore, it offers insight into the early natural history and rapid trajectory of functional decline in those with low education. Previous published studies have documented the association between low education and activities of daily living (23), physical vulnerability (24), and disability (2,3,25), but no prior studies have shown an association with PCD. Education level may have its most important effect during the early stages of the disablement process. The higher education group may be more likely to alter this slope of decline using additional resources. For example, this group is more likely to access diagnostic screening and preventive measures compared with low-education groups (26).
The relationship between education and PCD may be best explained by the socioeconomic implications of low-education attainment. Those with lower education may be at higher risk of functional decline due to comorbidity and fewer resources with which to compensate. PCD reflects the attempt to compensate for impairments to preserve function and is a marker of early decline when people may benefit from interventions more than when disability in one or more domains is established.
Participants in the lowest educational status represent a phenotype at great risk for steep transitions to disability and death. This is a group that could benefit from early identification and disability prevention interventions, which could start with simple questions such as, “Have you changed the way you walk ½ mile or walk up steps?”
Limitations include that our study includes only African Americans and whites. It is unclear whether these findings might apply to other races or ethnicities. This cohort is concentrated in an urban/suburban section of Baltimore City and County. These results thus may not generalize to more rural areas. Strengths of the current study include a well-characterized community-based sample, easily reportable measures of disability, and longitudinal design from high functioning to disability.
In conclusion, among a cohort of previously high- functioning older women, low-education attainment was independently associated with incident PCD. Future studies should address interventions among these vulnerable women that focus on increasing access to resources to prevent functional loss.
FUNDING
This work was supported by National Institute of Aging at the National Institute of Health Grant # R01 AG11703-01A11, K08HS17956-01 (P.C.G.), Duke Endowment fund 6160-SP (P.C.G.), and 1KL2RR025006 (S.L.S.).
References
- 1.Melzer D, Izmirlian G, Leveille SG, Guralnik J. Educational differences in the prevalence of mobility disability in old age: the dynamics of incidence, mortality, and recovery. J Gerontol B Soc Sci. 2001;56(5):S294–S301. doi: 10.1093/geronb/56.5.s294. [DOI] [PubMed] [Google Scholar]
- 2.Koster A, Penninx BWJH, Bosma H, et al. Is there a biomedical explanation for socioeconomic differences in incident mobility limitation? J Gerontol A Biol Sci Med Sci. 2005;60(8):1022–1027. doi: 10.1093/gerona/60.8.1022. [DOI] [PubMed] [Google Scholar]
- 3.Coppin AK, Ferrucci L, Lauretani F, et al. Low socioeconomic status and disability in old age: evidence from the InChianti study for the mediating role of physiological impairments. J Gerontol A Biol Sci Med Sci. 2006;61(1):86–91. doi: 10.1093/gerona/61.1.86. [DOI] [PubMed] [Google Scholar]
- 4.Crimmins EM, Saito Y. Trends in healthy life expectancy in the United States, 1970–1990: gender, racial, and educational differences. Soc Sci Med. 2001;52(11):1629–1641. doi: 10.1016/s0277-9536(00)00273-2. [DOI] [PubMed] [Google Scholar]
- 5.Kanjilal S, Gregg EW, Yiling JC, et al. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971–2002. Arch Intern Med. 2006;166(21):2348–2355. doi: 10.1001/archinte.166.21.2348. [DOI] [PubMed] [Google Scholar]
- 6.Seeman T, Merkin SS, Crimmins E, Koretz B, Charlette S, Karlamangla A. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988–1994) Soc Sci Med. 2008;66(1):72–87. doi: 10.1016/j.socscimed.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steenland K, Henley J, Thun M. All-cause and cause-specific death rates by educational status for two million people in two American Cancer Society cohorts, 1959–1996. Am J Epidemiol. 2002;156(1):11–21. doi: 10.1093/aje/kwf001. [DOI] [PubMed] [Google Scholar]
- 8.Sudore RL, Yaffe K, Satterfield S, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. J Gen Intern Med. 2006;21(8):806–812. doi: 10.1111/j.1525-1497.2006.00539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baker DW, Wolf MS, Feinglass J, Thompson BA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167(14):1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 10.Petersen KL, Marsland AL, Flory J, Vortruba-Drzal E, Muldoon MF, Manuck SB. Community socioeconomic status is associated with circulating interleukin-6 and C-reactive protein. Psychosom Med. 2008;70(6):646–652. doi: 10.1097/PSY.0b013e31817b8ee4. [DOI] [PubMed] [Google Scholar]
- 11.Chang M, Cohen-Mansfield J, Ferrucci L. Incidence of loss of ability to walk 400 meters in a functionally limited older population. J Am Geriatr Soc. 2004;52(12):2094–2098. doi: 10.1111/j.1532-5415.2004.52570.x. [DOI] [PubMed] [Google Scholar]
- 12.Chaves PHM, Garrett ES, Fried LP. Predicting the risk of mobility difficulty in older women with screening nomograms: the Women's Health and Aging Study II. Arch Intern Med. 2000;160(16):2525–2533. doi: 10.1001/archinte.160.16.2525. [DOI] [PubMed] [Google Scholar]
- 13.Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. J Gerontol A Med Sci. 2000;55(1):M43–M52. doi: 10.1093/gerona/55.1.m43. [DOI] [PubMed] [Google Scholar]
- 14.Fried LP, Herdman SJ, Kuhn KE, Rubin G, Tarano K. Preclinical disability: hypotheses about the bottom of the iceberg. J Aging Health. 1991;3(2):285–300. [Google Scholar]
- 15.Fried LP, Bandeen-Roche K, Williamson JD. Functional decline in older adults: expanding methods of ascertainment. J Gerontol A Med Sci. 1996;51A(5):M206–M214. doi: 10.1093/gerona/51a.5.m206. [DOI] [PubMed] [Google Scholar]
- 16.Fried LP, Young Y, Rubin G, Bandeen-Roche K. Self-reported preclinical disability identifies older women with early declines in performance and early disease. J Clin Epidemiol. 2001;54(9):889–901. doi: 10.1016/s0895-4356(01)00357-2. [DOI] [PubMed] [Google Scholar]
- 17.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19(1):2–21. [PubMed] [Google Scholar]
- 18.Guralnik J. Screening the community-dwelling population for disability. In: Fried LP, Guralnik JM, Simonsick EM, Kasper JD, Lafferty ME, editors. The Women's Health and Aging Study Health and Social Characteristics of Older Women With Disability. Bethesda, MD: National Institute of Health; 1995. p. 177. [Google Scholar]
- 19.Frick KD, Zema CZ. Income Data Imputation and Poverty Coding for WHASI Data Set: Complete Interview and Screener-Only Data. 1997. pp. 1–36. [Google Scholar]
- 20.Hosmer DW, Hosmer T, Cessie SL, Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med. 1997;16(9):965–980. doi: 10.1002/(sici)1097-0258(19970515)16:9<965::aid-sim509>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 21.Clark DO, Patrick DL, Grembowski D, Durham ML. Socioeconomic status and exercise self-efficacy in late life. J Behav Med. 1995;18(4):355–376. doi: 10.1007/BF01857660. [DOI] [PubMed] [Google Scholar]
- 22.Prentice RL, Gloeckler LA. Regression analysis of grouped survival data with application to breast cancer data. Biometrics. 1978;34(1):57–67. [PubMed] [Google Scholar]
- 23.Sulander T, Martelin T, Sainio P, Rahkonen O, Nissinen A, Antti U. Trends and educational disparities in functional capacity among people aged 65–84 years. Int J Epidemiol. 2006;35(5):1255–1261. doi: 10.1093/ije/dyl183. [DOI] [PubMed] [Google Scholar]
- 24.Clark DO, Stump DO, Miller DK, Long JS. Educational disparities in the prevalence and consequence of physical vulnerability. J Gerontol B Soc Sci. 2007;62(3):S193–S197. doi: 10.1093/geronb/62.3.s193. [DOI] [PubMed] [Google Scholar]
- 25.Nordstrom CK, Diex Roux AV, Schulz R, Haan MN, Jackson SA, Balfour JL. Socioeconomic position and incident mobility impairment in the Cardiovascular Health Study. BMC Geriatr. 2007;7:11. doi: 10.1186/1471-2318-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Merkin S, Karlamangla A, Crimmins E. Education differentials by race and ethnicity in the diagnosis and management of hypercholesterolemia: a national sample of U.S. adults (NHANES 1999–2002) Int J Public Health. 2009;54(3):166–174. doi: 10.1007/s00038-008-7030-4. [DOI] [PMC free article] [PubMed] [Google Scholar]