Abstract
Chronic intermittent hypoxia (IH) during sleep can result from obstructive sleep apnea (OSA), a disorder that is particularly prevalent in obesity. OSA is associated with high levels of circulating leptin, cardiovascular dysfunction, and dyslipidemia. Relationships between leptin and cardiovascular function in OSA and chronic IH are poorly understood. We exposed lean wild-type (WT) and obese leptin-deficient ob/ob mice to IH for 4 wk, with and without leptin infusion, and measured cardiovascular indices including aortic vascular stiffness, endothelial function, cardiac myocyte morphology, and contractile properties. At baseline, ob/ob mice had decreased vascular compliance and endothelial function vs. WT mice. We found that 4 wk of IH decreased vascular compliance and endothelial relaxation responses to acetylcholine in both WT and leptin-deficient ob/ob animals. Recombinant leptin infusion in both strains restored IH-induced vascular abnormalities toward normoxic WT levels. Cardiac myocyte morphology and function were unaltered by IH. Serum cholesterol and triglyceride levels were significantly decreased by leptin treatment in IH mice, as was hepatic stearoyl-Coenzyme A desaturase 1 expression. Taken together, these data suggest that restoring normal leptin signaling can reduce vascular stiffness, increase endothelial relaxation, and correct dyslipidemia associated with IH.
Keywords: sleep apnea, heart, hypertrophy, vascular compliance, pulse-wave velocity, endothelial function, nitric oxide
obstructive sleep apnea (OSA) is increasingly being recognized as a risk factor in the obesity-related pathogenesis of cardiovascular disease. OSA independently contributes to the development of systemic and pulmonary hypertension (21, 39), right and left ventricular dysfunction (9, 10), and coronary artery disease and stroke (2), all of which are associated with failure of endothelium-dependent vasodilation (8, 13). Chronic intermittent hypoxia (IH), which has independently been shown to increase systemic arterial hypertension in rodents (14, 24) and humans (44), is a primary clinical feature of OSA. Our previous studies using a mouse model of IH reproduced sleep-related hypoxemia and sleep fragmentation comparable with the levels found in OSA (22, 35) and demonstrated that these animals develop moderate systemic and pulmonary hypertension and left- and right-sided ventricular hypertrophy (7).
Chronic IH-induced cardiovascular remodeling is thought to result from interactions between hemodynamic and inflammatory changes. The adipocytokine leptin has been a focus of these investigations as a result of the role of leptin in sympathetic activation (29), nitric oxide (NO) production (23, 30), inflammation, and oxidative stress, which can all affect cardiovascular function. Circulating leptin concentration is generally proportional to body fat mass, although studies have suggested that leptin levels are further elevated in OSA patients compared with weight-matched controls (12, 18) with a proportional increase with OSA severity (45). Whether hyperleptinemia in obesity and OSA serves a protective role or causes detrimental effects in the cardiovascular system is still under debate. While some suggest that elevated leptin induces oxidative stress and sympathetic overactivation (20, 42), others have found the insulin-sensitizing and lipid lowering actions of leptin to be cardioprotective (31, 46).
We have previously shown that vascular and myocardial abnormalities in leptin-deficient ob/ob animals are attributable to the disruption of intact leptin signaling independent of body weight (4, 28, 43). Because IH exposure leads to exacerbation of well-established cardiovascular risk factors of hyperlipidemia and insulin resistance (17, 26), and ob/ob animals lack leptin-mediated protection against these developments, we hypothesized that IH may disrupt normal leptin signaling in WT and result in worsening of lipid-induced injury in ob/ob, leading to further exacerbation of cardiovascular function. We predicted that leptin repletion could rescue such defects in both WT and ob/ob. Moreover, the inhibitory actions of leptin on fatty acid synthesis may also offer cardiovascular benefits in lean WT mice exposed to IH. To test these hypotheses, we treated C57BL6J wild-type (WT) and ob/ob animals with IH vs. room air control (RA), with or without leptin, resulting in eight groups of animals. We examined vascular compliance with noninvasive Doppler detection of pulse-wave velocity (PWV) and endothelium-dependent vasodilation response to acetylcholine (ACh). We also measured myocyte contractility and calcium transients in response to isoproterenol (ISO) stimulation and evaluated myocyte histology and morphometry.
MATERIALS AND METHODS
Animals and study design.
Male 10-wk-old, WT C57BL/6 and leptin-deficient ob/ob mice were purchased from The Jackson Laboratory (n = 15–20 per group; Bar Harbor, ME) and housed in a university animal facility with a 12-h:12-h light/dark cycle and allowed water and food ad libitum. Subsets of both WT and ob/ob strains were exposed to chronic IH, leptin treatment, or a combination of the two. This gives a total of eight experimental groups: 1) WT-RA, 2) WT-IH, 3) WT-RA + Leptin, 4) WT-IH + Leptin, 5) OB-RA, 6) OB-IH, 7) OB-RA + Leptin, and 8) OB-IH + Leptin.
IH exposure followed a previously described protocol (7). Briefly, animals exposed to IH were housed in custom cages that delivered an intermittent hypoxic stimulus [5–21% Fi(O2), 30-s cycles during the 12-h light cycle]. A constant flow of RA was delivered to the cages during the dark cycle. The average arterial partial pressure of O2 over each hypoxic cycle under this protocol was previously determined to be 51.7 ± 4.2 mmHg, whereas air delivered at the same rate as hypoxic gases produced an average arterial partial pressure of O2 of 99.7 ± 2.1 mmHg (41). IH or RA exposure lasted for 4 wk. Mouse leptin (Amgen, Thousand Oaks, CA) was delivered at 0.3 mg/kg per day via osmotic minipumps (Alzet, Cupertino, CA) that were surgically implanted 1 day before commencing hypoxia exposure as previously described (4). At the end of the protocol, animals underwent noninvasive studies before being euthanized. They were heparinized (0.1 ml heparin sodium sc) for 10 min and then anesthetized with isoflurane before the hearts and aortas were excised for tissue collection or cardiac myocyte isolation/aortic ring sectioning. Animal treatment and care was provided in accordance with institutional guidelines. The Institutional Animal Care and Use Committee of The Johns Hopkins University School of Medicine approved all protocols and experimental procedures.
Serum lipid biomarker determinations.
Blood samples were obtained by cardiac puncture at the time of euthanasia and centrifuged at 12,000 g for 10 min to separate plasma for measurements. Leptin was assayed in triplicate by a sandwich ELISA kit specific for the detection of mouse leptin (Millipore, Billerica, MA) per the manufacturer's instructions. Fasting serum total cholesterol (TC) and triglyceride (TG) levels were determined with kits from Wako Diagnostics and serum free fatty acid (FFA) levels with a FFA Quantification Kit from Biovision. Malondialdehyde (MDA) levels in plasma were determined using a colorimetric assay kit (Oxis International, Beverly Hills, CA) on the basis of reaction with N-methyl-2-phenylindole. Data were normalized to WT-RA as percentage of increase of MDA level.
Assessment of vascular compliance using PWV.
Animals were anesthetized with isoflurane (5% for induction and 1.5% for maintenance in 100% oxygen) and positioned supine on a temperature-controlled printed circuit board (Indus Instruments, Houston, TX) with legs strapped to electrocardiogram electrodes. Body temperature was monitored with a rectal probe (Physitemp, Clifton, NJ) and maintained at 37°C. Doppler spectrograms of aortic outflow were acquired with a 2 mm, 10-MHz pulsed Doppler probe (Indus Instruments). Thoracic aortic outflow and abdominal aortic flow profiles were captured. PWV was calculated as the quotient of the separation distance between the thoracic and abdominal probe sites and the time difference between pulse arrivals; time was recorded with respect to the R-wave of the ECG.
Assessment of endothelium-dependent vascular relaxation.
Excised aortas were cleaned in ice-cold Krebs-Ringer-bicarbonate solution containing the following (in mM): 118.3 NaCl, 4.7 KCl, 1.6 CaCl2, 1.2 KH2PO4, 25 NaHCO3, 1.2 MgSO4, and 11.1 dextrose. Equal-size (2 mm) aortic rings were carefully cut. Vascular tension changes were determined as previously described (50). Briefly, one end of the aortic rings was connected to a transducer, and the other to a micromanipulator, with the entire structure immersed in a bath chamber filled with constantly oxygenated Krebs buffer at 37°C. All vessels were mounted using a microscope, ensuring no damage to the smooth muscle or endothelium. The aortas were brought to an optimal resting tension using the micromanipulator, after which a dose of 60 mM KCl was administered, and repeated after a wash with Krebs buffer. After these washes, the vessels were allowed to equilibrate for 20–30 min in indomethacine (3 μM), and then phenylephrine (1 μM) was administered to cause vasoconstriction. A dose-dependent response with the muscarinic agonist ACh was then performed to check endothelial function, with increasing doses (10−9–10−5 M; half logs) administered when the vasorelaxation in response to the prior dose reached steady state. Relaxation response is calculated as a percentage of tension following preconstriction. Sigmoidal dose-response curves were fitted to data with the minimum constrained to 0.
Assessment of NO production in aortic tissue.
Excised aortas were cleaned and carefully dissected in ice-cold Krebs-HEPES buffer containing the following (in mM): 110 NaCl, 4.7 KCl, 25 NaHCO3, 1.2 MgSO4, 1.03 KH2PO4, 11.1 d-(+)-glucose, 20.0 HEPES, and 1.87 CaCl2, pH 7.4 at 24°C. Aortic rings (2–4 mm) were cut open and pinned, endothelial side up, in a Silastic-coated Petri dish. Tissues were incubated with fresh Krebs-HEPES buffer containing 1 nM of the NO-sensitive fluorescent dye 4-amino-5methylamino-2′,7′-diaminofluoroscein (DAF-FM) diacetate (Molecular Probes, Eugene, OR) for 30 min at 37°C, followed by washout of DAF-FM and a 20-min equilibration period. Fluorescence intensity data were collected using the Nikon NIS-Element suite, with excitation and emission wavelengths set to 485 and 510 nm, respectively. Fluorescence intensity was recorded every 30 s for a period of 15 min, and the slope of intensity change was calculated to indicate rate of NO production. Data is then normalized to WT-RA = 100%.
Cardiac myocyte isolation.
Cardiac myocytes were prepared from each treatment group as previously described (28, 51), with slight modifications. Briefly, excised hearts were perfused retrograde with Ca2+-free HEPES buffer containing (in mM): 134 NaCl, 4.0 KCl, 1.2 MgSO4, 1.2 NaH2PO4, 11 glucose, 1.2 HEPES, 1.0 2,3-butanedione monoxime (Sigma, St. Louis, MO) and digested with collagenase type 2 (1.2 mg/ml; Worthington Biochemicals, Lakewood, NJ) and protease type XIV (0.05 mg/ml; Sigma). Myocytes were then separated by mechanically mincing digested hearts, followed by filtration, centrifugation, and suspension in 0.125 mM1 Ca2+ Tyrode solution containing (in mM): 140 NaCl, 5 KCl, 1 MgCl2, 10 HEPES, 5.5 glucose, and 1.2 NaH2PO4 adjusted to a pH of 7.4 with NaOH. Myocytes were resuspended first in 0.250 mM Ca2+ Tyrode solution, then in 0.5 mM Ca2+ Tyrode solution, and finally stored in Tyrode solution containing 1.0 mM Ca2+. Functional studies were completed within 6 h after isolation.
Cell shortening and Ca2+ transient measurements.
Isolated myocytes were incubated with 5 μM Fura-2 AM (Molecular Probes) for 10 min then transferred to a Lucite chamber on the stage of an inverted microscope (Nikon TE 200). The stage was kept at 37°C and continuously perfused at ∼2 ml/min with Tyrode solution containing 2.4 mM Ca2+. Rod-shaped myocytes with clear striations and no spontaneous contraction were selected for recording. Myocytes were stimulated with suprathreshold voltage at 1 Hz, and their sarcomere lengths were recorded with an IonOptix iCCD camera (IonOptix, Milton, MA). Intracellular Ca2+ concentration ([Ca2+]i) indicated by the Fura-2 AM fluorescence intensity (FFI) was simultaneously determined by calculating the 360-nm/380-nm dual-excitation fluorescence ratio of the probe. Isoproterenol (Tocris, 10−9-10−7 M), a nonselective β-adrenergic receptor agonist, was administered in 10-fold increasing doses. Each administration took place when myocyte response to the previous dose reached a steady state. Peak shortening and peak calcium rise were calculated as the absolute difference in sarcomere length and FFI, respectively. β-Adrenergic responses to isoproterenol are calculated as percent increases from baseline shortening and calcium transient and fitted with a sigmoidal dose-response curve with the bottom constrained to 0.
Echocardiographic evaluation.
In vivo cardiac geometry and function were assessed by transthoracic echocardiography (Sonos 5500, 15 MHz linear transducer; Agilent, Palo Alto, CA) in mice anesthetized with 1–2% isoflurane. LV end-systolic and -diastolic cross-sectional diameter and the mean of septal and posterior wall thicknesses were determined from an average of three to five cardiac cycles in M-mode images. LV fractional shortening and ejection fraction were calculated and LV mass was determined using a cylindrical model as previously described (4).
Histological evaluation of tissue and cellular morphometry and apoptosis.
Myocyte dimensions were determined from digitized images of hematoxylin and eosin-stained myocardium and analyzed using ImageJ (NIH, Bethesda, MD). Myocardial fibrosis was determined by Masson trichrome staining of paraffin-embedded sections and semiquantitatively rated by a blinded pathologist. TUNEL assay was also performed in heart tissue sections using the FragEL DNA Fragmentation Detection Kit (Calbiochem, Temecula, CA) per the manufacturer's instructions.
Statistical analysis.
All values are expressed as means ± SE. The effect of hypoxia and leptin within each animal strain was assessed with two-way ANOVA with Bonferroni post hoc tests. P values <0.05 were considered to be statistically significant. Unpaired, two-tailed t-tests were used to determine statistical significance and P value of differences between WT and ob/ob mice, with the Welch correction applied when appropriate. GraphPad Prism 5.0 (La Jolla, CA) and SigmaPlot 11 (Systat Software, Chicago, IL) were used for statistical analysis.
RESULTS
Chronic IH inhibits body weight gain in WT but not in ob/ob.
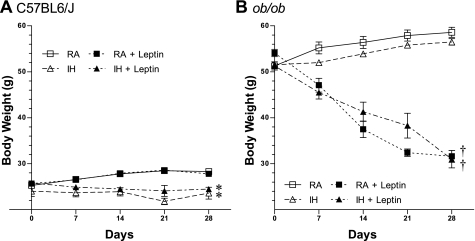
We exposed eight groups of mice in to 4 wk of IH in a 2 × 2 × 2 design as described above to assess the contribution of leptin in the cardiovascular abnormalities associated with an IH model of OSA. WT mice exposed to 4 wk of IH showed no change in body weight over time (23.6 ± 1.3 g at day 28 vs. 24.0 ± 1.1 g at day 0; P = NS), whereas normoxic WT mice continued to gain weight (28.3 ± 0.6 g at day 28 vs. 25.3 ± 0.5 g at day 0; P < 0.01) (Fig. 1A). Along with lower body weight, WT-IH mice displayed a decrease in serum leptin concentration compared with RA control group (1.6 ± 0.2 in WT-IH vs. 4.3 ± 1.1 ng/ml in WT-RA, P = 0.06). Exogenous leptin treatment significantly elevated circulating leptin levels in WT-IH animals (8.1 ± 0.9 ng/ml, P < 0.05 vs. WT-RA, P < 0.001 vs. WT-IH) but not in WT mice exposed to RA (6.5 ± 0.9 ng/ml, P = 0.16 vs. WT-RA). Body weight trends were unaltered by exogenous leptin administration in WT animals, regardless of hypoxia treatment.
Fig. 1.
Body weight over time. Body weight recorded over the 28-day treatment period for C57BL6/J WT mice (A) and ob/ob leptin-deficient mice (B) exposed to room air (RA) (□, solid line), RA + leptin (■, dotted line), intermittent hypoxia (IH) (▵, dashed line), and IH + leptin (▴, dot-dash line). Values are means ± SE, n = 4–12/group. *P < 0.01 vs. RA; †P < 0.001 vs. no leptin.
Leptin treatment of ob/ob mice significantly decreased body weight as expected (30.5 ± 0.7 g at day 28 vs. 54.3 ± 0.9 g at day 0; P < 0.0001), whereas control ob/ob animals continued to gain weight (58.6 ± 1.1 g at day 28 vs. 51.3 ± 0.9 g at day 0; P = 0.0001) (Fig. 1B). Hypoxia treatment did not inhibit body weight gain in ob/ob mice as seen in the WT. Concomitant hypoxia exposure and leptin repletion did not decrease the body weights of ob/ob below that of leptin treatment alone (−43.8 ± 1.3% weight change in OB-RA + Leptin vs. −39.7 ± 3.3% weight change in OB-IH + Leptin, P = NS) as shown in Table 1.
Table 1.
Basic characteristics for the eight groups
| Leptin Levels at day 28 | BW/TL, g/mm | HW/TL, mg/mm | HW/BW, mg/g | Leptin, ng/ml |
|---|---|---|---|---|
| C57BL6/J | ||||
| RA | 1.60 ± 0.03 | 7.18 ± 0.16 | 4.50 ± 0.08 | 4.3 ± 1.1 |
| RA + Leptin | 1.59 ± 0.02 | 7.25 ± 0.11 | 4.52 ± 0.08 | 6.5 ± 0.9 |
| IH | 1.41 ± 0.04* | 6.87 ± 0.23 | 4.88 ± 0.07* | 1.6 ± 0.2 |
| IH + Leptin | 1.46 ± 0.05* | 7.01 ± 0.17 | 4.88 ± 0.06* | 8.1 ± 0.9†‡ |
| ob/ob | ||||
| RA | 3.38 ± 0.05§ | 8.01 ± 0.17§ | 2.38 ± 0.04§ | ND§ |
| RA + Leptin | 1.97 ± 0.07†§ | 7.45 ± 0.28 | 3.80 ± 0.25†§ | 6.7 ± 0.8† |
| IH | 3.22 ± 0.10§ | 7.58 ± 0.20§ | 2.37 ± 0.08§ | ND§ |
| IH + Leptin | 1.82 ± 0.09†§ | 7.37 ± 0.18 | 4.12 ± 0.16†§ | 7.0 ± 1.0† |
Values are means ± SE, n = 4–12/group. See material and methods for calculations.
RA, room air; IH, intermittent hypoxia; BW, body weight; TL, tibia length; HW, heart weight.
P < 0.05 vs. RA,
P < 0.05 vs. no leptin,
Significant interaction between IH and leptin;
P < 0.05 ob/ob vs. C57BL6/J wild-type (WT). ND = not detectable.
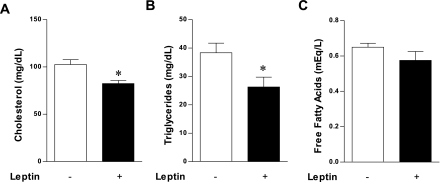
Leptin lowered serum lipids and hepatic stearoyl-coenzyme A desaturase (SCD-1) in WT exposed to IH.
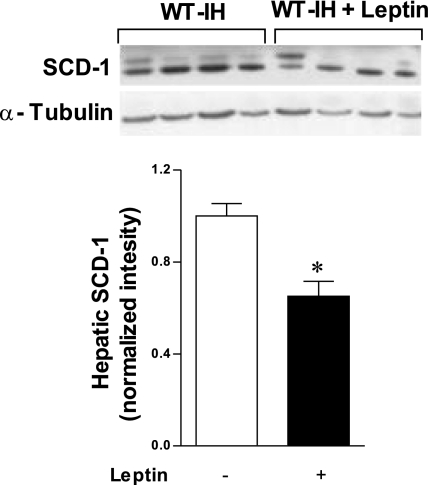
Lack of leptin and exposure to IH both lead to dyslipidemia, another well-documented risk factor for impaired vascular compliance and endothelial dysfunction. The lipid-lowering effects of leptin repletion in ob/ob animals are well established, but whether leptin has an inhibitory effect on IH-induced hyperlipidemia is not known. Fasting serum TC was lower in WT-IH + Leptin vs. IH mice (82.6 ± 3.2 vs. 102.6 ± 5.1 mg/dl, P < 0.001), as were the total TGs (26.3 ± 3.5 vs. 38.3 ± 3.4 mg/dl, P < 0.05) (Fig. 2). In WT, total serum FFA was not significantly altered although there was a slight trend toward decrease (0.58 ± 0.05 vs. 0.65 ± 0.02 meq/l, P = 0.21). Hepatic protein expression of SCD-1, which catalyzes monounsaturated fatty acid synthesis and is transcriptionally inhibited by leptin, was also lower in IH + Leptin vs. IH by Western blot (0.65 ± 0.07 vs. 1.00 ± 0.05 arbitrary units; P < 0.01; Fig. 3). On the basis of these findings, we suspect that leptin antagonizes the pathophysiological effects of IH by suppressing IH-induced vascular stiffness through a lipid-reducing mechanism.
Fig. 2.
Leptin lowers serum cholesterol and triglycerides in hypoxic wild-type (WT) animals. Hypoxia-induced elevations in fasting serum total cholesterol (A) and total triglycerides (B) were lowered with exogenous leptin treatment, whereas serum free fatty acids (C) tended toward a decrease with leptin treatment. Values are means ± SE, n = 5/group. *P < 0.05 vs. no exogenous leptin.
Fig. 3.
Leptin suppressed hepatic SCD-1 expression in hypoxic WT animals SCD-1. Hepatic expression of SCD-1 was attenuated with leptin treatment in hypoxia-exposed WT mice. Values are means ± SE, n = 5/group. *P < 0.05 vs. no exogenous leptin.
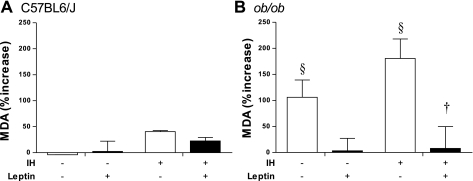
Leptin decreased lipid peroxidation in ob/ob exposed to IH.
Because oxidative stress is a major factor affecting the vasculature, we measured lipid peroxidation-derived oxidative stress using serum MDA measurement, normalized to WT-RA (Fig. 4). There was no statistically significant change in serum MDA levels among the WT groups. Lipid peroxidation was significantly elevated in ob/ob compared with WT mice (106 ± 33% in OB-RA vs. 0 ± 12% in WT-RA; P < 0.05). Leptin repletion in ob/ob led to significantly decreased serum MDA by two-way ANOVA (P < 0.05). Post hoc analysis demonstrated significance of leptin treatment in the ob/ob hypoxic comparison (180 ± 37% in OB-IH vs. 8 ± 42% in OB-IH + Leptin; P < 0.05) but not in the normoxic comparison (106 ± 33% in OB-RA vs. 3 ± 24% in OB-RA + Leptin; P = 0.414).
Fig. 4.
Leptin lowered lipid peroxidation in ob/ob animals exposed to IH. Serum malondialdehyde (MDA) levels from C57BL6/J WT mice (A) and ob/ob leptin-deficient mice (B) were measured as markers of lipid peroxidation. Values are means ± SE, n = 3/group. †P < 0.05 vs. no leptin, §P < 0.05 ob/ob vs. WT.
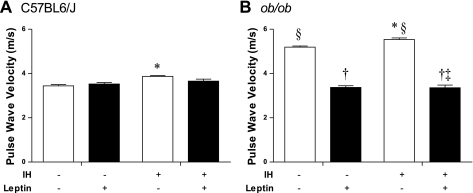
Leptin preserves vascular compliance after IH in both ob/ob and WT.
We first assessed in vivo vascular stiffness using PWV. WT-IH mice had increased vascular stiffness compared with WT-RA, as reflected by higher PWV (3.87 ± 0.04 vs. 3.44 ± 0.06 m/s; P < 0.001) (Fig. 5). Interestingly, vascular stiffness induced by hypoxic exposure was attenuated by leptin administration. There was no significant difference in WT-RA + Leptin and WT-IH + Leptin (3.53 ± 0.07 vs. 3.68 ± 0.08 m/s; P = NS; P = NS vs. WT-RA in both cases). As expected (43), leptin-deficient ob/ob mice had markedly increased PWV compared with WT (5.19 ± 0.05 m/s; P < 0.0001). OB-IH mice had even further elevation in PWV (5.54 ± 0.07 m/s; P < 0.05 vs. OB-RA). Leptin repletion dramatically decreased PWV in both OB-IH + Leptin and OB-RA + Leptin to WT-RA levels (3.37 ± 0.08 vs. 3.36 ± 0.12 m/s; P = NS; P < 0.0001 vs. OB-RA and P = NS vs. WT-RA in both cases). These results suggest that intact leptin-dependent signaling is necessary to prevent IH-induced vascular stiffness.
Fig. 5.
Pulse-wave velocity (PWV) as a measure of vascular compliance. PWV measurements of C57BL6/J WT mice (A) and ob/ob leptin-deficient mice (B) were recorded on day 28 to assess in vivo vascular compliance. Increased PWV indicates increased vascular stiffness. Values are means ± SE, n = 8–20/group. P < 0.05 vs. RA, †P < 0.05 vs. no leptin, ‡significant interaction between IH and leptin treatment; §P < 0.05 ob/ob vs. WT.
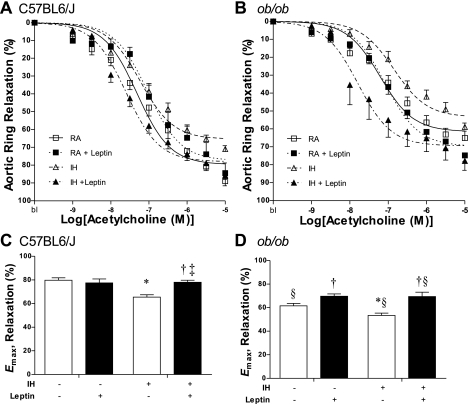
Restoring leptin signaling reverses effect of IH on vascular reactivity.
Next we correlated in situ endothelial-dependent and -independent aortic ring responses to our in vivo findings. Maximum aortic ring relaxation responses to ACh closely correlated with those for PWV (Fig. 6). Maximum ring relaxation was attenuated in WT-IH vs. WT-RA (Emax, 65 ± 2 vs. 80 ± 2%; P < 0.001), with no significant change in half-maximal effective concentration of ACh (log EC50: −7.1 ± 0.06 vs. −7.1 ± 0.05 M; P = NS). Leptin treatment of WT animals showed no significant change in aortic-ring maximum response to ACh (Emax 77 ± 3%, P = NS vs. WT-RA; log EC50: −6.9 ± 0.07 M; P < 0.05 vs. WT-RA) but restored the decreased relaxation response in WT exposed to IH (Emax 78 ± 2%, P < 0.001 vs. WT-IH, P = NS vs. WT-RA). The half-maximal effective concentration of ACh was decreased with combined leptin and IH exposure (log EC50: −7.5 ± 0.05 M; P < 0.05 vs. WT-IH). OB-RA had attenuated ring relaxation response to ACh compared with WT-RA (Emax 61 ± 2%, P < 0.001), and IH exposure led to further attenuation (Emax 53 ± 2%, P < 0.05 vs. OB-RA; log EC50: −6.7 ± 0.06 M; P < 0.05 vs. OB-RA). OB-RA + Leptin and OB-IH + Leptin showed improved responses to ACh vs. untreated OB-RA and OB-IH (Emax 70 ± 2 and 69 ± 4%; log EC50: −7.0 ± 0.05 and −7.6 ± 0.06 M). To confirm that the change in relaxation induced by IH was endothelial dependent, we measured endothelial-independent relaxation by sodium nitroprusside. There was no difference in endothelial-independent relaxation among groups (Emax 49.40 ± 18.14% in WT-IH vs. 60.52 ± 20.15% in OB-IH vs. 63.70 ± 18.73% in OB-IH + Leptin; P = NS). The parallel finding in endothelium-dependent relaxation response and PWV measurements suggest that disruption of endothelial function is responsible for reduced vascular compliance in ob/ob animals and animals exposed to IH.
Fig. 6.
Endothelium-dependent relaxation response to acetylcholine (ACh). Aortic rings were subjected to increasing doses of ACh for determination of endothelium-dependent relaxation function. Values are means ± SE, n = 10–20/group. Sigmoidal dose-response curves were fitted for C57BL6/J WT mice (A) and ob/ob leptin-deficient mice (B) exposed to RA (□, solid line), RA + leptin (■, dotted line), IH (▵, dashed line), and IH + leptin (▴, dot-dash line) with the bottom values constrained to 0. The maximum relaxation responses determined from the fitted curve were compared for WT (C) and ob/ob animals (D). Half-maximal effective concentrations of ACh were also compared for WT (E) and ob/ob animals (F). *P < 0.05 vs. RA, †P < 0.05 vs. no leptin, ‡significant interaction between IH and leptin; §P < 0.05 ob/ob vs. WT.
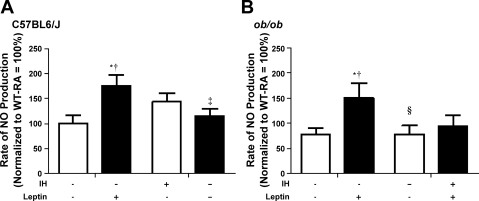
Ex vivo vascular NO production rate was not enhanced in leptin-treated IH animals.
NO has been proposed as a mechanistic link between endothelial function and vascular compliance (49), and leptin stimulation of both vascular smooth muscle and endothelial cells has been shown to increase NO production (23, 38). Therefore, we examined NO production in vascular tissue isolated from the eight groups of animals (Fig. 7). In WT mice, IH did not significantly affect ex vivo vascular tissue ability to produce NO (143 ± 18 vs. 100 ± 17%, P = NS vs. WT-RA). Exogenous leptin treatment increased aortic tissue rate of NO production (176 ± 21%, P < 0.001 vs. WT-RA), but this effect was absent with concomitant IH exposure (121 ± 13%, P < 0.05 vs. WT-RA + Leptin, P = NS vs. WT-IH). NO production rates were similar between normoxic WT and ob/ob tissue (75 ± 10%, P = NS vs. WT-RA), and IH exposure did not lead to a significant change in the ob/ob (78 ± 12%, P = NS vs. OB-RA). Leptin repletion enhanced the rate of NO production in normoxic ob/ob rings (OB-RA + Leptin: 150 ± 29%, P < 0.001 vs. OB-RA) but not in hypoxic rings (OB-IH + Leptin: 94 ± 23%, P < 0.05 vs. OB-RA + Leptin, P = NS vs. OB-IH). Importantly, these negative findings emphasize that, although NO production is affected by leptin signaling, it is not the primary mechanism for the suppression of leptin of vascular stiffness induced by IH.
Fig. 7.
Nitric oxide (NO) production. Rate of NO production by aortic tissues from C57BL6/J WT mice (A) and ob/ob leptin-deficient mice (B) were determined using 4-amino-5methylamino-2′,7′-diaminofluoroscein diacetate fluorescence. Values are means ± SE, n = 6–14/group. *P < 0.05 vs. RA, †P < 0.05 vs. no leptin, ‡significant interaction between IH and leptin; §P < 0.05 ob/ob vs. WT.
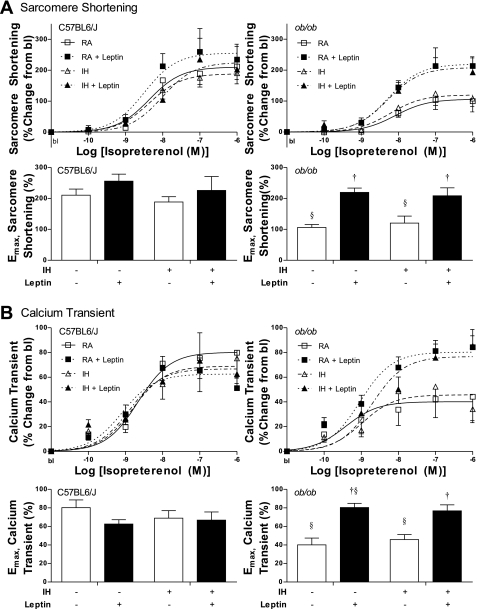
Cardiac myocyte response to β-adrenergic stimulation was attenuated in ob/ob but unaltered with IH.
In addition to vascular function, we examined whether cardiac myocyte function is compromised with IH. Contrary to our initial hypothesis, IH did not significantly alter basal or isoproterenol-stimulated peak sarcomere shortening in WT mice (Emax 189 ± 17% vs. 211 ± 20%, P = NS) (Fig. 8A). Exogenous leptin treatment in WT did not alter myocyte response to isoproterenol (Emax 256 ± 23%; P = NS vs. WT-RA), nor did combination treatment in the WT-IH + Leptin group (Emax 225 ± 45%; P = NS vs. WT-RA). Consistent with our previous results (28), sarcomere shortening of myocytes isolated from ob/ob mice had attenuated response to isoproterenol (Emax 106 ± 10%, P < 0.05 vs. WT), and this depressed β-adrenergic response was restored in OB-RA + Leptin mice (Emax 220 ± 14%; P < 0.0001 vs. OB-RA, P = NS vs. WT-RA). The depressed response to isoproterenol in ob/ob was unaltered with hypoxia exposure (Emax 120 ± 23%) and again restored to normal with leptin repletion (Emax 209 ± 26%; P < 0.0001 vs. OB-IH, P = NS vs. WT-RA). Percent calcium transient increase with isoproterenol stimulation followed the same trends as percent sarcomere shortening increase from baseline (Fig. 8B).
Fig. 8.
Cardiac myocyte contractile response to β-adrenergic stimulation with isoproterenol. Percent increase from baseline for peak sarcomere shortening (A) and calcium transient (B) in response to all isoproterenol concentrations are plotted for WT and for ob/ob mice exposed to RA (□, solid line), RA + leptin (■, dotted line), IH (▵, dashed line), and IH + leptin (▴, dot-dash line). Response curves were fitted with the baseline constrained to 0. The maximum relaxation responses determined from the fitted curves were compared. †P < 0.05 vs. no leptin; §P < 0.05 ob/ob vs. WT.
IH did not cause significant cardiac remodeling in the WT.
Although prior studies have suggested that right ventricular and LV remodeling are in response to IH (7), we did not observe significant cardiac myocyte function deterioration following 4 wk of IH in this study. We confirmed the lack of significant cardiac remodeling by echocardiography (Table 2). Histological evaluation of myocardial tissue (Fig. 9) revealed no difference in myocyte size (10.04 ± 0.39 μm in WT-RA vs. 10.71 ± 0.38 μm in WT-IH, P = NS), interstitial fibrosis (none to minimal in all sections from both groups), and apoptosis evaluated by TUNEL staining.
Table 2.
Echocardiography parameters for WT ± IH
| RA (n = 8) | Hypoxia (n = 7) | P | |
|---|---|---|---|
| HR, beats/min | 510.2 ± 23.5 | 493.4 ± 21.6 | 0.61 |
| LVEDD, mm | 3.04 ± 0.13 | 3.26 ± 0.14 | 0.27 |
| LVESD, mm | 1.47 ± 0.12 | 1.63 ± 0.07 | 0.26 |
| RWT | 0.51 ± 0.03 | 0.49 ± 0.03 | 0.61 |
| LV Mass, mg | 68.12 ± 5.53 | 79.43 ± 5.91 | 0.19 |
| FS, % | 52.10 ± 2.46 | 49.86 ± 0.95 | 0.42 |
| EF, % | 76.63 ± 2.36 | 74.81 ± 0.96 | 0.49 |
Values are means ± SE. Heart rate (HR), left ventricle end diastolic (LVEDD) and systolic (LVESD) diameters, relative wall thickness (RWT), calculated left ventricle (LV) mass, fractional shortening (FS), and ejection fraction (EF) are all calculated from echocardiography measurements. See materials and methods for calculations. Measures for the two groups are compared with unpaired, two-tail t-tests; P values are listed.
Fig. 9.
Histological evaluation of myocardial tissues from WT ± IH. Representative images of hematoxylin and eosin (A), Masson trichrome (B), and TUNEL stains (C) of cardiac tissues from C57BL6/J WT control animals and those exposed to 4-wk IH demonstrate no significant myocyte hypertrophy and apoptosis, nor development of fibrosis in response to hypoxia.
DISCUSSION
The major new finding of this study is that intact leptin signaling is essential to maintain normal vascular compliance under a hypoxic environment. Our studies clearly demonstrate that 1) leptin improves IH-induced dyslipidemia, 2) chronic IH exposure increases aortic vascular stiffness and attenuates ACh-induced endothelium-dependent vasodilation response, 3) leptin-deficient ob/ob mice show the same defects at baseline, which are aggravated with IH exposure, and 4) administration of exogenous leptin restores vascular compliance by improving lipid profiles via a mechanism independent of the NO pathway.
Previous studies have shown that 5-day IH exposure elevates circulating leptin levels (34), but this likely feeds back to prevent additional weight gain, thus resulting in lower body weight and explaining the lower leptin level observed at the 4-wk time point in this study. Vascular compliance and endothelial relaxation response to ACh were compromised in the hypoxic animals but were restored with exogenous leptin repletion, despite the lack of difference in final body weight between WT-IH and WT-IH + leptin groups. In WT mice, IH exposure led to attenuation of weight gain along with lower serum leptin concentrations compared with WT-RA. Consistent with our recent findings that leptin antagonism increases vascular stiffness (43), we conclude that intact leptin signaling is essential in maintaining normal vascular compliance independent of body weight.
In the ob/ob mice, the effect of IH in preventing body weight gain was lost, suggesting that inhibitory effect of hypoxia on weight may be leptin related. Leptin repletion in ob/ob with concomitant hypoxia exposure did not decrease the body weights of ob/ob below that of leptin treatment alone; however, it is difficult to assess the inhibitory effect of hypoxia on weight in this case because ob/ob mice given leptin were actively losing weight. Leptin repletion in ob/ob animals restored vascular properties toward WT-RA levels as would be expected and previously demonstrated (50). Importantly, IH exacerbated vascular abnormalities found in the ob/ob. The effects of IH and leptin deficiency on vascular reactivity seem to be additive but not multiplicative in this case. More importantly, leptin repletion entirely restored the vascular compliance in OB-IH to WT-RA levels, not just to WT-IH levels, and improved endothelial relaxation response. These results are consistent with our findings in the WT, where exogenous leptin rescues the vascular damage induced by hypoxia.
In an earlier characterization of this IH model, heart weight/body weight (HW/BW) ratio was increased in WT-IH compared with WT-RA although this observation was mostly driven by lower body weight in the WT-IH, rather than an increase in heart weight itself (7). In the present study, we normalized HW to tibia length (TL), which is a more consistent marker for lean body mass. We found that the HW/TL ratio was similar between WT-IH and WT-RA, and echocardiography showed no significant changes in LV wall thickness, chamber dimension, and ejection fraction. Taken together with the finding that myocyte size and mechanistic properties were unaltered, these results suggest no significant cardiac remodeling with 4-wk exposure to this IH protocol. Others have shown that mice exposed to a similar model of IH exhibited earlier and greater changes in aortic gene expression than those found in heart and lung tissues (15) although the exact timing and effects between different models are difficult to consolidate. Consistent with our prior findings, ob/ob animals showed higher HW/TL ratio compared with WT, and isolated cardiac myocytes demonstrated depressed response to β-adrenergic stimulation (4, 28). Both were restored with leptin repletion (4, 28), but IH did not alter this response.
Because NO had been shown to be affected by leptin in the vasculature and is an important mediator of endothelial relaxation, we first examined the rate of NO production in ex vivo vascular rings. The lack of enhanced rates of NO production by leptin in the WT and ob/ob groups exposed to IH suggests that NO is unlikely to be the mechanism by which leptin protects against IH-induced vascular dysfunction, even though leptin treatment in RA controls significantly increased the rate of NO production, consistent with prior studies (47).
Other factors contributing to vascular remodeling include altered lipid profile and changes in insulin sensitivity. Because of our results showing that leptin repletion corrects IH-induced altered lipid profile, we propose that the vascular protective effects of leptin may be a direct consequence of suppressing IH-induced hyperlipidemia. Chronic IH has been shown to cause or worsen lipid profile and insulin resistance. Studies have shown, in both WT and ob/ob, that IH exposure significantly increases cholesterol, phospholipids, and TG content, along with increased sterol regulatory element binding protein-1 (SREBP-1) expression (17, 25, 26). Leptin can prevent excess lipid accumulation in peripheral tissues by repressing de novo lipogenesis via decrease in fatty acid synthase gene expression and upregulating β-oxidation (46), thus preventing lipotoxicity and reducing serum TG and FFA concentrations (46). Leptin administration also inhibits de novo cholesterol synthesis and decreases intestinal cholesterol absorption (16, 48). We confirmed that altered lipid profiles in IH-exposed WT can be rescued by administration of leptin, suggesting correction of dyslipidemia as a mechanism of vascular protection by leptin. Whether IH can induce ectopic lipid deposition in the vasculature remains to be determined although the protective effect of leptin in this model stems at least in part from reducing sources of FFA and cholesterol in the serum. In addition, leptin is now considered as an inhibitor of SREBP-1 and SCD-1 expressions (5, 19). We have shown that hepatic expression of SCD-1 was suppressed in our model with leptin treatment in WT-IH animals. Genetic models of SCD-1 deficiency have demonstrated reduced body adiposity, increased insulin sensitivity, and resistance to diet-induced obesity in addition to decreased expression of lipid synthesis genes and low levels of TGs in the low- and very-low-density lipoprotein fractions compared with their WT counterparts (33). Given these results, we propose that leptin maintains a vascular-compliance lipolytic-dependent pathway independent of NO signaling.
Clinical implications.
In the clinical setting, leptin has been successfully used to treat forms of lipodystrophy (32) in addition to correcting rare congenital leptin deficiency (27). A recent report enhances the clinical potential of leptin by demonstrating that hyperleptinemia can reverse the consequences of a total lack of insulin and thus its possible usage in treating type 1 diabetes (53). The antihyperglycemic effects of leptin treatment are no longer limited to the interpretation that leptin potentiates residual levels of endogenous insulin but that it can replace some actions of insulin by suppressing glucagon action on the liver and enhancing the insulinomimetic actions of insulin-like growth factor 1 on skeletal muscle. The impact of these actions of leptin on the cardiovasculature warrants further investigation.
In this study, we described a novel effect for leptin signaling in reducing IH-induced vascular stiffness and endothelial dysregulation, associated with improved dyslipidemia. Patients exhibiting oxyhemoglobin desaturations at night, such as those with the OSA syndrome, show higher plasma TG and low-density lipoprotein cholesterol levels compared with subjects without hypoxemia (40). Chronic IH is associated with dyslipidemia and overexpression of hepatic SCD-1 in both humans and mice alike; SCD-1 deficiency attenuates IH-induced and high-fat-diet-induced dyslipidemia and atherosclerosis in mice (40). Given that leptin transcriptionally inhibits SCD-1, it is conceivable that leptin induction in a hypoventilatory state could serve a compensatory role by inhibiting rising lipid levels. Other benefits of normalizing leptin signaling may include maintaining tissue oxygenation by promoting angiogenesis and maintaining endothelium integrity (1, 6). This benefit may be lost in obese patients as central leptin resistance precludes the use of leptin to induce weight loss and normalize lipid profile. Emerging evidence suggests that the peripheral actions of leptin on cardiac myocytes and endothelial cells are also attenuated in diet-induced obesity (36, 37). Our results corroborate other evidence that suggests hyperleptinemia found in obesity and sleep-disordered breathing may be more reflective of a general state of leptin resistance. In such a state, treating with additional leptin would not be effective; however, restoring leptin sensitivity may be an important target for treating dyslipidemia and vascular dysfunction in cardiovascular diseases associated with sleep apnea and obesity.
Conclusions.
We have established that chronic IH increases vascular stiffness and compromises endothelial function in WT and ob/ob mice. Remarkably, leptin repletion not only restored normal vascular properties in both IH-exposed and control ob/ob mice, but also attenuated IH-induced vascular abnormalities in the WT. Thus impaired leptin signaling may represent an important mechanism of IH-induced vascular injury. The inhibitory actions of leptin on fatty acid synthesis may provide vascular benefits in sleep apnea and hyperlipidemia and offer new therapeutic strategies in patients with these conditions.
GRANTS
This study was supported by NIH/NHLBI R01-HL077785 (to C. O'Donnell); R01-AG021523 (to D. Berkowitz), R01-HL80105 and American Heart Association Grant-in-Aid 10GRNT3360001 (to V. Polotsky); SCCOR 5P50HL084945 (to V. Polotsky); NIH 5T32-HL007227 (to V. Watts); the German Research Foundation (DFG) Research Fellowship grant RE 2842/1-1 (to C. Reinke); the WW Smith Charitable Trust (to L. Barouch); American Heart Association Beginning Grant-In-Aid 09BGIA2250379 (to L. Barouch); American Diabetes Association 1-10-BS-11 Research Award (to L. Barouch); and K08-HL076220 (to L. Barouch).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
ACKNOWLEDGMENTS
The authors thank Konrad Vandegaer, Lakshmi Santhanam, Alanah K. Webb, and Jonathan Jun for technical assistance and expertise. Andre Camara is presently at Metro West Medical Center, Framingham Union Hospital, Framingham, MA. Jill Larson is presently at Northwestern Feinberg School of Medicine, Chicago, IL.
REFERENCES
- 1. Anagnostoulis S, Karayiannakis AJ, Lambropoulou M, Efthimiadou A, Polychronidis A, Simopoulos C. Human leptin induces angiogenesis in vivo. Cytokine 42: 353– 357, 2008 [DOI] [PubMed] [Google Scholar]
- 2. Arzt M, Young T, Finn L, Skatrud JB, Bradley TD. Association of sleep-disordered breathing and the occurrence of stroke. Am J Respir Crit Care Med 172: 1447– 1451, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Balasubramaniyan V, Nalini N. The potential beneficial effect of leptin on an experimental model of hyperlipidemia, induced by chronic ethanol treatment. Clin Chim Acta 337: 85– 91, 2003 [DOI] [PubMed] [Google Scholar]
- 4. Barouch LA, Berkowitz DE, Harrison RW, O'Donnell CP, Hare JM. Disruption of leptin signaling contributes to cardiac hypertrophy independently of body weight in mice. Circulation 108: 754– 759, 2003 [DOI] [PubMed] [Google Scholar]
- 5. Biddinger SB, Miyazaki M, Boucher J, Ntambi JM, Kahn CR. Leptin suppresses stearoyl-CoA desaturase 1 by mechanisms independent of insulin and sterol regulatory element-binding protein-1c. Diabetes 55: 2032– 2041, 2006 [DOI] [PubMed] [Google Scholar]
- 6. Bouloumie A, Drexler HCA, Lafontan M, Busse R. Leptin, the product of ob gene, promotes angiogenesis. Circ Res 83: 1059– 1066, 1998 [DOI] [PubMed] [Google Scholar]
- 7. Campen MJ, Shimoda LA, O'Donnell CP. Acute and chronic cardiovascular effects of intermittent hypoxia in C57BL/6J mice. J Appl Physiol 99: 2028– 2035, 2005 [DOI] [PubMed] [Google Scholar]
- 8. Carlson J, Rångemark C, Hedner J. Attenuated endothelium-dependent vascular relaxation in patients with sleep apnoea. J Hypertens 14: 577– 584, 1996 [DOI] [PubMed] [Google Scholar]
- 9. Chen L, Zhang J, Gan TX, Chen-Izu Y, Hasday JD, Karmazyn M, Balke CW, Scharf SM. Left ventricular dysfunction and associated cellular injury in rats exposed to chronic intermittent hypoxia. J Appl Physiol 104: 218– 223, 2008 [DOI] [PubMed] [Google Scholar]
- 10. Dematteis M, Julien C, Guillermet C, Sturm N, Lantuejoul S, Mallaret M, Levy P, Gozal E. Intermittent hypoxia induces early functional cardiovascular remodeling in mice. Am J Respir Crit Care Med 177: 227– 235, 2008 [DOI] [PubMed] [Google Scholar]
- 11. Donahoo WT, Stob NR, Ammon S, Levin N, Eckel RH. Leptin increases skeletal muscle lipoprotein lipase and postprandial lipid metabolism in mice. Metabolism. Epub ahead of print (PMID: 20494377; doi: 10.1016/j.metabol.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 12. Drummond M, Winck JC, Guimaraes JT, Santos AC, Almeida J, Marques JA. Autoadjusting-CPAP effect on serum leptin concentrations in obstructive sleep apnoea patients (Abstract). BMC Pulm Med 8: 21, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Duchna HW, Stoohs R, Guilleminault C, ChristineAnspach M, Schultze-Werninghaus G, Orth M. Vascular endothelial dysfunction in patients with mild obstructive sleep apnea syndrome. Wien Med Wochenschr 156: 596– 604, 2006 [DOI] [PubMed] [Google Scholar]
- 14. Fletcher EC, Lesske J, Qian W, Miller CC, 3rd, Unger T. Repetitive, episodic hypoxia causes diurnal elevation of blood pressure in rats. Hypertension 19: 555– 561, 1992 [DOI] [PubMed] [Google Scholar]
- 15. Greenberg H, Ye X, Wilson D, Htoo AK, Hendersen T, Liu SF. Chronic intermittent hypoxia activates nuclear factor-kappaB in cardiovascular tissues in vivo. Biochem Biophys Res Commun 343: 591– 596, 2006 [DOI] [PubMed] [Google Scholar]
- 16. Igel M, Lindenthal B, Giesa U, von BK. Evidence that leptin contributes to intestinal cholesterol absorption in obese (ob/ob) mice and wild-type mice. Lipids 37: 153– 157, 2002 [DOI] [PubMed] [Google Scholar]
- 17. Iiyori N, Alonso LC, Li J, Sanders MH, Garcia-Ocana A, O'Doherty RM, Polotsky VY, O'Donnell CP. Intermittent hypoxia causes insulin resistance in lean mice independent of autonomic activity. Am J Respir Crit Care Med 175: 851– 857, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ip MS, Lam KS, Ho C, Tsang KW, Lam W. Serum leptin and vascular risk factors in obstructive sleep apnea. Chest 118: 580– 560, 2000 [DOI] [PubMed] [Google Scholar]
- 19. Kakuma T, Lee Y, Higa M, Wang Z, Pan W, Shimomura I, Unger RH. Leptin, troglitazone, and the expression of sterol regulatory element binding proteins in liver and pancreatic islets. Proc Natl Acad Sci USA 97: 8536– 8541, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Korda M, Kubant R, Patton S, Malinski T. Leptin-induced endothelial dysfunction in obesity. Am J Physiol Heart Circ Physiol 295: H1514– H1521, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lavie P, Herer P, Hoffstein V. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ 320: 479– 482, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lee EJ, Woodske ME, Zou B, O'Donnell CP. Dynamic arterial blood gas analysis in conscious, unrestrained C57BL/6J mice during exposure to intermittent hypoxia. J Appl Physiol 107: 290– 294, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lembo G, Vecchione C, Fratta L, Marino G, Trimarco V, d'Amati G, Trimarco B. Leptin induces direct vasodilation through distinct endothelial mechanisms. Diabetes 49: 293– 297, 2000 [DOI] [PubMed] [Google Scholar]
- 24. Lesske J, Fletcher E, Bao G, Unger T. Hypertension caused by chronic intermittent hypoxia—influence of chemoreceptors and sympathetic nervous system. J Hypertens 15: 1593– 1603, 1997 [DOI] [PubMed] [Google Scholar]
- 25. Li J, Grigoryev DN, Ye SQ, Thorne L, Schwartz AR, Smith PL, O'Donnell CP, Polotsky VY. Chronic intermittent hypoxia upregulates genes of lipid biosynthesis in obese mice. J Appl Physiol 99: 1643– 1648, 2005 [DOI] [PubMed] [Google Scholar]
- 26. Li J, Thorne LN, Punjabi NM, Sun CK, Schwartz AR, Smith PL, Marino RL, Rodriguez A, Hubbard WC, O'Donnell CP, Polotsky VY. Intermittent hypoxia induces hyperlipidemia in lean mice. Circ Res 97: 698– 706, 2005 [DOI] [PubMed] [Google Scholar]
- 27. Licinio J, Caglayan S, Ozata M, Yildiz BO, deMiranda PB, O'Kirwan F, Whitby R, Liang L, Cohen P, Bhasin S, Krauss RM, Veldhuis JD, Wagner AJ, DePaoli AM, McCann SM, Wong ML. Phenotypic effects of leptin replacement on morbid obesity, diabetes mellitus, hypogonadism, and behavior in leptin-deficient adults. Proc Natl Acad Sci USA 101: 4531– 4536, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Minhas KM, Khan SA, Raju SV, Phan AC, Gonzalez DR, Skaf MW, Lee K, Tejani AD, Saliaris AP, Barouch LA, O'Donnell CP, Emala CW, Berkowitz DE, Hare JM. Leptin repletion restores depressed β-adrenergic contractility in ob/ob mice independently of cardiac hypertrophy. J Physiol 565: 463– 474, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Morgan DA, Thedens DR, Weiss R, Rahmouni K. Mechanisms mediating renal sympathetic activation to leptin in obesity. Am J Physiol Regul Integr Comp Physiol 295: R1730– R1736, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nickola MW, Wold LE, Colligan PB, Wang GJ, Samson WK, Ren J. Leptin attenuates cardiac contraction in rat ventricular myocytes. Role of NO. Hypertension 36: 501– 505, 2000 [DOI] [PubMed] [Google Scholar]
- 31. Ogawa Y, Masuzaki H, Hosoda K, Aizawa-Abe M, Suga J, Suda M, Ebihara K, Iwai H, Matsuoka N, Satoh N, Odaka H, Kasuga H, Fujisawa Y, Inoue G, Nishimura H, Yoshimasa Y, Nakao K. Increased glucose metabolism and insulin sensitivity in transgenic skinny mice overexpressing leptin. Diabetes 48: 1822– 1829, 1999 [DOI] [PubMed] [Google Scholar]
- 32. Oral EA, Simha V, Ruiz E, Andewelt A, Premkumar A, Snell P, Wagner AJ, DePaoli AM, Reitman ML, Taylor SI, Gorden P, Garg A. Leptin-replacement therapy for lipodystrophy. N Engl J Med 346: 570– 578, 2002 [DOI] [PubMed] [Google Scholar]
- 33. Paton CM, Ntambi JM. Biochemical and physiological function of stearoyl-CoA desaturase. Am J Physiol Endocrinol Metab 297: E28– E37, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Polotsky VY, Li J, Punjabi NM, Rubin AE, Smith PL, Schwartz AR, O'Donnell CP. Intermittent hypoxia increases insulin resistance in genetically obese mice. J Physiol 552: 253– 264, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Polotsky VY, Rubin AE, Balbir A, Dean T, Smith PL, Schwartz AR, O'Donnell CP. Intermittent hypoxia causes REM sleep deficits and decreases EEG delta power in NREM sleep in the C57BL/6J mouse. Sleep Med 7: 7– 16, 2006 [DOI] [PubMed] [Google Scholar]
- 36. Procopio C, Andreozzi F, Laratta E, Cassese A, Beguinot F, Arturi F, Hribal ML, Perticone F, Sesti G. Leptin-stimulated endothelial nitric-oxide synthase via an AMPK/Akt signalling pathway is attenuated by interaction with C reactive protein. Endocrinology 150: 3584– 3593, 2009 [DOI] [PubMed] [Google Scholar]
- 37. Ren J, Zhu BH, Relling DP, Esberg LB, Ceylan-Isik AF. High-fat diet-induced obesity leads to resistance to leptin-induced cardiomyocyte contractile response. Obesity (Silver Spring) 16: 2417– 2423, 2008 [DOI] [PubMed] [Google Scholar]
- 38. Rodriguez A, Fortuno A, Gomez-Ambrosi J, Zalba G, Diez J, Fruhbeck G. The inhibitory effect of leptin on angiotensin II-induced vasoconstriction in vascular smooth muscle cells is mediated via a nitric oxide-dependent mechanism. Endocrinology 148: 324– 331, 2007 [DOI] [PubMed] [Google Scholar]
- 39. Sajkov D, McEvoy RD. Obstructive sleep apnea and pulmonary hypertension. Prog Cardiovasc Dis 51: 363– 370, 2009 [DOI] [PubMed] [Google Scholar]
- 40. Savransky V, Jun J, Li J, Nanayakkara A, Fonti S, Moser AB, Steele KE, Schweitzer MA, Patil SP, Bhanot S, Schwartz AR, Polotsky VY. Dyslipidemia and atherosclerosis induced by chronic intermittent hypoxia are attenuated by deficiency of stearoyl coenzyme A desaturase. Circ Res 103: 1173– 1180, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Savransky V, Bevans S, Nanayakkara A, Li J, Smith PL, Torbenson MS, Polotsky VY. Chronic intermittent hypoxia causes hepatitis in a mouse model of diet-induced fatty liver. Am J Physiol Gastrointest Liver Physiol 293: G871– G877, 2007 [DOI] [PubMed] [Google Scholar]
- 42. Shek EW, Brands MW, Hall JE. Chronic leptin infusion increases arterial pressure. Hypertension 31: 409– 414, 1998 [DOI] [PubMed] [Google Scholar]
- 43. Sikka G, Yang R, Reid S, Benjo A, Koitabashi N, Camara A, Baraban E, O'Donnell CP, Berkowitz DE, Barouch LA. Leptin is essential in maintaining normal vascular compliance independent of body weight. Int J Obes 34: 203– 206, 2010 [DOI] [PubMed] [Google Scholar]
- 44. Tamisier R, Gilmartin GS, Launois SH, Pepin JL, Nespoulet H, Thomas RJ, Levy P, Weiss JW. A new model of chronic intermittent hypoxia in humans: Effect on ventilation, sleep and blood pressure. J Appl Physiol 107: 17– 24, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tokuda F, Sando Y, Matsui H, Koike H, Yokoyama T. Serum levels of adipocytokines, adiponectin and leptin, in patients with obstructive sleep apnea syndrome. Intern Med 47: 1843– 1849, 2008 [DOI] [PubMed] [Google Scholar]
- 46. Unger RH. Hyperleptinemia: protecting the heart from lipid overload. Hypertension 45: 1031– 1034, 2005 [DOI] [PubMed] [Google Scholar]
- 47. Vecchione C, Maffei A, Colella S, Aretini A, Poulet R, Frati G, Gentile MT, Fratta L, Trimarco V, Trimarco B, Lembo G. Leptin effect on endothelial nitric oxide is mediated through Akt-endothelial nitric oxide synthase phosphorylation pathway. Diabetes 51: 168– 173, 2002 [DOI] [PubMed] [Google Scholar]
- 48. Vanpatten S, Karkanias GB, Rossetti L, Cohen DE. Intracerebroventricular leptin regulates hepatic cholesterol metabolism. Biochem J 379: 229– 233, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wang YX. Do measures of vascular compliance correlate with endothelial function? Curr Diab Rep 7: 265– 268, 2007 [DOI] [PubMed] [Google Scholar]
- 50. Winters B, Mo Z, Brooks-Asplund E, Kim S, Shoukas A, Li D, Nyhan D, Berkowitz DE. Reduction of obesity, as induced by leptin, reverses endothelial dysfunction in obese (Lepob) mice. J Appl Physiol 89: 2382– 2390, 2000 [DOI] [PubMed] [Google Scholar]
- 51. Wolska BM, Solaro RJ. Method for isolation of adult mouse cardiac myocytes for studies of contraction and microfluorimetry. Am J Physiol Heart Circ Physiol 271: H1250– H1255, 1996 [DOI] [PubMed] [Google Scholar]
- 52. Yu X, Park BH, Wang MY, Wang ZV, Unger RH. Making insulin-deficient type 1 diabetic rodents thrive without insulin. Proc Natl Acad Sci USA 105: 14070– 14075, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]