Abstract
Functional and structural heterogeneity exists among skeletal muscle vascular beds related, in part, to muscle fiber type composition. This study was designed to delineate whether the vulnerability to vascular dysfunction in insulin resistance is uniformly distributed among skeletal muscle vasculatures and whether physical activity modifies this vulnerability. Obese, hyperphagic Otsuka Long-Evans Tokushima fatty rats (20 wk old) were sedentary (OSED) or physically active (OPA; access to running wheels) and compared with age-matched sedentary Long-Evans Tokushima Otsuka (LSED) rats. Vascular responses were determined in isolated, pressurized feed arteries from fast-twitch gastrocnemius (GFAs) and slow-twitch soleus (SFAs) muscles. OSED animals were obese, insulin resistant, and hypertriglyceridemic, traits absent in LSED and OPA rats. GFAs from OSED animals exhibited depressed dilation to ACh, but not sodium nitroprusside, and enhanced vasoconstriction to endothelin-1 (ET-1), but not phenylephrine, compared with those in LSED. Immunoblot analysis suggests reduced endothelial nitric oxide synthase phosphorylation at Ser1177 and endothelin subtype A receptor expression in OSED GFAs. Physical activity prevented reduced nitric oxide-dependent dilation to ACh, but not enhanced ET-1 vasoconstriction, in GFA from OPA animals. Conversely, vasoreactivity of SFAs to ACh and ET-1 were principally similar in all groups, whereas dilation to sodium nitroprusside was enhanced in OSED and OPA rats. These data demonstrate, for the first time, that SFAs from insulin-resistant rats exhibit reduced vulnerability to dysfunction versus GFAs and that physical activity largely prevents GFA dysfunction. We conclude that these results demonstrate that vascular dysfunction associated with insulin resistance is heterogeneously distributed across skeletal muscle vasculatures related, in part, to muscle fiber type and activity level.
Keywords: Otsuka Long-Evans Tokushima fatty rat, diabetes mellitus, metabolic syndrome, exercise, endothelial dysfunction
vascular dysfunction associated with insulin resistance is characterized by impaired endothelium-dependent dilation, enhanced sensitivity to vasoconstrictors, and microvascular rarefaction (15, 22, 38). These detrimental changes contribute to attenuated resting skeletal muscle blood flow and functional hyperemia in this state, thereby compromising the effective matching of perfusion with metabolic demand (4, 6, 14, 28, 45). Previous work from our laboratory demonstrates that local hemodynamic environments and vascular reactivity vary dramatically in the skeletal muscle microcirculation perfusing muscles of different fiber types (i.e., oxidative vs. glycolytic) (1, 3, 32, 42). Given the established role of local hemodynamics in determining/modulating endothelial phenotype (12, 19, 31), we investigated whether these variations infer differential vulnerability of skeletal muscle vascular beds to the development of dysfunction in insulin resistance.
Blood flow to the primarily slow-twitch oxidative soleus muscle is two- to fourfold greater than that to the primarily fast-twitch glycolytic gastrocnemius muscle in standing rats (3). Much of this difference is due to recruitment of the soleus during standing/walking versus the gastrocnemius that is recruited during heavier activity (i.e., running) (3). Indeed, during treadmill exercise, blood flows to the soleus and gastrocnemius muscles are relatively similar (3). The high resting blood flow/shear stress in the soleus feed artery (SFA) is critical for the maintenance of endothelium-dependent dilation and endothelial nitric oxide (NO) synthase (eNOS) expression in this vessel (3, 43, 44). Furthermore, exercise training does not enhance endothelium-dependent dilation or eNOS expression in the SFA but increases eNOS expression in the gastrocnemius feed artery (GFA) (24, 32). Thus it appears that local hemodynamics produce an exercise-training-like phenotype of the SFA.
Physical activity and exercise training appear to be effective in treating/preventing the functional and structural alterations in skeletal muscle vessels of diabetic rats and the forearm circulation of diabetic patients (15, 36, 46). Exercise-induced increases in shear stress and reduction of comorbidities are believed to contribute to the maintenance/restoration of vascular function (22, 26). As discussed above, evidence suggests that exercise-induced benefits are most pronounced in vessels experiencing the greatest relative increase in blood flow during exercise such as the GFA. Therefore, given the exercise-training-like phenotype of the SFA, we examined the hypotheses that the vascular dysfunction associated with insulin resistance 1) is attenuated in SFAs compared with GFAs and 2) is prevented in both vessels in response to daily wheel-running activity. These hypotheses were examined in isolated GFAs and SFAs from insulin-resistant Otsuka Long-Evans Tokushima fatty (OLETF) rats and control Long-Evans Tokushima Otsuka (LETO) rats. Vascular responses to NO-dependent and -independent dilators as well as to vasoconstrictors known to be upregulated by insulin resistance, particularly endothelin-1 (ET-1), were examined as indicators of vascular health/dysfunction.
METHODS
Animals
All animal protocols were approved by the Institutional Animal Care and Use Committee at the University of Missouri. Male OLETF and LETO rats (4 wk of age) were kindly supplied by the Tokushima Research Institute, Otsuka Pharmaceutical (Tokushima, Japan). OLETF rats were randomly designated as sedentary (OSED) or physically active (OPA). All non-insulin resistant LETO animals were sedentary (LSED). OPA animals were housed (at 4 wk) in cages equipped with voluntary running wheels outfitted with a bicycle computer to measure daily running activity. Voluntary running was selected to approximate the natural activity state of the animal, similar to a previous study (34). Animals were housed in a temperature-controlled room (12-h:12-h light-dark cycle) and provided water and standard rodent chow (Formulab 5008, Purina Mills, St Louis, MO) ad libitum.
At 20 wk of age, rats were anesthetized (pentobarbital sodium, 100 mg/kg) and euthanized by exsanguination 5 h after locking of the running wheels (OPA) and removal of food from cages (all groups). Body weight and percent body fat were determined and blood samples obtained for the determination of plasma glucose, insulin, triglycerides, and NOx (NO2 and NO3), as recently described (11). Aortas from the animals used in the present study were used for a recently published study (11).
Isolation of Feed Arteries
GFAs and SFAs were isolated as previously described (42) and placed in ice-cold MOPS-buffered physiological saline solution (PSS) containing (in mM) 145.0 NaCl, 5.2 KCl, 2.0 CaCl2, 1.17 MgSO4, 1.2 NaH2PO4, 5.0 glucose, 2.0 pyruvate, 0.02 EDTA, and 25.0 MOPS at pH 7.4. Vasomotor responses were determined in one GFA and SFA per animal. Feed arteries from the contralateral leg were isolated and frozen (−80°C) for immunoblot analysis.
Determination of Vasomotor Responses
Preparation of arteries.
Following isolation, feed arteries were cannulated with resistance-matched (<1% difference in electrical resistance) glass micropipettes, secured at each end with 9-0 ophthalmic suture and attached to separate reservoirs containing PSS plus albumin (1 g/100 ml) that were adjusted to achieve an approximate in vivo intraluminal pressure of 90 cmH2O (41). Arteries were equilibrated for ∼1 h at 37°C and visualized on an inverted microscope, and luminal diameters were measured with a videomicrometer. Arteries with leaks were discarded. Following equilibration, arteries were preconstricted with phenylephrine (PE) to achieve 30–60% tone for examination of vasomotor responses.
Vasomotor responses.
Endothelium-dependent dilation of feed arteries was determined in response to acetylcholine (ACh; 1 nM–10 mM). Responses to the endothelium-independent dilator and NO-donor sodium nitroprusside (SNP; 1 nM–10 mM) and the vasoconstrictor ET-1 (0.1–10 nM) were also determined. In a separate set of experiments, arteries were pretreated with the NO synthase (NOS) inhibitor NG-nitro-l-arginine methyl ester (l-NAME; 300 μM) for 30 min before ACh concentration response curves but after initial preconstriction with PE. At the end of each experiment, the PSS bath solution was replaced with Ca2+-free PSS to determine maximal passive diameter.
Drugs and Solutions
All drugs and solutions were obtained from Sigma (St. Louis, MO). PSS solutions and drugs were prepared before the study, frozen, and thawed each day. SNP was prepared on the day of the experiment.
Immunoblot Analysis
To obtain sufficient protein for immunoblot analysis, GFAs from three different animals were pooled for each sample and prepared similar to a previous study (8). Briefly, pooled feed artery samples were digested and the total protein content of each sample determined using a NanoOrange protein quantitation kit (Invitrogen). Ten micrograms protein/lane were separated by 12% SDS-PAGE, transferred to polyvinylidene diflouride membranes, and blocked in 5% nonfat milk-Tris-buffered saline-Tween-20 solution for 1 h. Rat brain tissue extract (Assay Designs) and rat lung were used as positive controls. Primary antibodies (in 5% nonfat milk-Tris-buffered saline-Tween-20 solution) targeting eNOS (140 kDa; 1:1,000; BD Transduction), Ser1177 phosphorylated eNOS (p-eNOS; 140 kDa; 1:250; BD Transduction), and endothelin subtype A (ETA; 29 kDa; 1:500; Sigma) and subtype B (ETB; 40 kDa; 1:500; Sigma) receptors were incubated overnight at room temperature (eNOS, p-eNOS) or 4°C (ETA, ETB), followed by incubation with secondary antibody conjugated to horseradish peroxidase. After the membranes were probed for p-eNOS, the membranes were stripped with stripping buffer (50°C, 30 min) and reprobed with the eNOS antibody. The ratio of p-eNOS to eNOS was subsequently determined. Protein was detected by enhanced chemiluminescence (SuperSignal Extended Duration Substrate, Thermo Scientific) and analyzed by densitometry on a Kodak Image Station 4000R. Equal loading of protein across lanes was confirmed by Coomassie staining.
Data Analysis and Statistics
Data are presented as means ± SE. Dilator responses are presented as percent maximal dilation, calculated as [(Dd − Db)/(Dmax − Db)]·100, where Dd is diameter after a drug intervention, Db is baseline diameter, and Dmax is maximal passive diameter. The NOS-dependent component of ACh dilation was calculated as the difference between dose-dependent responses to ACh in the absence and presence of l-NAME. Constrictor responses presented as percent possible constriction calculated as [(Db − Dd)/Db]·100. Statistical analysis was performed with one- or two-way ANOVA with a Tukey post hoc analysis in SigmaStat, as appropriate. A P value < 0.05 was considered significant.
RESULTS
Animal Characteristics
Phenotypic data for the 20-wk-old animals used in this study were previously published in a study that used aortas from these animals (11). When compared with LSED animals, OSED animals are obese (body weight, 478 ± 7 vs. 607 ± 11 g; and percent body fat, 16 ± 1 vs. 30 ± 1%; P < 0.05) and insulin resistant (fasting plasma glucose, 331 ± 38 vs. 542 ± 58 mg/dl; and fasting plasma insulin, 9 ± 1 vs. 13 ± 1 ng/ml; P < 0.05) and have elevated plasma triglycerides (43 ± 4 vs. 177 ± 25 mg/dl, P < 0.05) and reduced plasma NOx levels (12 ± 1 vs. 7 ± 1 nM/ml media, P < 0.05) (11). Plasma variables were measured after a 5-h fast and in many cases do not represent fully fasted values. Together with issues such as stressful transport of animals between buildings before death, this likely contributes to the elevation of plasma glucose in LSED animals compared with those in previous reports (18, 20). LSED animals are not chronically hyperglycemic at 20 wk of age, however, as demonstrated by normal HbA1c levels (4.6% vs. 5.4% in OSED, P < 0.05) (39).
Average daily wheel-running distance for OPA animals peaked at 9 wk of age at 10.7 ± 0.3 km/day and declined to 5.3 ± 0.2 km/day at 20 wk of age. OPA animals exhibited elevated red gastrocnemius citrate synthase activity (335 ± 32 nmol·min−1·μg−1, P < 0.05) compared with LSED and OSED (271 ± 31 and 253 ± 21 nmol·min−1·μg−1) animals, respectively (11). Daily physical activity maintained body weight (435 ± 11 g), percent body fat (11 ± 2%), fasting plasma glucose (380 ± 53 mg/dl), insulin (10 ± 1 ng/ml), and triglycerides (71 ± 11 mg/dl) at levels similar to those of LSED rats. Plasma NOx levels, however, were not maintained by physical activity and were similar to OSED values (6 ± 1 nM/ml media) (11).
Feed Artery Characteristics
Maximal diameters (Table 1) and the concentration of PE necessary for preconstriction (0.55 μM for GFAs, and 0.25 μM for SFAs) were similar for each vessel. OPA GFAs exhibited greater PE-induced tone than OSED GFAs (Table 1). PE-induced tone was similar for SFAs from the groups.
Table 1.
Feed artery diameters
| n | Passive Diameter, μm | Preconstriction, % | |
|---|---|---|---|
| GFA | |||
| LSED | 18 | 316 ± 15 | 41 ± 2 |
| OSED | 17 | 321 ± 13 | 40 ± 3 |
| OPA | 19 | 339 ± 13 | 51 ± 3* |
| SFA | |||
| LSED | 17 | 191 ± 5 | 45 ± 5 |
| OSED | 22 | 199 ± 7 | 51 ± 3 |
| OPA | 22 | 187 ± 5 | 48 ± 4 |
Values are means ± SE; n, sample size.
GFA, gastrocnemius feed artery; SFA, soleus feed artery; LSED, Long-Evans Tokushima Otsuka rat; OSED and OPA, Otsuka Long-Evans Tokushima fatty rats that are sedentary and physically active, respectively.
P < 0.05 vs. OSED.
Feed Artery Vasomotor Responses
Endothelium-dependent vasodilation.
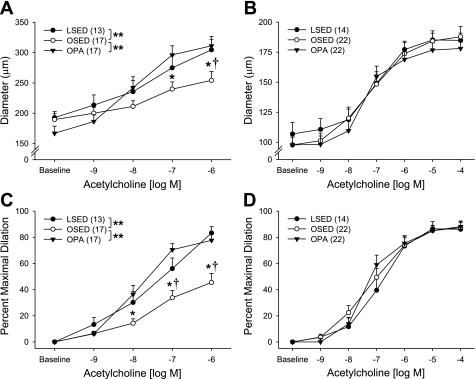
In GFAs, vasomotor responses to ACh doses above 1 μM were excluded because they induced vasoconstriction. Maximal ACh-induced dilation (1 μM ACh) was attenuated in OSED compared with LSED rats in GFAs (45 ± 7 vs. 83 ± 5%, P < 0.05; Fig. 1). Maximal dilation to ACh was maintained in GFAs from OPA rats (78 ± 5%, Fig. 1) similar to LSED rats. Conversely, maximal dilation to ACh (10 mM) in SFAs was similar between all groups (Fig. 1).
Fig. 1.
Concentration-response curves to acetylcholine (ACh) in gastrocnemius feed arteries (GFAs; A and C) and soleus feed arteries (SFAs; B and D). Data are presented as absolute diameter (A and B) and percent possible dilation (C and D). Values are means ± SE; sample size in parentheses. Otsuka Long-Evans Tokushima fatty rats that are sedentary (OSED) and physically active (OPA) are shown. *P < 0.05 vs. OPA; **P < 0.05 for comparison indicated; †P < 0.05 vs. Long-Evans Tokushima Otsuka (LSED) rats.
Previous work has demonstrated that endothelium-dependent dilation is acutely enhanced by a single bout of exercise (21). To examine the possibility that enhanced ACh-induced dilation of OPA GFA acutely resulted from the last exercise bout, a subset of OPA rats (n = 5) were made inactive for 53 h before death. In the GFAs from these animals, ACh-mediated dilation was comparable with that after 5 h of inactivity (data not shown); therefore, the maintenance of endothelial function by physical activity likely represents a chronic adaptation rather than an acute exercise effect.
Endothelium-independent vasodilation.
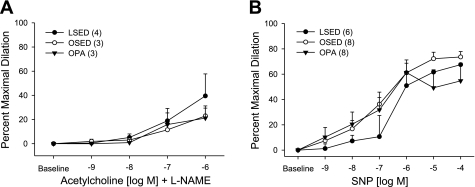
Dilation to SNP was similar among treatment groups in GFAs (Fig. 3B). In SFAs, dilation to SNP was greater in OSED and OPA rats compared with LSED rats (P < 0.05; Fig. 4C).
Fig. 3.
Concentration-response curves to ACh of GFAs in the presence of the nitric oxide synthase (NOS) inhibitor NG-nitro-l-arginine methyl ester (l-NAME; 300 μM; A) and to the NO donor sodium nitroprusside (SNP; B). Values are means ± SE; sample size in parentheses.
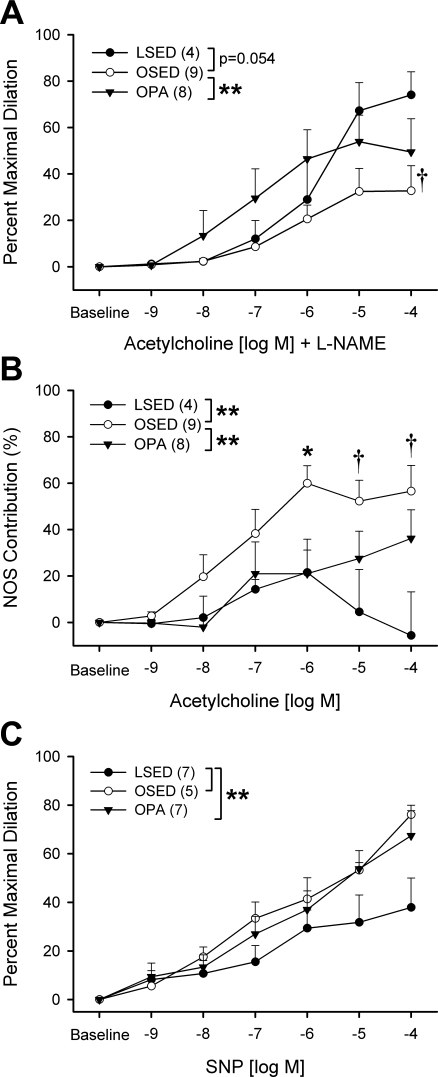
Fig. 4.
A: concentration-response curves to ACh of SFAs in the presence of the NOS inhibitor l-NAME (300 μM). B: NOS-dependent component of ACh dilation (difference with and without l-NAME). C: concentration-response curves to the NO donor SNP. Values are means ± SE; sample size in parentheses. *P < 0.05 vs. OPA; **P < 0.05 for comparison indicated; †P < 0.05 vs. LSED.
Vasoconstrictor responses.
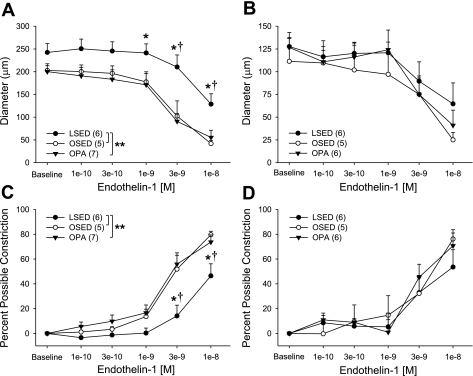
Constrictor responses to ET-1 were enhanced in both OLETF groups (OSED and OPA) compared with the LSED group in GFAs (Fig. 2). Maximal ET-1 constriction (10 nM) was 80 ± 3% in OSED, 74 ± 6% in OPA, and 46 ± 10% in LSED rats. This does not appear to represent a generalized enhancement of GFA vasoconstrictor responses since vasoconstriction to the α1-adrenergic agonist PE was not different in GFAs from all groups (data not shown). In SFAs, ET-1-induced vasoconstriction was similar among groups (Fig. 2).
Fig. 2.
Concentration-response curves to endothelin-1 in GFAs (A and C) and SFAs (B and D). Data are presented as absolute diameter (A and B) and percent possible dilation (C and D). Values are means ± SE; sample size in parentheses. *P < 0.05 vs. OPA; **P < 0.05 for comparison indicated; †P < 0.05 vs. OSED.
Role of NO in vasomotor responses.
In GFAs, NOS blockade with l-NAME similarly increased baseline tone among groups (14 ± 5% in LSED, 16 ± 12% in OSED, and 24 ± 8% in OPA). NOS blockade significantly reduced ACh-mediated dilation in GFAs and abolished group differences in dilation to ACh (Fig. 3A). In SFAs, NOS blockade increased baseline tone by 21 ± 7% in LSED, 16 ± 3% in OSED, and 4 ± 4% in OPA rats (P < 0.05, LSED vs. OPA) and had differential effects on ACh-induced dilation in SFAs (Fig. 4A). NOS blockade revealed an enhanced NO-dependent component of ACh-mediated dilation of SFAs in OSED versus LSED and OPA rats (Fig. 4B). These data reveal that the mechanisms mediating SFA dilation to ACh differ across groups.
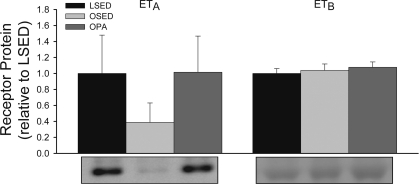
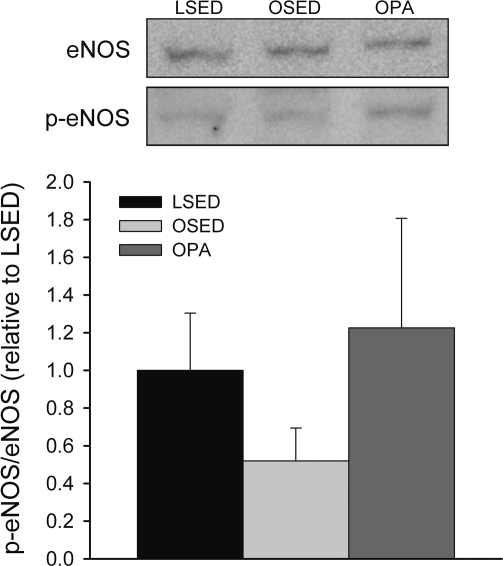
Immunoblot Analysis
The noted changes in GFA reactivity in response to insulin resistance and physical activity were further examined via immunoblot analysis of proteins relevant to NO and ET-1-mediated vascular responses. Immunoblot results for p-eNOS (140 kDa), eNOS (140 kDa), ETA (29 kDa), and ETB (40 kDa) receptors revealed isolated bands for each protein at the anticipated molecular weight, according to the manufacturer's specifications. Because of the necessity to pool vessels, four lanes of GFAs (3 vessels/lane) from each group were examined, representing 12 animals/group. Statistical power is reduced due to pooling feed arteries such that n = 12 vessels is reduced to n = 4 lanes for analysis. Figure 5 presents GFA gels probed for ETA and ETB receptors. In GFAs (Fig. 5), ETA and ETB receptor protein expression was not statistically different among groups. Furthermore, as shown in Fig. 6, the p-eNOS-to-eNOS ratio was lower in OSED GFAs compared with those of LSED and OPA rats but was also not statistically significant. There were no differences in total eNOS protein content of the GFAs among groups; thus this trend appears to be driven by potential differences in eNOS phosphorylation at Ser1177.
Fig. 5.
Immunoblot analysis of endothelin subtypes A (ETA) and B (ETB) receptor protein expression in GFAs. Bands were detected at expected molecular masses for ETA (29 kDa) and ETB (40 kDa) receptors. Values are means ± SE, expressed relative to LSED mean value.
Fig. 6.
Immunoblot analysis of phosphorylated endothelial NOS (p-eNOS; Ser1177)-to-eNOS ratios in GFAs. Ratios were calculated using optical densities for p-eNOS and eNOS. Values are means ± SE, expressed relative to LSED values, and represent 3 lanes (9 vessels) for LSED, 4 lanes (12 vessels) for OSED, and 4 lanes (12 vessels) for OPA.
DISCUSSION
This study examined whether differences in muscle fiber type composition (and related differences in recruitment patterns and local hemodynamics) are associated with the vulnerability of skeletal muscle vascular beds to vascular dysfunction in insulin resistance. The principal findings are that the insulin-resistant OLETF rat exhibits 1) attenuated endothelium-dependent dilation of GFAs but not SFAs and 2) enhanced ET-1-mediated vasoconstriction in GFAs but not SFAs and that 3) daily physical activity prevents endothelial dysfunction, but not enhanced ET-1 vasoconstriction, in GFAs. These results support our hypothesis that arteries perfusing muscles of different fiber types are differentially susceptible to the vascular dysfunction associated with insulin resistance. Furthermore, they demonstrate that physical activity prevents some, but not all, functional consequences of insulin resistance-associated vascular dysfunction.
Effect of Fiber Type
Previous work has demonstrated differential vascular reactivity of vessels perfusing primarily slow-twitch oxidative (i.e., soleus) and fast-twitch glycolytic (i.e., gastrocnemius) muscles (1, 13, 32, 37, 42). Our results extend these findings by revealing that the SFA demonstrates a reduced vulnerability to the vascular dysfunction associated with insulin resistance compared with the GFA. Specifically, the attenuated ACh-mediated dilation and enhanced ET-1-mediated constriction observed in the GFA are absent in the SFA of insulin-resistant OSED animals. Recently, our laboratory demonstrated no decrement in ACh-mediated dilation of the abdominal aorta from the same animals used in the present study (11). These combined results highlight that caution must be exercised in generalizing results from the aorta as representative of other arteries (11).
Reduced NO bioavailability is a hallmark of endothelial dysfunction in insulin resistance (38). Our results are consistent with this being the primary cause of reduced endothelium-dependent dilation of the GFA of OSED animals. Plasma NOx levels were reduced in OSED compared with LSED animals, indicating a systemic reduction in NO release. In the isolated GFA, NOS inhibition abolished between-group differences in ACh-mediated dilation, whereas SNP sensitivities were unchanged in LSED and OSED animals. These data clearly demonstrate that a reduction in NO bioavailability rather than reduced GFA sensitivity to NO accounts for the attenuation of ACh dilation in this vessel. Our immunoblot results suggest that this may be due to attenuated NO production, owing to reduced eNOS phosphorylation at Ser1177. This observation is consistent with previous studies that report attenuated methacholine-stimulated NO release in aorta from the obese Zucker rat (16, 17). Other factors such as increased superoxide scavenging of NO or eNOS uncoupling, however, cannot be ruled out. Indeed, previous work has demonstrated a partial restoration of skeletal muscle arteriolar dilation to ACh following treatment with exogenous antioxidants (14, 16). Reduced levels of tetrahydrobiopterin, a necessary eNOS cofactor, in insulin resistance may also contribute via eNOS uncoupling and oxidant production (38).
Reduced NO bioavailability in OSED GFAs may also contribute to the enhanced vasoconstriction to ET-1 in these vessels, given the influence of NO on vascular reactivity to ET-1 (33). Furthermore, our results suggest that ETA receptor expression is reduced or not altered in OSED GFAs, clearly showing that increased ETA receptor numbers are not involved. Enhanced ETB receptor expression in GFA smooth muscle may also contribute to this; however, immunoblot data from intact GFAs as used in this study cannot differentiate changes in endothelial versus smooth muscle ETB expression. Thus these observations suggest that an increased sensitivity of GFA ETA receptors or possibly increased smooth muscle ETB expression may occur in insulin resistance. Similar ETA sensitization and enhanced ETB-mediated vascular tone have been previously reported in the canine and mouse coronary circulation, respectively (7, 29). This is consistent with the widespread findings of increased basal vascular tone and enhanced sensitivity to vasoconstrictors, especially ET-1, in models of insulin resistance (7, 14, 35). Our results demonstrate, however, that the enhanced ET-1 constriction is not indicative of a generalized increase in vasoconstrictor sensitivity since constriction to the α1-adrenergic agonist PE was not enhanced in OSED GFAs. Similar findings of differential vasoconstrictor sensitivity in insulin resistance have been reported, and a recent study suggests that this may result from temporal shifts in vasoconstrictor sensitivity during the onset and progression of diabetes (7, 35).
In contrast to the GFAs, endothelium-dependent dilation and ET-1-mediated constriction of the SFAs from OSED animals was comparable with that in SFAs from control LSED animals. Pretreatment of these vessels with l-NAME revealed that whereas the overall dilation to ACh is maintained, the mechanisms mediating this dilation are altered by insulin resistance. Specifically, we demonstrate that the NO-dependent component of ACh-mediated dilation is enhanced in SFAs from OSED animals, at least in part, due to enhanced smooth muscle sensitivity to NO. Together, our results suggest that the maintenance of ACh-mediated dilation in OSED SFAs is due to compensatory shifts in the pathways activated by ACh, thus making the SFAs less vulnerable to dysfunction induced by insulin resistance than the GFAs. The underlying cause of this shift is unclear but may result from enhanced soluble guanylate cyclase sensitivity induced by reduced NO bioavailability or enhanced oxidative stress (5, 10, 25). It remains unclear whether this shift represents early insulin resistance-induced dysfunction of the SFAs, which is compensated for by increased smooth muscle sensitivity to NO. Additionally, our data stimulate interest in whether the noted changes in both the GFA and SFA impact on the control of skeletal muscle blood flow during activity/exercise, and future studies are needed to more directly address this issue.
Our results reveal, for the first time, that the feed artery of slow-twitch oxidative muscle is less vulnerable to the development of dysfunction associated with insulin resistance than that of fast-twitch glycolytic muscle. The mechanisms mediating this differential vulnerability are not known, but based on previous data from our laboratory, we posit the concept that the SFA demonstrates an exercise-training-like vascular phenotype at rest and is likely less susceptible to dysfunction in disease (17, 26, 46). The soleus vasculature does not exhibit enhanced vasomotor function following exercise training in contrast to marked enhancements in the gastrocnemius vasculature (24, 32, 37). We believe that differences in local hemodynamics of the SFA and GFA are primary contributors to these differences. Specifically, blood flow to the soleus is two to fourfold greater than that to the gastrocnemius in a standing rat due mostly to the recruitment of the soleus as a postural muscle during standing/walking (3, 23). This high resting blood flow and shear stress in the SFA are critical for the maintenance of endothelium-dependent dilation and eNOS expression in this vessel (3, 43, 44). Furthermore, blood flow increases in the soleus are relatively mild during moderate- to high-intensity exercise compared with those measured in the gastrocnemius (3). Thus we argue that the SFA exhibits an exercise-training-like phenotype in response to normal cage activity, which infers a reduced vulnerability to the dysfunction associated with insulin resistance relative to that in the GFA.
Effect of Physical Activity
Increased daily physical activity is associated with the prevention/reversal of insulin resistance and associated cardiovascular events (26, 30). Thus exercise prescription is recommended for obese, insulin-resistant and diabetic patients (2). Mechanistically, physical activity may positively impact the vascular wall directly via episodic increases in shear stress and indirectly via reduction of comorbidities often associated with insulin resistance (i.e., hyperglycemia, hypercholesterolemia) (26). We have previously demonstrated that endurance and interval sprint training enhance vascular function of the gastrocnemius, but not soleus, vasculature of healthy animals (32, 37). Here we extend these findings by demonstrating that daily wheel running is sufficient to prevent the declines/changes in endothelial function associated with insulin resistance in GFAs and SFAs.
The OLETF rat is a unique model of obesity and insulin resistance in that it displays high levels of spontaneous activity on running wheels, a quality absent in other obese animal models (40). Indeed, with unlimited access to running wheels, OPA rats ran ∼8 km/day, encompassing ∼4 h/day of activity throughout the 16 wk of this study. This type of activity approximates the natural activity state of these animals and prevented the development of obesity and insulin resistance, confirming previous studies (11, 34). Our data further demonstrate that daily physical activity prevents declines in ACh-mediated dilation of the GFA via maintenance of NO bioavailability and possibly eNOS phosphorylation at Ser1177. Daily activity also prevented the increased NO-dependent component of ACh-mediated dilation of the SFA. Therefore, regarding endothelium-dependent dilation of skeletal muscle feed arteries, OPA animals exhibited responses similar to those in control LSED animals. Whether the maintenance of endothelial function results from the vascular benefits of activity, the prevention of other systemic risk factors or a combination of the two remains unclear. The differential distribution of vascular dysfunction associated with insulin resistance (i.e., present in the GFA but not the SFA) coupled with the maintenance of GFA function by physical activity supports the former. In other words, if the dysfunction seen in OSED animals were induced by systemic risk factors, we would expect to find similar dysfunction in the GFA and SFA. Thus our data argue that the distinctive local hemodynamic environments of the GFA and SFA are a primary contributor to the differential vulnerabilities of these vessels to dysfunction in insulin resistance. If shear stress in the GFA is increased by increased blood flow during physical activity, as we would expect, our results in OPA GFAs are consistent with studies demonstrating that elevations in shear rate are able to increase, or in our case maintain, eNOS levels, phosphorylation at Ser1177, and agonist-mediated NO production (31). Physical activity did not prevent the enhancement of ET-1-mediated constriction in the GFA seen in the OSED animals. This may indicate the presence of other elevated systemic risk factors that impact ET-1 vasoreactivity (i.e., cytokines, adipokines) in OPA animals. Surprisingly, wheel running did not prevent the reduction of plasma NOx levels, a marker of systemic basal NO release, thereby suggesting that this type of activity may not prevent endothelial dysfunction in all vasculatures. Future studies are needed to address the mechanistic basis of these differential findings, particularly as it relates to local hemodynamics in the skeletal muscle vasculature.
Perspectives
Our data suggest the hypothesis that the vascular dysfunction associated with insulin resistance is localized to the skeletal muscle vascular beds perfusing fast-twitch, but not slow-twitch, fibers. This likely contributes to the attenuated skeletal muscle blood flow and oxygen consumption kinetics noted in insulin resistance patients and animals (6, 14, 28, 46); however, the determination of fiber type effects in patients is hindered by the mixed fiber-type nature of human muscle. If this hypothesis is true and exercise can restore endothelial function in all resistance arteries, this should have a significant impact on exercise prescription for patients with insulin resistance that currently consists of 150 min/wk of moderate physical activity (i.e., aerobic training) (2). Recent data, however, suggest that high-intensity exercise that recruits fast-twitch fibers may have more beneficial effects on cardiorespiratory and metabolic fitness in patients with insulin resistance (9, 27). With regard to the present study, it remains unclear whether wheel running activity is more similar to endurance or interval sprint training. It may represent a hybrid activity, given that OLETF rats housed with a running wheel are active in frequent short (<1 min) bursts of activity similar to interval sprint training protocols, and we estimate that these animals run at an average speed of ∼35 m/min, similar to speeds used in endurance training protocols. Our finding of a 32% increase of citrate synthase activity in the red portion of the gastrocnemius muscle of OPA animals demonstrates some endurance training-like adaptations. Thus wheel running activity presents an activity regimen that is difficult to define with regard to classical rat treadmill training protocols. Regardless, since it is reasonable to expect that wheel running increases blood flow through the GFA, we speculate that the absence of physical activity and these increases of GFA flow in OSED animals is a primary mechanism accounting for the enhanced vulnerability of this vessel to the dysfunction associated with insulin resistance. Future work is necessary, however, to more clearly examine the intricacies of this issue.
Conclusions
Findings from this investigation reveal, for the first time, that feed arteries perfusing a muscle composed primarily of slow-twitch fibers (i.e., soleus) demonstrate a reduced vulnerability to the development of dysfunction in insulin-resistant rats than do feed arteries of predominantly fast-twitch muscle (i.e., gastrocnemius). This vascular dysfunction is characterized, in part, by reduced NO bioavailability and enhanced ET-1-mediated vasoconstriction. Furthermore, our data reveal that spontaneous wheel running activity is sufficient to prevent the development of endothelial dysfunction in GFAs. We assert that an underlying contributor to the nonuniform development of dysfunction in the GFA and SFA is differential local hemodynamic environments in these vessels that are made qualitatively more similar during physical activity.
GRANTS
This work was supported by the National Institutes of Health Grants HL-36088, HL-52490 (to M. H. Laughlin), DK-83182 (to R. S. Rector), and AR-048523 (to S. B. Bender); the University of Missouri Department of Internal Medicine (to J. A. Ibdan), the University of Missouri Research Board (to F. W. Booth), and a gift to the University of Missouri (to F. W. Booth).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
ACKNOWLEDGMENTS
OLETF and LETO rats were a generous gift of the Tokushima Research Institute, Otsuka Pharmaceuticals (Tokushima, Japan). We are grateful to Dr. Frank Booth for access to these animals and to Pam Thorne, Grace Uptergrove, Ann Melloh, Dr. Aaron Bunker, Kristi Larned, and Whitney Collins for assistance.
REFERENCES
- 1. Aaker A, Laughlin MH. Diaphragm arterioles are less responsive to α1-adrenergic constriction than gastrocnemius arterioles. J Appl Physiol 92: 1808– 1816, 2002 [DOI] [PubMed] [Google Scholar]
- 2. American Diabetes Association Standards of medical care in diabetes—2010. Diabetes Care 34, Suppl 1: S11– S61, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Armstrong RB, Laughlin MH. Blood flows within and among rat muscles as a function of time during high speed treadmill exercise. J Physiol 344: 189– 208, 1983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bauer TA, Reusch JE, Levi M, Regensteiner JG. Skeletal muscle deoxygenation after the onset of moderate exercise suggests slowed microvascular blood flow kinetics in type 2 diabetes. Diabetes Care 30: 2880– 2885, 2007 [DOI] [PubMed] [Google Scholar]
- 5. Bauersachs J, Bouloumie A, Fraccarollo D, Hu K, Busse R, Ertl G. Endothelial dysfunction in chronic myocardial infarction despite increased vascular endothelial nitric oxide synthase and soluble guanylate cyclase expression: role of enhanced vascular superoxide production. Circulation 100: 292– 298, 1999 [DOI] [PubMed] [Google Scholar]
- 6. Behnke BJ, Kindig CA, McDonough P, Poole DC, Sexton WL. Dynamics of microvascular oxygen pressure during rest-contraction transition in skeletal muscle of diabetic rats. Am J Physiol Heart Circ Physiol 283: H926– H932, 2002 [DOI] [PubMed] [Google Scholar]
- 7. Bender SB, Klabunde RE. Altered role of smooth muscle endothelin receptors in coronary endothelin-1 and α1-adrenoceptor-mediated vasoconstriction in Type 2 diabetes. Am J Physiol Heart Circ Physiol 293: H2281– H2288, 2007 [DOI] [PubMed] [Google Scholar]
- 8. Bender SB, Tune JD, Borbouse L, Long X, Sturek M, Laughlin MH. Altered mechanism of adenosine-induced coronary arteriolar dilation in early-stage metabolic syndrome. Exp Biol Med (Maywood) 234: 683– 692, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Boule NG, Kenny GP, Haddad E, Wells GA, Sigal RJ. Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in Type 2 diabetes mellitus. Diabetologia 46: 1071– 1081, 2003 [DOI] [PubMed] [Google Scholar]
- 10. Brandes RP, Kim D, Schmitz-Winnenthal FH, Amidi M, Godecke A, Mulsch A, Busse R. Increased nitrovasodilator sensitivity in endothelial nitric oxide synthase knockout mice: role of soluble guanylyl cyclase. Hypertension 35: 231– 236, 2000 [DOI] [PubMed] [Google Scholar]
- 11. Bunker AK, Arce-Esquivel AA, Rector RS, Booth FW, Ibdah JA, Laughlin MH. Physical activity maintains aortic endothelium-dependent relaxation in the obese type 2 diabetic OLETF rat. Am J Physiol Heart Circ Physiol 298: H1889– H1901, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dai G, Kaazempur-Mofrad MR, Natarajan S, Zhang Y, Vaughn S, Blackman BR, Kamm RD, Garcia-Cardena G, Gimbrone MA., Jr Distinct endothelial phenotypes evoked by arterial waveforms derived from atherosclerosis-susceptible and -resistant regions of human vasculature. Proc Natl Acad Sci USA 101: 14871– 14876, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Delp MD. Myogenic and vasoconstrictor responsiveness of skeletal muscle arterioles is diminished by hindlimb unloading. J Appl Physiol 86: 1178– 1184, 1999 [DOI] [PubMed] [Google Scholar]
- 14. Frisbee JC. Impaired skeletal muscle perfusion in obese Zucker rats. Am J Physiol Regul Integr Comp Physiol 285: R1124– R1134, 2003 [DOI] [PubMed] [Google Scholar]
- 15. Frisbee JC. Obesity, insulin resistance, and microvessel density. Microcirculation 14: 289– 298, 2007 [DOI] [PubMed] [Google Scholar]
- 16. Frisbee JC. Reduced nitric oxide bioavailability contributes to skeletal muscle microvessel rarefaction in the metabolic syndrome. Am J Physiol Regul Integr Comp Physiol 289: R307– R316, 2005 [DOI] [PubMed] [Google Scholar]
- 17. Frisbee JC, Samora JB, Peterson J, Bryner R. Exercise training blunts microvascular rarefaction in the metabolic syndrome. Am J Physiol Heart Circ Physiol 291: H2483– H2492, 2006 [DOI] [PubMed] [Google Scholar]
- 18. Fukaya N, Mochizuki K, Tanaka Y, Kumazawa T, Jiuxin Z, Fuchigami M, Goda T. The alpha-glucosidase inhibitor miglitol delays the development of diabetes and dysfunctional insulin secretion in pancreatic beta-cells in OLETF rats. Eur J Pharmacol 624: 51– 57, 2009 [DOI] [PubMed] [Google Scholar]
- 19. Garcia-Cardena G, Comander J, Anderson KR, Blackman BR, Gimbrone MA., Jr Biomechanical activation of vascular endothelium as a determinant of its functional phenotype. Proc Natl Acad Sci USA 98: 4478– 4485, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Guo Z, Bu S, Yu Y, Ghatnekar G, Wang M, Chen L, Bu M, Yang L, Zhu B, Feng Z, Huang Q. Diazoxide prevents abdominal adiposity and fatty liver in obese OLETF rats at prediabetic stage. J Diabetes Complications 22: 46– 55, 2008 [DOI] [PubMed] [Google Scholar]
- 21. Haram PM, Adams V, Kemi OJ, Brubakk AO, Hambrecht R, Ellingsen O, Wisloff U. Time-course of endothelial adaptation following acute and regular exercise. Eur J Cardiovasc Prev Rehabil 13: 585– 591, 2006 [DOI] [PubMed] [Google Scholar]
- 22. Hodnett BL, Hester RL. Regulation of muscle blood flow in obesity. Microcirculation 14: 273– 288, 2007 [DOI] [PubMed] [Google Scholar]
- 23. Jasperse JL, Laughlin MH. Flow-induced dilation of rat soleus feed arteries. Am J Physiol Heart Circ Physiol 273: H2423– H2427, 1997 [DOI] [PubMed] [Google Scholar]
- 24. Jasperse JL, Laughlin MH. Vasomotor responses of soleus feed arteries from sedentary and exercise-trained rats. J Appl Physiol 86: 441– 449, 1999 [DOI] [PubMed] [Google Scholar]
- 25. Jebelovszki E, Kiraly C, Erdei N, Feher A, Pasztor ET, Rutkai I, Forster T, Edes I, Koller A, Bagi Z. High-fat diet-induced obesity leads to increased NO sensitivity of rat coronary arterioles: role of soluble guanylate cyclase activation. Am J Physiol Heart Circ Physiol 294: H2558– H2564, 2008 [DOI] [PubMed] [Google Scholar]
- 26. Joyner MJ, Green DJ. Exercise protects the cardiovascular system: effects beyond traditional risk factors. J Physiol 587: 5551– 5558, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kang J, Robertson RJ, Hagberg JM, Kelley DE, Goss FL, DaSilva SG, Suminski RR, Utter AC. Effect of exercise intensity on glucose and insulin metabolism in obese individuals and obese NIDDM patients. Diabetes Care 19: 341– 349, 1996 [DOI] [PubMed] [Google Scholar]
- 28. Kingwell BA, Formosa M, Muhlmann M, Bradley SJ, McConell GK. Type 2 diabetic individuals have impaired leg blood flow responses to exercise: role of endothelium-dependent vasodilation. Diabetes Care 26: 899– 904, 2003 [DOI] [PubMed] [Google Scholar]
- 29. Knudson JD, Rogers PA, Dincer UD, Bratz IN, Araiza AG, Dick GM, Tune JD. Coronary vasomotor reactivity to endothelin-1 in the prediabetic metabolic syndrome. Microcirculation 13: 209– 218, 2006 [DOI] [PubMed] [Google Scholar]
- 30. Lakka TA, Laaksonen DE. Physical activity in prevention and treatment of the metabolic syndrome. Appl Physiol Nutr Metab 32: 76– 88, 2007 [DOI] [PubMed] [Google Scholar]
- 31. Laughlin MH, Newcomer SC, Bender SB. Importance of hemodynamic forces as signals for exercise-induced changes in endothelial cell phenotype. J Appl Physiol 104: 588– 600, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Laughlin MH, Woodman CR, Schrage WG, Gute D, Price EM. Interval sprint training enhances endothelial function and eNOS content in some arteries that perfuse white gastrocnemius muscle. J Appl Physiol 96: 233– 244, 2004 [DOI] [PubMed] [Google Scholar]
- 33. Lavallée M, Takamura M, Parent R, Thorin E. Crosstalk between endothelin and nitric oxide in the control of vascular tone. Heart Fail Rev 6: 265– 276, 2001 [DOI] [PubMed] [Google Scholar]
- 34. Laye MJ, Rector RS, Warner SO, Naples SP, Perretta AL, Uptergrove GM, Laughlin MH, Thyfault JP, Booth FW, Ibdah JA. Changes in visceral adipose tissue mitochondrial content with type 2 diabetes and daily voluntary wheel running in OLETF rats. J Physiol 587: 3729– 3739, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lesniewski LA, Donato AJ, Behnke BJ, Woodman CR, Laughlin MH, Ray CA, Delp MD. Decreased NO signaling leads to enhanced vasoconstrictor responsiveness in skeletal muscle arterioles of the ZDF rat prior to overt diabetes and hypertension. Am J Physiol Heart Circ Physiol 294: H1840– H1850, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Maiorana A, O'Driscoll G, Cheetham C, Dembo L, Stanton K, Goodman C, Taylor R, Green D. The effect of combined aerobic and resistance exercise training on vascular function in type 2 diabetes. J Am Coll Cardiol 38: 860– 866, 2001 [DOI] [PubMed] [Google Scholar]
- 37. McAllister RM, Jasperse JL, Laughlin MH. Nonuniform effects of endurance exercise training on vasodilation in rat skeletal muscle. J Appl Physiol 98: 753– 761, 2005 [DOI] [PubMed] [Google Scholar]
- 38. Rask-Madsen C, King GL. Mechanisms of disease: endothelial dysfunction in insulin resistance and diabetes. Nat Clin Pract Endocrinol Metab 3: 46– 56, 2007 [DOI] [PubMed] [Google Scholar]
- 39. Rector RS, Thyfault JP, Uptergrove GM, Morris EM, Naples SP, Borengasser SJ, Mikus CR, Laye MJ, Laughlin MH, Booth FW, Ibdah JA. Mitochondrial dysfunction precedes insulin resistance and hepatic steatosis and contributes to the natural history of non-alcoholic fatty liver disease in an obese rodent model. J Hepatol 52: 727– 736, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Stern JS, Johnson PR. Spontaneous activity and adipose cellularity in the genetically obese Zucker rat (fafa). Metabolism 26: 371– 380, 1977 [DOI] [PubMed] [Google Scholar]
- 41. Williams DA, Segal SS. Feed artery role in blood flow control to rat hindlimb skeletal muscles. J Physiol 463: 631– 646, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Woodman CR, Price EM, Laughlin MH. Aging induces muscle-specific impairment of endothelium-dependent dilation in skeletal muscle feed arteries. J Appl Physiol 93: 1685– 1690, 2002 [DOI] [PubMed] [Google Scholar]
- 43. Woodman CR, Price EM, Laughlin MH. Shear stress induces eNOS mRNA expression and improves endothelium-dependent dilation in senescent soleus muscle feed arteries. J Appl Physiol 98: 940– 946, 2005 [DOI] [PubMed] [Google Scholar]
- 44. Woodman CR, Schrage WG, Rush JW, Ray CA, Price EM, Hasser EM, Laughlin MH. Hindlimb unweighting decreases endothelium-dependent dilation and eNOS expression in soleus not gastrocnemius. J Appl Physiol 91: 1091– 1098, 2001 [DOI] [PubMed] [Google Scholar]
- 45. Xiang L, Dearman J, Abram SR, Carter C, Hester RL. Insulin resistance and impaired functional vasodilation in obese Zucker rats. Am J Physiol Heart Circ Physiol 294: H1658– H1666, 2008 [DOI] [PubMed] [Google Scholar]
- 46. Xiang L, Naik J, Hester RL. Exercise-induced increase in skeletal muscle vasodilatory responses in obese Zucker rats. Am J Physiol Regul Integr Comp Physiol 288: R987– R991, 2005 [DOI] [PubMed] [Google Scholar]